Abstract
Background
The purpose of this retrospective study was to investigate the determinants of postoperative respiratory failure in elderly patients with hip fracture.
Methods
The subjects of this study were 663 elderly patients who had hip fracture and had been treated with hip surgery at our hospital from January 2014 to May 2020. According to the occurrence of postoperative respiratory failure, 626 patients with no respiratory failure were retrospectively included in the control group, and 37 cases combined with respiratory failure were enrolled in the PRF group. The clinical and surgical data of the two groups were collected and analyzed to evaluate the determinants of respiratory failure by logistic regression analysis.
Results
There were no significant differences in the demographics and baseline variables including age, gender, fracture type and location between the groups (P > 0.05). All patients received hip surgery including total hip arthroplasty (THA), hemiarthroplasty (HA) and internal fixation with PFNA (proximal femoral nail anti-rotation). There were no significant differences in operative time and intraoperative blood loss between the groups (P > 0.05). However, close associations were found between pulmonary hypertension (univariate analysis: OR = 3.792, 95% CI = 1.421–10.203; multivariate analysis: OR = 1.132, 95% CI = 1.003–1.251), obstructive pulmonary disease (OR = 1.119, 95% CI = 1.009–1.238; multivariate analysis: OR = 13.298, 95% CI = 4.021–43.298), bronchiectasis and emphysema (OR = 4.949, 95% CI = 1.919–9.873; multivariate analysis: OR = 11.231, 95% CI = 187.87), and history of respiratory failure (OR = 6.098, 95% CI = 2.012–12.198; multivariate analysis: OR = 8.389, 95% CI = 2.391–21.982) with postoperative respiratory failure (P < 0.05).
Conclusion
Pulmonary hypertension, obstructive pulmonary disease, bronchiectasis, emphysema, history of respiratory failure, and hypoproteinemia may be risk factors for postoperative respiratory failure in elderly patients with hip fracture.
Similar content being viewed by others
Background
With an increasing aging population in China, osteoporotic hip fracture remains a crucial health issue because it is related to a high mortality and morbidity, and costs [1]. However, most elderly patients suffering from hip fracture have different levels of comorbidity; meanwhile, traditional conservative treatment requires prolonged recumbency, and is accompanied with multiple adverse events, and healing is difficult to achieve, and even death may ensue. As a result, it is recommended that surgical treatment should be conducted as early as possible.
Previous data showed that the 1-year mortality rate of elderly patients with hip fracture was 8 times that of the same age group without hip fracture, and the mortality rate of males was significantly higher than that of females [2]. Among various postoperative complications in elderly patients with hip fracture, the incidence of wound infection and internal fixation failure caused by fracture surgery is low. As a matter of fact, respiratory complications, including respiratory failure and pneumonia, are most common, and delirium is the second most common, with an incidence of 4.1–14.1% during hospitalization, and is more harmful [3]. Postoperative respiratory failure (PRF) is one of the most common complications in elderly patients with hip fracture and could lead to longer hospital stays, higher expenses and increased mortality [4].
Considering the high mortality rate of PRF in elderly patients with hip fracture, it has become a key topic of clinical research to identify the risk factors of PRF. However, there has been a paucity of reports on PRF in elderly patients after hip surgery. In order to optimize postoperative outcomes and prevent complications, it is critical to identify patients at high risk of PRF preoperatively. Therefore, this prospective study aimed to explore the determinants of PRF in elderly patients after THA.
Methods
Study population
The study protocol was approved by the Institutional Ethics Committee of Hebei General Hospital. The participants were informed about the study and signed written informed consent. All the experimental protocols were conducted in accordance with the Declaration of Helsinki.
