Abstract
Background
Femoral rotational landmarks may vary according to the population. Our aim is to find out the relationship of the landmarks used in total knee arthroplasty in an Indian population and compare it with reported landmarks in other ethnic populations.
Materials and methods
We retrospectively reviewed MR images of 124 knees in 124 patients to determine the relationship of bony landmarks by measuring the condylar twist angle (CTA), Whiteside-posterior condylar angle (W-PC), and Whiteside-epicondylar angle (W-EP). The difference between the genders and the sides was analyzed.
Results
The mean CTA, W-EP and W-PC were 5.92°, 88.99° and 94.09° respectively. The mean CTA, W-EP and W-PC in males were 5.77°, 89.16° and 94.22° and they were 6.24°, 88.61° and 93.82° in females. On the left side, the CTA, W-EP and W-PC were 5.90°, 89.37° and 94.45° while they were 5.93°, 88.65° and 93.73° on the right side. There was no statistically significant difference between the genders or the sides.
Conclusion
The CTA was around 6° in our study, and the posterior condylar angle (PCA) would be 3° as the difference between them is 3°. Hence, we conclude that the conventional jigs used in the measured resection technique using 3° external rotation in reference to the posterior condyles are still an appropriate option in normal and varus knees. And there is no difference between Indians and Caucasians, but there was a significant difference with Chinese populations. Although determining rotation based on the posterior condylar axis is more practical, it is prudent to combine it with other methods.
Similar content being viewed by others
Background
Rotational mal-alignment of the femoral component in total knee arthroplasty (TKA) impacts the outcome by requiring early revision [1–3]. Correct rotational alignment is necessary for normal patellar tracking and knee stability [4, 5]. Even a minor degree (1°–4°) of internal malrotation can cause lateral tracking and tilting [6]. Excessive external rotation may lead to flexion instability [7] and mechanical overload on the medial side of the joint [8]. The commonly used anatomical landmarks in achieving correct rotational alignment of the femoral component during surgery are the posterior condylar axis [5], anteroposterior axis [9], and transepicondylar axis [10, 11].
In India, TKA is done with data which has been derived from Western studies and there could be ethnicity-based differences which have not been studied yet in detail. But studies in other ethnic groups have reported that there was a definite anatomical difference between Japanese, Chinese, and Caucasians [12–14]. We have done a MRI-based study to determine the normal values of the variables like condylar twist angle (CTA), Whiteside-epicondylar angle (W-EP), and Whiteside-posterior condylar angle (W-PC) in an Indian population. The purpose of the study was to find out the relationship of the landmarks used in TKA in an Indian population and compare it with other populations to find out the modifications required when performing total knee replacement. Our hypothesis was that rotational landmarks in the Indian population would be different from those of the Caucasian population.
Materials and methods
We retrospectively reviewed non-arthritic MR images of 124 knees of 124 patients stored in the diagnostic center system after obtaining approval from the Precision Diagnostics, India institutional review board. There were 124 patients including 86 males and 38 females, and the average age was 33.7 years (range 19 to 60 years). Our inclusion criterion was any patient who had undergone MRI for posttraumatic evaluation. Any patient with cartilage damage or any form of degenerative changes was excluded from the study.
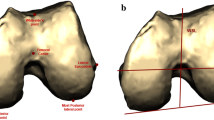
MRI was done using the following: 1.5 T units and 4000/80 (TR/TE); field of view—16 cm2; matrix—224 × 288; 5-mm slice thickness with an interslice gap of 1 mm; and excitations 2. Axial T2 FS images were used to assess the transepicondylar axis (TEA), anteroposterior axis, and posterior condylar axis (Fig. 1). The surgical TEA is drawn from the medial epicondylar sulcus to the prominent point of the lateral epicondyle. The clinical TEA was measured between the most prominent points of the medial and lateral epicondyles. The anteroposterior axis is a line drawn from the deepest part of the trochlear sulcus to the center of the intercondylar notch. The posterior condylar axis is a tangent connecting the posterior most summits of the posterior condyles.
The condylar twist angle (CTA) is the angle between the clinical transepicondylar axis and posterior condylar axis [10, 15]. The posterior condylar angle (PCA) is the angle between the surgical epicondylar axis and posterior condylar axis [10]. Both have been used in clinical studies to analyze the component rotation, but Suter et al. have proved that CTA is more reproducible than PCA in their CT-based study [16]; hence, we have used the clinical transepicondylar axis in our study. Based on these axes, the CTA, Whiteside-epicondylar angle (W-EP), and Whiteside-posterior condylar angle (W-PC) were calculated.
