Abstract
Background
Implant-related osteomyelitis (IRO) is recently controlled with local antibiotic delivery systems to overcome conventional therapy disadvantages. In vivo evaluation of such systems is however too little.
Questions/purposes
We asked whether vancomycin (V)-containing poly-l-lactic acid/β-tricalcium phosphate (PLLA/β-TCP) composites control experimental IRO and promote bone healing in vivo.
Methods
Fifty-six rats were distributed to five groups in this longitudinal controlled study. Experimental IRO was established at tibiae by injecting methicillin-resistant Staphylococcus aureus (MRSA) suspensions with titanium particles in 32 rats. Vancomycin-free PLLA/β-TCP composites were implanted into the normal and infected tibiae, whereas V-PLLA/β-TCP composites and coated (C)-V-PLLA/β-TCP composites were implanted into IRO sites. Sham-operated tibiae established the control group. Radiological and histological scores were quantified with microbiological findings on weeks 1 and 6.
Results
IRO is resolved in the CV- and the V-PLLA/β-TCP groups but not in the PLLA/β-TCP group. MRSA was not isolated in the CV- and the V-PLLA/β-TCP groups at all times whereas the bacteria were present in the PLLA/β-TCP group. Radiological signs secondary to infection are improved from 10.9 ± 0.9 to 3.0 ± 0.3 in the V-PLLA/β-TCP group but remained constant in the PLLA/β-TCP group. Histology scores are improved from 24.7 ± 6.5 to 17.6 ± 4.8 and from 27.6 ± 7.9 to 32.4 ± 8.9 in the CV-PLLA/β-TCP and the V-PLLA/β-TCP groups, respectively. New bone was formed in all the PLLA/β-TCP group at weeks 1 and 6.
Conclusions
CV- and V-PLLA/β-TCP composites controlled experimental IRO and promoted bone healing.
Clinical relevance
CV- and V-PLLA/β-TCP composites have the potential of controlling experimental IRO and promoting bone healing.
Similar content being viewed by others
Introduction
Implant-related osteomyelitis (IRO) [1] is a complex bone infection that requires the surgical removal of sequester or implant [2] followed with the debridement of the infected tissues [3] and high dosage antibiotic regimen for 6 weeks [4]. Staphylococcus aureus is the main causative organism for osteomyelitis [5]. It can form a biofilm, an extracellular polymeric matrix, in which cells can communicate and protect themselves from antibacterial agents [6]. Methicillin-resistant S. aureus (MRSA) is a strain of S. aureus, which mainly caused nosocomial bone infections [7]. Vancomycin is a frequently used antibiotic against infections caused by MRSA [8]. Local antibiotic delivery systems [9],[10] are proposed to control IRO safely and efficiently as parenteral administration of high doses of vancomycin for long durations may lead to some effects [11].
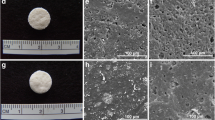
Although various degradable polymers [12],[13] and β-TCP [14] were used to release antibiotics, in vivo evaluation of these systems was rarely [15],[16] undertaken. A vancomycin-containing poly-l-lactic acid/β-tricalcium phosphate (V-PLLA/β-TCP) composite was recently developed and characterized for this reason [17]. PLLA slowed vancomycin release and β-TCP aided mesenchymal stem and Saos-2 bone cells attachment, proliferation, and differentiation in vitro[17]. This composite was further dip coated (C) with PLLA and 63.1% and 91.9% of the vancomycin released on days 1 and 42, respectively. CV- and V-PLLA/β-TCP composites furthermore generated the extracellular bone matrix and attained mineralization that may point out tissue regeneration [17]. In this study, we asked whether CV- and V-PLLA/β-TCP composites controlled experimental IRO and promoted bone healing in vivo.
