Abstract
Introduction
Given the possibility of inadvertent bacterial contamination of salvaged blood, the use of cell salvage is relatively contraindicated in cases of reimplantation for chronic hip periprosthetic joint infection (PJI). However, there are no published data supporting this assertion. The purpose of the current study was to compare the reinfection rate and rate of postoperative allogeneic blood transfusion (ABT) in second-stage reimplantation for PJI with or without intraoperative cell salvage reinfusion.
Materials and methods
We identified 125 patients who underwent two-stage exchange for chronic hip PJI between November 2012 and April 2019. The groups of patients who had (n = 61) and had not (n = 64) received intraoperative cell salvage reinfusion were compared with respect to the curative infection-free rate. Moreover, we compared the need for postoperative ABT and identified independent factors associated with ABT using multiple regression analysis.
Results
The log-rank survival curve with an endpoint of infection eradication failure was not significantly different between the cell salvage group (98.4%, 95% CI 95.3–99.9%) and the control group (95.3%, 95% CI 90.2–99.9%) at one year (log rank, P = .330). The rates of postoperative ABT in the cell salvage group were significantly lower than those in the control group (11.5% vs 26.6%, P = .041). In multivariable models, patient age, body mass index, preoperative hemoglobin level, and intraoperative cell salvage were independent predictors of ABT exposure (P < .05).
Conclusions
The use of cell salvage during reimplantation in two-stage exchange for chronic hip PJI did not appear to increase the reinfection rate, while it significantly reduced the rate of postoperative allogeneic red blood transfusion. Greater age, lower BMI, lower preoperative hemoglobin, and non-intraoperative cell salvage reinfusion were associated with higher rate of allogeneic red blood transfusion.
Similar content being viewed by others
Introduction
Revision hip arthroplasty is a complex procedure that is associated with substantial perioperative blood loss and high allogeneic blood transfusion requirements [1]. However, allogeneic blood transfusion in revision total hip arthroplasty is associated with deleterious effects, including deep venous thrombosis, wound healing problems, and most importantly, an increased risk of periprosthetic joint infection (PJI) [2]. Numerous approaches are used to avoid allogeneic transfusions, including optimization of preoperative anemia, antifibrinolytic therapy, and the use of cell salvage systems [3,4,5]. Cell salvage offers an effective approach to reduce the need for allogeneic blood transfusion in primary total hip arthroplasty (THA) and aseptic revision [6]. However, the evidence for its use in patients undergoing two-stage PJI treatment remains unknown.
Historically, two-stage exchange arthroplasty using an antibiotic-loaded cement spacer is recognized as the “gold standard” for treating chronic PJI [7]. However, positive intraoperative cultures at second-stage reimplantation are reported to be found in up to 44% of patients [8], and the cumulative incidence of reinfection after two-stage exchange was 4% at 1 year and 14% at 5 years [9]. Given the possibility of persistent or undetectable infection and potential risk of bacterial dissemination, the use of cell salvage is relatively contraindicated in cases of hip revisions for PJI [10]. While several non-orthopedic studies specifically evaluated whether it is safe to reinfuse washed blood products in the setting of infection [11,12,13], their results demonstrated little, if any, evidence of bacterial dissemination from cell salvage devices [11, 12, 14, 15]. Otherwise, other orthopedic surgeons did not consider infection to be a contraindication to the use of cell salvage in the setting of revision hip surgery, which has sometimes been implemented in second-stage reimplantation for PJI [10, 16]. To date, no published data have been found in favor of or against the use of cell salvage in the setting of reimplantation for PJI. Compared with non-orthopedic surgeries, joint arthroplasty or revision is more demanding in terms of ensuring asepsis. Thus, the risks and benefits of using cell salvage during reimplantation must be weighed.
The objectives of the study were (1) to evaluate whether the use of cell salvage during reimplantation in two-stage exchange for PJI increases the reinfection rate, (2) to determine if the use of cell salvage during reimplantation decreases the need for postoperative allogeneic blood transfusion, and (3) to identify the potential factors associated with postoperative allogeneic blood transfusion. Our hypothesis was that the use of cell salvage during reimplantation for the treatment of chronic hip PJI would not increase the reinfection rate and may reduce the need for postoperative allogeneic blood transfusion.
