Abstract
Background
It is known that mortality after hip fracture increases compared to the general population; the trend in mortality is a controversial issue.
The objective of this study is to examine incidence, trends, and factors associated with mortality in patients with osteoporotic hip fractures.
Methods
This is a retrospective cohort study that uses the Registry for Hospital Discharges of the National Health System of our hospital. Patients older than 45 having an osteoporotic hip fracture between 1999 and 2015 were identified. Demographic data and comorbidities were obtained. A survival analysis was performed (Cox regression and Kaplan-Meier). Incidence rate, standardized death rate (SDR), trend (Poisson regression), and risk (hazard ratio) were calculated.
Results
During 1999–2015, in our hospital, there were a total of 3992 patients admitted due to osteoporotic hip fracture. Out of these 3992 patients, 3109 patients (77.9%) were women with an average age of 84.47 years (SD 8.45) and 803 (22.1%) were men with an average age of 81.64 years (SD 10.08). The cumulative incidence of mortality was 69.38%. The cumulative mortality rate for 12 months was 33%. The annual mortality was 144.9/1000 patients/year. The 1-year mortality rate increased significantly by 2% per year (IRR 1.020, CI95% 1.008–1.033). The median overall survival was 886 days (CI95% 836–951). The probability of mortality density for a period of 10 years following a hip fracture was 16% for women and 25% for men (first 90 days). The SDR was 8.3 (CI95% 7.98–8.59). Variables that showed statistically significant association with mortality were aged over 75, masculine, institutionalization, mild to severe liver disease, chronic kidney disease, COPD, dementia, heart failure, diabetes, the Charlson Index > 2 , presence of vision disorders and hearing impairment, incontinence, and Downton scale.
Conclusions
For the last 17 years, an increase of mortality for patients with hip fracture and a higher mortality rate in men than in women were observed. Institutionalization combined with comorbidities is associated with a higher mortality.
Similar content being viewed by others
Mini abstract
The purpose of this study is to analyze mortality trend after having a first episode of osteoporotic hip fracture and factors associated with mortality over a long period of time (17 years). It was observed that the 1-year mortality rate increased 2% per year during the study period. Institutionalization combined with comorbidities is associated with a higher mortality.
Introduction
Osteoporotic hip fracture is a major health problem due to increased mortality, morbidity, and functional impact in these patients (only 30–40% of these patients recover their previous functional status) [1, 2], as well as the economic cost for the National Health System. In addition, it is expected to increase as life expectancy increases.
Increased mortality after hip fracture has been widely reported. The cumulative mortality after 1 year of a hip fracture occurrence ranges between 20 and 40% [3,4,5,6,7] with higher mortality rates in men than in women [8,9,10]. After having a hip fracture, the mortality risk from any other cause increases between five and eight times, and although it decreases over the first years, excess mortality stays higher than mortality for the general population for a period of at least 10 years [10, 11].
Literature describes different factors associated with mortality, among them were age, masculine gender, dementia, heart pathology, institutionalization, comorbidity, and change of residence or rehabilitation programs carried out after hip fracture [12,13,14].
One aspect of mortality associated with hip fracture, and seldom researched, is the trend of mortality rates over a long period of time.
The purpose of this study is to analyze mortality, as well as factors associated and trends in mortality over time in patients with osteoporotic hip fracture in an urban municipality of Spain.
Material and methods
Retrospective observational cohort study for the area covered by the Hospital Universitario Fundación Alcorcon from January 1, 1999, until December 31, 2015.
Introduction
Alcorcon is in the metropolitan area of Madrid in Spain. It is a clear example of a dormitory town since half of its population works in Madrid. Its population pyramid is typical of an aging population. The Hospital of Alcorcon is the only public hospital servicing this district and all the hip fractures occurring in the area. Until 2011, the sphere of influence of the Hospital included 18 municipalities (17 were rural and 1 urban), among them was Alcorcon city, with a total population of 273,703 inhabitants. However, from 2012, the hospital only attended one municipality: Alcorcon city with 167,136 inhabitants.