Measurements were done by two independent observers. The interobserver correlation coefficient was 0.5 (p = 0.001), and the intraobserver correlation coefficient was 0.64 (p = 0.032). The difference between the genders and the sides was analyzed with independent T test. A p value of <0.05 was taken to be statistically significant. Statistical analysis was done using IBM SPSS Statistics for Windows, Version 20.0, Armonk, NY: IBM Corp.
Results
The mean CTA, W-EP, and W-PC were 5.92° (SD 2.32; range 0–13), 88.99° (SD 2.86; range 81–94), and 94.09° (SD 2.84; range 86–99), respectively (Table 1). The mean CTA, W-EP, and W-PC in males were 5.77°, 89.16°, and 94.22°, respectively, and they were 6.24°, 88.61°, and 93.82° in females. On the left side, the CTA, W-EP, and W-PC were 5.90°, 89.37°, and 94.45°, respectively, while they were 5.93°, 88.65°, and 93.73°, respectively, on the right side. There is no statistically significant difference between the genders or the sides for all the parameters (Table 2).
Discussion
Correct rotational alignment of the distal femoral component is one of the determinants of good functional outcome following TKA. Excessive internal rotation results in patellar complications while excessive external rotation can cause flexion instability [4, 5]. To achieve the correct rotation, appropriate landmarks and angles should be used as they vary across populations [12, 13].
Studies determining the exact rotational position of the bony anatomy of the distal femur have usually employed three different methods. They are direct measurement with a goniometer either intraoperatively or in a cadaver and measurement using CT scan and MRI [11, 17–19]. Direct measurement is confounded by difficulty in determining the exact position of the sulcus in the medial epicondyle. During surgery, rotational alignment is measured with the cartilage in situ but many studies looking into the rotational alignment of the femoral component have employed CT scan, which does not give good assessment of the cartilage anatomy. We felt a MRI-based study would be more appropriate as the angles could vary based on the cartilage thickness [20, 21]. Moreover, during the surgery, the bony resections and component position are influenced by the cartilage thickness.
Among the epicondylar axes, the surgical epicondylar axis was proved to be representing the true rotational axis as the flexion-extension of the knee happens around this axis [22, 23]. But the medial sulcus could not be identified in nearly 50 % of the cases even on CT [15, 18]. Moreover, identifying the medial sulcus during surgery is even more challenging as it requires extensive dissection especially in an arthritic knee [14, 18]. Suter et al. have shown that the clinical epicondylar axis was more reproducible while using CT [16]. We faced the same problem of identifying the sulcus and calculating the posterior condylar angle (PCA); hence, we used the clinical epicondylar axis and measured the condylar twist angle (CTA).
In our study, the mean CTA was 5.92° (SD 2.32) with a variation of 5.78° in males and 6.24° in females. But the difference is statistically not significant. In 1987, Yoshioka et al. were the first one to describe the CTA in a cadaveric study, and the CTA was 5° and 6° in males and females, respectively [24].
Our CTA is in concurrence with most of other cadaveric studies in a Caucasian population (Table 3). The CTA reported by most of them lies between 4.4° and 6.1° [9, 10, 24–26]. But Chinese knees appear to be more externally rotated as compared to Indian knees, and their adjusted CTA would be 8.5° based on their PCA values [13].
Our result demonstrates increased CTA compared to that of Poilvache et al. (5.92° vs. 3.6°), and the difference could be possibly due to difficulty in determining the exact position of the medial sulcus intraoperatively [14]. It is less likely to represent any racial difference (Indian vs. Caucasian) as other cadaveric studies in Caucasians have shown a similar CTA.
CT-based studies (Table 3) were done in both normal and arthritic knees [27, 28]. Previous studies in Japanese knees found that there was not any significant difference in CTA between normal and arthritic varus knees [27, 28] as the posterior femoral condyles were well preserved till the end even in arthritic knees [29]. CT-based results in the Japanese population were close to our results and concur with another MRI-based study in a Japanese population as well [19].
Our CTA is slightly higher as compared to that of a previous Indian study [30], but there is no significant difference compared to other MRI-based studies (Table 3). Overall, comparing the CT- and MRI-based studies, CTA value is slightly more in MRI-based studies. This phenomenon may be due to the difference in the cartilage thickness and concurs with Tashiro et al.’s observation [20].
