Abstract
Objective
We aimed to evaluate reliability, radiological outcomes, and the impacts of anterior cervical hybrid construction on the adjacent segments for the multilevel cervical degenerative disc disease (mCDDD) and spondylotic spinal stenosis (SSS).
Methods
A retrospective analysis was performed using data extracted from the medical files of 195 patients (105 males, 90 females; mean age: 47.7 years). From 2008 to 2018, these patients underwent anterior cervical hybrid construction for symptomatic contiguous at least 2-level cervical degenerative disc diseases and cervical spondylosis. Clinical and radiological data including Neck Disability Index (NDI), visual analogue scale (VAS), local cervical degenerative disk disease in adjacent segments on magnetic resonance imaging (MRI) views, and complications were reviewed.
Results
The mean clinical and radiological follow-up was 45.2 months (range 24 to 102). Radiculopathy and/or myelopathy were the main clinical problems in all patients. The mean VAS scores of HC for arm pain were 7.4 ± 0.8 preoperatively; 2.8 ± 0.6, 1 month after surgery; 2.3 ± 0.6, 6 months after surgery; 1.8 ± 0.6, 12 month after surgery; and 1.6 ± 0.6, 24 months after surgery. The mean NDI scores (mean ± SD) of HC significantly improved after surgery (on admission, 57.2 ± 5.5%; 1 month after surgery, 27.35 ± 5.3%; 6 month after surgery, 21.43 ± 2.8%; 12 months after surgery, 21.9 ± 2.3%; 24 months after surgery, 20.6 ± 2.6%, p = 0.006). Hoarseness and dysphagia were the most common complications and osteophyte formation was the most frequent radiographic change.
Conclusion
Anterior cervical hybrid construction appears to be an acceptable option in the management of multilevel cervical degenerative disc diseases and spondylotic spinal stenosis.
Similar content being viewed by others
Introduction
Multilevel cervical disc disease (mCDD) and spondylotic spinal myelopathy (SSM) are frequent disorders of the human spine [1]. The ideal surgical treatment approach for mCDD and SSM is as yet questionable [2].
Anterior cervical discectomy and fusion (ACDF) is a notable treatment strategy that has been demonstrated to accomplish positive clinical outcomes in patients with mCDD. However, there are drawbacks such as adjacent segment disease (ASD) and segmental instability [1]. Cervical total disc replacement (C-TDR) which is called cervical disc prosthesis is utilized to maintain motion at the treated level [1]. Preserving physiological movement instead of fusing between two vertebrae postoperatively avoids abnormal kinematic loading at the intervertebral space above and below the level of procedure [1]. Fixation and fusion alter the physiological biomechanical behavior of the cervical spine, the range of motion (ROM) of the surgical segment is lost, which amplifies the degeneration of the adjacent segment [3]. As it were, ACDF may increase the risk of end-plate and intradiscal stress together with an overload on facets, which can quicken the degenerative course on adjacent segments [2, 4].
The utility of these 2 techniques (C-TDR + ACDF) together is called hybrid construction (HC). Hybrid construction differs from hybrid decompression. Various combinations of cervical discectomy and corpectomy have been described in hybrid decompression [5,6,7,8]. However, C-TDR and ACDF with or without plate are mentioned in HC.
In relevant publications, diminution of the active cervical ROM has been noted after the performance of ACDF with a maximum reduction of 39.5% in flexion [2]. In this context, HC combined with fusion and arthroplasty techniques in selected cases can be an option in mCDD [9].
In the present study, we aimed to assess the mid-long-term follow-up results, radiographic parameters, clinical outcomes, and complications of HC.
Materials and methods
After the approval of the institutional ethics committee (2020/21-06), a retrospective survey was carried out. Between January 2008 and October 2018, a total of 195 patients underwent HC procedure in the neurosurgery department of our tertiary care center. The data were extracted from the hospital database. Our series consisted of 105 men (53.8%) and 90 women (46.2%), with a mean age of 47.7 years (range 26–73 years). Inclusion criteria were the consecutive levels of mCDD between C3–C4 and C6–C7 with disc herniation or spondylosis, with radiculopathy or myelopathy, which was unresponsive to conservative treatment (during at least 6 weeks). All patients were followed-up clinically and radiographically for a minimum of 2 years.
