Abstract
Background
Patellar instability has a high incidence and occurs particularly in young and female patients. If the patella dislocates for the first time, treatment is usually conservative. However, this cautious approach carries the risk of recurrence and of secondary pathologies such as osteochondral fractures. Moreover, there is also risk of continuous symptoms apparent, as recurrent patella dislocation is related to patellofemoral osteoarthritis as well. An initial surgical treatment could possibly avoid these consequences of recurrent patella dislocation.
Methods
A prospective, randomized-controlled trial design is applied. Patients with unilateral first-time patella dislocation will be considered for participation. Study participants will be randomized to either conservative treatment or to a tailored patella stabilizing treatment. In the conservative group, patients will use a knee brace and will be prescribed outpatient physical therapy. The surgical treatment will be performed in a tailored manner, addressing the pathologic anatomy that predisposes to patella dislocation.
The Banff Patellofemoral Instability-Instrument 2.0, recurrence rate, apprehension test, joint degeneration, and the Patella Instability Severity Score will serve as outcome parameters. The main analysis will focus on the difference in change of the scores between the two groups within a 2-year follow-up.
Statistical analysis will use linear mixed models. Power analysis was done for the comparison of the two study arms at 2-year follow-up with regard to the BPII Score. A sample size of N = 64 per study arm (128 overall) provides 80% power (alpha = 0.05, two-tailed) to detect a difference of 0.5 standard deviations in a t-test for independent samples.
Discussion
Although several studies have already dealt with this issue, there is still no consensus on the ideal treatment concept for primary patellar dislocation. Moreover, most of these studies show a unified surgical group, which means that all patients were treated with the same surgical procedure. This is regarded as a major limitation as surgical treatment of patella dislocation should depend on the patient’s anatomic pathologies leading to patellar instability. To our knowledge, this is the first study investigating whether patients with primary patella dislocation are better treated conservatively or operatively with tailored surgery to stabilize the patella.
Trial registration
The study will be prospectively registered in the publicly accessible database www.ClinicalTrials.gov.
Similar content being viewed by others
Introduction
Instability of the patella has a high incidence, particularly in the young and female population. Because the vast majority of unstable patella are unstable towards lateral and because instability is objective when the patella is fully dislocated the term “lateral patella dislocation (LPD)” is used throughout this study protocol.
First time or primary LPD is often treated conservatively. Although this is a cautious approach, it bears risks of recurrence and secondary pathologies like osteochondral fractures or patellofemoral osteoarthritis [1, 2]. Therefore, it might well be speculated whether primary LPD should better be treated surgically, not only for short time clinical improvement, but also for prevention of PF osteoarthritis. With this regard, several researchers already dealt with that issue. Table 1 gives an overview on current evidence on conservative vs. surgical treatment of patients with first-time lateral patella dislocation. However, only studies with level of evidence 1 or 2 were taken into account.
Apostolovic et al. performed a prospective, non-randomized-controlled trial comparing 23 conservatively treated patients with 14 surgically treated patients in the context of primary LPD [3]. The criterion to treat surgically was the presence of (osteo)chondral lesions. Besides loose body removal/refixation, the patients received medial capsular repair and lateral retinacular release. The authors reported no differences between groups regarding recurrence rate or Cincinnati Knee scores, which goes along with the findings of Christiansen et al. [4]. Eighty patients with primary LPD were randomized to either conservative therapy or medial patellofemoral ligament (MPFL) repair. Patients were followed 2 years and demonstrated no significant differences between groups with regard to recurrence rate, KOOS Score, and Kujala Score.
However, there are considerable studies describing benefits of an initial surgical procedure. Bitar et al. conducted a randomized-controlled trial on primary LPD [5]. Thirty-nine patients were randomized to either non-operative treatment (immobilization and physical therapy) or reconstruction of the MPFL. At 2-year follow-up, the MPFL group was superior in terms of Kujala scores and recurrence rates. Camanho et al. also investigated patients with primary LPD [6]. Thirty-three patients were randomly assigned to either conservative treatment (immobilization and physiotherapy) or MPFL repair. The authors reported superior results in the surgical group. Two studies very similar to each other were published by Sillanpää et al. in 2008 and 2009 [7, 8]. The outcome parameters recurrence rates, Kujala scores and “return to sports – rate” were determined in patients with conservative treatment and in those with surgery. While the surgical group was superior in terms of “return-to-sports” there were no significant differences in the other outcome parameters [7]. In contrast, Sillanpää et al. stated in the following randomized-controlled study that patients treated surgically were superior in terms of recurrence rate but not in the other parameters [8]. Finally, a randomized-controlled trial published by Petri et al. should be mentioned [9]. In a multicentric approach, patients with primary LPD were randomized to either conservative treatment or MPFL repair. Unfortunately, the trial was discontinued after 20 patients and did therefore not reach sufficient power.
