Abstract
Background
Free flaps have been a useful modality in the management of lower extremity osteomyelitis particularly in limb salvage. This study aimed to determine the factors affecting the outcome of free flap reconstruction in the treatment of osteomyelitis.
Methods
This retrospective study assessed 65 osteomyelitis patients treated with free flap transfer from 2015 to 2020. The treatment outcomes were evaluated in terms of the flap survival rate, recurrence rate of osteomyelitis, and amputation rate. The correlation between outcomes and comorbidities, causes of osteomyelitis, and treatment modalities was analyzed. The following factors were considered: smoking, peripheral artery occlusive disease, renal disease, diabetic foot ulcer, flap types, using antibiotic beads, and negative pressure wound therapy.
Result
Among the 65 patients, 21 had a severe peripheral arterial occlusive disease. Osteomyelitis developed from diabetic foot ulcers in 28 patients. Total flap failure was noted in six patients, and osteomyelitis recurrence was noted in eight patients, for which two patients underwent amputation surgery during the follow-up period. Only end-stage renal disease had a significant correlation with the recurrence rate (odds ratio = 16.5, p = 0.011). There was no significant relationship between outcomes and the other factors.
Conclusion
This study showed that free flaps could be safely used for the treatment of osteomyelitis in patients with comorbidities and those who had osteomyelitis developing from diabetic foot ulcers. However, care should be taken in patients diagnosed with end-stage renal disease.
Similar content being viewed by others
Background
Osteomyelitis (OM) has been one of the most difficult complications. Patients with OM have to face the possibility of amputation that can adversely affect their quality of life [1]. The treatment of OM aims to eradicate infection, obliterate dead space, and cover soft-tissue defects. Over the last three decades, free tissue transfer has been an important option that can overcome the limitations of typical methods such as skin grafts, local flaps, or muscle flaps. Free flaps can provide a wide range of tissues including skin, muscle, bone, or a combination of these to allow for more aggressive resection of affected tissues. Consequently, this decreases the recurrence rate of osteomyelitis and increases the rate of limb salvage. Numerous studies have reported favorable results of using free flaps in the treatment of osteomyelitis [2,3,4]. However, to the best of our knowledge, factors affecting the operative results have not been well established. Therefore, we aimed to determine whether co-morbidities and other factors could influence the outcome of using free flaps in the treatment of lower extremity osteomyelitis.
Patients and methods
This retrospective study was approved by the Institutional Review Board of our medical center (AJIRB-MED-MDB-16-402) and we assessed patient records from 2015 to 2020. Sixty-five patients diagnosed with osteomyelitis and treated with free flaps were included. The average follow-up period was 18 months (range, 6 to 48 months). Patients with incomplete reports or those who followed up for less than 6 months were excluded. Patients under 16 years of age were also excluded from this study.
The following data was collected via patient charts: demography, radiographs of the lower extremity, details of the wounds and treatment, complications, and follow-up information. The outcomes of treatment were evaluated based on flap success rate, recurrence rate of OM, and amputation rate during the follow-up period. The correlation between outcomes and comorbidities, causes of osteomyelitis, and treatment modalities were analyzed.
Statistical analysis
Categorical variables were summarized as frequencies and percentages while continuous variables were expressed as mean and standard deviations. Chi-square and Fisher’s exact tests were used to analyze the difference in flap survival rate and the recurrence rate of osteomyelitis in patients with and without the following factors: smoking, peripheral artery occlusive disease (PAOD), end-stage renal disease (ESRD), diabetic foot ulcer, flap types, using antibiotic beads, and negative pressure wound therapy (NPWT). A p value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 20.0. (IBM Corp., Armonk, NY, USA).
Treatment protocol
The diagnosis of osteomyelitis was based on clinical symptoms; laboratory tests including WBC, ESR, CRP, tissue culture, and bone culture; and radiological images including plain X-rays, MRI, and bone scans. Simultaneously, patients were thoroughly examined for cardiac, endocrine, and renal conditions. These conditions were managed by specialist physicians whenever necessary. Lower extremity blood vessel status was also carefully evaluated. If CT-angiography was unclear, it was supplemented with traditional angiography. All of the patients with severe stenosis (greater than 75% of the diameter) or total occlusion underwent percutaneous transluminal angioplasty. Serial debridement was performed to radically resect the infected tissues including soft tissue and bone. Deep soft tissue and bone cultures were taken to confirm the diagnosis and direct the antibiotic treatment. Patients received broad-spectrum antibiotic treatment before culture results, and specific antibiotics following the confirmation of culture results. Antibiotic beads (Vancomycin) were used in 15 cases and NPWT was applied in 44 cases.