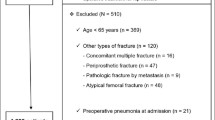
The data were collected as part of routine patient care between January 2014 and May 2020. The inclusion criteria were as follows: (1) diagnosis of trochanteric fracture or femoral neck fractures by X-ray, CT, and 3D reconstruction; (2) hip surgery including total hip arthroplasty, hemiarthroplasty and internal fixation with PFNA; (3) ability to stand and walk before fracture; (4) complete clinical data; (5) unilateral hip fracture; (6) hospitalization for surgical treatment; (7) no pathological fracture. The exclusion criteria were as follows: (1) severe coagulation dysfunction; (2) severe femoral proximal deformity; (3) severe hepatic renal failure; (4) complications or concomitant multiple injuries in other organs; (5) cerebrovascular disease within 3 months; (6) combined neurotropic joint disease or autoimmune disease; (7) malignancy; (8) loss to follow-up. Finally, 663 patients were enrolled in this study. The recruited cases were divided into two groups as the control group (n = 626) and the PRF group (n = 37) according to the occurrence of PRF.
Observation indicator
General information included age, sex, blood routine and biochemical examination, preoperative bed time, hypertension, cerebrovascular disease, diabetes and renal insufficiency, and pulmonary disease.
Operation-related indicators included operative time and intraoperative blood loss.
Statistical analysis
Excel 2016 was used to collect data, and SPSS 23.0 was used to analyze the data. Mean ± SD was used to represent measurement data, and t-test was used for analysis. Categorical data were expressed by rate (%), and chi-square test was used for analysis. The risk factors of PRF in elderly patients with hip fracture were analyzed by logistic regression. P < 0.05 indicated significant difference.
Results
Baseline characteristics
The PRF group included 21 males and 16 females with a range of age of 67–83 years and an average age of (73.03 ± 9.02) years. The fracture types included 23 trochanteric fractures and 14 neck fractures. In the control group, 359 males and 267 females aged from 67 to 82 years, with an average age of (73.29 ± 9.09) years. Fracture types included 296 trochanteric fracture and 330 femoral neck fracture. In addition, the types of fracture and position were compared between the two groups. The results showed no difference in these variables. Therefore, the general data of the two groups were comparable (P > 0.05, Table 1).
The comparison of operation-related indicators
There were no significant differences in operative time and intraoperative blood loss between the two groups (P > 0.05), as shown in Table 2.
The comparison of underlying diseases
Comparison of the rates of pulmonary hypertension, hypoproteinemia, obstructive pulmonary disease, bronchiectasis, emphysema and previous respiratory failure history in the two groups showed significant differences (P < 0.05). However, no difference was found in the rates of hypertension and diabetes, and preoperative bed time between the two groups (P > 0.05). The comparisons of underlying diseases are shown in Table 3.
The potential risk factors of PRF in regression analysis
Taking the occurrence of PRF as the dependent variable and the factors with differences in the above data, such as pulmonary hypertension, hypoproteinemia, obstructive pulmonary disease, bronchiectasis and emphysema, and previous history of respiratory failure as independent variables, univariate logistic regression analysis showed that pulmonary hypertension, obstructive pulmonary disease, bronchiectasis and emphysema, and history of respiratory failure were all risk factors of PRF in elderly patients after hip surgery, and the differences were significant (P < 0.05), as shown in Table 4. Multivariate logistic regression analysis showed that pulmonary hypertension, obstructive pulmonary disease, bronchiectasis and emphysema, and previous history of respiratory failure were all risk factors of PRF in elderly patients with hip fracture, with significant differences (P < 0.05), as shown in Table 5.
Discussion
In this study, the proportion of elderly patients with hip fracture complicated with PRF was 5.58% (37/663), which is consistent with the results of Hung’s research [3]. Due to the characteristics of elderly patients with hip fracture, various complications easily develop. Hip surgery is one of the effective methods for the treatment of hip fracture, which can effectively relieve pain, improve joint function, and enhance the patients’ quality of life [5]. Respiratory failure is a common complication in elderly patients with hip fracture, which not only affects the normal physical function and metabolism of patient, but also has an important influence on the prognosis of elderly patients with hip fracture.