In synopsis of the abovementioned studies, there is no consensus on whether patients with first time LPD should be treated conservatively or surgically (Table 1). Besides, in most of those studies the surgically group was uniform, meaning that all patients were treated with the same surgical procedure. In addition, previous studies have focused more on the rate of re-dislocation and were not based upon modern and relevant PROM scores. Treatment with the same surgical procedure is regarded as a major limitation as surgical treatment of LPD should be done in a tailored manner, depending on the patient’s anatomic pathologies which lead to LPD [10, 11]:
MPFL reconstruction
Reconstruction of the medial patellofemoral ligament (MPFL) is a proven technique for LPD [10,11,12] and today’s established standard treatment. However, some authors have reported a considerable complication rate [13, 14]. Many failures were reported due to inappropriate indications. The latter means performing isolated MPFL in patients with coexisting severe osseous pathologies like high-grade trochlear dysplasia or a pathologic tuberositas-tibiae-trochlea-groove distance (TT-TG distance) [15, 16]. Isolated MPFL reconstruction is regarded as inappropriate in patients with: (1) TT-TG distance > 20 mm, (2) femoral anteversion ≥ 40° (n. Waidelich/Strecker), (3) high-grade trochlea dysplasia, (4) severe patella alta, and (5) tibiofemoral valgus > 5°. Moreover, it is striking that most abovementioned studies applied MPFL repair. Only Bitar et al. performed MPFL reconstruction [5]. With accurate indications and surgical technique isolated MPFL reconstruction provides a good outcome in patients with LPD [17, 18].
Trochleoplasty
When the trochlea is flat or convex (dysplasia Dejour type B, C or D) a “deepening trochleoplasty” should be considered. The aim of the trochleoplasty is to (a) reduce the too prominent anterior bone stock, (b) create better conformity with the patella (concave groove) and a lateral trochlea facet as restraint against the lateralizing quadriceps pull, and (c) to lateralize the groove when there is trochlea asymmetry in order to normalize TT-TG distance [19, 20]. Many authors have reported that trochleoplasty leads to a good clinical outcome in patients’ LPD due to a dysplastic femoral trochlea [12, 19, 21,22,23,24,25,26,27].
Tibial tuberosity transfer
The most popular type of osteotomy in the setting of LPD is certainly the osteotomy and transfer of the tibial tuberosity (TTT). Many articles reported good clinical success for medialising TTT in patients with LPD and high TT-TG values [12, 28,29,30,31,32]. Similarly, good results were found for distalizing TTT in patients with LPD and patella alta [33, 34]. TTT can be tailored to the pathology of the patient by performing combined medialization and distalization.
Derotational osteotomy
Derotational osteotomies of the femur (externally rotating) provide good results in patients with LPD and associated torsional deformities [35,36,37]. However, the literature is incongruent on whether rotational osteotomies of the femur should be performed at the proximal or distal aspect [38,39,40,41]. In the authors hand’s, derotational osteotomy is carried out at the distal femur.
Varus osteotomy
Distal femoral varus osteotomies have been described in the recent years to be successful in the management of patellofemoral instability with genu valgum [42]. They have been described as promising and useful in the management of patellofemoral instability with genu valgum, leading to an improved patellar alignment and to a reduction in the risk of recurrent patella dislocation [42, 43].
Aims of the study
Due to the abovementioned lack of consistent evidence, it is the aim of the study to investigate whether patients with primary LPD are better treated conservatively or operatively (tailored surgery to stabilize the patella).
Hypotheses
It is hypothesized that patients with primary LPD when treated either conservatively or surgically (tailored stabilizing procedure) will show significant differences after two years in terms of the Banff Patellofemoral Instability-Instrument (BPII) 2.0 (hypothesis 1). We assume as well that the abovementioned groups also differ significantly in terms of recurrent patella dislocations (hypothesis 2).
Methods
Study design and participants
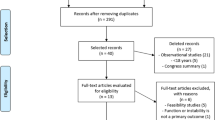
A prospective, randomized-controlled trial design is applied. Before commencement of the study, approval of the ethical committees (EC) of the participating centers is obtained. Patients with objective, unilateral first time LPD, based on patient’s history and physical examination, will be considered for participation. After written informed consent the patients are included in the study at their first visit at the emergency department. Excluded are (a) patients with osteochondral lesions requiring removal/refixation, (b) patients with recurrent LPD, (c) pregnant patients, and (d) patients > 45 years of age and patients with physical maturity Kramer stage 1 to stage 3a [44, 45].
Clinical workup includes thorough history, physical evaluation, plain radiographs, and magnetic resonance imaging (MRI) in all patients. When the physical examination reveals suspicion of maltorsion syndrome, MRI (or CT scan) is done of the hip, knee, and ankle to quantify femoral and tibial torsion. When the physical examination reveals suspicion of a relevant genu valgum or varum a long-standing x-ray is performed.