Reconstruction was performed once all the infected tissues were resected and the wound had a good blood supply. The operation began with appropriate debridement followed by dissection of the recipient vessels. Major arteries with higher blood pressure were preferred over small branches as the recipient vessels. These branches were preserved to prevent further damage. Arteriorrhaphy was attempted in all cases with an end-to-side approach; an end-to-end anastomosis was performed if the end-to-side approach was unsuccessful. The type of flap was decided according to the size and depth of the defect. Although the fasciocutaneous flap was most commonly used, myocutaneous flaps were selected to obliterate dead space in cases with deep defects.
Case reports
Case 1
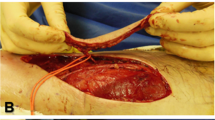
A 56-year-old male diabetic patient was referred to our department with diabetic foot osteomyelitis. He had been hypertensive for 20 years and diabetic for 24 years. CT-angiography revealed severe stenosis of the popliteal artery and total occlusion of the dorsalis pedis artery of his right leg. Immediate balloon angioplasty was performed. Serial debridement and minor amputation were done—his fourth and fifth toes were resected. A fasciocutaneous anterolateral thigh free flap (ALT) was applied to completely cover the defect with antibiotic beads inserted underneath. Due to atherosclerosis, the anastomosis was performed in an end-to-side fashion to the anterior tibial artery proximal to the occlusion. The flap healed uneventfully and the patient was ambulatory during 8 months of follow-up (Fig. 1).
Case 2
A 55-year-old man, diabetic for 20-years, was admitted for the development of wet gangrene in his fifth toe. The toe was resected, and serial debridement was performed. Preoperative angioplasty indicated the absence of blood flow from the posterior tibial artery to the pedal arch due to total occlusion. He underwent balloon angioplasty of the left posterior tibial artery and plantar artery. After angioplasty, a complete pedal arch was seen with the supply from both the dorsalis pedis artery and the plantar artery. A myocutaneous ALT flap was designed and harvested based on the size of the defect. The flap was then anastomosed to the anterior tibial artery in an end-to-side manner. No additional surgery was required. Forty-one months of follow-up revealed a well-healed, well-perfused free flap without any sign of osteomyelitis recurrence (Fig. 2).
Results
Patient demographics are listed in Table 1. A total of 65 patients with lower leg osteomyelitis were treated with microvascular free flaps. The mean age was 51.2 ± 15.8 (range, 18 to 82 years), with 49 male patients and 16 female patients. Twenty-four patients were active smokers. Thirty-one patients had diabetes, 21 had severe obstruction of lower extremity arteries, which needed angioplasty, and five patients had ESRD. The defects were most commonly located in the foot (43.1%), followed by the tibia, heel, and ankle (14 patients, 13 patients, and 6 patients, respectively). Twenty-nine patients developed osteomyelitis following trauma, 28 patients had diabetic foot ulcer osteomyelitis. The other causes were pressure sore, burn, skin infection.
The ALT flap was most commonly used (92.3%) followed by three medial sural artery perforator flaps, one superficial circumflex iliac perforator flap, and one thoracodorsal artery perforator flap. Out of 65 cases, total flap loss was seen in six patients (9.23%). Three of the six flap failures were successfully replaced with new fasciocutaneous free flaps. The other three patients underwent additional debridement with split-thickness skin grafts or NPWT and secondary healing.
Recurrence of OM was seen in eight patients (12.3%). Amongst these, two patients underwent below the knee amputation, one patient underwent another ALT free flap surgery and five patients were treated with minor debridement and oral antibiotics. Both patients who underwent major amputation suffered from serious medical conditions with diabetic foot ulcers, ESRD, and severe occlusion of the lower limb arteries. Although they successfully underwent angioplasty, one patient presented a total flap necrosis then he was treated with NPWT and secondary healing. Their osteomyelitis recurred within three months of primary treatment.