Materials and methods
A longitudinal controlled study in rat tibiae was designed after ethical committee approval. Independent variables were groups (n =5) and time (n =2) and dependent variables were radiological, histological, and microbiological scores. Free online software was used to calculate the sample size of the study. The power 1-beta and type I error rate alpha were set to 0.8% and 5%, respectively. Power analysis with 56 rats revealed 0.81% confidence; therefore, minimum 10 rats were assigned into one of the five experimental groups. In the control group, the tibiae of the rats underwent sham operation without IRO establishment (n =12). PLLA/β-TCP composites were implanted into the non-infected tibiae in the second group (n =12). The PLLA/β-TCP, the V-PLLA/β-TCP, and the CV-PLLA/β-TCP composites were implanted into the IRO-established tibiae (n =12, n =10, and n =10), respectively, in the last three groups (Figure 1). We examined the groups after 1 and 6 weeks and quantified their radiological, histological, and microbiological findings.
Composites were developed and characterized as previously described [17]. Briefly, 8% vancomycin solution was prepared with 920 mg deionized water. This solution was mixed with 720 mg β-TCP and dried at 37°C for 12 h. The final mixture was added to 3% PLLA solution that contained 2.67 g chloroform and molded to obtain a spherical shape. MRSA (strain: ATCC 2592) was obtained from the microbiological collection of Ankara Numune Hospital Microbiology Laboratory. We used 3-month-old male Sprague–Dawley rats weighing 300–350 g housed in a temperature-controlled room (22°C–24°C) with 12-h light and 12-h dark cycles. Rats were given free access to water and food without antibiotics for 24 h a day. They were anesthetized by intraperitoneal 0.2 mL ketamine chloride (Ketasol 10%, Richter-Pharma, Wels, Austria) and 0.1 mL xylazine (Alfazyne 2%, Alfasan, Woerden, the Netherlands) injection. The left hind limb was shaved and cleaned with iodine solution (Polyod, Drogsan, Ankara, Turkey). The proximal anterior cortex of the tibia was exposed and drilled through with a 3.2-mm burr (Dremel, Gerlingen, Germany). We irrigated the burr hole with 0.09% sodium chloride solution (Eczacıbaşı-Baxter, Istanbul, Turkey) and injected a 0.1 mL MRSA suspension (1 × 106 CFU/cm3) into the intramedullary cavity with approximately 200 1.0 × 1.0-mm titanium particles to establish IRO in the last three groups. The burr hole was closed with bone wax (Ethicon, Johnson & Johnson, New Brunswick, NJ, USA) to prevent MRSA from leaking into the subcutaneous soft tissues. A sham operation was undertaken in the control group. Only the tibia was exposed and no other intervention was taken place. For the PLLA/β-TCP implantation, the tibiae were drilled and no MRSA suspension was given. The skin and subcutaneous tissues were sutured with 2.0 silk (Doğsan, Trabzon, Turkey), and closure was cleaned and sprayed with an antibacterial film (Opsite, Smith & Nephew, London, England) [18]. Rats were put into cages allowing their free movement and fed with regular diet. Anterior-posterior and lateral radiographs of the tibia were obtained after 3 weeks in the IRO groups using the Siemens Multix-C (Siemens AG, Erlangen, Germany) X-ray device at a setting of 46 kV and 2.5 mAs/s to confirm radiological signs of IRO establishment. The distance between the X-ray source and the samples was 100.0 cm at examination. Agfa Crurix X-ray films (Agfa, Mortsel, Belgium) and the Crurix 60 (Agfa, Mortsel, Belgium) automatic developing machine were used. When macroscopic and radiologic signs of IRO became definite, all closures were reopened and only one composite implanted into the burr hole was found in the tibia based on its group. After 1 and 6 weeks, radiographs were obtained and two orthopedic surgeons who had no prior information of the groups independently evaluated the radiographs for the presence of IRO. Radiologic criteria were: (1) periosteal reaction, (2) diaphyseal widening, (3) osteolysis, (4) bone deformation, (5) sequestrum formation, (6) joint effusion, and (7) soft tissue swelling. Parameters 1 to 4 were graded as (0) absent, (1) mild, (2) moderate, and (3) severe, and parameters 5 to 7 were graded as (0) absent and (1) present [19]. Swab cultures were obtained for microbiological