Randomization
Patients successfully included in the study are then randomized to either conservative treatment or to a tailored patella stabilizing treatment. Block randomization will be used to ensure a balanced ratio of group sizes. The total number of patients will be divided into blocks of the same size. This will be followed by a balanced but random allocation of the treatment groups in the individual blocks. Patients will be divided into 10 blocks of 16 patients each and will be assigned to the two different treatment groups.
Block randomization is performed in advance with SPSS (IBM SPSS statistics, Chicago, IL, USA) to guarantee equal group sizes. Syntax and seed for the random number generator are kept for reproducibility of the processes.
Documentation
The investigator records the participation on a special identification list of patients. This list gives the possibility for a later identification of the patients and contains the patient number, full name, date of birth, and the date of the enrolment into the study. The identification list of patients remains in the study center after the closure of the study. It is the responsibility of the investigator to document all data of the clinical study correctly and completely into the database. Important harms or unintended effects will be recorded in each group.
Dropouts and exclusion of the clinical trial
To account for 20% attrition during the study period (“dropouts”), it is planned to recruit 80 patients per study group (160 overall) at baseline (see section “Statistics”). If patients request after randomization on their own free will a different treatment method — for example, if a patient requests surgery in conservative group — they have to be excluded from the study.
Interventions
In both groups, in case of relevant hemarthrosis and danger of skin or soft tissue exposure, a joint aspiration is performed [46].
Conservative group
In the conservative group, patients use a motion-restricting knee brace that (a) protects the patella from lateralization and (b) limits knee range of motion. The range of motion limitation is set to 0-20-40° for week 1-2, 0-10-60° for week 3–4, and 0-0-90° for week 5-8. Partial weight-bearing is applied for week 1 and 2. Patients are prescribed outpatient physical therapy following a protocol suggested earlier by the “Patellofemoral Committee of the German-Speaking Arthroscopy Society (AGA)” [46]:
-
Phase 1 (week 1 + 2). Range of motion 0-20-40°, partial weight-bearing
-
Phase 2 (week 3 + 4). Range of motion 0-10-60°, progression to full weight-bearing, emphasis on quadriceps recruitment (especially vastus medialis)
-
Phase 3 (week 5–8). Range of motion 0-0-90°, re-acquiring activities of daily living, core stability, sensorimotor training (leg axes stabilization), strength training
-
Phase 4. Return to sports, dependent on the type and previous level of sports activity, gradual increase of training volume and intensity
Surgical group
The surgical treatment is performed in a tailored manner, addressing the respecting pathologic anatomy that predisposes to LPD. MPFL reconstruction is performed in every patient. Other surgical techniques listed below will be applied in individual combinations, dependent on patient’s needs.
MPFL reconstruction
MPFL reconstruction is applied in all patients of the surgical group
MPFL reconstructionhas been reported with a high variety of surgical techniques (graft type, single vs. double bundle, type of fixation, etc.). The specific surgical technique is carried out on surgeon’s preference at the respective center of the multicentric study.
Trochleoplasty
Deepening trochleoplasty will be carried out in those patients of the surgical group who suffer from high-grade trochlea dysplasia.
Tibial tuberosity transfer
Medializing TTT will be applied to those patients with TT-TG distances ≥ 18 mm in the MRI. Distalizing TTT will be applied in patients with Caton-Deschamps Index > 1.2 [47].
Derotational osteotomy
In those patients with femoral antetorsion ≥ 40° (n. Waidelich/Strecker), a distal femoral derotational osteotomy is carried out. The precise surgical technique for that procedure is given over to the surgeon of the respective center.
Varus osteotomy
In patients with valgus clinical appearance, a weight-bearing long-standing x-ray should be performed to precisely assess the degree of the deformity in the frontal plane (mechanical femorotibial angle).
In cases with a mechanical femorotibial angle > 5°, a varus osteotomy is performed at the location of the deformity.
Applying a “pragmatic” surgical approach, not each single pathology in the patient’s anatomy is addressed. Instead, a maximum of 3 surgical techniques (including the MPFL reconstruction) are performed in one patient. This means, that the 3 leading pathologies are surgically addressed, even in the rare case that 4 or more surgical techniques could be considered. In this sense, lateral release or lateral lengthening and arthroscopy are — for this protocol — not counted as distinct techniques.
Outcome parameters
Patient-reported outcome
The Banff Patellofemoral Instability-Instrument (BPII) 2.0 was reported as valid, reliable, and responsive patient-reported outcome tool in the field of patellofemoral instability [48, 49] and is used in the validated German version [50]. The BPII 2.0 serves as one of two major outcome instruments (hypothesis 1).