Data source and definitions
Records on hip fractures (HFx) were obtained from the admissions’ database of this hospital. All hospitals in Spain use this database which collects the minimum basic data set (MBDS) of each patient admitted to any Spanish hospital: reasons for admission, procedures, and diagnosis codified in accordance with International Classification of Diseases 9 (ICD-9). We ascertained all hip fracture cases occurred in persons 45 years old or older from ICD-9 codes 820.0 to 820.9 in the study years. All cases that occurred to subjects aged 45 years or older from ICD-9 820.0 to 820.9 codes during that period of study were identified, including both first and second instances of fracture. Thanks to a recent work published by our team and where the same database was used, we know that 7.5% of all fractures included in that period correspond to second fractures [15]. Only osteoporotic fractures were taken into consideration. As an example, pathologic fractures (ICD-9 733.1–733.19), metastasis, metabolic diseases such as Paget’s disease (M89.9), femur fractures of different location (821.0–821.9), or acetabular pelvis fractures (808.0–808.9) as well as fractures due to traffic accident (V87.9) were excluded. Data derived from readmissions were removed. An admission in the same center within the first 30 days after discharge due to the same medical reason was considered a readmission. Patients having a fracture within that period had a follow-up until the end of the study (December 31, 2015). The MBDS was queried to check whether the patient had died or had been readmitted for a different reason after the fracture. Losses to follow-up or deceased patients were cross-checked with death certificates obtained from the National Death Index or INDEF, by its Spanish acronym (https://indef.msssi.es/indefWeb/loginAction.do). Second fractures were excluded from the survival analysis, and only the date of the first fracture was considered for analysis. In this study, with the objective of facilitating the comparison with previous studies, only population over 45 years of age were included.
The following data were collected at the moment of the first fracture: sex, age, place of residence (nursing home or own home), type of fracture (intra- or extracapsular), time elapsed until surgery, and time of hospitalization. Additionally, the following data on comorbidity (identified by ICD code) were recorded: dementia, diabetes mellitus, obesity, neoplasm, mild to severe liver disease (defined as evidence of portal hypertension: ascites, esophageal varices, or encephalopathy), chronic obstructive pulmonary disease, skin sores, cardiovascular disease (ischemic cardiopathology, brain stroke, congestive heart failure, and peripheral artery disease). Charlson Index calculation was performed based on comorbidity data. Additional data were collected from the Nursing Assessment Form on admission. This questionnaire started to be used in our center in 2010, so only data from the last 5 years of study were collected. During this period of 5 years, 1154 patients were included, and out of this total, the form was completed for 810 patients. Data collected by this questionnaire consisted of vision disorder and hearing impairment, urinary and/or fecal incontinence, all the Norton scale items plus its final score that quantifies the risk of bed sores, the Downton scale, technical aid to the patient’s evolution, and habitual treatment.
To calculate standardized mortality ratios (SMRs), the population and mortality in Madrid were used as a reference. Data were obtained from the Statistical Institute of the Community of Madrid (http://www.madrid.org/iestadis).
Statistical analysis
The follow-up period covers the time between the dates of hospital admission, due to hip fracture, and patient’s death. Three 4-year initial periods and one 5-year final period were defined for the analysis.
The annual mortality rate was calculated after the occurrence of an osteoporotic hip fracture per 100,000 inhabitants in people older than 45 and by sex, the numerator being the cases of death after first hip fracture registered in the MBDS and the denominator being the population at risk (those who had a first hip fracture and were still alive).
The cumulative rate of mortality was calculated for 1, 3, 6, 12, and 36 months over the time of study (17 years), global, and by sex. The probability of mortality density was also analyzed during a period of 10 years following a hip fracture. Specific mortality rates by age and sex, based on the time between fracture and death or end of study, were compared to rates of expected mortality by age and sex in the Madrid population (standardized mortality ratios or SMRs). Assuming a Poisson distribution, statistical significance and the respective 95% confidence intervals (CI95%) were calculated.
Kaplan-Meier survival analysis was used to compare survival time between the different periods and by age and sex. Bivariate and multivariate Cox regression analyses were performed to analyze differences between patients and factors associated with mortality. Results were expressed as hazard ratios (HR) with their corresponding CI95% values.
Change in the annual rates of death after hip fracture was analyzed by generalized linear models (GLM) with Poisson distribution or negative binomial distribution in case of over-dispersed data. Models were used to estimate the incidence rate ratio of the variables at 1, 3, and 12 months with CI95%; the p value of association was noted as a result of the trend test. The significance level was established at 1% to account for the use of aggregated data. To allow for a clearance period, year 1999 was excluded from the analysis.