analysis. A sterile stripe was smeared into the implantation site to take culture. The stripes were streaked onto blood agar plates and incubated at 37°C for 12 h and the presence or absence of growth in the media was recorded. The animals were sacrificed by lethal doses of anesthetics and tibiae of the left hind leg were dissected. All soft tissues were removed and bones were fixed in 10% phosphate buffered formalin (pH 7.0) at room temperature for histological analysis at termination. Samples were then decalcified by immersion in De Castro solution [nitric acid (Merck, Darmstadt, Germany), chloral hydrate (Merck, Darmstadt, Germany), and distilled water] for 5–10 days before dehydration. Tibiae were rinsed in buffer and dehydrated in a graded series of ethanol before embedding in paraffin in an automated tissue processor (TP-1020, Leica, Wetzlar, Germany). For each tibia, we determined the severity of infection with 60–80 5-μm-thick hematoxylin and eosin and trichrome-stained serial sections using a DMR 6000 microscope equipped with the DC500 digital camera (Leica, Wetzlar, Germany). Semi-quantitative image analysis was undertaken using the Qwin Plus computer image analysis system (Leica, Wetzlar, Germany). The medullar cavity (leukocytes, microabscesses, granulation tissue, fibrosis), cortex (destruction of the cortex, enlarged Haversian canals, leukocytes, microabscesses, granulation tissue, fibrosis), and periosteal reaction (quantity) were scored according to the literature [according to severity as none, slight, moderate, or much from 0 to 4] in at least ten regions of interest [20]. The total score was calculated and noted for the statistical analysis.
Descriptive values are expressed as the minimum, the maximum, and the median. As all the scores for the control group were zero, this group was taken off from statistical analysis. Normality of distribution and homogeneity of variances were adjusted using the Shapiro-Wilk test. Radiological and the histological scores were analyzed by nonparametric tests (Kruskal-Wallis for multiple comparison and Mann Whitney U as post hoc test with Bonferroni correction; p <0.0083 was considered significant.). Spearman’s test was used to assess correlations between continuous radiology and histology variables. The Pearson product–moment correlation coefficient test was used for the interobserver and intraobserver reliabilities.
Each author certifies that Hacettepe University Animal Care and Use Ethics Committee approved (no. 2007/65-1) the animal protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Results
MRSA did not grow in the CV- and V-PLLA/β-TCP groups at any time. MRSA and Escherichia coli were isolated from four and two of six, and from three and three of six tibiae in the PLLA/β-TCP group at week 1 and 6, respectively. Radiological score of the V-PLLA/β-TCP group improved (p =0.043) at week 6 (Figure 2). Interobserver and intraobserver reliabilities (r) for the presence or absence of infection were 0.95 and 0.98, respectively. The radiographic scores correlated with histological scores at weeks 1 (r =0.896; p <0.05) and 6 (r =0.90; p <0.05). Microbiological and radiological scores from this in vivo study suggest that IRO was controlled in the CV- and V-PLLA/β-TCP groups but not in the PLLA/β-TCP group.
PLLA/β-TCP composites implanted into normal bone without IRO presented healthy cortical osteons and minimal or no periosteal reaction histologically, receiving better scores than the other groups at week 1 (Figure 3). PLLA/β-TCP composites with IRO exhibited cortical bone damage with enlarged Haversian canals and granulation tissue formation. Mononuclear cells infiltrated the medullary canal in the same group. Broad periosteal reaction at weeks 1 and 6 were observed in the PLLA/β-TCP groups with IRO. The CV-PLLA/β-TCP group had comparatively better (p =0.004) histological scores compared with that of the PLLA/β-TCP group at week 6 (Figure 4).
The descriptive data of histological scores of the groups are shown for weeks 1 and 6: (minimum, maximum, and median values). PLLA/β-TCP without IRO exhibited better scores than the other groups at weeks 1 and 6. V-PLLA/β-TCP and CV-PLLA/β-TCP presented better scores compared with that of PLLA/β-TCP with IRO at week 6. Note that p <0.0083 for a-b, a-c, a-d, e-f, e-g, e-h.