For exploratory reasons, the following further patient-reported parameters will be assessed in both groups: As second disease specific score, patients accomplish the Kujala Score [51] which was quoted as a reliable, valid, and responsive tool for patellofemoral disorders [52, 53]. In addition, the Short-Form 12 is used (version 2, German; SF-12v2) [54] to determine the general health outcome and the Marx activity scale to rate a patient’s physical activity [55]. The Marx Score asks for the highest activity in the last year. For postoperative monitoring of a patient’s activity, a “modified version of the Marx Score” will be used that refers to the last 2 months.
All abovementioned outcome scores are self-administered and will be assessed preoperatively, 6 and 12 months postoperatively, and then yearly. Those scores are collected during routine visits at the hospital. Alternatively, the questionnaires for assessment of the outcome scores can be filled out online by the patients to reduce dropouts.
The follow-up period is planned for 2 years. However, with the patient’s consent, the period can also be prolonged.
Other outcome parameters
Recurrence rate is assessed as second major outcome parameter (hypothesis 2). To keep proper medical records on recurrent patella dislocations, the patients are interviewed by telephone on a monthly basis (in addition to the abovementioned visits at the hospital).
The apprehension test is assessed by an experienced observer during the abovementioned routine clinical visits (grade 0, no evasion; grade 1, slight evasion/avoidance; grade 2, gross evasion/avoidance; grade 3, patient too anxious to allow the test).
Joint degeneration is assessed preoperatively and every three years postoperatively by means of MRI (PD-FSE with fat-sat high-resolution in all three planes/T1-TSE, sagittal/T2 weighted, isotrope 3D sequence sagittal reformatted in all three planes). The semi-quantitative MRI Osteoarthritis Knee Score (MOAKS scoring) is applied to rate the degenerative changes determined by MRI [56]. The MOAKS scoring is determined by always the same experienced musculoskeletal radiologist. Additionally, TT-TG distance is measured on postoperative MRI.
In addition, the Patella Instability Severity Score is assessed for exploratory reasons [57].
Statistics
Patient characteristics will be presented as means, standard deviations, and percentages. The main analysis will use linear mixed models that allow data modeling with a varying number of assessments per patient and time-varying covariates. Such a model will be used to compare the differences in changes over time between the two study groups. The following terms will be included in the model: a random baseline, a first-order autocorrelation covariance matrix, a fixed-effect patient group, a fixed effect time point, and the group-by-time interaction (reflecting the intervention effect). The BPII 2.0 will serve as the primary outcome parameters. The main analysis is “intention to treat” and will focus on the group difference in the change of BPII 2.0 scores between pre-op and 2-year follow-up. The abovementioned secondary outcome parameters will be analyzed with the same model.
Power/sample size analysis was done for the comparison of the two study arms at a 2-year follow-up with regard to the BPII Score. As there are no specific minimal important difference (MID) for the BPII available from the literature, we defined the MID to be 0.5 standard deviations following general recommendations from the literature [58]. A sample size of N = 64 per study arm (128 overall) provides 80% power (alpha = 0.05, two-tailed) to detect a difference of 0.5 standard deviations in a t-test for independent samples. To account for 20% attrition during the study period (“dropouts”), we plan to recruit 80 patients per study group (160 overall) at baseline.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 3D:
-
Three-dimensional
- AGA:
-
Gesellschaft für Arthroskopie und Gelenkchirurgie
- BPII:
-
Banff Patellofemoral Instability-Instrument
- CT:
-
Computer tomography
- EC:
-
Ethics committee
- ICF:
-
Informed consent form
- LPD:
-
Lateral patella dislocation
- MID:
-
Minimal important difference
- MOAK scoring:
-
MRI Osteoarthritis Knee Score
- MPFL:
-
Medial patellofemoral ligament
- MRI:
-
Magnetic resonance imaging
- N:
-
Sample size
- PD-FSE:
-
Proton density-fast spin echo
- PF:
-
Patellofemoral
- PROM:
-
Patient-reported Outcome Measures
- SF-12v2:
-
Short-Form 12 version 2
- TSE:
-
Turbo spin echo
- TTT:
-
Transfer of the tibial tuberosity
- TT-TG distance:
-
Tuberositas-tibiae-trochlea-groove distance
References
Conchie H, Clark D, Metcalfe A, Eldridge J, Whitehouse M. Adolescent knee pain and patellar dislocations are associated with patellofemoral osteoarthritis in adulthood: a case control study. Knee. 2016;23(4):708–11 Available from: https://pubmed.ncbi.nlm.nih.gov/27180253/. [cited 2021 May 7].
Salonen EE, Magga T, Sillanpää PJ, Kiekara T, Mäenpää H, Mattila VM. Traumatic patellar dislocation and cartilage injury: a follow-up study of long-term cartilage deterioration. Am J Sports Med. 2017;45(6):1376–82 Available from: https://pubmed.ncbi.nlm.nih.gov/28298062/. [cited 2021 May 7].
