Abstract
Background
Radiological outcomes between anterior and posterior approach in Lenke 5C curves were still controversial. Meta-analysis on published articles to compare fusion segments and radiological outcomes between the two surgical approaches was performed.
Methods
Electronic database was conducted for searching studies concerning the anterior versus posterior approach in Lenke 5C curves. After quality assessment, data of means, standard deviations, and sample sizes were extracted. RevMan 5.3 was adopted for data analysis.
Results
Seven case-control studies involving 308 Lenke 5C AIS patients were identified in the meta-analysis. No significant differences were noted in correction rate of thoracolumbar/lumbar curve (95 % CI −6.02 to 4.32, P = 0.75) and incidence of proximal junctional kyphosis (95 % CI 0.12 to 7.19, P = 0.94) of final follow-up, in change values of thoracolumbar/lumbar curve (95 % CI −3.28 to 7.19, P = 0.46) and thoracic kyphosis (95 % CI −4.10 to 0.13, P = 0.07). The anterior approach represented a significant shorter fusion segments compared to posterior approach (95 % CI −1.72 to −0.71, P < 0.00001). The posterior approach obtained a larger increasing Cobb angle of lumbar lordosis than the anterior approach (95 % CI −6.06 to −0.61, P = 0.02).
Conclusions
The anterior and posterior approach can obtain comparable coronal correction, change values of thoracic kyphosis, and incidence of proximal junctional kyphosis. The anterior approach saves approximate one more fusion segment, and the posterior approach can obtain a larger increasing Cobb angle of lumbar lordosis, from preoperation to final follow-up.
Trial registration
The article type of this study is meta-analysis and prospective registration is not required.
Similar content being viewed by others
Background
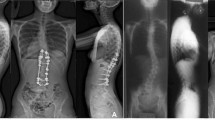
Adolescent idiopathic scoliosis (AIS) afflicted 1–3 % adolescents at danger age of 10–16 years, and the pathogenesis continued to be obscure [1]. Lenke 5 AIS could be defined as a structural thoracolumbar/lumbar (TL/L) curve, with the upper thoracic and main thoracic curves were nonstructural. Lenke 5 AIS was then subdivided into A, B, or C according to lumbar spine modifier, and “C” indicates the central sacral vertical line medial to the lumbar apex [2]. The generally approved threshold for surgical treatment in AIS was a prime curve larger than 45° [1].
Anterior invasive technique was introduced by Dwyer and Schafer [3]. From the primitive Dwyer cable to the later Zeilke-instrumentation, vertebral screw [4], and screw-single rod system, anterior approach had been practiced excellently in the correction of coronal plane [5]. With shorter fusion levels, anterior invasive technique was once the primary option for Lenke 5C curves. However, the disadvantages of the anterior approach were the poor derotation, kyphosis tendency, impairment of pulmonary function, and higher occurrence rate of implant breakage [6–8].
Posterior instrumentation continued to be the domination of surgical treatment for AIS patients. In 1962, Harrington initially introduced the operational invasive technique for spine deformity, which was regarded as the revolution of orthopedic surgery [9]. Cotrel-Dubousset system, the modern third-generation instrumentation, was constituted of segmental lamina grapple hooks and cross-linked double rods [10]. With the fantastic pull-out strength of pedicle screws comparing to traditional hooks, the pedicle screws resulted in the evolution of fourth-generation instrumentation [11–13]. However, the potential risk of implant malposition, neurological injury, increased operation time, and implant cost, which were related to pedicle screw placement, should be taken into a serious consideration [14–17].
Radiological outcomes between the two approaches in Lenke 5C curves were still controversial. Scholars used to be focused on the coronal correction and obtained different results [5, 13], and the sagittal correction had drawn more and more attentions in recent few years, especially for thoracic kyphosis (TK) and proximal junctional kyphosis (PJK; Cobb angle between the most proximal instrumented vertebra and the segment two levels cephalad) [18, 19]. In addition, to achieve a more stable correction with less fusion segments was the aim of each surgeon. The purpose of the current article was to compare the fusion segments, correction rate of TL/L curve, incidence of PJK, and change values of TL/L curve, TK, lumbar lordosis (LL) from preparation to final follow-up.