Patients’ clinical and demographic characteristics were described. Quantitative data were described by their median and standard deviation or by median and interquartile range (IQR). Qualitative data were described by counts and percentage. The relative frequency of the different variables for each period was also analyzed in order to find out if they have changed over the study period.
The statistical analysis was carried out with IBM SPSS 24.0 and Stata 14 software.
Results
During the study period (1999–2015), there were a total of 3992 patients admitted due to osteoporotic hip fracture. Out of these 3992 patients, 3109 patients (77.9%) were women with an average age of 84.47 years (SD 8.45) and 803 (22.1%) were men with an average age of 81.64 years (SD 10.08). Moreover, 86.2% were patients of age over 75 years.
The majority of patients (73.9%) were living in their own homes and not institutionalized before the fracture occurrence. Among institutionalized patients, 81.95% were women. The average Charlson Index was 1.08 (SD 1.50), and in women, it was 0.70 (SD 1.14). Out of the total amount, 7.4% of patients had a Charlson Index above 2 (men 12.1% out of the total of men and women 6.1% out of the total of women).
Cumulative mortality
Global cumulative mortality over the 17 years of study was 69.38% (634 men and 2136 women). Cumulative mortality rate for 1, 3, 6, 12, and 36 months after fracture was 9.2%, 17.4%, 24.6%, 33%, and 56%, respectively, being higher in men than in women (men 13.7%, 25%, 32.7%, 43.3%, and 65.6%; women 7.9%, 15.7%, 22.3%, 30%, 53.2%).
Mortality rates
Table 1 shows crude mortality rate adjusted by age, sex, and year of study. Annual mortality rate in population older than 45 years was 144.9/1000 patients/year (173.70 in men and 138.11 in women). Table 2 shows crude mortality rate by sex and age-adjusted.
Trend in mortality
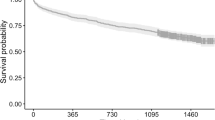
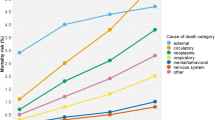
Through the use of GLM, it is observed that 1-year mortality rate increased 2% per year in a significant way (IRR 1.020, CI95% 1.008–1.033). One-month mortality rate remained stable without increasing or decreasing (IRR 1.020, CI95% 0.967–1.050) and the same happened for 6-month mortality rate (IRR 1.016, CI95% 0.997–1.035) (Fig. 1).
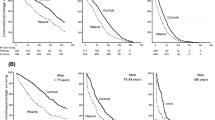
Probability of mortality density
Figure 2 shows probability of mortality density for a period of 10 years following the hip fracture occurrence. It is around 16% of women and 25% of men in the first 90 days, falling rapidly in the first year and stabilizing around 2% every 90 days in the following years.
Standardized mortality
Regarding general mortality in Madrid, the standardized mortality ratio (SMR) in the 17 years of study was 8.3 (CI95% 7.98–8.59) with very similar values in men (8.03; CI95% 7.43–8.47) and women (8.77; CI95% 8.41–9.14).
Factors associated to mortality after hip fracture occurrence
The bivariate regression Cox analysis (Table 3) shows association between mortality and the following items: age (IRR 1.05, CI95% 1.04–1.06), masculine gender (IRR 1.32, CI95% 1.21–1.44), institutionalization (IRR 1.48, CI95% 1.36–1.60), Charlson Index 2 (IRR 1.98, CI95% 1.73–2.26), mild or severe hepatic disease (IRR 3.25, CI95% 2.17–4.86), kidney failure (IRR 1.87, CI95% 1.60–2.18), heart failure (IRR 2.50, CI95% 2.07–3.00), chronic obstructive pulmonary disease (IRR 1.46, CI 95% 1.30–1.64), diabetes (IRR 1.11, CI95% 1.02–1.2), or dementia prior to the fracture (IRR 1.46, CI95% 1.30–1.62). From the factors collected in the Nursing Assessment Form, those associated were hearing impairment (IRR 1.552, CI95% 1.18–1.97) and previous vision disorders (IRR 1.50, CI95% 1.11–2.03), urinary incontinence (IRR 1.53, CI95% 1.25–1.88) and fecal incontinence (IRR 1.66, CI95% 1.32–2.07), and Downton scale total score (IRR 1.65, CI95% 1.32–2.08).