Radiological data involved static and dynamic radiographs, computerized tomography (CT) scans, and magnetic resonance imaging (MRI) views. Patients who had been recently traumatized at C3–C7 levels, who had cancer metastases, and posterior compression of the spinal cord were excluded.
In HS, C-TDR or ACDF was decided preoperatively utilizing finding from radiographs, CT scans, and MRI views. C-TDR was preferred at the level without segmental instability (defined by flexion-extension radiographs of > 3.5 mm or > 15͑ͦ angular motion) and without facet joint degeneration. In cases with flexion-extension radiographic signs of cervical instability, significant vertebral body spondylosis, facet degeneration, and loss of segmental mobility, ACDF was performed. Since myelopathy was not detected in all patients and some cases presented with only radiculopathy, Japanese Orthopedic Association (JOA) scores were not included in evaluation [10].
Surgical procedure
The technique applied for HC was identical with microsurgical discectomy, corpectomy, and neural decompression method performed with the standard Cloward approach. The patient was placed in a supine position under general anesthesia. The right-sided horizontal incision was performed as for the disc level along the skin wrinkle over the neck. Intraoperative fluoroscopy was routinely used to confirm the target level in each case. The neck was slightly extended to provide physiological lordosis after surgery. In all procedures, one level of C-TDR and discectomy with interbody cage and/or anterior plate or reinforced corpectomy with a titanium cage and anterior plate were performed depending on the pathological condition in the cervical spine. The surgical procedures were performed by 2 experienced neurosurgeons in the same hospital. All materials used in surgical interventions had CE and FDA approvals and were MRI compatible.
Clinical outcomes
Clinical outcomes were reviewed based on the visual analog scale (VAS) and neck disability index (NDI) questionnaires on admission and at 1, 6, 12, and 24 months of follow-up. Pain severity was reported from 0 to 10 using a VAS (0 = no pain; 10 = the worst pain imaginable), while the NDI scores varied from 0 to 50.
Radiological evaluation
Preoperative flexion-extension radiographs, CT scans, and MRI views of the cervical spine were collected. The operative plan, the levels of fusion, and application of disc prosthesis were decided according to the analysis of the radiological images. In the MRI and CT images performed at the postoperative 12th and 24th months, findings consistent with the degeneration in the adjacent segments and spinal stenosis were investigated.
Results
In our tertiary care center, 195 patients with 2 or 3 consecutive levels of mCDD were treated using HC over 9 years. In the clinical follow-up period, the number of patients lost for follow-up were 12 and 25, respectively. The mean clinical and radiological follow-up was 45.2 months (range 24 to 102). Radiculopathy and/or myelopathy were the main clinical problems in all patients. The clinical and demographic data of the 195 patients are demonstrated in Table 1. Radiculopathy (n = 117, 60%), myelopathy (n = 58, 29.7%), and both radiculopathy and myelopathy (n = 32, 16.4%) were the most frequent disorders in this series.
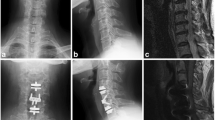
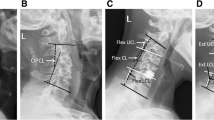
The male-to-female ratio was 105:90 and the average age was 47.7 years (range 26 to 73). The procedures and radiological images are presented in Figs. 1, 2, 3, 4, 5, 6, 7, and 8. Table 2 indicates the levels of cervical disc disease and spondylotic spinal stenosis, types of surgical interventions, and the number of patients (n) per each group.