Materials and methods
Study design and patients
Prior to conduction of the study, institutional Clinical Trials and Biomedical Ethics Committee approval was obtained. All patients knew the use of cell salvage was relatively contraindicated in cases of hip revisions for PJI and gave their written informed consent before reimplantation. We performed a single-center, retrospective, cohort study that enrolled consecutive patients who were treated for chronic hip PJI in a two-stage revision from November 1, 2012 to April 30, 2019, in which availability of second-stage culture results was mandatory. PJI was diagnosed according to the criteria published by the Musculoskeletal Infection Society and modified by the International Consensus Group as of 2014 [17], and chronic PJI was defined as any PJI present for more than 4 weeks from the index surgery [18]. Exclusion criteria comprised patients who (1) received intraoperative allogeneic blood transfusion or allograft bone transplantation during the second-stage reimplantation because these may increase the risk of reinfection and confound the analysis of reinfection sources; (2) had a known allergy to tranexamic acid (TXA), a history of arterial or venous thromboembolic event (e.g., stroke, pulmonary embolism, deep venous thromboembolism), coronary artery disease (placement of an arterial stent or myocardial infarction within the past six months), renal failure (serum creatinine > 200 mmol/l, creatinine clearance < 50 ml/min, dialysis), disseminated intravascular coagulation, hepatic failure, severe pulmonary disease; (3) had undergone preoperative anticoagulation therapy (excluding aspirin) or refusal of allogeneic blood transfusion; (4) treated with TXA in a way that deviated from the following standard practices in our institution from November 2012: TXA was routinely administrated a bolus (15 mg/kg) 5 min before incision, and administrated again if the duration of reimplantation exceeded 2 h. This study was conducted and reported in line with STROCSS 2019 criteria [19].
Two-stage revision procedure
All revision procedures were performed using a classical posterolateral approach by 4 senior surgeons who specialized in total joint arthroplasty. During the first-stage revision procedure, thorough debridement was completed to excise sinus tracts, all infected tissues, and devitalized bone after removal of all foreign materials. Then, the wounds were repeatedly cleansed in 3% hydrogen peroxide for 4–5 min, irrigated with 0.9% saline, and finally cleansed in 2.5% povidone iodine for 4–5 min. This is the standard procedure in cases of PJI in our institution. Broad-spectrum antibiotics were administrated intravenously after the surgical fields were thoroughly irrigated with saline using a low-pressure system. Five to eight solid samples, both bone and soft-tissue, and a sample of synovial fluid were routinely obtained in the procedure and sent for microbiological culture and histological examination. All hips underwent implantation of an antibiotic-impregnated, handmade polymethylmethacrylate bone cement spacer containing 2 g of vancomycin and 1 g gentamicin per pack of Palacos cement (Biomet, Warsaw, IN).
Postoperative antibiotic administration protocol was under the guidance of infectious diseases specialists according to the antimicrobial susceptibility test. In all cases of PJI, medical therapy was initiated using broad-spectrum antibiotics (typically vancomycin and cefuroxime). If the tissue sample cultures were positive, organism-specific antibiotics were administered; otherwise, the empirical antibiotics strategy was vancomycin and cefuroxime. Patients received intravenous antibiotics for 6 weeks and oral antibiotics for 6 weeks following the first-stage revision. Second-stage reimplantation was considered when the general status of the patient was suitable and there were no signs of infection, which was confirmed by the downtrend of C-reactive protein and erythrocyte sedimentation rate to normal or near normal levels.
The second-stage reimplantation was performed under targeted prophylactic-guided antibiotics. Synovial fluid was routinely taken for bacterial culture before antibiotic administration. Frozen sections were also routinely performed to exclude residual infection. Frozen sections with greater than 10 white blood cells per high-power field were considered to have persistent infection; 5 to 9 white blood cells per high-power field were considered to have suspicious infection; and less than 5 white blood cells per high-power field were considered to eradicate infection [20]. After removal of the bone cement spacer, the joint cavity was cleansed in hydrogen peroxide and povidone iodine and irrigated with saline which was consistent with the procedure of the first-stage revision. All patients had cementless, porous-coated, diaphyseal engaging non-modular femoral stems.