In a previous CT-based study by Mullaji et al. in normal Indian knees, the PCA was 5° [30] but they did not differentiate between the CTA and PCA and they suggested 2° additional of external rotation when using the posterior condyles as reference to avoid internal rotation of the femoral implant. A study by Katz et al. [26] also failed to differentiate them. There is a definite confusion in literature in differentiating the two, and we also believe that most surgeons use epicondylar prominence for component rotation which is essentially the CTA.
Measured resection is the most popular technique in India, and the conventional jigs have 3° of inbuilt external rotation. Failure to make the difference between the CTA and PCA would lead to component position in additional 3° of external rotation along with 3° inbuilt external rotation. Even though only few studies emphasized the effects of excessive external rotation, it leads to more bone resection from the medial side, medial overloading, and medial instability [2, 7, 8]. We do not have any long-term clinical studies which specifically looked at minor degrees (3°–6°) of excessive external rotation, and there is no clear cutoff value for that. Further studies are warranted to find out what constitute excessive based on ethnicity and long-term effects of minor degrees of excessive external rotation.
Yoshino et al. in their CT-based study have stated that PCA can be calculated from the condylar twist angle by subtracting 3° [18], and this view was reiterated by Akagi et al. and they proved that the relation between the CTA and PCA was a constant 3° of external rotation if the femoral valgus angle is less than 9° [15]. In that case, our PCA would be approximately 3°, which is consistent with the other studies. So, it is more appropriate to use a combination of 3° external rotation and clinical epicondylar axis.
The mean W-PC was 94.09° (externally rotated), and the mean W-EP was 88.99° (internally rotated). There was no statistically significant difference between the genders and sides. The W-PC value indicates that the component has to be 4° externally rotated to the posterior condylar axis to match the Whiteside line. Based on the W-EP values, the femoral component needs to be parallel or slightly internally rotated to the clinical epicondylar axis to align with the Whiteside line. These values are approximately close to those reported by Arima et al. and Katz et al. in which the W-PC was 93.1° (SD 1.7) and 93.4°, respectively [9, 26]. But reproducing the exact alignment during surgery is still difficult as intraoperative errors are common [31, 32]. Poilvache et al.’s intraoperative measurement in Caucasians which resulted in W-PC and W-EP of 86.92° and 90.33°, respectively, supports this [14].
The limitation of our study is that we have not measured the mechanical axis of the lower extremity. We have taken the difference of 3° between the CTA and PCA which was studied in the Caucasian population, and we have not measured the difference between the PCA and CTA in the Indian population.
The surgical epicondylar axis represents the true rotational axis of the knee; hence, determining rotation using the surgical epicondylar axis is the best method, but intraoperative errors are common as it is difficult to identify the medial sulcus in an arthritic knee. Moreover, intraoperatively, it is easy to identify the epicondylar prominences but the clinical epicondylar axis is 3° more externally rotated in relation to the surgical epicondylar axis, and failure to make this difference would lead to more external rotation (around 3°) than required. So, it is rather more practical and reproducible to use the posterior condylar axis to determine the rotation.
Conclusions
From our study, the CTA is around 6° and the PCA would be 3° as the difference between them is 3°. Hence, we conclude that the conventional jigs used in the measured resection technique using 3° external rotation in reference to the posterior condyles are still an appropriate option in normal and varus knees. And there is no difference between Indians and Caucasians, but there was a significant difference with Chinese populations. Although determining rotation based on the posterior condylar axis is more practical, it is prudent to combine it with other methods.
Abbreviations
- CTA:
-
condylar twist angle
- PCA:
-
posterior condylar angle
- TEA:
-
transepicondylar axis
- TKA:
-
total knee arthroplasty
- W-EP:
-
Whiteside-epicondylar angle
- W-PC:
-
Whiteside-posterior condylar angle
References
Incavo SJ, Wild JJ, Coughlin KM, Beynnon BD. Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res. 2007;458:131–6.
Victor J. Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res. 2009;95:365–72.
Pietsch M, Hofmann S. Early revision for isolated internal malrotation of the femoral component in total knee arthroplasty. Knee Surg Sport Traumatol Arthrosc. 2012;20:1057–63.
Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res. 1993;287:170–7.
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, et al. Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Nucl Med. 1999;366:155–63.
Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–53.
Olcott CW, Scott RD. The Ranawat Award. Femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res. 1999;367:39–42.
Hanada H, Whiteside LA, Steiger J, Dyer P, Naito M. Bone landmarks are more reliable than tensioned gaps in TKA component alignment. Clin Orthop Relat Res. 2007;462(sep):137–42.
Arima J, Whiteside LA, McCarthy DS, White SE, Missouri SL. Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee—a technical note. J bone Jt surgery(Br). 1995;77:1331–4.