As shown in Table 3, the mean VAS scores of HC for arm pain were 7.4 ± 0.8 preoperatively; 2.8 ± 0.6, 1 month after surgery; 2.3 ± 0.6, 6 months after surgery; 1.8 ± 0.6, 12 months after surgery; and 1.6 ± 0.6, 24 months after surgery. The mean NDI scores (mean ± SD) of HC significantly improved after surgery (on admission, 57.2 ± 5.5%; 1 month after surgery, 27.35 ± 5.3%; 6 month after surgery, 21.43 ± 2.8%; 12 months after surgery, 21.9 ± 2.3%; 24 months after surgery, 20.6 ± 2.6%, p = 0.006). Calculation of ROM and adjacent segment angulation were not used in the follow-up of patients because we thought that there may be significant differences in in vivo circumstances it depends on the radiography technique and the patient’s position during imaging. Instead, our goal was to determine whether adjacent segment disease occurred and the cervical spinal MRI and CT images were obtained at the 12th- and 24th-month follow-up. Besides, the clinically apparent signs of ASD were recorded (Table 3).
A survey of complications detected peri- and post-operatively are presented in Table 4. In our series, no cases of implant dislodgment, screw pull out, progressive kyphosis, and evidence of pseudarthrosis at the fusion levels were noted.
Discussion
There is controversy on the ideal treatment modality for mCDD [11]. The frequency of mCDD increases with age, more than 85% of the population older than 60 may suffer from severe degeneration at least at one cervical level. In the light of current literature, HC seems to be a safe and feasible treatment alternative for some patients with mCDD scheduled for operation using the anterior approach [12, 13].
Even though posterior cervical decompression, including laminectomy and laminoplasty and posterior instrumentation are effective for the achievement of backward mobility of the spinal cord, C5 nerve root palsy and axial neck pain constitute the major disadvantages. The advantages of anterior decompression are the direct removal of the lesion, including removal of osteophytes of the posterior longitudinal ligament, and correction of the cervical alignment [14].
Clinical and experimental trials yielded that fusion of cervical segments can remarkably expand the ROM of adjacent segments and intradiscal pressure, in this way increasing the risk of adjacent segment disorders particularly at the levels around the fusion [15]. In cadaver models, intradiscal pressures adjacent to a fused level were found to be as much as 73% [16].
The spondylotic spine is mostly linked with multiple-level degeneration. C-TDR may constitute an adequate alternative to fusion owing to the theoretical advantages of C-TDR, such as reduction of the non-physiological biomechanics of adjacent segments, preservation of ROM, maintenance of the functional spinal unit, and prevention of ASD. However, since C-TDR indications are more restricted than ACDF due to various criteria, it cannot be applied to every pathological segment [17].
ACDF is an accepted, safe, and reliable strategy for single-level or multi-level cervical disc disease. Nonetheless, fusion can cause a reduction in ROM and increase the stress on adjacent levels [1, 2, 4, 14, 18,19,20,21]. Moreover, numerous publications have demonstrated an increase in the number of segments involved in fusion was associated with amplification of the compensatory motion and biomechanical stress in adjacent segments. This process may eventually lead to a more prominent ASD. Biomechanical and clinical studies have shown the occurrence of symptomatic disc disease at adjacent segments [4]. A meta-analysis conducted by Tian et al. yielded that hybrid construction provided excellent clinical and radiological outcomes. Postoperative cervical ROM was found to be similar with the physiological state and no reduction was detected in ROM of the adjacent segment in HC cases [15].
There is no consensus on the segment for the performance of HC. Hybrid construction was indicated in patients with cervical spondylotic radiculopathy or myelopathy caused by continuous degeneration from C3 to C7, which were unresponsive to conservative treatment for at least 6 weeks [22]. To select and perform the optimal treatment strategy of HC, parameters such as decreasing the motion and facet force compensation at adjacent segments should be taken into account [2].
There are many reports on the clinical outcomes of ASD after ACDF in the current literature. A 10-year radiographic follow-up review indicated that there were hypermobility and degenerative changes in the non-fused segments of the spine, including disc space narrowing, end-plate sclerosis, and osteophyte formation in 50% of patients after ACDF. The rate of re-operation ranged from 5 to 20% due to symptomatic ASD [23]. Hilibrand et al. reported that ASD occurred at an annual rate of 2.9% for 10 years after ACDF [24]. C-TDR may diminish the stress on adjacent discs and thereby, potentially reducing the rate of ASD, which is estimated to be 3% per year [25].