According to the policy of our institution, we employed intraoperative cell salvage collection (3000P, Jingjing Medical Equipment, Beijing, China) for all second-stage revision hip procedures. Any fluid visibly contaminated by infection, metallic debris, and cement was not collected. All blood from operative fields and gauze was centrifuged with a leucocyte depletion filter (40 µm, Nanjing Shuangwei, Nanjing, China) and washed with 1000 mL of 0.9% sodium chloride, and then transferred to a sterile collecting bag. The volume of salvaged blood was standardized to hematocrit 55%. As per the result of hemoglobin and hematocrit measured intraoperatively using blood gas analysis, salvaged blood was processed to transfuse once the estimated blood loss exceeded 500 ml. The patients who did not have intraoperative cell salvage transfusion were included in the control group as their estimated blood loss was less than 500 ml.
Strict transfusion criterions were implemented in keeping with the clinical practice guidelines recommended from the American Association of Blood Bank [21], postoperative allogenic blood transfusion was only allowed for patients with a hemoglobin level < 70 g/l or with a hemoglobin level between 80 and 100 g/l in the setting of pre-existing cardiovascular disease, active bleeding, arterial thromboembolic event or sepsis, persistent symptoms despite adequate volume resuscitation. Plasma was transfused if more than four blood units were transfused or if coagulation parameters were out of acceptable ranges. When allogeneic blood transfusion was indicated, 1 unit of packed red blood cells was transfused to increase Hb levels to 8.0 g/dl.
Systemic intravenous antibiotics against the microorganism isolated at the first-stage revision were maintained until microbiological results were available. In general, if synovial cultures were positive, organism-specific antibiotics were administered for 4 weeks and then orally for 4 weeks. If no microorganisms were identified, intravenous antibiotic strategy was the same as that for the first-stage revision for one week and then orally for an additional 2 weeks. If a new microorganism was identified in more than 2 samples, organism-specific systemic antibiotics were administrated for 8 weeks.
Assessments
We obtained demographic data as well as comorbidities, antibiotic administration, and culture results at the time point of reimplantation from all patients. McPherson’s host classification [22], patient-related risk factors (diabetes mellitus, inflammatory arthritis, chronic hepatitis, chronic anemia, tobacco use, alcoholism, resistant organism), component exchange, and positive culture are associated with an increase in reinfection rate. Hence, we obtained and compared these results between the 2 groups (Tables 1, 2).
Clinical follow-up was conducted routinely at 3 weeks, 3 months, and 6 months after two-stage revision and annually thereafter until the final follow-up. The definition of a successful treated infection was based on the modified Delphi-based international multidisciplinary criteria [17]: (1) a healed wound, without a fistula, drainage, or pain and without recurrence caused by the same organism, (2) no subsequent surgical intervention for persistent or peri-operative infection, (3) no occurrence of PJI-related mortality; (4) no requirement for long-term (> 6 months) suppressive antibiotic treatment. If one of these criteria was not met, infection eradication failure was considered as established.
Furthermore, we analyzed whether the use of cell salvage during reimplantation led to a decreased rate or volume in postoperative allogeneic blood transfusion and identified the risk factors for allogeneic blood transfusion. We recorded preoperative and postoperative hemoglobin levels, preoperative and postoperative hematocrit levels, postoperative allogeneic blood transfusion (rates and units) within 7 days of reimplantation, and the amount of blood from cell salvage reinfused during reimplantation. The calculated blood loss = the patient’s blood volume (PBV) * (Hctpre—Hctpost)/Hctave (Hctpre refers to the preoperative hematocrit level. Hctpost refers to the minimum hematocrit level before transfusion. Hctave refers to the average of Hctpre and Hctpost) [23]. PBV = k1 * height (m3) + k2 * weight (kg) + k3 (k1 = 0.3669, k2 = 0.03219, and k3 = 0.6041 for men; and k1 = 0.3561, k2 = 0.03308, and k3 = 0.1833 for women) [19, 24]. All hemoglobin and hematocrit levels were measured routinely up to day 5 after the procedure.