Methods
Search strategy
The searched database included the following: MEDLINE, the Web of Science, EMBASE, and Cochrane Library. Keywords included “Lenke 5” OR “thracolumbar/lumbar scoliosis”, and the publication date was from January 2005 to March 2016. In order to avoid potentially relevant studies escaped by the initial search, the “relevant items” and “references” of the included studies were also searched. In total of 717 potentially relevant studies identified from electronic databases. Two authors independently searched and extracted the data. Any difference was settled by mutual agreement.
Selection criteria
Selection criteria: (1) AIS diagnosis; (2) Lenke 5C type; (3) case-control studies included anterior and posterior approach; (4) 1-year minimum follow-up; (5) articles published after January 2005; and (6) adequate data (sample size, mean, and SD) was provided for meta-analysis. All studies that did not fulfill the above principles were eliminated. In order to elucidate the possible repetition of patients, articles published in the space of a couple of years with similar title and authors were excluded.
Data extraction
For the published studies that fulfill our inclusion criteria, information was cautiously extracted and computerized. The extracted variables were as follows (1) fusion segments; (2) Cobb angle of TL/L curve, TK, and LL, including preoperation and final follow-up; (3) correction rate of TL/L curve of final follow-up; (4) incidence of PJK of final follow-up; (5) study characteristics; (6) duration of follow-up; (7) sample size and gender of patients; (8) Risser sign; and (9) authors’ names and publication of year.
Quality assessment
In order to reduce the risk of bias, the Cochrane Handbooks version 5.1.0 recommended the Newcastle-Ottawa scale (NOS) to evaluate the non-randomized controlled trial (RCT) articles. Rather than case reports, all the potentially relevant articles were case-control studies, so the NOS was competent for quality assessment. The NOS covers three dimensions to assess the included articles, including selection, comparability, and exposure [20]. Study with a score less than six was regarded as a high risk of bias, and it should be excluded. Quality assessment was undertaken by two independent reviews and differences being resolved by consensus if necessary.
Statistical analysis
For statistical analysis, the RevMan software (the Cochrane Collaboration, Version 5.3) was adopted. With regard to continuous variables, such as correction rate of TL/L curve, mean different and 95 % confidence interval were presented, while dichotomous variables as incidence of PJK, odds ratios, and 95 % confidence interval were reported. When heterogeneity test showed I 2 ≥ 50 %, we adopted the random effects model, and the fixed effect model was used when I 2 < 50 %. In some studies, change values were not reported, a statistical transformation was conducted according to the data of preoperation and final follow-up, and the transformation formula we adopted was recommended by the Cochrane Handbooks version 5.1.0.
Results
Description of study
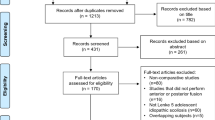
Meta-analysis was performed on outcomes of seven case-control studies [21–27], two articles were excluded for parallel publication [28, 29]. The details of the study selection were shown in Fig. 1. All of the seven studies, 308 patients diagnosed with Lenke 5C AIS were included, and no significant differences were observed in age and preoperative TL/L Cobb angle between the anterior and posterior approach. The description information about the included articles was shown in Table 1.
Quality assessment
Seven articles were rated by two independent reviews, and differences were resolved by consensus if necessary. The score of the seven articles were six to eight according to the NOS, which suggested that all the seven articles should be included. The detailed quality assessment was showed in Table 2.
Fusion segments
Data of the fusion segments were extracted from seven studies [21–27]. Compared with the posterior approach, anterior approach represented a significant shorter fusion segments (95 % CI −1.72 to −0.71, P < 0.00001; I 2 = 84 %; Fig. 2), which suggested that the anterior approach saved approximate one fusion segment.