Compensatory hyperkinesis is less likely to occur in adjacent segments if the segment involved in surgery maintains mobility [16]. A systematic review by Lu et al. had shown that the ROM at levels C2–C7 was significantly higher than ACDF after HC, and adjacent upper ROM and lower ROM were significantly lower [20]. Hybrid construction resulted in a better recovery of the NDI score at 2 years of follow-up and a similar improvement of the VAS score was noted compared to ACDF [21].
Heterotopic ossification (HO) is the bone formation outside the skeletal system. The occurrence rate of HO ranged from 16.1 to 85.7%, and the overall prevalence was 46.4% (95% CI, 40.1–52.8%) by the random-effects model. It is supposed to be an inevitable postoperative complication after cervical ADR. It can decrease the ROM of the index segment, which is in contrast with the fundamental goal of the artificial disc. The prevalence of both HO and severe HO exhibited a trend of progression. The factors associated with HO occurrence are obscure. The influence of prosthesis on the occurrence of HO needs to be elucidated in future trials [26]. In the present study, we determined a HO incidence of 5.12% and this relatively low rate may be attributed to our selection criteria or loss for follow-up.
Our data indicated that the fused segment may be overloaded on the lower or upper adjacent disc prosthesis, which may result in impairment or dislodgement. The wide range of ROM recovery measurements may be attributed to the types of prosthesis used, as well as the X-ray shooting technique and the position of the patient at that moment. The flexibility of the cervical region compared to the thoracic and lumbar regions may also remarkably influence the angle measurements.
Conclusion
To conclude, the results of the present study indicated that HS is a safe and effective alternative to multilevel fusion for the management of mCDD. Analysis of our radiological results demonstrated that HC restored the normal function of artificial disc prostheses during the follow-up periods. Furthermore, no clinical and radiological ASD was observed. We suggest that HC can be considered as an alternative therapy to multilevel fusion in selected patients with mCDD.
Availability of data and materials
All data are available in the Dokuz Eylül University Faculty of Medicine PACKS system. When requested, any information can be accessed transparently.
Abbreviations
- mCDD:
-
Multilevel cervical disc disease
- SSM:
-
Spondylotic spinal myelopathy
- ACDF:
-
Anterior cervical discectomy and fusion
- C-TDR:
-
Cervical total disc replacement
- ASD:
-
Adjacent segment disease
- HC:
-
Hybrid construction
- VAS:
-
Visual analog scale
- NDI:
-
Neck disability index
- JOA:
-
Japanese Orthopedic Association
- CT:
-
Computerized tomography
- MRI:
-
Magnetic resonance imaging
References
Lee SB, Cho KS, Kim JY, Yoo DS, Lee TG, Huh PW. Hybrid surgery of multilevel cervical degenerative disc disease: review of literature and clinical results. J Korean Neurosurg Soc. 2012;52(5):452–8. https://doi.org/10.3340/jkns.2012.52.5.452.
Zhang J, Meng F, Ding Y, Li J, Han J, Zhang X, et al. Hybrid surgery versus anterior cervical discectomy and fusion in multilevel cervical disc diseases: a meta-analysis. Medicine. 2016;95:e3621. https://doi.org/10.1097/MD.0000000000003621 Retraction in: Medicine (Baltimore). 2019; 98:e17483. Erratum in: Medicine (Baltimore). 2016; 95:e569e. Corrected and republished in: Medicine (Baltimore). 2020; 99:e19055.
Xiong Y, Xu L, Yu X, Yang Y, Zhao D, Hu Z, et al. Comparison of 6-year follow-up result of hybrid surgery and anterior cervical discectomy and fusion for the treatment of contiguous two-segment cervical degenerative disc diseases. Spine. 2018;43:1418–25. https://doi.org/10.1097/BRS.0000000000002639.
Wang KF, Duan S, Zhu ZQ, Liu HY, Liu CJ, Xu S. Clinical and radiologic features of 3 reconstructive procedures for the surgical management of patients with bilevel cervical degenerative disc disease at a minimum follow-up period of 5 years: a comparative study. World Neurosurg. 2018;113:e70–6. https://doi.org/10.1016/j.wneu.2018.01.157.