Statistical analysis
All statistical analyses were carried out using SPSS version 26 (IBM Corporation, Armonk, NY, USA). The normality of the distributions was tested for all scale variables by Kolmogorov–Smirnov’s test. Differences between groups were analyzed using Fisher’s exact test for categorical variables while continuous variables were compared by Mann–Whitney U test. Categorial variables are presented using counts and percentages, while continuous variables are summarized using the median with 25th and 75th percentiles. The primary analysis was to evaluate the influence of cell salvage during reimplantation by comparing the rate of infection eradication failure by Kaplan–Meier curve and log-rank test. Next, a multiple logistic regression was performed to identify independent variables associated with the need for allogeneic red blood transfusion. Covariates with a P value < 0.05 by univariate analysis were integrated stepwise into the multivariate regression model. For all comparisons, the level of statistical significance was set at P < 0.05. A post hoc power analysis (PASS, version 19.0) considered an alpha error probability of 0.05, a study power of 80%, a proportion of 30% of patients who did not receive intraoperative cell salvage reinfusion, and a relative risk of 2.5. The required sample size was 57 patients per group.
Results
Patients’ demographics
We initially identified a total of 141 patients with a minimum 2-year follow-up after reimplantation. Of these, patients who received intraoperative allogeneic blood transfusion (n = 4), those who received allograft bone transplantation (n = 3), those who had a history of deep venous thromboembolic event (n = 1), and those who did not follow the standard TXA practices for PJI in our institution (n = 7) were excluded. The final cohort consisted of 125 patients and was divided into 2 groups: patients who received intraoperative cell salvage reinfusion (n = 61) and those who did not receive intraoperative cell salvage reinfusion (n = 64), as the control group. Table 1 shows and compares baseline and perioperative characteristics between the cell salvage reinfused group and the control group; there was no significant difference observed between the 2 groups. The median follow-up time was 73.0 (53.0–89.0) months for all patients, 70.0 (54.5–94.0) months for the cell salvage group and 75.0 (46.3–84.8) months for the control group (P = 0.592). A total of 36 patients (28.8%) had ≥ 1 positive culture and 2 patients (1.6%) had ≥ 2 positive cultures at second-stage reimplantation (Table 2).
Infection eradication rate
There were 4 patients who were considered to have infection eradication failure in this study, one in the cell salvage reinfused group and 3 in the control group. The reinfection of the 4 patients occurred within one year. The microbiological results of the synovial fluid culture of the 4 patients are summarized in Table 3. The one-year infection-free rate was 98.4% (95% confidence interval 95.3–99.9%) for the cell salvage reinfused group and 95.3% (95% confidence interval 90.2–99.9%) for the control group (log-rank, P = 0.330).
Postoperative allogeneic blood transfusion
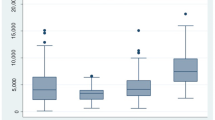
In total, 24/125 (19.2%) patients received allogeneic blood transfusion up to 7 days after reimplantation: 7/61 (11.5%) in the cell salvage reinfused group, and 17/64 (26.6%) in the control group. In relation to the proportion, the postoperative allogeneic red blood transfusion rate was significantly lower in patients who received cell salvage reinfusion than in the control group (11.5% vs 26.6%, P = 0.041). However, there was no significant difference observed in the rate of postoperative fresh frozen plasma transfusion between the 2 groups (6.6% vs 7.8%; P = 1.000). When comparing the volume of postoperative allogeneic red blood and fresh frozen plasma per case, there was also no significant difference between the 2 groups (2.0 units vs 1.5 units, P = 0.630; 300 ml vs 200 ml, P = 0.896). The majority of allogeneic red blood (14/25, 56.0%) was transfused on day 1. The calculated blood loss was significantly lower in patients in whom cell salvage was set up than in controls (846 ml vs 1195 ml, P = 0.002). The clinical results related to postoperative allogeneic blood transfusion are shown in Table 4.