Change values of TL/L curve
Data of TL/L curve were available in five articles [21, 22, 24, 25, 27]. No significant difference was showed in the change values of TL/L curve between the anterior and posterior approach (95 % CI −3.28 to 7.19, P = 0.46; I 2 = 83 %; Fig. 3), from preoperation to final follow-up.
Correction rate of TL/L curve
Data of TL/L curve correction rate were available in four articles [22, 23, 25, 27]. No significant difference was showed in TL/L curve correction rate of final follow-up between the two approaches (95 % CI −6.02 to 4.32, P = 0.75; I 2 = 77 %; Fig. 4).
Change values of TK
In the analysis of TK, data were extracted from six studies [21–23, 25–27]. No significant differences were found in the change values of TK between the anterior and posterior approach (95 % CI −4.10 to 0.13, P = 0.07; I 2 = 29 %; Fig. 5), from preoperation to final follow-up.
Change values for LL
Data of LL were available in six articles [21–23, 25, 27]. According to the statistical analysis, significant difference was showed in the change values of LL (95 % CI −6.06 to −0.61, P = 0.02; I 2 = 8 %; Fig. 6). The posterior approach obtained a larger increasing Cobb angle of LL than the anterior approach, from preoperation to final follow-up.
Incidence of PJK
The data were extracted from three studies [21, 24, 26]. However, no significant difference was noted between the two approaches in incidence of PJK of final follow-up (95 % CI 0.12 to 7.19, P = 0.94; I 2 = 65 %; Fig. 7).
Discussion
The clinical outcome and early disc degeneration of saving one more fusion segment were still unclear. Helenius et al. reviewed 98 consecutive patients at a minimum of 19.1 years follow-up and concluded that no association between the spondylodesis fusion segment and the Scoliosis Research Society total score [30]. Danielsson et al. compared patients fused to L3 (n = 102) versus L4 (n = 37) and reported that saving one more segment had no clinical relevance at least 23 years follow-up [31]. Regarding to the early disc degeneration, Sudo et al. reported that patients with anterior approach did not preserve the patients from disc degeneration [32]. Perez-Grueso et al. reported a similar paper with a minimum follow-up of 10 years and concluded that patients who underwent spinal fusion surgery had a similar disc degeneration to general population [33].
Data of the fusion segments were extracted from seven studies. Compared with posterior approach, anterior approach represented a significant shorter fusion segments (95 % CI −1.72 to −0.71, P < 0.00001), which suggested that the anterior approach saved approximate one fusion segment. Although the clinical outcome and early disc degeneration of saving one fusion segment were still unclear, saving fusion segment indicates less anchors and less implant cost. Wang et al. reported the comparison of implant cost between the anterior and posterior approach ($ 6157 vs. 10,336, P < 0.0001) [12]. Medical expense was important to the decision of surgeons, especially in developing countries. Sudo et al. reported that the anterior approach produced satisfactory radiographic, clinical, and functional outcomes in Lenke 5C AIS with a mean of 17.2 years follow-up [32]. Therefore, the one less fusion segment of anterior approach was the potential advantage in Lenke 5C AIS.
The advantages of the anterior approach in Lenke 5C AIS had been recorded by many scholars. Verma et al. reported that anterior instrumentation for TL/L curves of AIS obtained optimal radiographic and clinical outcomes, relatively short fusion segments [34]. Maurice et al. considered that anterior approach in lumbar curves of AIS offered extremely acceptable radiological and surgical outcomes at mid-term follow-up of 6 years [35]. Furthermore, after long-term follow-up of 17 years, Kelly et al. reported that anterior approach offered satisfactory score of the SRS and Oswestry tests, excellent functional outcomes [36]. Sudo et al. reported that the anterior approach in Lenke 5C curves offered appropriate clinical measures and radiographic outcomes with acceptable impairment of pulmonary function, after a maximum follow-up of 23 years [37].