A significant difference in recurrence rate was found in patients with ESRD and those without ESRD (p = 0.011, OR = 16.5). PAOD and diabetic foot ulcers had no correlation with flap survival as well as recurrence rate. Similarly, other factors had no significant correlation with the outcomes. Although the association was not significant, there was a tendency of reducing recurrence in patients treated using antibiotic beads and NPWT (OR = 0.439 and 0.769, respectively) (Table 2).
Discussion
Although the diagnosis and treatment of osteomyelitis has improved, it remains a significant challenge to physicians. Management of osteomyelitis involves using antibiotics, radical debridement, and reconstruction with well-vascularized tissue. Several studies reported the efficacy of using free tissue transfer in the treatment of chronic osteomyelitis [5,6,7,8,9,10]. Free flaps regardless of the composition provide reliable tissues not only to cover large defects but also to obliterate dead space, without further compromising local tissue [2, 11]. In this study, the authors aimed to evaluate the influence of co-morbidities and other factors such as diabetic foot ulcers, flap types, using antibiotic beads and NPWT on the outcome of osteomyelitis treated with free flaps. The only factor that had a significant correlation with recurrence rate was ESRD. Patients with ESRD had 16.5 times higher odds of OM recurrence (p = 0.011). Renal failure has been known to impair wound healing in several ways [12, 13]. Additionally, it has been considered as a risk factor for free flap failure and limb amputation [14,15,16]. Therefore, caution must be taken when treating OM in patients with ESRD and free flaps should be carefully monitored post-operation.
PAOD is closely related to diabetes and smoking. Atherosclerotic changes decrease blood supply to the distal parts of the extremities. Consequently, it compromises the wound healing process and increases the rate of flap failure. Lee et al. reported a high rate of flap loss when they performed a combination of revascularization and free flap for severe PAOD patients [16]. Similarly, Oh et al. reported 10.212 times higher odds of flap failure in PAOD patients [17]. Nevertheless, our previous study showed the safe utilization of free flaps in PAOD patients following a successful angioplasty, particularly in cases where angioplasty achieved the complete revascularization of the pedal arch [18]. Similarly, in this study, all 21 patients with severely stenotic arteries underwent angioplasty before flap surgery, and complete flap necrosis was only seen in two cases. We believe that maximizing the blood flow by arterial intervention played a critical role in the reconstruction of ischemic wounds of the lower extremities.
Osteomyelitis following diabetic foot ulcers is a critical condition associated with complications and a high rate of lower limb amputation [19]. Choosing conservative or surgical treatment for diabetic foot osteomyelitis has been debated for years; however, the management of diabetic foot osteomyelitis still varies from center to center [1, 20,21,22]. In our institute, we believe that the combination of surgical and medical treatment would provide the better result. Although radical debridement often results in a large defect, this defect is frequently able to obliterate by the free flap transfer. With this in mind, the surgeon can completely resect the infected and unviable tissue including skin, soft tissue, and bone without any hesitation. The result of our study showed no statistically significant difference of the outcomes between the group with diabetic foot ulcer and those with non-diabetic foot ulcer. Other studies also revealed similar results with a relatively high rate of limb salvage, which was very encouraging for the treatment of osteomyelitis secondary to a diabetic foot [17, 23].
Besides the typical treatment modalities, adjuvant therapies including antibiotic beads and NPWT have been proven effective in the management of OM [24,25,26]. Data analysis revealed that there was a tendency of reduced recurrence in patients who used antibiotic beads and NPWT. However, it was not statistically significant.
This study has several limitations since it was a single-center, retrospective, non-randomized study with a small sample size. Additionally, the small number of patients who underwent major amputation (two patients) was the reason we could not perform statistical analysis in this group. However, it revealed a high rate of limb salvage (96.9%) comparable to other studies. The relatively short duration of follow-up was the other limitation, as osteomyelitis can recur several years after treatment. Hence, further investigation should be continued in these patients. Despite these limitations, we believe that this study showed the efficacy of free flaps in the treatment of osteomyelitis and limb salvage even in patients with co-morbidities.
Conclusion
This study found patients with ESRD had a higher rate of recurrence of osteomyelitis after treatment. The other factors had no significant correlation with the outcomes. Free flap coverage for OM patients is a reliable approach to achieve successful remission and limb salvage. The keystones of treatment are to eradicate infections, cover wounds with well-vascularized tissue and simultaneously control comorbid conditions. Besides, maximizing the distal blood supply of the lower extremity essentially contributes to enhancing the success rate of the treatment, especially in patients with severe PAOD.