Factors associated with postoperative allogeneic red blood transfusion
Univariate logistic regression analysis showed that age, BMI, preoperative hemoglobin, and intraoperative cell salvage reinfusion were associated with the rate of postoperative allogeneic red blood transfusion (P = 0.031, 0.004, 0.005, and 0.037, respectively). After adjustment for covariates with the use of the multivariate logistic model, greater age (hazard ratio (HR) 3.092, 95% CI 1.048–9.123, P = 0.041), lower BMI (HR 0.805, 95% CI 0.687–0.944, P = 0.007), lower preoperative Hb (HR 0.092, 95% CI 0.018–0.477, P = 0.004), and non-intraoperative cell salvage reinfusion (HR 0.176, 95% CI 0.051–0.608, P = 0.006) were identified as independent factors associated with a higher rate of postoperative allogeneic red blood transfusion. The results of the binary logistic regression analysis are summarized in Table 5.
Discussion
In our series of chronic hip PJIs managed with a two-stage revision protocol, we found an infection eradication failure rate of 3.2%. Receiving cell salvage during reimplantation did not increase the reinfection rate in our study. The use of cell salvage during reimplantation reduced the need for postoperative allogeneic red blood transfusion, confirming our hypothesis. Greater age, lower BMI, lower preoperative hemoglobin, and non-intraoperative cell salvage reinfusion were identified as independent factors associated with higher rate of postoperative allogeneic red blood transfusion (Table 5).
Reinfection is one of the most common complications after two-stage revision of PJI with severe medical and economic impacts on the affected patients and healthcare budgets [25]. Prior studies have been published regarding risk factors for reinfection after two-stage revision [26, 27], but no data have addressed cell salvage during reimplantation. Considering that contaminated blood caused by persistent or undetected infection may lead to bacteremia, sepsis, or the possibility of reinfection after revision, the use of cell salvage is relatively contaminated in cases of septic revisions [10]. However, several non-orthopedic studies have specifically evaluated whether it is safe to reinfuse these products in infection circumstances; Ozmen et al. [28] found that patients receiving washed blood collected from the peritoneal cavity during abdominal trauma exploration did not have increased wound infection compared with those who received bank blood, and Bowley et al. [29] reported that cell salvage during laparotomy for penetrating abdominal trauma did not increase the postoperative reinfection rate. Although several orthopedic surgeons also did not consider PJI as a relative contraindication to cell salvage which has sometimes been implemented in second-stage reimplantation, no evidence has been found in favor of or against the use of cell salvage during reimplantation. In the present study, we found similar results to previous non-orthopedic studies in which the use of cell salvage during reimplantation did not appear to increase the reinfection rate. One possible reason could be that almost all persistent bacteria during reimplantation were removed by a combination of cell washing and leukocyte depletion filtering. Waters et al. [14] showed that the combination of cell salvage washing and leukocyte depletion filtration resulted in a 97.6 to 100% removal of bacterial loads. Another possible reason may be that the reinfection rate after second-stage reimplantation in our cohorts was significantly lower than that in previous studies [9, 26, 30, 31], which might be insufficient to detect significant differences.
Few absolute contraindications have been clearly proposed for cell salvage [10]. Due to end-organ damage as a result of administering lysed red blood cells, anything that results in red cell lysis or destruction is defined as a definite or absolute contraindication [32]. In terms of blood contamination caused by undetected infection of PJI, reinfusion of such blood is of theoretical risk of reinfection. In fact, bacterial contamination of salvaged blood appears to be common [11, 33]. Previous studies have demonstrated that cell salvage can be used safely in the face of bacterial contamination and noted that washing and filtration can remove bacterial contaminants up to a concentration of 103 cfu/ml [14]. For patients undergoing second-stage reimplantation, bacterial loads of positive cultures in the blood are low concentration after administering systematic antibiotics and strictly following the indications for second-stage reimplantation. Thus, we consider that the use of cell salvage during second-stage reimplantation for PJI will not increase the reinfection rate.
There is ongoing discussion about the effect of cell salvage on the need for additional allogeneic blood transfusion [34]. Previous studies demonstrated that the use of cell salvage significantly decreased the allogeneic transfusion requirement in aseptic hip revision [34, 35]. However, unlike aseptic hip revision, procedures performed for PJI are associated with more complex surgical techniques and higher blood loss [16]. In our cohorts, we found that patients receiving cell salvage during reimplantation had a significantly lower exposure rate of postoperative allogeneic red blood transfusion, but a similar volume of allogeneic red blood transfusion. These findings are in line with the results of aseptic hip revisions reported in former studies [34, 35]. However, the rate of postoperative allogeneic transfusion in the cell salvage group (11.5%) was significantly lower than the previously reported rates, of 37% and 55% [34, 35]. A lower allogeneic transfusion rate may demonstrate development in patient blood management, including the use of antifibrinolytic agents (such as TXA), more efficient cell salvage, and improvement in the surgical technique of revision for PJI.