However, the mechanism of PRF after hip surgery remains unclear and may be the result of multiple factors. At present, there are few clinical studies on PRF in elderly patients with hip fracture. To our knowledge, this is the first study to analyze the risk factors of PRF divided into groups after hip surgery in a large sample population. According to an review, alterations in respiratory physiology associated with aging must be appreciated to anticipate and minimize potential complications associated with surgery and anesthesia in the elderly [6].
In our study, all elderly patients received intraspinal anesthesia to minimize intraoperative respiratory perturbations. However, older patients are accompanied by underlying diseases that cannot be avoided, like hypertension, diabetes, malnutrition, and cardiopulmonary disease. Meanwhile, the results of this study showed that the rates of pulmonary hypertension, obstructive pulmonary disease, bronchiectasis and emphysema, history of respiratory failure and hypoproteinemia were significant different between the control group and the PRF group (P < 0.05). It is suggested that PRF is more likely to occur in elderly patients with pulmonary hypertension, hypoproteinemia, obstructive pulmonary disease, bronchiectasis and emphysema, history of respiratory failure, and hypoproteinemia after hip surgery.
Pulmonary hypertension is a common disease of the body's respiratory and circulatory system. Increased pulmonary vascular pressure and resistance, and even vessel occlusion and muscular pulmonary vascular plexus lesions not only restrict the body's respiratory function, but also induce respiratory exhaustion and death [7].
In addition, especially elderly patients, due to the deterioration of physical function, face the phenomenon of cardiopulmonary function compensation, reduced stress ability and anti-hypoxia ability, further aggravating disease progression. Hypoproteinemia is one of the important indicators affecting acute diseases. Due to the poor viscera function in elderly patients and the need for anesthesia during hip surgery, liver function is further affected and albumin synthesis is inhibited. In addition, because surgery increases capillary permeability, resulting in increased albumin leakage. Moreover, catabolism increases and albumin consumption rises under surgical stress [8]. Data showed that hypoproteinemia is very common in elderly patients with hip fracture after surgery, and hypoproteinemia in elderly patients is easy to induce serious complications such as heart failure, pleural effusion, lung infection and brain dysfunction, which is not conducive to postoperative recovery [9].
Chronic obstructive pulmonary disease (COPD) is still a common disease globally. Patients have characteristic restricted respiratory air flow, damage to the lung function and irreversible development sustainability. Respiratory failure is the end stage of COPD. Respiratory failure is hard to cure and death easily occurs because of the compled etiology of respiratory failure [10, 11]. Furthermore, one study showed that a history of COPD, dyspnea at rest, dependent functional status, and malnutrition were independently associated with higher rates of PRF [12]. Therefore, it is suggested that respiratory failure is more likely to develop in hip fracture patients with COPD.
Bronchial dilatation is caused by a variety of bronchial diseases and irresupence expansion, and emphyloedema can damage the alveoli and the disease causes the patient to breathe oxygen and discharge carbon dioxide, leading to hypoxia, lung damage, and breathing difficulties, finally respiratory failure, and may even jeopardize the patient's life.
Our univariate logistic regression analysis showed that pulmonary hypertension, obstructive pulmonary disease, bronchiectasis and emphysema, and history of respiratory failure were all risk factors of PRF in elderly patients with hip fracture. Our multivariate logistic regression analysis further revealed that pulmonary hypertension, obstructive pulmonary disease, bronchiectasis and pulmonary emphysema, a history of respiratory failure and hypoalbuminemia were independent risks of elderly patients. It is suggested that the risk factors of PRF in elderly patients with hip fracture include pulmonary hypertension, obstructive pulmonary disease, bronchiectasis and emphysema, and history of respiratory failure.
This study further analyzed surgical indicators and found no difference in operative time, incision length, intraoperative blood loss, postoperative drainage volume and time to ambulation between the two groups. It is suggested that PRF in elderly patients with hip fracture may not be related to surgical indicators, but the specific mechanism needs further study.