Availability of data and materials
Please contact the corresponding author for data request.
Abbreviations
- OM:
-
Osteomyelitis
- PAOD:
-
Peripheral arterial occlusive disease
- ESRD:
-
End-stage renal disease
- NPWT:
-
Negative pressure wound therapy
- ALT:
-
Anterolateral thigh
References
Game FL. Osteomyelitis in the diabetic foot: diagnosis and management. Med Clin North Am. 2013;97(5):947–56. https://doi.org/10.1016/j.mcna.2013.03.010.
Musharafieh R, Osmani O, Musharafieh U, Saghieh S, Atiyeh B. Efficacy of microsurgical free-tissue transfer in chronic osteomyelitis of the leg and foot: review of 22 cases. J Reconstr Microsurg. 1999;15(4):239–44. https://doi.org/10.1055/s-2007-1000097.
Kendall JV, McNally M, Taylor C, Ferguson J, Galitzine S, Critchley P, et al. The Effect of Age on Outcome in Excision of Chronic Osteomyelitis with Free Muscle Flap Reconstruction. J Bone Jt Infect. 2019;4(4):181–8. https://doi.org/10.7150/jbji.31764.
Yazar S, Lin CH, Lin YT, Ulusal AE, Wei FC. Outcome comparison between free muscle and free fasciocutaneous flaps for reconstruction of distal third and ankle traumatic open tibial fractures. Plast Reconstr Surg. 2006;117(7):2468–75; discussion 76-7. https://doi.org/10.1097/01.prs.0000224304.56885.c2.
Zweifel-Schlatter M, Haug M, Schaefer DJ, Wolfinger E, Ochsner P, Pierer G. Free fasciocutaneous flaps in the treatment of chronic osteomyelitis of the tibia: a retrospective study. J Reconstr Microsurg. 2006;22(1):41–7. https://doi.org/10.1055/s-2006-931906.
Sofiadellis F, Liu DS, Webb A, Macgill K, Rozen WM, Ashton MW. Fasciocutaneous free flaps are more reliable than muscle free flaps in lower limb trauma reconstruction: experience in a single trauma center. J Reconstr Microsurg. 2012;28(5):333–40. https://doi.org/10.1055/s-0032-1313764.
Suh HP, Hong JP. The role of reconstructive microsurgery in treating lower-extremity chronic wounds. Int Wound J. 2019;16(4):951–9. https://doi.org/10.1111/iwj.13127.
Hong JPJ, Goh TLH, Choi DH, Kim JJ, Suh HS. The Efficacy of Perforator Flaps in the Treatment of Chronic Osteomyelitis. Plast Reconstr Surg. 2017;140(1):179–88. https://doi.org/10.1097/PRS.0000000000003460.
Salgado CJ, Mardini S, Jamali AA, Ortiz J, Gonzales R, Chen HC. Muscle versus nonmuscle flaps in the reconstruction of chronic osteomyelitis defects. Plast Reconstr Surg. 2006;118(6):1401–11. https://doi.org/10.1097/01.prs.0000239579.37760.92.
Kovar A, Colakoglu S, Iorio ML. Choosing between Muscle and Fasciocutaneous Free Flap Reconstruction in the Treatment of Lower Extremity Osteomyelitis: Available Evidence for a Function-Specific Approach. J Reconstr Microsurg. 2020;36(3):197–203. https://doi.org/10.1055/s-0039-1698469.
Buono P, Castus P, Dubois-Ferriere V, Ruegg EM, Uckay I, Assal M, et al. Muscular Versus Non-Muscular Free Flaps for Soft Tissue Coverage of Chronic Tibial Osteomyelitis. World J Plast Surg. 2018;7(3):294–300. https://doi.org/10.29252/wjps.7.3.294.
Maroz N, Simman R. Wound Healing in Patients With Impaired Kidney Function. J Am Coll Clin Wound Spec. 2013;5(1):2–7. https://doi.org/10.1016/j.jccw.2014.05.002.
Beyene RT, Derryberry SL Jr, Barbul A. The Effect of Comorbidities on Wound Healing. Surg Clin North Am. 2020;100(4):695–705. https://doi.org/10.1016/j.suc.2020.05.002.