Ding F, Jia Z, Wu Y, Li C, He Q, Ruan D. Fusion-nonfusion hybrid construct versus anterior cervical hybrid decompression and fusion: a comparative study for 3-level cervical degenerative disc diseases. Spine. 2014;39:1934–42. https://doi.org/10.1097/BRS.0000000000000588.
Liu JM, Peng HW, Liu ZL, Long XH, Yu YQ, Huang SH. Hybrid decompression technique versus anterior cervical corpectomy and fusion for treating multilevel cervical spondylotic myelopathy: which one is better? World Neurosurg. 2015;84(6):2022–9. https://doi.org/10.1016/j.wneu.2015.08.039.
Odate S, Shikata J, Kimura H, Soeda T. Hybrid decompression and fixation technique versus plated 3-vertebra corpectomy for 4-segment cervical myelopathy: analysis of 81 cases with a minimum 2-year follow-up. Clin Spine Surg. 2016;29:226–33. https://doi.org/10.1097/BSD.0b013e31827ada34.
Ashkenazi E, Smorgick Y, Rand N, Millgram MA, Mirovsky Y, Floman Y. Anterior decompression combined with corpectomies and discectomies in the management of multilevel cervical myelopathy: a hybrid decompression and fixation technique. J Neurosurg Spine. 2005;3(3):205–9. https://doi.org/10.3171/spi.2005.3.3.0205.
Li Y, Zhu J, Liao Z, Zhang Z, Liu W. Hybrid constructs for performing three-level hybrid surgery: a finite element study. World Neurosurg. 2018;114:e1302–9. https://doi.org/10.1016/j.wneu.2018.03.202.
Hukuda S, Xiang LF, Imai S, Katsuura A, Imanaka T. Large vertebral body, in addition to narrow spinal canal, are risk factors for cervical myelopathy. J Spinal Disord. 1996;9(3):177–86.
Hu L, Wu T, Liu H, Wang B, Zhang J, Meng Y, et al. Influence of fusion on the behavior of adjacent disc arthroplasty in contiguous 2-level hybrid surgery ın vivo. World Neurosurg. 2019;132:e929–40. https://doi.org/10.1016/j.wneu.2019.07.073.
Xu S, Liang Y, Yu G, Zhu Z, Wang K, Liu H. Exploration on sagittal alignment and clinical outcomes after consecutive three-level hybrid surgery and anterior cervical discectomy and fusion: a minimum of a 5-year follow-up. J Orthop Surg Res. 2020;15(1):79. https://doi.org/10.1186/s13018-020-01589-7.
Barrey C, Campana S, Persohn S, Perrin G, Skalli W. Cervical disc prosthesis versus arthrodesis using one-level, hybrid and two-level constructs: an in vitro investigation. Eur Spine J. 2012;21(3):432–42. https://doi.org/10.1007/s00586-011-1974-4.
Lee MJ, Dumonski M, Phillips FM, Voronov LI, Renner SM, Carandang G, et al. Disc replacement adjacent to cervical fusion: a biomechanical comparison of hybrid construct versus two-level fusion. Spine. 2011;36:1932–9. https://doi.org/10.1097/BRS.0b013e3181fc1aff.
Chen J, Xu L, Jia YS, Sun Q, Li JY, Zheng CY, et al. Cervical anterior hybrid technique with bi-level Bryan artificial disc replacement and adjacent segment fusion for cervical myelopathy over three consecutive segments. J Clin Neurosci. 2016;27:59–62. https://doi.org/10.1016/j.jocn.2015.07.030.
Zang L, Ma M, Hu J, Qiu H, Huang B, Chu T. Comparison of hybrid surgery ıncorporating anterior cervical discectomy and fusion and artificial arthroplasty versus multilevel fusion for multilevel cervical spondylosis: a meta-analysis. Med Sci Monit. 2015;21:4057–67. https://doi.org/10.12659/msm.896584.