Apostolovic M, Vukomanovic B, Slavkovic N, Vuckovic V, Vukcevic M, Djuricic G, et al. Acute patellar dislocation in adolescents: operative versus nonoperative treatment. Int Orthop. 2011;35(10):1483–7 Available from: https://pubmed.ncbi.nlm.nih.gov/21574051/. [cited 2020 Oct 5].
Christiansen SE, Jakobsen BW, Lund B, Lind M. Isolated repair of the medial patellofemoral ligament in primary fislocation of the patella: a prospective randomized study. Arthrosc - J Arthrosc Relat Surg. 2008;24(8):881–7 Available from: https://pubmed.ncbi.nlm.nih.gov/18657736/. [cited 2020 Oct 5].
Bitar AC, Demange MK, D’Elia CO, Camanho GL. Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med. 2012;40(1):114–22 Available from: https://pubmed.ncbi.nlm.nih.gov/22016458/. [cited 2020 Oct 5].
Camanho GL, Viegas A d C, Bitar AC, Demange MK, Hernandez AJ. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthrosc - J Arthrosc Relat Surg. 2009;25(6):620–5 Available from: https://pubmed.ncbi.nlm.nih.gov/19501292/. [cited 2020 Oct 5].
Sillanpää PJ, Mäenpää HM, Mattila VM, Visuri T, Pihlajamäki H. Arthroscopic surgery for primary traumatic patellar dislocation: a prospective, nonrandomized study comparing patients treated with and without acute arthroscopic stabilization with a median 7-year follow-up. Am J Sports Med. 2008;36(12):2301–9 Available from: https://pubmed.ncbi.nlm.nih.gov/18762668/. [cited 2020 Oct 5].
Sillanpää PJ, Mattila VM, Mäenpää H, Kiuru M, Visuri T, Pihlajamäki H. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation: a prospective randomized study. J Bone Jt Surg - Ser A. 2009;91(2):263–73 Available from: https://pubmed.ncbi.nlm.nih.gov/19181969/. [cited 2020 Oct 5].
Petri M, Liodakis E, Hofmeister M, Despang FJ, Maier M, Balcarek P, et al. Operative vs conservative treatment of traumatic patellar dislocation: results of a prospective randomized controlled clinical trial. Arch Orthop Trauma Surg. 2013;133(2):209–13 Available from: https://pubmed.ncbi.nlm.nih.gov/23138693/. [cited 2020 Oct 5].
Migliorini F, Oliva F, Maffulli GD, Eschweiler J, Knobe M, Tingart M, et al. Isolated medial patellofemoral ligament reconstruction for recurrent patellofemoral instability: analysis of outcomes and risk factors [Internet]. J Orthop Surg Res. 2021;16 Available from: https://pubmed.ncbi.nlm.nih.gov/33823887/. [cited 2021 May 7].
Ronga M, Oliva F, Longo UG, Testa V, Capasso G, Maffulli N. Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2009;37(9):1735–42 Available from: https://pubmed.ncbi.nlm.nih.gov/19470945/. [cited 2021 May 7].
Vetrano M, Oliva F, Bisicchia S, Bossa M, De Carli A, Di Lorenzo L, et al. I.S.Mu.L.T. First-time patellar dislocation guidelines [Internet]. Muscles Ligaments Tendons J. 2017;7:1–10 Available from: https://pubmed.ncbi.nlm.nih.gov/28717605/. [cited 2021 May 7].
Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation [Internet]. Am J Sports Med. 2012;40:1916–23 Available from: http://journals.sagepub.com/doi/10.1177/0363546512442330. [cited 2020 Oct 5].
Feucht MJ, Mehl J, Forkel P, Achtnich A, Schmitt A, Izadpanah K, et al. Failure analysis in patients with patellar redislocation after primary isolated medial patellofemoral ligament reconstruction. Orthop J Sport Med. 2020;8(6) Available from: https://pubmed.ncbi.nlm.nih.gov/32613021/. [cited 2021 May 7].
Hopper GP, Leach WJ, Rooney BP, Walker CR, Blyth MJ. Does degree of trochlear dysplasia and position of femoral tunnel influence outcome after medial patellofemoral ligament reconstruction? Am J Sports Med. 2014;42(3):716–22 Available from: https://pubmed.ncbi.nlm.nih.gov/24458241/. [cited 2020 Oct 5].
Wagner D, Pfalzer F, Hingelbaum S, Huth J, Mauch F, Bauer G. The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sport Traumatol Arthrosc. 2013;21(2):318–24 Available from: https://pubmed.ncbi.nlm.nih.gov/22538501/. [cited 2020 Oct 5].