In the survival analysis, men die more frequently and earlier than women after hip fracture (Additional file 1: Figure S1). In the analysis by periods, the trend is that mortality is also earlier (Fig. 3).
Discussion
Numerous studies proved that the mortality risk after hip fracture is increasing [10, 11, 16, 17]. This increase in mortality is not exclusive to hip fracture, and it is also associated with vertebral fractures [18, 19] and practically all major osteoporotic fractures, such as humerus fracture [20, 21], pelvis fracture [22, 26], distal end of femur fracture[22], and rib fracture [22, 26], and at all ages [18, 19]. Moreover, a second fracture results in an additional increase in mortality [18].
In this study, mortality in patients with hip fracture has been analyzed over a long period of time (1999–2015). This allowed for research into trends in mortality rates, which is currently a controversial topic. The main finding of this study is that the trend in 1-year mortality rate has increased 2% per year during the period of study. Other findings corroborate well-known results obtained from other studies: in the first place, mortality in patients with hip fracture increases a lot compared to the general population; secondly, mortality rate is higher in men than in women; thirdly, death risk is very high right after the fracture occurrence (it drops over the first year and remains stable afterwards); fourthly, institutionalization combined with comorbidity is associated with a higher mortality.
A few studies presented results on trends in mortality after osteoporotic hip fracture. Some of them, from different nationalities, show that mortality remained stable over the years [16, 23, 24]. Other studies described small increases in excess mortality due to hip fracture in specific population groups (elderly women) [10], and others described a variable reduction, although moderate in general, in mortality rates over time [25,26,27,28]. Being a study that covers a long period of time, this study allows us to analyze trends in mortality in patients with hip fracture. The study observes a growing trend of mortality of 2% per year at 1 year, while short-term mortality remains stable (1 to 6 months). We believe that the observed increase in mortality rate is due to a growing proportion of men over women occurred over the years of the study period, and men, as is explained below, have a higher mortality rate. While in the first period of the study (1999–2002) men had 21.5% of all fractures, in the final period (2011–2015), this figure increased up to 25.7%. Another factor, probably having an impact on this raise, is the increase in comorbidity observed over the period of study. While in the first period (1999–2002) 5.3% of patients had a Charlson Index over 2, in the final period (2011–2015), it increased up to 11.1%.
In accordance with different studies, cumulative 1-year mortality after hip fracture varies between 20 and 40% [5, 29, 30] with higher rates of mortality observed in men than women [8, 31]. In previous studies done in Spain, 1-year mortality has been placed around 21–23% [12, 13] and varies widely depending on the regions [32]. In this study, a cumulative 1-year mortality of 30% in women and 43% in men has been obtained, which is clearly higher than data obtained from previous studies. The difference between results obtained in this study and previous studies can possibly be found in the methodology used. In this study, we have searched for patients’ deaths through the national database of death certificates, while in the rest of studies this was not done.
In this study, the standardized mortality index for the whole period of study (17 years) has been analyzed in comparison with the global mortality in Madrid based on data obtained from the National Institute of Statistics (INE, by its Spanish acronym). We obtained an 8 SMR. This finding is similar to those of other authors working with series such as the Forsen study [33], the Johnell study [34], or the Fransen study [35]. Forsen et al. [33] found a 1-year mortality risk of 9 in subjects aged between 50 and 74 years, 5.1 for subjects aged between 75 and 85 years, and 5.7 for subjects older than 85. Johnel et al. [34] found a 1-year mortality risk of 10.2 in men and 9.1 in women. Fransen et al. [35, 40] found a 2-year mortality risk of 7.18 in women.
Epidemiological studies have consistently proved that men present a higher risk of mortality [8, 9]. This study, as other studies did, found a higher risk of mortality in men than in women. Masculine sex presents a 30% increase in death risk compared to women. In contrast to other studies that do not find that excess mortality in men compared to women is due to comorbidities [36], this study observed that men present higher comorbidity, measured by the Charlson Index which would justify this increase of mortality.
Likewise, the study observes, as other studies do [7], the fact that death risk is very high immediately after hip fracture and that this risk rapidly drops over the first year, stabilizing with a slight trend downwards over the following years (Fig. 2).