Histological images (A-E). PLLA/β-TCP without IRO group had a mild tissue reaction in (A) week 1 with HE (B) and week 6 with MT. The implant is degrading but still present at 6 weeks. PLLA/β-TCP with IRO group had evident bone damage and granulation tissue formation with mononuclear cell infiltration and periosteal reaction in (C) week 1 with MT and (D) week 6 with HE, respectively. V-PLLA/β-TCP had better morphologic features of the bone and marrow in (E) week 1 with HE with the presence of new forming healthy spongy bone. CT connective tissue, TB trabecular bone, CB compact bone, BM bone marrow, GT granulation tissue, I implant, HE hematoxylin and eosin, MT Masson’s trichrome.
Discussion
Staphylococcal bacteria have adhesion potential to biomaterials [21] resulting in chronic osteomyelitis and IRO [6]. This bone infection can be controlled with local drug delivery systems. CV- and V-PLLA/β-TCP composites can be a choice since remission of IRO was achieved with these implants. This study had some limitations. E. coli was isolated in three PLLA/β-TCP composites, which indicated surgical site contamination. Complex bacterial contamination is a frequent state in osteomyelitis due to the open wounds and/or multiple surgeries [22]; however, CV- and V-PLLA/β-TCP composites were able to overcome this complication. In vivo degradation time and reduction of mechanical strength of our material were not measured, as eradication of MRSA was our primary aim.
Microbiologic findings revealed control of the infection in the CV- and V-PLLA/β-TCP groups. Bacteria did not grow in these groups at any time. Radiological scores correlated well with histological scores and improvement was achieved in the CV- and V-PLLA/β-TCP groups. These findings were in line with previous studies [23],[24]. The radiologic score of the PLLA/β-TCP group without IRO group deteriorated slightly at week 6 most probably due to composite degradation [25]. A decrease in pH owing to PLLA degradation could have caused bone resorption [26] in this group. Histological findings of the CV- and V-PLLA/β-TCP groups presented favorable biocompatibility. TCP is an osteoconductive material [27] and influences bone ingrowth in the pores of the composite. This finding was in line with another study [16] that demonstrated new trabecular bone formation at the defect margins in biodegradable TCP composites. Quantitative histology revealed biocompatibility and osteointegration as in another study [28].
Conclusion
In conclusion, vancomycin-containing PLLA/β-TCP composites presented favorable radiological, histological, and microbiological results of remission and according to clinical relevance of the study, they can be used to control IRO in the near future.
Authors’ contributions
BK and FK carried out the in vivo studies, and drafted the manuscript. PK and EB carried out the histology studies. BK, FK, and PK participated in the design of the study and BK, PK, and EB performed the statistical analysis. All authors read and approved the final manuscript.
References
Ozturan KE, Yucel I, Kocoglu E, Cakici H, Guven M: Efficacy of moxifloxacin compared to teicoplanin in the treatment of implant-related chronic osteomyelitis in rats. J Orthop Res. 2010, 28 (10): 1368-1372. 10.1002/jor.21159.
Zimmerli W: Infection and musculoskeletal conditions: prosthetic-joint-associated infections. Best Pract Res Clin Rheumatol. 2006, 20 (6): 1045-1063. 10.1016/j.berh.2006.08.003.
Orhan Z, Cevher E, Yıldız A, Ahıskalı R, Sensoy D, Mülazımoğlu L: Biodegradable microspherical implants containing teicoplanin for the treatment of methicillin-resistant Staphylococcus aureus osteomyelitis. Arch Orthop Trauma Surg. 2010, 130: 135-142. 10.1007/s00402-009-0886-9.
Jiang JL, Li YF, Fang TL, Zhou J, Li XL, Wang YC, Dong J: Vancomycin-loaded nano-hydroxyapatite pellets to treat MRSA-induced chronic osteomyelitis with bone defect in rabbits. Inflamm Res. 2012, 61 (3): 207-215. 10.1007/s00011-011-0402-x.