Posterior pedicle screw system was the most prevalent operating treatment in Lenke 5C curves. A large series of 114 TL/L curves was enrolled in the research, and it concluded that the average curve correction of posterior pedicle screw system was 66 % [38]. Bennett et al. conducted a study with TL/L patients, who were taken posterior spinal fusion with 5 years follow-up, and drew a conclusion that the curve correction of coronal plane and sagittal plane was well maintained [39]. Furthermore, the finite element analysis was used to estimate possible surgical results of the anterior and posterior approach in Lenke 5 curves, and Zhang et al. found that the posterior spinal fusion was regarded as the ideal surgical procedure [40].
In this study, data of TL/L curve were available in five articles, and no significant difference was observed in the change values of TL/L curve between anterior and posterior approach (95 % CI −3.28 to 7.19, P = 0.46). Similarly, no significant difference was showed in TL/L curve correction rate of final follow-up between the two approaches (95 % CI −6.02 to 4.32, P = 0.75).
Sagittal correction attracted more and more surgeons’ attention. Previous studies compared the anterior and posterior approach for sagittal plane and still did not come to an agreement [41]. TK was the critical parameter of sagittal correction. Sucato et al. reviewed multicenter surgical database of AIS and reported that the anterior approach (n = 135) remained greater TK than posterior instrumentation [18]. Schmidt et al. included 42 thoracic lordoscoliosis patients and concluded that anterior invasive technique obtained significantly better restoration of TK than posterior spinal fusion [42]. Izatt et al. found that TK was restored at mean Cobb angle of 11.8°, 2 years after anterior approach surgery [43], while Rushton et al. prospectively compared 42 consecutive patients and reported anterior invasive technique had no overall effect of sagittal correction while posterior spinal fusion significantly reduced kyphosis [44]. In the analysis of TK, data were extracted from six studies and no significant differences were found in the change values of TK between the anterior and posterior approach (95 % CI −4.10 to 0.13, P = 0.07), from preoperation to final follow-up.
PJK was a frequent cause of reoperation, and it could be defined as pathological kyphosis deformity adjacent from the caudal endplate of the upper instrumented vertebrae to the cephalad endplate of two vertebrae proximal and might be involved with retention of proximal intervertebral elements [45]. Mendoza-Lattes et al. found that sagittal balance and TK were the predictors of PJK according to logistic regression [46]. The data of PJK were extracted from three studies. However, no significant difference was noted between the two approaches in incidence of PJK of final follow-up (95 % CI 0.12 to 7.19, P = 0.94). LL was an important component in keeping sagittal balance. Data of LL were available in six articles, and significant difference was showed in the change values of LL (95 % CI −6.06 to −0.61, P = 0.02). The posterior approach obtained a larger increasing Cobb angle of LL than the anterior approach, from preoperation to final follow-up.
Some limitations should not be ignored in this meta-analysis. First, some important comparisons to evaluate the surgical treatment of AIS were limited. Such as hospital charges, quality of life, complications, and surgical revision rates, which issues were needed to be clarified in the future studies. Second, the sample size was not large and restricted by the low rates of Lenke 5C AIS. Third, most included articles were retrospective instead of RCT studies, and the quality of included articles was lower.
Conclusions
This is the first meta-analysis comparing the two surgical approaches in Lenke 5C curves.
The anterior and posterior approach can obtain comparable coronal correction, change values of thoracic kyphosis, and incidence of proximal junctional kyphosis. The anterior approach saves approximate one more fusion segment, and the posterior approach can obtain a larger increasing Cobb angle of lumbar lordosis, from preoperation to final follow-up.