Mackay ND, Smith NA, Parsons N, Spalding T, Thompson P, Sprowson AP. Medial patellofemoral ligament reconstruction for patellar dislocation: a systematic review. Orthop J Sport Med. 2014;2(8) Available from: https://pubmed.ncbi.nlm.nih.gov/26535352/. [cited 2020 Oct 5].
Stupay KL, Swart E, Shubin Stein BE. Widespread implementation of medial patellofemoral ligament reconstruction for recurrent patellar instability maintains functional outcomes at midterm to long-term follow-up while decreasing complication rates: a systematic review [Internet]. Arthrosc J Arthrosc Relat Surg. 2015;31:1372–80 Available from: https://pubmed.ncbi.nlm.nih.gov/25703288/. [cited 2020 Oct 5].
Ntagiopoulos PG, Byn P, Dejour D. Midterm results of comprehensive surgical reconstruction including sulcus-deepening trochleoplasty in recurrent patellar dislocations with high-grade trochlear dysplasia. Am J Sports Med. 2013;41(5):998–1004 Available from: https://pubmed.ncbi.nlm.nih.gov/23589587/. [cited 2020 Oct 5].
Paiva M, Blønd L, Hölmich P, Barfod KW. Effect of medialization of the trochlear groove and lateralization of the tibial tubercle on TT-TG distance: a cross-sectional study of dysplastic and nondysplastic knees. Am J Sports Med. 2021;49(4):970–4 Available from: https://pubmed.ncbi.nlm.nih.gov/33595335/. [cited 2021 May 7].
Neumann MV, Stalder M, Schuster AJ. Reconstructive surgery for patellofemoral joint incongruency. Knee Surg Sport Traumatol Arthrosc. 2016;24(3):873–8 Available from: https://pubmed.ncbi.nlm.nih.gov/25358690/. [cited 2020 Oct 5].
Banke IJ, Kohn LM, Meidinger G, Otto A, Hensler D, Beitzel K, et al. Combined trochleoplasty and MPFL reconstruction for treatment of chronic patellofemoral instability: a prospective minimum 2-year follow-up study. Knee Surg Sport Traumatol Arthrosc. 2014;22(11):2591–8 Available from: https://pubmed.ncbi.nlm.nih.gov/23851967/. [cited 2020 Oct 5].
Dejour D, Byn P, Ntagiopoulos PG. The Lyon’s sulcus-deepening trochleoplasty in previous unsuccessful patellofemoral surgery. Int Orthop. 2013;37(3):433–9 Available from: https://pubmed.ncbi.nlm.nih.gov/23275080/. [cited 2020 Oct 5].
Thaunat M, Bessiere C, Pujol N, Boisrenoult P, Beaufils P. Recession wedge trochleoplasty as an additional procedure in the surgical treatment of patellar instability with major trochlear dysplasia: Early results. Orthop Traumatol Surg Res. 2011;97(8):833–45 Available from: https://pubmed.ncbi.nlm.nih.gov/22112463/. [cited 2020 Oct 5].
Utting MR, Mulford JS, Eldridge JDJ. A prospective evaluation of trochleoplasty for the treatment of patellofemoral dislocation and instability. J Bone Jt Surg - Ser B. 2008;90(2):180–5 Available from: https://pubmed.ncbi.nlm.nih.gov/18256084/. [cited 2020 Oct 5].
Blønd L, Haugegaard M. Combined arthroscopic deepening trochleoplasty and reconstruction of the medial patellofemoral ligament for patients with recurrent patella dislocation and trochlear dysplasia. Knee Surg Sport Traumatol Arthrosc. 2014;22(10):2484–90 Available from: https://pubmed.ncbi.nlm.nih.gov/23370988/. [cited 2020 Oct 5].
Nelitz M, Dreyhaupt J, Lippacher S. Combined trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocations in severe trochlear dysplasia: a minimum 2-year follow-up study. Am J Sports Med. 2013;41(5):1005–12 Available from: https://pubmed.ncbi.nlm.nih.gov/23467555/. [cited 2020 Oct 5].
Longo UG, Rizzello G, Ciuffreda M, Loppini M, Baldari A, Maffulli N, et al. Elmslie-Trillat, Maquet, Fulkerson, Roux Goldthwait, and other distal realignment procedures for the management of patellar dislocation: systematic review and quantitative synthesis of the literature [Internet]. Arthrosc J Arthroscopic Relat Surg. 2016;32:929–43 Available from: https://pubmed.ncbi.nlm.nih.gov/26921127/. [cited 2020 Oct 5].
Barber FA, McGarry JE. Elmslie-Trillat procedure for the treatment of recurrent patellar instability. Arthrosc - J Arthrosc Relat Surg. 2008;24(1):77–81 Available from: https://pubmed.ncbi.nlm.nih.gov/18182206/. [cited 2020 Oct 5].