Li D, Gromov K, Søballe K, Puzas JE, O’Keefe RJ, Awad H, Drissi H, Schwarz EM: Quantitative mouse model of implant-associated osteomyelitis and the kinetics of microbial growth, osteolysis, and humoral immunity. J Orthop Res. 2008, 26 (1): 96-105. 10.1002/jor.20452.
Lew DP, Waldvogel FA: Osteomyelitis. Lancet. 2004, 364: 369-379. 10.1016/S0140-6736(04)16727-5.
Yin LY, Calhoun JH, Thomas JK, Shapiro S, Schmitt-Hoffmann A: Efficacies of ceftobiprole medocaril and comparators in a rabbit model of osteomyelitis due to methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2008, 52 (5): 1618-1622. 10.1128/AAC.00638-07.
Fang T, Wen J, Zhou J, Shao Z, Dong J: Poly (ε-caprolactone) coating delays vancomycin delivery from porous chitosan/β-tricalcium phosphate composites. J Biomed Mater Res B Appl Biomater. 2012, 100 (7): 1803-1811. 10.1002/jbm.b.32747.
Makarov C, Berdicevsky I, Raz-Pasteur A, Gotman I:In vitro antimicrobial activity of vancomycin-eluting bioresorbable β-TCP-polylactic acid nanocomposite material for load-bearing bone repair. J Mater Sci Mater Med. 2013, 24 (3): 679-687. 10.1007/s10856-012-4832-y.
Park PI, Makoid M, Jonnalagadda S: The design of flexible ciprofloxacin-loaded PLGA implants using a reversed phase separation/coacervation method. Eur J Pharm Biopharm. 2011, 77 (2): 233-239. 10.1016/j.ejpb.2010.11.014.
Petrone C, Hall G, Langman M, Filiaggi MJ: Compaction strategies for modifying the drug delivery capabilities of gelled calcium polyphosphate matrices. Acta Biomater. 2008, 4 (2): 403-413. 10.1016/j.actbio.2007.09.007.
Ahola N, Männistö N, Veiranto M, Karp M, Rich J, Efimov A, Seppälä J, Kellomäki M: An in vitro study of composites of poly (L-lactide-co-ε-caprolactone), β-tricalcium phosphate and ciprofloxacin intended for local treatment of osteomyelitis. Biomatter. 2013, 3 (2): 1-13. 10.4161/biom.23162.
Korkusuz F, Korkusuz P, Ekşioğlu F, Gürsel İ, Hasırcı V:In vivo response to biodegradable controlled antibiotic release systems. J Biomed Mater Res. 2001, 55: 217-228. 10.1002/1097-4636(200105)55:2<217::AID-JBM1008>3.0.CO;2-Y.
Gbureck U, Vorndran E, Barralet JE: Modeling vancomycin release kinetics from microporous calcium phosphate ceramics comparing static and dynamic immersion conditions. Acta Biomater. 2008, 4: 1480-1486. 10.1016/j.actbio.2008.02.027.
Miyai T, Ito A, Tamazawa G, Matsuno T, Sogo Y, Nakamura C, Yamazaki A, Satoh T: Antibiotic-loaded poly-ε-caprolactone and porous β-tricalcium phosphate composite for treating osteomyelitis. Biomaterials. 2008, 29: 350-358. 10.1016/j.biomaterials.2007.09.040.
Luginbuehl V, Ruffieux K, Hess C, Reichardt D, von Rechenberg B, Nuss K: Controlled release of tetracycline from biodegradable β-tricalcium phosphate composites. J Biomed Mater Res B Appl Biomater. 2010, 92B: 341-352.
Kankilic B, Bayramli E, Kilic E, Dağdeviren S, Korkusuz F: Vancomycin containing PLLA/β-TCP controls MRSA in vitro. Clin Ortop Relat Res. 2011, 469: 3222-3228. 10.1007/s11999-011-2082-9.