Abbreviations
AIS, adolescent idiopathic scoliosis; LL, lumbar lordosis; NOS, Newcastle-Ottawa scale; PJK, proximal junctional kyphosis; RCT, randomized controlled trial; TK, thoracic kyphosis; TL/L, thoracolumbar/lumbar
References
Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet (London, England). 2008;371(9623):1527–37.
Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-a(8):1169–81.
Dwyer AF, Schafer MF. Anterior approach to scoliosis. Results of treatment in fifty-one cases. J Bone Joint Surg Br Vol. 1974;56(2):218–24.
Luk KD, Leong JC, Reyes L, Hsu LC. The comparative results of treatment in idiopathic thoracolumbar and lumbar scoliosis using the Harrington, Dwyer, and Zielke instrumentations. Spine. 1989;14:275–80.
Wang T, Zeng B, Xu J, Chen H, Zhang T, Zhou W, Kong W, Fu Y. Radiographic evaluation of selective anterior thoracolumbar or lumbar fusion for adolescent idiopathic scoliosis. Eur Spine J. 2008;17:1012–8.
Faciszewski T, Winter RB, Lonstein JE, Denis F, Johnson L. The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1223 procedures. Spine. 1995;20:1592–9.
McDonnell MF, Glassman SD, Dimar 2nd JR, Puno RM, Johnson JR. Perioperative complications of anterior procedures on the spine. J Bone Joint Surg Am. 1996;78:839–47.
Coe JD, Arlet V, Donaldson W, Berven S, Hanson DS, Mudiyam R, Perra JH, Shaffrey CI. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine. 2006;31:345–9.
Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44-a:591–610.
Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10–23.
Ghanem IB, Hagnere F, Dubousset JF, Watier B, Skalli W, Lavaste F. Intraoperative optoelectronic analysis of three-dimensional vertebral displacement after Cotrel-Dubousset rod rotation. A preliminary report. Spine. 1997;22:1913–21.
Helenius I, Remes V, Yrjonen T, Ylikoski M, Schlenzka D, Helenius M, Poussa M. Harrington and Cotrel-Dubousset instrumentation in adolescent idiopathic scoliosis. Long-term functional and radiographic outcomes. J Bone Joint Surg Am. 2003;85-a:2303–9.
Hamill CL, Lenke LG, Bridwell KH, Chapman MP, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis. Is it warranted? Spine. 1996;21:1241–9.
Ledonio CG, Polly Jr DW, Vitale MG, Wang Q, Richards BS. Pediatric pedicle screws: comparative effectiveness and safety: a systematic literature review from the Scoliosis Research Society and the Pediatric Orthopaedic Society of North America task force. J Bone Joint Surg Am. 2011;93:1227–34.
Kamerlink JR, Quirno M, Auerbach JD, Milby AH, Windsor L, Dean L, et al. Hospital cost analysis of adolescent idiopathic scoliosis correction surgery in 125 consecutive cases. J Bone Joint Surg Am. 2010;92:1097–104.
Kuklo TR, Potter BK, Lenke LG, P. D Jr, Sides B, Bridwell KH. Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine. 2007;32(20):2258–64.
Samdani AF, Belin EJ, Bennett JT, Pahys JM, Marks MC, Miyanji F, et al. Unplanned return to the operating room in patients with adolescent idiopathic scoliosis: are we doing better with pedicle screws? Spine. 2013;38(21):1842–7.
Sucato DJ, Agrawal S, O'Brien MF, Lowe TG, Richards SB, Lenke L. Restoration of thoracic kyphosis after operative treatment of adolescent idiopathic scoliosis: a multicenter comparison of three surgical approaches. Spine. 2008;33(24):2630–6.
Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK. Proximal junctional measurement in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine. 2005;30(18):2045–50.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Hee HT, Yu ZR, Wong HK. Comparison of segmental pedicle screw instrumentation versus anterior instrumentation in adolescent idiopathic thoracolumbar and lumbar scoliosis. Spine. 2007;32(14):1533–42.