Karataglis D, Green MA, Learmonth DJA. Functional outcome following modified Elmslie-Trillat procedure. Knee. 2006;13(6):464–8 Available from: https://pubmed.ncbi.nlm.nih.gov/17011193/. [cited 2020 Oct 5].
Kumar A, Jones S, Bickerstaff DR, Smith TWD. Functional evaluation of the modified Elmslie-Trillat procedure for patello-femoral dysfunction. Knee. 2001;8(4):287–92 Available from: https://pubmed.ncbi.nlm.nih.gov/11706691/. [cited 2020 Oct 5].
Nakagawa K, Wada Y, Minamide M, Tsuchiya A, Moriya H. Deterioration of long-term clinical results after the Elmslie-Trillat procedure for dislocation of the patella. J Bone Jt Surg - Ser B. 2002;84(6):861–4 Available from: https://pubmed.ncbi.nlm.nih.gov/12211679/. [cited 2020 Oct 5].
Magnussen RA, De Simone V, Lustig S, Neyret P, Flanigan DC. Treatment of patella alta in patients with episodic patellar dislocation: a systematic review [Internet]. Knee Surg Sports Traumatol Arthrosc. 2014;22:2545–50 Available from: https://pubmed.ncbi.nlm.nih.gov/23392290/. [cited 2020 Oct 5].
Mayer C, Magnussen RA, Servien E, Demey G, Jacobi M, Neyret P, et al. Patellar tendon tenodesis in association with tibial tubercle distalization for the treatment of episodic patellar dislocation with patella alta. Am J Sports Med. 2012;40(2):346–51 Available from: https://pubmed.ncbi.nlm.nih.gov/22109545/. [cited 2020 Oct 5].
Dickschas J, Harrer J, Pfefferkorn R, Strecker W. Operative treatment of patellofemoral maltracking with torsional osteotomy. Arch Orthop Trauma Surg. 2012;132(3):289–98 Available from: https://pubmed.ncbi.nlm.nih.gov/21479863/. [cited 2020 Oct 5].
Nelitz M, Dreyhaupt J, Williams SRM, Dornacher D. Combined supracondylar femoral derotation osteotomy and patellofemoral ligament reconstruction for recurrent patellar dislocation and severe femoral anteversion syndrome: surgical technique and clinical outcome. Int Orthop. 2015;39(12):2355–62 Available from: https://pubmed.ncbi.nlm.nih.gov/26156717/. [cited 2020 Oct 5].
Strecker W, Dickschas J. Torsional osteotomy : operative treatment of patellofemoral maltracking. Oper Orthop Traumatol. 2015;27(6):505–24. https://doi.org/10.1007/s00064-015-0430-8.
Bruce WD, Stevens PM. Surgical correction of miserable malalignment syndrome. J Pediatr Orthop. 2004;24(4):392–6 Available from: https://pubmed.ncbi.nlm.nih.gov/15205621/. [cited 2020 Oct 5].
Delgado ED, Schoenecker PL, Rich MM, Capelli AM. Treatment of severe torsional malalignment syndrome. J Pediatr Orthop. 1996;16(4):484–8 Available from: https://pubmed.ncbi.nlm.nih.gov/8784702/. [cited 2020 Oct 5].
Dickschas J, Harrer J, Reuter B, Schwitulla J, Strecker W. Torsional osteotomies of the femur. J Orthop Res. 2015;33(3):318–24 Available from: https://pubmed.ncbi.nlm.nih.gov/25399673/. [cited 2020 Oct 5].
Stevens PM, Gililland JM, Anderson LA, Mickelson JB, Nielson J, Klatt JW. Success of torsional correction surgery after failed surgeries for patellofemoral pain and instability. Strateg Trauma Limb Reconstr. 2014;9(1):5–12 Available from: https://pubmed.ncbi.nlm.nih.gov/24338661/. [cited 2020 Oct 5].
Tan SHS, Hui SJ, Doshi C, Wong KL, Lim AKS, Hui JH. The outcomes of distal femoral varus osteotomy in patellofemoral instability: a systematic review and meta-analysis [Internet]. J Knee Surg. 2020;33:504–12 Available from: https://pubmed.ncbi.nlm.nih.gov/30822786/. [cited 2021 May 7].
Nha KW, Ha Y, Oh S, Nikumbha VP, Kwon SK, Shin WJ, et al. Surgical treatment with closing-wedge distal femoral osteotomy for recurrent patellar dislocation with genu valgum. Am J Sports Med. 2018;46(7):1632–40. https://doi.org/10.1177/0363546518765479.
Krämer JA, Schmidt S, Jürgens K-U, Lentschig M, Schmeling A, Vieth V. The use of magnetic resonance imaging to examine ossification of the proximal tibial epiphysis for forensic age estimation in living individuals. Forensic Sci Med Pathol [Internet]. 2014;10(3):306–13. Available from: http://link.springer.com/10.1007/s12024-014-9559-2. [cited 2020 Jun 22].