Lastly, the role of comorbidities as a factor increasing risk mortality is controversial [37]. In our study, the risk factors most strongly associated with mortality (HR > 2) were moderate-severe liver disease, to be older than 75 years, and heart failure. Other risk factors also associated with mortality (HR between 1 and 2) were male, Charlson index greater than 2, diabetes mellitus, living in a nursing home, COPD, myocardial infarction, dementia, and renal failure. It has been hypothesized that comorbidities play a major role as a cause of mortality after fracture. In fact, several studies [12, 38], as this study did, found an association between the severity of comorbidities and mortality risk. In a study based on Medicare USA data, after adjustment by comorbidities, the risk of mortality dropped significantly over the early post-fracture period (first 6 months) and disappeared completely over the later post fracture period of follow-up (over 6 months) [37]. Due to this dramatic drop of excess mortality with adjustment of state of health, the authors concluded that the majority of early deaths and all late deaths were not attributable to hip fracture. In a different Spanish study, the severity of comorbidities was also found to be associated with an increase of mortality after vertebral fracture [37]. Nevertheless, not all studies found an association between comorbidity and post-fracture mortality. In the Study Osteoporotic Fractures (SOF), the adjustment by comorbidity did not affect the relationship between mortality risk and any of the examined fractures [39]. Similar findings were obtained in other studies [40]. This study is groundbreaking as we had the chance to analyze the data collected from a Nursing Assessment Form on admission for a subgroup of 810 patients. This form collects specific data on the patient’s quality of life before admission, such as vision and hearing capacity, presence of urinary incontinence, fecal incontinence, Downton scale (measuring risk of falling), and Norton scale (measuring risk of developing bedsores). In this study, it was found that, with the exception of Norton scale total score, all these factors are associated with risk of death. It seems that we can conclude that a previous bad quality of life is associated with a higher mortality after hip fracture. Unfortunately, the absence of data on established treatments does not allow us to assess with certainty whether different treatments have been taken or avoided in these groups with higher risk. It is striking that among the associated factors are institutionalized and older people, that is, the more fragile patients who sometimes have to stabilize before proceeding with surgical treatment, delaying one of the known factors that increase mortality. In relation to the increase in mortality in males, the associated comorbidities that sometimes require prior stabilization is also one of the main causes of surgical delays. In daily practice, knowing the most vulnerable subgroups forces us to maximize therapeutic care in these subgroups with a higher risk of mortality.
This study also presents some limitations, among them were those typical of a retrospective study that uses administrative databases as main source, and these limitations may cause a loss of data. Additionally, since it is a large-scale population and a long period of study, some variables could not be obtained from all patients (for example, date of surgery or data collected on the Nursing Assessment Form on admission which was only implemented in our center for the last few years of study). Time delay between the fracture and surgery could not be observed. Important variables for this profile of patient, i.e., the use of different treatments such as bisphosphonates and other therapeutic methods, could not be examined since our database lacks this type of data. Another limitation of our work, it is that which refers to the use of HR in retrospective cohort studies. The use of the HR for causal inference is not straightforward even in the absence of unmeasured confounding, measurement error, and model misspecification. Endowing a HR with a causal interpretation is risky for 2 key reasons: the HR may change over time, and the HR has a built-in selection bias. Nevertheless, this study presents some strength. It is a series with a large number of patients (3992) that includes all osteoporotic hip fractures treated in a tertiary hospital. For this reason, we think that this study is very representative of the urban population of the center of Spain, and it was carried out over a long period of time (17 years). Additionally, numerous variables were collected, and some of them, related to mortality after hip fracture, have not been studied until now, such as Downton or Norton scales.
In conclusion, in this study, we found that 1-year mortality has increased over the last 17 years, and we corroborate specific aspects of mortality that were established in other previous epidemiologic studies, i.e., that mortality in patients with hip fracture increased highly compared to the general population, that mortality risk is higher in men than in women, that death risk is very high immediately after fracture and drops over the first year remaining stable afterwards, and that institutionalization combined with comorbidity are associated with higher mortality. Additionally, some factors related to quality of life before hip fracture are identified, i.e., vision disorders, hearing impairment, incontinence, or Downton scale, which are associated with an increase in mortality for these patients.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available due to the protected data from the Hospital records but are available from the corresponding author on reasonable request. Some data like population census are available at the National Statistical Institute of Spain (www.ine.es). Some data such as the Spanish minimal hospital common data or CMBD are available at the URL https://pestadistico.inteligenciadegestion.mscbs.es.