Wang Y, Fei Q, Qiu G, Lee CI, Shen J, Zhang J, et al. Anterior spinal fusion versus posterior spinal fusion for moderate lumbar/thoracolumbar adolescent idiopathic scoliosis: a prospective study. Spine. 2008;33(20):2166–72.
Li M, Ni J, Fang X, Liu H, Zhu X, He S, et al. Comparison of selective anterior versus posterior screw instrumentation in Lenke5C adolescent idiopathic scoliosis. Spine. 2009;34(11):1162–6.
Geck MJ, Rinella A, Hawthorne D, Macagno A, Koester L, Sides B, et al. Comparison of surgical treatment in Lenke 5C adolescent idiopathic scoliosis: anterior dual rod versus posterior pedicle fixation surgery: a comparison of two practices. Spine. 2009;34(18):1942–51.
Zhan SQ, Chang YB, Zeng SX, Wang YS, Ke YH, Ma YC. Comparison of surgical treatment in single thoracolumbar-lumbar adolescent idiopathic scoliosis: anterior versus posterior surgery. Zhonghua wai ke za zhi [Chinese journal of surgery]. 2010;48(6):419–22.
Eljure G, Francheri Wilson A, Noel M, et al. Proximal junctional kyphosis in Lenke 5C curves. A comparison between anterior and posterior surgery. Rev Asoc Argent Ortop Traumatol. 2014;79(1):19–26.
Dong Y, Weng X, Zhao H, Zhang J, Shen J, Qiu G. Lenke 5C curves in adolescent idiopathic scoliosis: anterior vs posterior selective fusion. Neurosurgery. 2016;78(3):324–31.
Qiu G, Wang Y, Fei Q, et al. Anterior spine fusion versus posterior spine fusion with pedical screws for lumbar and thoracolumbar AIS. Chin J Orthop. 2007;27:743–7.
Geck MJ, Rinella A, Hawthorne D, Macagno A, Koester L, Sides B, Lenke L, Bridwell K, O'Brien M, Shufflebarger HL. Anterior dual rod versus posterior pedicle fixation surgery for the surgical treatment in Lenke 5C adolescent idiopathic scoliosis: a multicenter, matched case analysis of 42 patients. Spine Deformity. 2013;1:217–22.
Helenius I, Remes V, Yrjonen T, Ylikoski M, Schlenzka D, Helenius M, et al. Comparison of long-term functional and radiologic outcomes after Harrington instrumentation and spondylodesis in adolescent idiopathic scoliosis: a review of 78 patients. Spine. 2002;27(2):176–80.
Danielsson AJ, Nachemson AL. Back pain and function 23 years after fusion for adolescent idiopathic scoliosis: a case-control study-part II. Spine. 2003;28(18):E373–83.
Sudo H, Kaneda K, Shono Y, Iwasaki N. Selection of the upper vertebra to be instrumented in the treatment of thoracolumbar and lumbar adolescent idiopathic scoliosis by anterior correction and fusion surgery using dual-rod instrumentation: a minimum 12-year follow-up study. Spine J. 2016;16(3):281–7.
Perez-Grueso FS, Fernandez-Baillo N, Arauz de Robles S, Garcia Fernandez A. The low lumbar spine below Cotrel-Dubousset instrumentation: long-term findings. Spine. 2000;25(18):2333–41.
Verma K, Auerbach JD, Kean KE, Chamas F, Vorsanger M, Lonner BS. Anterior spinal fusion for thoracolumbar scoliosis: comprehensive assessment of radiographic, clinical, and pulmonary outcomes on 2-years follow-up. J Pediatr Orthop. 2010;30:664–9.
Maurice B. Anterior instrumentation (dual screws single rod system) for the surgical treatment of idiopathic scoliosis in the lumbar area: a prospective study on 33 adolescents and young adults, based on a new system of classification. Eur Spine J. 2013;22 Suppl 2:S149–63.