We found that patients with greater age, lower BMI, lower preoperative Hb (< 120 g/l), and non-receiving transfusion were more likely to receive postoperative allogeneic blood transfusion. These findings were similar to the results of primary THA and aseptic hip revisions [36,37,38]. In a large cohort study by Adam et al. [36], age (HR per ten years = 10.1) and BMI of ≤ 30 kg/m2 (HR = 1.4) were found to be significant predictors for receiving allogeneic transfusion after THA. Slover et al. [37] reported, in a statewide database, similar results that greater age had a significantly higher odds of red blood transfusion after THA. Walsh et al. reported that preoperative hemoglobin level (HR = 0.35) was an independent predictor of postoperative allogeneic blood transfusion after aseptic hip revision [38]. Importantly, the use of cell salvage had a protective effect on the risk of postoperative allogeneic blood transfusion, suggesting that the use of cell salvage during reimplantation for PJI was clinically beneficial. Our study justified the routine use of cell salvage during reimplantation for PJI patients with greater age and lower BMI, and strongly supported the use for patients with preoperative hemoglobin less than 120 g/l.
While this is the first study evaluating the safety and efficacy of cell salvage during second-stage reimplantation by a standardized diagnostic and therapeutic algorithm for PJI, it has several limitations. First, the retrospective design decreased the level of evidence and implies selection and recall bias. Second, the small sample size, especially the relative infrequency of reinfection rate (3.2%), might be underpowered to reveal differences in the use of cell salvage and predict risk factors for reinfection after surgery. Therefore, the effect of the use of cell salvage during reimplantation on the reinfection rate in this study needs to be interpreted with caution and studies with larger sample sizes are needed. Third, four different surgeons used cell salvage during second-stage reimplantation, which inevitably led to variability. However, each of the 4 surgeons had a high volume of PJI cases every year, performed similar surgical techniques, and followed the same antibiotic protocols in treating patients with PJIs.
Conclusion
The use of cell salvage during reimplantation in two-stage exchange for chronic hip PJI did not appear to increase the reinfection rate, while it significantly reduced the rate of postoperative allogeneic red blood transfusion. Greater age, lower BMI, lower preoperative hemoglobin, and non-intraoperative cell salvage use were identified as risk factors for higher rate of postoperative allogeneic red blood transfusion.
Availability of data and materials
Please contact author for data requests.
Abbreviations
- PJI:
-
Periprosthetic joint infection
- ABT:
-
Allogeneic blood transfusions
- THA:
-
Total hip arthroplasty
- TXA:
-
Tranexamic acid
- PBV:
-
Patient’s blood volume
- PASS:
-
Post hoc power analysis
- BMI:
-
Body mass index
- HR:
-
Hazard ratio
References
Goel R, Buckley P, Sterbis E, Parvizi J. Patients with infected total hip arthroplasty undergoing 2-stage exchange arthroplasty experience massive blood loss. J Arthroplasty. 2018;33(11):3547–50.
Kim JL, Park JH, Han SB, Cho IY, Jang KM. Allogeneic blood transfusion is a significant risk factor for surgical-site infection following total hip and knee arthroplasty: a meta-analysis. J Arthroplasty. 2017;32(1):320–5.
Munoz M, Acheson AG, Auerbach M, Besser M, Habler O, Kehlet H, et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia. 2017;72(2):233–47.
Peck J, Kepecs DM, Mei B, Safir OA, Backstein D, Gross AE, et al. The effect of preoperative administration of intravenous tranexamic acid during revision hip arthroplasty: a retrospective study. J Bone Joint Surg Am. 2018;100(17):1509–16.
Klein AA, Bailey CR, Charlton AJ, Evans E, Guckian-Fisher M, McCrossan R, et al. Association of anaesthetists guidelines: cell salvage for peri-operative blood conservation 2018. Anaesthesia. 2018;73(9):1141–50.