Krämer JA, Schmidt S, Jürgens KU, Lentschig M, Schmeling A, Vieth V. Forensic age estimation in living individuals using 3.0T MRI of the distal femur. Int J Legal Med. 2014;128(3):509–14 Available from: https://pubmed.ncbi.nlm.nih.gov/24504560/. [cited 2020 Jun 22].
Attal R, Becher C, Green DW, Pagenstert G, Seitlinger G, Balcarek P, et al. Die Therapie der instabilen Patella [Internet]. 2016. Available from: https://www.aga-online.ch/komitees/knie-patellafemoral/heft-ii-die-therapie-der-instabilen-patella/
Caton JH, Dejour D. Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34(2 SPECIAL ISSUE):305–9 Available from: https://pubmed.ncbi.nlm.nih.gov/20066411/. [cited 2020 Oct 5].
Hiemstra LA, Kerslake S, Lafave M, Mohtadi NG. Concurrent validation of the Banff patella instability instrument to the norwich patellar instability score and the Kujala score in patients with patellofemoral instability. Orthop J Sport Med. 2016;4(5) Available from: https://pubmed.ncbi.nlm.nih.gov/27231700/. [cited 2020 Oct 5].
Lafave MR, Hiemstra L, Kerslake S. Factor analysis and item reduction of the Banff patella instability instrument (BPII). Am J Sports Med. 2016;44(8):2081–6 Available from: https://pubmed.ncbi.nlm.nih.gov/27166290/. [cited 2020 Oct 5].
Becher C, Attal R, Balcarek P, Dirisamer F, Liebensteiner M, Pagenstert G, et al. Successful adaption of the Banff patella instability instrument (BPII) 2.0 into German. Knee Surg Sport Traumatol Arthrosc. 2018;26(9):2679–84 Available from: https://pubmed.ncbi.nlm.nih.gov/28785790/. [cited 2020 Oct 5].
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–63 Available from: https://pubmed.ncbi.nlm.nih.gov/8461073/. [cited 2020 Oct 5].
Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85(5):815–22 Available from: https://pubmed.ncbi.nlm.nih.gov/15129407/. [cited 2020 Oct 5].
Watson CJ, Propps M, Ratner J, Zeigler DL, Horton P, Smith SS. Reliability and responsiveness of the lower extremity functional scale and the anterior knee pain scale in patients with anterior knee pain. J Orthop Sports Phys Ther. 2005;35(3):136–46 Available from: https://pubmed.ncbi.nlm.nih.gov/15839307/. [cited 2020 Oct 5].
Ware JE, Kosinski M, Keller SD. A 12-Item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33 Available from: https://pubmed.ncbi.nlm.nih.gov/8628042/. [cited 2020 Oct 5].
Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–8 Available from: https://pubmed.ncbi.nlm.nih.gov/11292048/. [cited 2020 Oct 5].
Hunter DJ, Guermazi A, Lo GH, Grainger AJ, Conaghan PG, Boudreau RM, et al. Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthr Cartil. 2011;19(8):990–1002 Available from: https://pubmed.ncbi.nlm.nih.gov/21645627/. [cited 2020 Oct 5].
Balcarek P, Oberthür S, Hopfensitz S, Frosch S, Walde TA, Wachowski MM, et al. Which patellae are likely to redislocate? Knee Surg Sport Traumatol Arthrosc. 2014;22(10):2308–14 Available from: https://pubmed.ncbi.nlm.nih.gov/24005331/. [cited 2020 Oct 5].
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life. Med Care. 2003;41(5):582–92 Available from: https://pubmed.ncbi.nlm.nih.gov/12719681/. [cited 2020 Oct 5].
Acknowledgements
Not applicable.
Funding
Article-processing charges are funded by the AGA — Gesellschaft für Arthroskopie und Gelenkchirurgie, Seefeldstrasse 123, 8034 Zurich, Switzerland.
Author information
Authors and Affiliations
Contributions
All authors were involved in the drafting of the study protocol. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Prior to study start, the study protocol and/or other appropriate documents were submitted to the ethics committee for approval. The study protocol was approved by the local ethics committee of the Medical University of Innsbruck (No. 1062/2020).
Every patient has to give his/her written consent before participation in the clinical trial.
The content of the consent information is documented on the patient information/informed consent form (ICF). The patient will be notified, if essential findings appear during the study.
Consent for publication
For any individual person’s data in any form (including any individual details, images or videos), consent for publication must be obtained from that person, or in the case of children, their parent or legal guardian.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liebensteiner, M., Keiler, A., El Attal, R. et al. Conservative versus tailored surgical treatment in patients with first time lateral patella dislocation: a randomized-controlled trial. J Orthop Surg Res 16, 378 (2021). https://doi.org/10.1186/s13018-021-02513-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-021-02513-3