Kelly DM, McCarthy RE, McCullough FL, Kelly HR. Long-term outcomes of anterior spinal fusion with instrumentation for thoracolumbar and lumbar curves in adolescent idiopathic scoliosis. Spine. 2010;35:194–8.
Sudo H, Ito M, Kaneda K, Shono Y, Abumi K. Long-term outcomes of anterior dual-rod instrumentation for thoracolumbar and lumbar curves in adolescent idiopathic scoliosis: a twelve to twenty-three-year follow-up study. J Bone Joint Surg Am. 2013;95:e49.
Lehman Jr RA, Lenke LG, Keeler KA, Kim YJ, Buchowski JM, Cheh G, Kuhns CA, Bridwell KH. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine. 2008;33:1598–604.
Bennett JT, Hoashi JS, Ames RJ, Kimball JS, Pahys JM, Samdani AF. The posterior pedicle screw construct: 5-year results for thoracolumbar and lumbar curves. J Neurosurg Spine. 2013;19:658–63.
Zhang H, Hu X, Wang Y, Yin X, Tang M, Guo C, Liu S, Wang Y, Deng A, Liu J, Wu J. Use of finite element analysis of a Lenke type 5 adolescent idiopathic scoliosis case to assess possible surgical outcomes. Comput Aided Surg. 2013;18:84–92.
Rhee JM, Bridwell KH, Won DS, Lenke LG, Chotigavanichaya C, Hanson DS. Sagittal plane analysis of adolescent idiopathic scoliosis: the effect of anterior versus posterior instrumentation. Spine. 2002;27(21):2350–6.
Schmidt C, Liljenqvist U, Lerner T, Schulte TL, Bullmann V. Sagittal balance of thoracic lordoscoliosis: anterior dual rod instrumentation versus posterior pedicle screw fixation. Eur Spine J. 2011;20(7):1118–26.
Izatt MT, Adam CJ, Verzin EJ, Labrom RD, Askin GN. CT and radiographic analysis of sagittal profile changes following thoracoscopic anterior scoliosis surgery. Scoliosis. 2012;7(1):15.
Rushton PR, Grevitt MP, Sell PJ. Anterior or posterior surgery for right thoracic adolescent idiopathic scoliosis (AIS)? A prospective cohorts’ comparison using radiologic and functional outcomes. J Spinal Disord Tech. 2015;28(3):80–8.
Cammarata M, Aubin CE, Wang X, Mac-Thiong JM. Biomechanical risk factors for proximal junctional measurement: a detailed numerical analysis of surgical instrumentation variables. Spine. 2014;39(8):E500–7.
Mendoza-Lattes S, Ries Z, Gao Y, Weinstein SL. Proximal junctional measurement in adult reconstructive spine surgery results from incomplete restoration of the lumbar lordosis relative to the magnitude of the thoracic kyphosis. Iowa Orthop J. 2011;31:199–206.
Acknowledgements
All the authors were directly involved in the whole process; therefore, it is disclosed that all the authors contributed equally towards the research. We sincerely thank Dr. Kun Wang for her guide in statistical method.
Funding
The authors declare that they have no funding.
Availability of data and material
As a meta-analysis, all raw data of this study are extracted from seven included studies. The datasets supporting the conclusions of this article are available in the seven included studies [21–27].
Authors’ contributions
LX and ML conceived the design of the study. ML, WGW, and MKS performed and collected the data and contributed to the design of the study. ML and WGW prepared and revised the manuscript. All authors read and approved the final content of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable
Ethics approval and consent to participate
Not applicable
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Luo, M., Wang, W., Shen, M. et al. Anterior versus posterior approach in Lenke 5C adolescent idiopathic scoliosis: a meta-analysis of fusion segments and radiological outcomes. J Orthop Surg Res 11, 77 (2016). https://doi.org/10.1186/s13018-016-0415-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-016-0415-9