Korkusuz F, Uchida A, Shinto Y, Inoue K, Ono K: Biomaterial centered chronic osteomyelitis. Turk J Med Res. 1992, 10: 268-292.
Aktekin CN, Ozturk AM, Tabak AY, Altay M, Korkusuz F: A different perspective for radiological evaluation of experimental osteomyelitis. Skeletal Radiol. 2007, 36: 945-950. 10.1007/s00256-007-0342-2.
Petty W, Spanier S, Shuster JJ, Silverthorne C: The influence of skeletal implants on incidence of infection: experiment in a canine model. J Bone Joint Surg Am. 1985, 67: 1236-1244.
Lawson MC, Hoth KC, Deforest CA, Bowman CN, Anseth KS: Inhibition of Staphylococcus epidermidis biofilms using polymerizable vancomycin derivatives. Clin Orthop Relat Res. 2010, 468 (8): 2081-2091. 10.1007/s11999-010-1266-z.
Klemm K: The use of antibiotic-containing bead chains in the treatment of chronic bone infections. Clin Microbiol Infect. 2001, 7: 28-31. 10.1046/j.1469-0691.2001.00186.x.
Ozturk AM, Tabak AY, Aktekin CN, Altay M, Erdemli E, Karahuseyinoglu S, Korkusuz F: Alendronate enhances antibiotic-impregnated bone grafts in the treatment of osteomyelitis. Int Orthop. 2008, 32: 821-827. 10.1007/s00264-007-0396-8.
Lucke M, Schmidmaier G, Sadoni S, Wildemann B, Schiller R, Haas NP: Gentamicin coating of metallic implants reduces implant-related osteomyelitis in rats. Bone. 2003, 32 (5): 521-531. 10.1016/S8756-3282(03)00050-4.
Pihlajamäki H, Böstman O, Tynninen O, Laitinen O: Long-term tissue response to bioabsorbable poly-l-lactide and metallic screws: an experimental study. Bone. 2006, 39: 932-937. 10.1016/j.bone.2006.04.009.
Cao L, Duan PG, Wang HR, Li XL, Yuan FL, Fan ZY, Li SM, Dong J: Degradation and osteogenic potential of a novel poly (lactic acid)/nano-sized β-tricalcium phosphate scaffold. Int J Nanomedicine. 2012, 7: 5881-5888. 10.2147/IJN.S38127.
Soundrapandian C, Sa B, Datta S: Organic-inorganic composites for bone drug delivery. AAPS PharmSciTech. 2009, 10 (4): 1158-1171. 10.1208/s12249-009-9308-0.
Baro M, Sanchez E, Delgado A, Perera A, Evora C:In vitro-in vivo characterization of gentamicin bone implants. J Control Release. 2002, 83: 353-364. 10.1016/S0168-3659(02)00179-7.
Acknowledgments
We thank Muharrem Timuçin and Nursen Koç of the Middle East Technical University, Department of Metallurgical and Material Engineering, Ankara, Turkey who produced and provided the β-TCP. We thank Erdal Bayramlı of the Middle East Technical University, Department of Chemistry for his help in producing composites. We also thank Akif Muhtar Öztürk MD and Alparslan Şenköylü MD of the Gazi University, Faculty of Medicine, Department of Orthopaedics and Traumatology, Ankara, Turkey for independently scoring the radiographs. Sezin Dagdeviren of the Middle East Technical University, Department of Biotechnology assisted the surgeries. Çagla Köprü of the Hacettepe University Institute of Pure and Applied Sciences, Nanotechnology and Nanomedicine Division helped at the preparation and evaluation of histological specimens. A part of this project was supported by the Ministry of Science, Industry and Technology of Turkey, San-Tez Research Grant 00817.STZ.2011-01.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kankilic, B., Bilgic, E., Korkusuz, P. et al. Vancomycin containing PLLA/β-TCP controls experimental osteomyelitis in vivo. J Orthop Surg Res 9, 114 (2014). https://doi.org/10.1186/s13018-014-0114-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-014-0114-3