Dusik CJ, Hutchison C, Langelier D. The merits of cell salvage in arthroplasty surgery: an overview. Can J Surg. 2014;57(1):61–6.
Mortazavi SM, Vegari D, Ho A, Zmistowski B, Parvizi J. Two-stage exchange arthroplasty for infected total knee arthroplasty: predictors of failure. Clin Orthop Relat Res. 2011;469(11):3049–54.
Cabo J, Euba G, Saborido A, Gonzalez-Panisello M, Dominguez MA, Agullo JL, et al. Clinical outcome and microbiological findings using antibiotic-loaded spacers in two-stage revision of prosthetic joint infections. J Infect. 2011;63(1):23–31.
Petis SM, Perry KI, Mabry TM, Hanssen AD, Berry DJ, Abdel MP. Two-stage exchange protocol for periprosthetic joint infection following total knee arthroplasty in 245 knees without prior treatment for infection. J Bone Joint Surg Am. 2019;101(3):239–49.
Esper SA, Waters JH. Intra-operative cell salvage: a fresh look at the indications and contraindications. Blood Transfus. 2011;9(2):139–47.
Bland LA, Villarino ME, Arduino MJ, McAllister SK, Gordon SM, Uyeda CT, et al. Bacteriologic and endotoxin analysis of salvaged blood used in autologous transfusions during cardiac operations. J Thorac Cardiovasc Surg. 1992;103(3):582–8.
Verwaal VJ, Wobbes T, Koopman-Van Gemert AW, Buskens FG, Theeuwes AG. Effect of perioperative blood transfusion and cell saver on the incidence of postoperative infective complications in patients with an aneurysm of the abdominal aorta. Eur J Surg. 1992;158(9):477–80.
Nessly ML. Infection and cell-saver use. Ann Thorac Surg. 1990;50(3):509–10.
Waters JH, Tuohy MJ, Hobson DF, Procop G. Bacterial reduction by cell salvage washing and leukocyte depletion filtration. Anesthesiology. 2003;99(3):652–5.
Schwieger IM, Gallagher CJ, Finlayson DC, Daly WL, Maher KL. Incidence of cell-saver contamination during cardiopulmonary bypass. Ann Thorac Surg. 1989;48(1):51–3.
Palmer AJR, Lloyd TD, Gibbs VN, Shah A, Dhiman P, Booth R, et al. The role of intra-operative cell salvage in patient blood management for revision hip arthroplasty: a prospective cohort study. Anaesthesia. 2020;75(4):479–86.
Parvizi J, Gehrke T, International Consensus Group on Periprosthetic Joint Infection (2014) Definition of periprosthetic joint infection. J Arthroplasty 29(7):1331
Tsukayama DT, Goldberg VM, Kyle R (2003) Diagnosis and management of infection after total knee arthroplasty. J Bone Joint Surg Am 85-A Suppl 1:S75–80
Agha R, Abdall-Razak A, Crossley E, Dowlut N, Iosifidis C, Mathew G, et al. STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int J Surg. 2019;72:156–65.
Della Valle CJ, Bogner E, Desai P, Lonner JH, Adler E, Zuckerman JD, et al. Analysis of frozen sections of intraoperative specimens obtained at the time of reoperation after hip or knee resection arthroplasty for the treatment of infection. J Bone Joint Surg Am. 1999;81(5):684–9.
Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, et al. Red blood cell transfusion: a clinical practice guideline from the AABB*. Ann Intern Med. 2012;157(1):49–58.
Mcpherson EJ, Woodson C, Holtom P, Roidis N, Shufelt C, Patzakis M. Periprosthetic total hip infection: outcomes using a staging system. Clin Orthop Relat Res. 2002;403:8–15.
Gross JB. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983;58(3):277–80.
Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51(2):224–32.
Corona PS, Vicente M, Carrera L, Rodriguez-Pardo D, Corro S. Current actual success rate of the two-stage exchange arthroplasty strategy in chronic hip and knee periprosthetic joint infection. Bone Joint J 2020;102-B(12):1682–1688
Theil C, Freudenberg SC, Gosheger G, Schmidt-Braekling T, Schwarze J, Moellenbeck B. Do positive cultures at second stage re-implantation increase the risk for reinfection in two-stage exchange for periprosthetic joint infection? J Arthroplasty. 2020;35(10):2996–3001.