However, due to the small number of patients involved and single-center study, there may be group bias, and some indicators cannot fully reflect the overall situation of hip fracture, which should be confirmed by a randomized controlled multi-center study in the future.
Conclusion
The risk factors of PRF in elderly patients after hip surgery included pulmonary hypertension, obstructive pulmonary disease, bronchiectasis and emphysema, and a history of respiratory failure. Therefore, surgeons should pay attention to the above factors in elderly patients. A detailed and comprehensive preoperative evaluation is essential. As for the adjustable indicators, preoperative adjustment of the patient's physiological status to acceptable range, consultation with relevant departments, and effective non-surgical treatment will improve the quality of life of patients as much as possible.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
25 May 2022
A Correction to this paper has been published: https://doi.org/10.1186/s13018-022-03164-8
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- PRF:
-
Postoperative respiratory failure
- THA:
-
Total hip arthroplasty
References
Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51:364–70.
Flikweert ER, Wendt KW, Diercks RL, Izaks GJ, Landsheer D, Stevens M, Reininga IHF. Complications after hip fracture surgery: are they preventable? Eur J Trauma Emerg Surg. 2018;44:573–80.
Hung WW, Egol KA, Zuckerman JD, Siu AL. Hip fracture management: tailoring care for the older patient. JAMA. 2012;307:2185–94.
Canet J, Gallart L. Postoperative respiratory failure: pathogenesis, prediction, and prevention. Curr Opin Crit Care. 2014;20:56–62.
Ouanezar H, Jalaguier T, Franck F, Pibarot V, Bothorel H, Saffarini M, Piton JP. Mid-term outcomes of titanium modular neck femoral stems in revision total hip arthroplasty. Ann Transl Med. 2019;7:92.
Sprung J, Gajic O, Warner DO. Review article: age related alterations in respiratory function—anesthetic considerations. Can J Anaesth. 2006;53:1244.
Vahdatpour C, Ryan J, Zimmerman J, MacCormick S, Palevsky H, Alnuaimat H and Ataya A. Advanced airway management and respiratory care in decompensated pulmonary hypertension. Heart Fail Rev 2021
Calverley PMA. Respiratory failure in chronic obstructive pulmonary disease. Eur Respir J. 2003;22:26s–30s.
Sim S, Sim Y, Tay K, Howe T, Png M, Chang C, Abdullah H, Koh J. Preoperative hypoalbuminemia: poor functional outcomes and quality of life after hip fracture surgery. Bone. 2021;143:115567.
MacLeod M, Papi A, Contoli M, Beghé B, Celli B, Wedzicha J, Fabbri L. Chronic obstructive pulmonary disease exacerbation fundamentals: diagnosis, treatment, prevention and disease impact. Respirology (Carlton, Vic). 2021;26:532–51.
Raveling T, Vonk J, Struik F, Goldstein R, Kerstjens H, Wijkstra P, Duiverman M. Chronic non-invasive ventilation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2021;8:CD002878.
Fischer J, Shang E, Butler C, Nelson J, Braslow B, Serletti J, Kovach S. Validated model for predicting postoperative respiratory failure: analysis of 1706 abdominal wall reconstructions. Plast Reconstr Surg. 2013;132:826e–35e.
Acknowledgements
None.
Funding
This study was supported by Key Research Projects in Medical Science (2017) (Grant No. 20170278).
Author information
Authors and Affiliations
Contributions
JC and ZT designed the study, collected and analyzed the data, and wrote the manuscript. HZ, LS, WB, TH, JZ and NG collected the data, and revised the manuscript. WL designed the study, collected the data, and revised the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Ethics Committee of Hebei General Hospital. The participants were informed about the study and signed the written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: the methods and conclusion section have been updated.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, J., Tian, Z., Zhang, H. et al. Risks of postoperative respiratory failure in elderly patients after hip surgery: a retrospective study. J Orthop Surg Res 17, 140 (2022). https://doi.org/10.1186/s13018-022-02909-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-02909-9