Abbreviations
- CI95%:
-
95% confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- HFx:
-
Hip fracture
- HR:
-
Hazard ratio
- ICD-9:
-
International Classification of Diseases 9
- INDEF:
-
Índice Nacional de Defunción
- IRR:
-
Incidence rate ratio
- MBDS:
-
Minimum basic data set
- SD:
-
Standard deviation
- SDR:
-
Standardized death rate
References
O’Neill TW, Roy DK. How many people develop fractures with what outcome? Best Pract Res Clin Rheumatol. 2005;19:879–8955.
Cree M, Soskolne CL, Belseck E, Hornig J, McElhaney JE, Brant R, Suarez-Almazor M. Mortality and institutionalization following hip fracture. J Am Geriatr Soc. 2000;48:283–8.
Tarazona-Santabalbina FJ, Belenguer-Varea A, Rovira-Daudi E, Salcedo-Mahiques E, Cuesta-Peredó D, Doménech-Pascual JR, Salvador-Pérez MI, Avellana-Zaragoza JA. Early interdisciplinary hospital intervention for elderly patients with hip fractures: functional outcome and mortality. Clinics (Sao Paulo). 2012;67(6):547–56.
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353(9156):878–82.
Browner WS, Pressman AR, Nevitt MC, Cummings SR. Mortality following fractures in older women. The study of osteoporotic fractures. Arch Intern Med. 1996;156(14):1521–5.
Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761–7.
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK. The components of excess mortality after hip fracture. Bone. 2003;32(5):468–73.
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20(10):1633–50.
Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B. Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing. 2010;39(2):203–9.
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–90.
Omsland TK, Emaus N, Tell GS, Magnus JH, Ahmed LA, Holvik K, et al. Mortality following the first hip fracture in Norwegian women and men (1999-2008). A NOREPOS study. Bone. 2014;63:81–6.
Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43(6):676–85.
L Riska BS, Forsén L, Omsland TK, Søgaard AJ, Meyer HE, Holvik K. Does the association of comorbidity with 1-year mortality after hip fracture differ according to gender? The Norwegian Epidemiologic Osteoporosis Studies (NOREPOS). J Am Geriatr Soc. 2018;66(3):553–8.
Ha Y, Park Y, Nam KW, Kim S. Trend in hip fracture incidence and mortality in Korea: a prospective cohort study from 2002 to 2011. J Korean Med Sci. 2015;30(4):483–8.
Ariza-Vega P, Kristensen MT, Martín-Martín L, Jiménez-Moleón JJ. Predictors of long-term mortality in older people with hip fracture. Arch Phys Med Rehabil. 2015;96(7):1215–21.
Menéndez-Colino R, Alarcon T, Gotor P, Queipo R, Ramírez-Martín R, Otero A, et al. Baseline and pre-operative 1-year mortality risk factors in a cohort of 509 hip fracture patients consecutively admitted to a co-managed orthogeriatric unit (FONDA Cohort). Injury. 2018.
Jacobs H, Zeeb H, Hoffmann F. Incidence rates of and mortality after hip fracture among German nursing home residents. Int J Environ Res Public Health. 2018;15:2.
Ireland AW, Kelly PJ, Cumming RG. Associations between hospital-based rehabilitation for hip fracture and two-year outcomes for mortality and independent living: an Australian database study of 1724 elderly community-dwelling patients. J Rehabil Med. 2016;48(7):625–31.
Mazzucchelli R, Pérez-Fernández E, Crespí N, García-Vadillo A, Rodriguez Caravaca G, Gil de Miguel A, et al. Second hip fracture: incidence, trends, and predictors. Calcif Tissue Int. 2017.
Yoon H, Park C, Jang S, Jang S, Lee Y, Ha Y. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011;26(8):1087–92.
Vestergaard P, Rejnmark L, Mosekilde L. Has mortality after a hip fracture increased? J Am Geriatr Soc. 2007;55(11):1720–6.
Bliuc D, Milch VE, Nguyen TV, et al. Mortality risk associated with low-trauma Osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301:513–21.