Corro S, Vicente M, Rodriguez-Pardo D, Pigrau C, Lung M, Corona PS. Vancomycin-gentamicin prefabricated spacers in 2-stage revision arthroplasty for chronic hip and knee periprosthetic joint infection: insights into reimplantation microbiology and outcomes. J Arthroplasty. 2020;35(1):247–54.
Ozmen V, McSwain NE Jr, Nichols RL, Smith J, Flint LM. Autotransfusion of potentially culture-positive blood (CPB) in abdominal trauma: preliminary data from a prospective study. J Trauma. 1992;32(1):36–9.
Bowley DM, Barker P, Boffard KD. Intraoperative blood salvage in penetrating abdominal trauma: a randomised, controlled trial. World J Surg. 2006;30(6):1074–80.
Frank JM, Kayupov E, Moric M, Segreti J, Hansen E, Hansen E et al. The Mark Coventry, MD, Award: oral antibiotics reduce reinfection after two-stage exchange: a multicenter, randomized controlled trial. Clin Orthop Relat Res 2017; 475(1):56-61
Akgun D, Muller M, Perka C, Winkler T (2017) A positive bacterial culture during re-implantation is associated with a poor outcome in two-stage exchange arthroplasty for deep infection. Bone Joint J 99-B(11):1490–1495
From the Centers for Disease Control and Prevention (1999) Hemolysis associated with 25% human albumin diluted with sterile water—United States, 1994–1998. JAMA 281(12):1076–7
Kang Y, Aggarwal S, Pasculle AW, Freeman JA, Martin LK. Bacteriologic study of autotransfusion during liver transplantation. Transplant Proc. 1989;21(3):3538.
Bridgens JP, Evans CR, Dobson PM, Hamer AJ (2007) Intraoperative red blood-cell salvage in revision hip surgery: a case-matched study. J Bone Joint Surg Am 89(2):270–275
Garvin KL, Feschuk CA, Sekundiak TD, Lyden ER. Blood salvage and allogenic transfusion needs in revision hip arthroplasty. Clin Orthop Relat Res. 2005;441:205–9.
Hart A, Khalil JA, Carli A, Huk O, Zukor D, Antoniou J (2014) Blood transfusion in primary total hip and knee arthroplasty. Incidence, risk factors, and thirty-day complication rates. J Bone Joint Surg Am 96(23):1945–51
Slover J, Lavery JA, Schwarzkopf R, Iorio R, Bosco J, Gold HT. Incidence and risk factors for blood transfusion in total joint arthroplasty: analysis of a statewide database. J Arthroplasty. 2017;32(9):2684–7.
Walsh TS, Palmer J, Watson D, Biggin K, Seretny M, Davidson H, et al. Multicentre cohort study of red blood cell use for revision hip arthroplasty and factors associated with greater risk of allogeneic blood transfusion. Br J Anaesth. 2012;108(1):63–71.
Acknowledgements
We would like to thank the staff of the Department of Orthopedic Surgery, West China Hospital.
Funding
This research was supported by Key Research & Development program of Science & Technology Department of Sichuan Province (No. 2018SZ0255) and 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (No. ZYJC18039). The founders had no role in study design, data collection, data analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
ZL and XY applied for ethical and registered this study, drafted the work, and revised it critically for important intellectual content. ZL and XY contributed equally to this work and should be considered as equal first authors. E-ZZ, XW, and GC collected data and analyzed data for the study. ZZ contributions to the design of the work and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study was approved by the Ethics Committee and Institutional Review Board of West China Hospital, Sichuan University (2012-268). Informed consent was obtained from each patient.
Consent for publication
No conflict of interest exits in the submission of this manuscript, and the manuscript approved by all authors for publication.
Competing of interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Z., Yang, X., Zhao, EZ. et al. The use of cell salvage during second-stage reimplantation for the treatment of chronic hip periprosthetic joint infection: a retrospective cohort study. J Orthop Surg Res 17, 85 (2022). https://doi.org/10.1186/s13018-022-02955-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-02955-3