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–7.
Griffin FM, Math K, Scuderi GR, Insall JN, Poilvache PL. Anatomy of the epicondyles of the distal femur—MRI analysis of normal knees. J Arthroplasty. 2000;15:354–9.
Yip DK, Zhu Y, Chiu K, Ng T. Distal rotational alignment of the Chinese femur and its relevance in total knee arthroplasty. J Arthroplasty. 2004;19:613–9.
Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G. Differences of knee anthropometry between Chinese and white men and women. J Arthroplasty. 2011;26:124–30.
Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE. Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:35–46.
Akagi M, Yamashita E, Nakagawa T, Asano T, Nakamura T: Knee alignment and reference axes in the distal femur. Clin Orthop Relat Res 2001;(388):147–156
Suter T, Zanetti M, Schmid M, Romero J. Reproducibility of measurement of femoral component rotation after total knee arthroplasty using computer tomography. J Arthroplasty. 2006;21:744–8.
Kanekasu K, Kondo M, Kadoya Y: Axial radiography of the distal femur to assess rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 2005;(434):193–197
Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty. 2001;16:493–7.
Matsuda S, Miura H, Nagamine R, Urabe K, Mawatari T, Iwamoto Y. A comparison of rotational landmarks in the distal femur and the tibial shaft. Clin Orthop Relat Res. 2003;414:183–8.
Tashiro Y, Uemura M, Matsuda S, Okazaki K, Kawahara S, Hashizume M, et al. Articular cartilage of the posterior condyle can affect rotational alignment in total knee arthroplasty. Knee Surg Sport Traumatol Arthrosc. 2012;20:1463–9.
Silva A, Pinto E, Sampaio R: Rotational alignment in patient-specific instrumentation in TKA: MRI or CT? Knee Surg Sport Traumatol Arthrosc 2014, Oct 26.:[Epub ahead of print].
Asano T, Akagi M, Nakamura T. The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: in vivo analysis using a biplanar image-matching technique. J Arthroplasty. 2005;20(8):1060–7.
Churchill D, Incavo S, Johnson C, Beynnon B. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res. 1998;356:111–8.
Yoshioka Y, Siu D, Cooke T. The anatomy and functional axes of the femur. J bone Jt surgery(Br). 1987;69:873–80.
Mantas JP, Bloebaum RD, Skedros JG, Hofmann AA. Implications of reference axes used for rotational alignment of the femoral component in primary and revision knee arthroplasty. J Arthroplasty. 1992;7:531–5.
Katz MA, Beck TD, Silber JS, Seldes RM, Lotke PA. Determining femoral rotational alignment in total knee arthroplasty. J Arthroplasty. 2001;16:301–5.
Nagamine R, Miura H, Inoue Y, Urabe K, Matsuda S, Okamoto Y, et al. Reliability of the anteroposterior axis and the posterior condylar axis for determining rotational alignment of the femoral component in total knee arthroplasty. J Orthop Sci. 1998;3(4):194–8.
Takai S, Yoshino N, Isshiki T, Hirasawa Y. Kneeling view. J Arthroplasty. 2003;18:478–83.
Matsuda S, Matsuda H, Miyagi T, Sasaki K, Iwamoto Y, Miura H. Femoral condyle geometry in the normal and varus knee. Clin Orthop Relat Res. 1998;349:183–8.
Mullaji AB, Sharma AK, Marawar SV, Kohli AF, Singh DP. Distal femoral rotational axes in Indian knees. J Orthop Surg (Hong Kong). 2009;17:166–69.
Yau WP, Chiu KY, Tang WM. How precise is the determination of rotational alignment of the femoral prosthesis in total knee arthroplasty: an in vivo study. J Arthroplasty. 2007;22:1042–8.
Yau WP, Leung A, Liu KG, Yan CH, Wong LS, Chiu KY. Errors in the identification of the transepicondylar and anteroposterior axes of the distal femur in total knee replacement using minimally-invasive and conventional approaches: a cadaver study. J Bone Joint Surg Br. 2008;90:520–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SR contributed to the study design, data collection, coordination, and preparation of the manuscript. KC contributed to the statistics and preparation of the manuscript. RS contributed to the data collection and coordination with the scan center. MKP contributed to the study design and preparation and editing of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Raju, S., Chinnakkannu, K., Sunderayan, R. et al. Rotational landmarks of the distal femur in Indian population: A MRI-based study. J Orthop Surg Res 10, 186 (2015). https://doi.org/10.1186/s13018-015-0333-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-015-0333-2