Huntjens KM, Kosar S, van Geel TA, et al. Risk of subsequent fracture and mortality within a period of 5 years after a non-vertebral fracture. Osteoporos Int. 2010;21:2075–82.
Johnell O, Kanis JA, Oden A, et al. Fracture risk following an osteoporotic fracture. Osteoporos Int. 2004;15:175–9.
Piirtola M, Vahlberg T, Lopponen M, Raiha I, et al. Fractures as predictors of excess mortality in the aged – a population-based study with a 12-year followup. Eur J Epidemiol. 2008;23:747–55.
Melton LJ 3rd, Achenbach SJ, Atkinson EJ, et al. Long-term mortality following fractures at different skeletal sites: a population-based cohort study. Osteoporos Int. 2013;24:1689–96.
Somersalo A, Paloneva J, Kautiainen H, et al. Increased mortality after upper extremity fracture requiring inpatient care. Acta Orthop. 2015;86:533–57.
Karlsson MK, Hasserius R, Obrant KJ. Individuals who sustain nonosteoporotic fractures continue to also sustain fragility fractures. Calcif Tissue Int. 1993;53(4):229–31.
Karampampa K, Ahlbom A, Michaëlsson K, Andersson T, Drefahl S, Modig K. Declining incidence trends for hip fractures have not been accompanied by improvements in lifetime risk or post-fracture survival--a nationwide study of the Swedish population aged 60 years and older. Bone. 2015;78:55–61.
Chau PH, Wong M, Lee A, Ling M, Woo J. Trends in hip fracture incidence and mortality in Chinese population from Hong Kong 2001-09. Age Ageing. 2013;42(2):229–33.
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–9.
Finnes TE, Meyer HE, Falch JA, Medhus AW, Wentzel-Larsen T, Lofthus CM. Secular reduction of excess mortality in hip fracture patients >85 years. BMC Geriatr. 2013;13:25.
Sullivan KJ, Husak LE, Altebarmakian M, Brox WT. Demographic factors in hip fracture incidence and mortality rates in California, 2000-2011. J Orthop Surg Res. 2016;11:4.
Leslie WD, O'Donnell S, Jean S, Lagacé C, Walsh P, Bancej C, et al. Trends in hip fracture rates in Canada. JAMA. 2009;302(8):883–9.
Orces CH, Alamgir AH. Trends in hip fracture-related mortality in Texas, 1990-2007. South Med J. 2011;104(7):482–7.
Medin E, Goude F, Melberg HO, Tediosi F, Belicza E, Peltola M. European regional differences in all-cause mortality and length of stay for patients with hip fracture. Health Econ. 2015;24(Suppl 2):53–64.
Mazzucchelli Esteban R, Pérez-Fernández E, Crespí-Villarías N, García-Vadillo A, Rodriguez-Caravaca G, Gil de Miguel A, et al. Trends in osteoporotic hip fracture epidemiology over a 17-year period in a Spanish population: Alcorcón 1999-2015. Arch Osteoporos. 2017;12(1):84.
Forsén L, Sogaard AJ, Meyer HE, et al. Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int. 1999;10:73–8.
Johnell O, Kanis JA, Odén A, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15:38–42.
Fransen M, Woodward M, Norton R, et al. Excess mortality or institutionalization after hip fracture: men are at greater risk than women. J Am Geriatr Soc. 2002;50:685–90.
Acknowledgements
The authors thank the staff of the Research Unit of the Spanish Society of Rheumatology for their support in the editing and translation of the manuscript. To my good friend Caligula, who faithfully accompanies me in my research work.
Funding
There was no funding in the development of the article.
Author information
Authors and Affiliations
Contributions
OGI and RM wrote the paper. OGI, RM, and NCV designed the research. EPF and CAB did the main data analysis. CAB also helped in the figures. FJQD and MP collaborated in the bibliographical research process and contributed with the CMBD (hospital data) process. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Clinical Ethics Committee of the Hospital Universitario Fundacion Alcorcón approved the study.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Figure S1. Supplementary material. Survival analysis by sex. (DOCX 153 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Guzon-Illescas, O., Perez Fernandez, E., Crespí Villarias, N. et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res 14, 203 (2019). https://doi.org/10.1186/s13018-019-1226-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-019-1226-6