Moran SL, Illig KA, Green RM, Serletti JM. Free-tissue transfer in patients with peripheral vascular disease: a 10-year experience. Plast Reconstr Surg. 2002;109(3):999–1006. https://doi.org/10.1097/00006534-200203000-00031.
Attinger CE, Ducic I, Neville RF, Abbruzzese MR, Gomes M, Sidawy AN. The relative roles of aggressive wound care versus revascularization in salvage of the threatened lower extremity in the renal failure diabetic patient. Plast Reconstr Surg. 2002;109(4):1281–90; discussion 91-2. https://doi.org/10.1097/00006534-200204010-00011.
Lee YK, Park KY, Koo YT, Baek RM, Heo CY, Eun SC, et al. Analysis of multiple risk factors affecting the result of free flap transfer for necrotising soft tissue defects of the lower extremities in patients with type 2 diabetes mellitus. J Plast Reconstr Aesthet Surg. 2014;67(5):624–8. https://doi.org/10.1016/j.bjps.2014.01.047.
Oh TS, Lee HS, Hong JP. Diabetic foot reconstruction using free flaps increases 5-year-survival rate. J Plast Reconstr Aesthet Surg. 2013;66(2):243–50. https://doi.org/10.1016/j.bjps.2012.09.024.
Thai DQ, Lee DH, Lee WB, Hahn HM, Lee IJ. What is the impact of infrapopliteal endovascular intervention on free flap survival in diabetic foot reconstruction? J Orthop Surg Res. 2021;16(1):42. https://doi.org/10.1186/s13018-020-02173-9.
Lipsky BA, Berendt AR, Deery HG, Embil JM, Joseph WS, Karchmer AW, et al. Diagnosis and treatment of diabetic foot infections. Plast Reconstr Surg. 2006;117(7 Suppl):212S–38S. https://doi.org/10.1097/01.prs.0000222737.09322.77.
Lázaro-Martínez JL, Tardáguila-García A, García-Klepzig JL. Diagnostic and therapeutic update on diabetic foot osteomyelitis. Endocrinol Diabetes Nutr (English ed). 2017;64(2):100–8.
Giurato L, Meloni M, Izzo V, Uccioli L. Osteomyelitis in diabetic foot: A comprehensive overview. World J Diabetes. 2017;8(4):135–42. https://doi.org/10.4239/wjd.v8.i4.135.
Aragon-Sanchez FJ, Cabrera-Galvan JJ, Quintana-Marrero Y, Hernandez-Herrero MJ, Lazaro-Martinez JL, Garcia-Morales E, et al. Outcomes of surgical treatment of diabetic foot osteomyelitis: a series of 185 patients with histopathological confirmation of bone involvement. Diabetologia. 2008;51(11):1962–70. https://doi.org/10.1007/s00125-008-1131-8.
Schirmer S, Ritter RG, Fansa H. Vascular surgery, microsurgery and supramicrosurgery for treatment of chronic diabetic foot ulcers to prevent amputations. PLoS One. 2013;8(9):e74704. https://doi.org/10.1371/journal.pone.0074704.
Kim BS, Choi WJ, Baek MK, Kim YS, Lee JW. Limb salvage in severe diabetic foot infection. Foot Ankle Int. 2011;32(1):31–7. https://doi.org/10.3113/FAI.2011.0031.
Sun PQ, Ma Y, Zhang YC, Cheng MG. Application of antibiotic impregnated beads on the patients with tibial chronic osteomyelitis. Pak J Pharm Sci. 2018;31(6(Special)):2783–6.
Stengel D, Bauwens K, Sehouli J, Ekkernkamp A, Porzsolt F. Systematic review and meta-analysis of antibiotic therapy for bone and joint infections. Lancet Infect Dis. 2001;1(3):175–88. https://doi.org/10.1016/S1473-3099(01)00094-9.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conception and design: IJL. Data collection: DQT, YKJ. Analysis and interpretation: DQT, HMH, YKJ. Writing article: DQT. Critical revision of the article: HMH, IJL. Final approval of the article: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Ajou Medical Center (AJIRB-MED-MDB-16-402).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Thai, D.Q., Jung, Y.K., Hahn, H.M. et al. Factors affecting the outcome of lower extremity osteomyelitis treated with microvascular free flaps: an analysis of 65 patients. J Orthop Surg Res 16, 535 (2021). https://doi.org/10.1186/s13018-021-02686-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-021-02686-x