Li Y, Fogel GR, Liao Z, Tyagi R, Liu W. Prosthesis and hybrid strategy consideration for treating two-level cervical disc degeneration in hybrid surgery. Spine. 2018;43:379–87. https://doi.org/10.1097/BRS.0000000000002316.
Tian P, Fu X, Li ZJ, Sun XL, Ma XL. Hybrid surgery versus anterior cervical discectomy and fusion for multilevel cervical degenerative disc diseases: a meta-analysis. Sci Rep. 2015;5(1):13454. https://doi.org/10.1038/srep13454.
Zhao CM, Chen Q, Zhang Y, Huang AB, Ding WY, Zhang W. Anterior cervical discectomy and fusion versus hybrid surgery in multilevel cervical spondylotic myelopathy: a meta-analysis. Medicine. 2018;97:e11973. https://doi.org/10.1097/MD.0000000000011973 Erratum in: Medicine (Baltimore). 2018;97:e12618.
Lu VM, Zhang L, Scherman DB, Rao PJ, Mobbs RJ, Phan K. Treating multi-level cervical disc disease with hybrid surgery compared to anterior cervical discectomy and fusion: a systematic review and meta-analysis. Eur Spine J. 2017;26(2):546–57. https://doi.org/10.1007/s00586-016-4791-y.
Chang HC, Tu TH, Chang HK, Wu JC, Fay LY, Chang PY, et al. Hybrid corpectomy and disc arthroplasty for cervical spondylotic myelopathy caused by ossification of posterior longitudinal ligament and disc herniation. World Neurosurg. 2016;95:22–30. https://doi.org/10.1016/j.wneu.2016.07.065.
Cho BY, Lim J, Sim HB, Park J. Biomechanical analysis of the range of motion after placement of a two-level cervical ProDisc-C versus hybrid construct. Spine. 2010;35:1769–76. https://doi.org/10.1097/BRS.0b013e3181c225fa.
Jia Z, Mo Z, Ding F, He Q, Fan Y, Ruan D. Hybrid surgery for multilevel cervical degenerative disc diseases: a systematic review of biomechanical and clinical evidence. Eur Spine J. 2014;23(8):1619–32. https://doi.org/10.1007/s00586-014-3389-5.
Hilibrand AS, Carlson GD, Palumbo MA, Bohlman HH. Radiculopathy andmyelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1998;81:519–28.
Zhou J, Li X, Zhou X, Lin H, Dong J. Anterior decompression and hybrid reconstruction with titanium mesh cage plus plate and self-locking stand-alone cage for the treatment of three-level cervical spondylotic myelopathy. J Clin Neurosci. 2017;43:196–201. https://doi.org/10.1016/j.jocn.2017.04.022.
Kong L, Ma Q, Meng F, Cao J, Yu K, Shen Y. The prevalence of heterotopic ossification among patients after cervical artificial disc replacement: a systematic review and meta-analysis. Medicine. 2017;96:e7163. https://doi.org/10.1097/MD.0000000000007163.
Acknowledgments
None.
Funding
No financial support or funding was received for this paper.
Author information
Authors and Affiliations
Contributions
Murat YILMAZ writing. Kemal YUCESOY data collection. Resat S ERBAYRAKTAR data collection and supervision. Rifat S ALTINAG data collection. All the authors read and approved the final manuscript.
Authors’ information
Murat Yilmaz: A/Professor in Neurosurgery
Kemal Yucesoy: Professor in Neurosurgery
Resat S Erbayraktar: Professor in Neurosurgery
Rıfat S Altinag: Specialist in Neurosurgery
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the local institutional review board (2020/21-06). Written informed consent from all participants had been obtained for use of data. Strict adherence to principles announced in the Declaration of Helsinki was provided.
Consent for publication
(2020/21-06). This is attached to the editor in the form of a separate letter
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yilmaz, M., Yucesoy, K., Erbayraktar, R.S. et al. Anterior hybrid construction of multilevel cervical disc disease and spondylotic spinal stenosis: surgical results and factors affecting adjacent segment problems. J Orthop Surg Res 16, 298 (2021). https://doi.org/10.1186/s13018-021-02393-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-021-02393-7