Abstract
Background
Resuscitative endovascular balloon occlusion of the aorta (REBOA) has been used to control massive hemorrhages. Although there is no consensus on the efficacy of REBOA, it remains an option as a bridging therapy in non-trauma centers where trauma surgeons are not available. To better understand the current landscape of REBOA application, we examined changes in its usage, target population, and treatment outcomes in Japan, where immediate hemostasis procedures sometimes cannot be performed.
Methods
This retrospective observational study used the Japan Trauma Data Bank data. All cases in which REBOA was performed between January 2004 and December 2021 were included. The primary outcome was the in-hospital mortality rate. We analyzed mortality trends over time according to the number of cases, number of centers, severity of injury, and overall and subgroup mortality associated with REBOA usage. We performed a logistic analysis of mortality trends over time, adjusting for probability of survival based on the trauma and injury severity score.
Results
Overall, 2557 patients were treated with REBOA and were deemed eligible for inclusion. The median age of the participants was 55 years, and male patients constituted 65.3% of the study population. Blunt trauma accounted for approximately 93.0% of the cases. The number of cases and facilities that used REBOA increased until 2019. While the injury severity score and revised trauma score did not change throughout the observation period, the hospital mortality rate decreased from 91.3 to 50.9%. The REBOA group without severe head or spine injuries showed greater improvement in mortality than the all-patient group using REBOA and all-trauma patient group. The greatest improvement in mortality was observed in patients with systolic blood pressure ≥ 80 mmHg. The adjusted odds ratios for hospital mortality steadily declined, even after adjusting for the probability of survival.
Conclusions
While there was no significant change in patient severity, mortality of patients treated with REBOA decreased over time. Further research is required to determine the reasons for these improvements in trauma care.
Similar content being viewed by others
Background
Hemorrhage is one of the primary causes of mortality in trauma cases and accounts for an estimated 30–40% of traumatic deaths [1]. Resuscitation of massive hemorrhages often requires massive transfusions and fluids, and rapid hemorrhage control is essential. Traditionally, aortic cross-clamping (ACC) has been used to temporarily control massive hemorrhage. However, ACC adds further invasiveness to a patient who has already sustained severe trauma, and managing bleeding from the incision site poses additional challenges [2]. Resuscitative endovascular balloon occlusion of the aorta (REBOA) has emerged as an alternative approach for controlling hemorrhages with minimal invasion [3]. However, its effectiveness is controversial. Some studies have shown that compared to ACC, REBOA has a better prognosis [2, 4], while others suggested that it is associated with a poorer prognosis [5,6,7]. Recently, a randomized trial conducted in major trauma centers in the United Kingdom suggested that REBOA increased the risk of death and prolonged the time to definitive hemostasis [7]. However, REBOA remains an option as a bridging therapy in non-trauma centers where trauma surgeons are not always available.
The situation surrounding REBOA is progressing without sufficient evidence. Off-the-job training courses for REBOA have been conducted worldwide, and devices have been improved, including the release of a narrower-diameter access route [8, 9], based on theoretical benefits. However, the validation of these efforts is insufficient. To better understand the current situation surrounding REBOA, we examined changes in its usage, target population, and treatment outcomes in Japan, where immediate hemostasis procedures sometimes cannot be performed.
Methods
Study design and settings
This retrospective observational study used data from the Japan Trauma Data Bank. The study was conducted from January 2004 to December 2021. The JTDB is required to register all severe trauma cases with AIS 3 or higher injuries and was established by the Japanese Association for Acute Medicine and Japanese Association for The Surgery of Trauma to understand the current status and improve the quality of trauma care, akin to the Trauma Quality Improvement Program in the United States. By the end of December 2021, the JTDB included 303 facilities providing trauma care in Japan, of which 95% were government-certified tertiary care centers.
In Japan, trauma patients are usually transported by ambulance staffed with paramedics, although physician-staffed ground or air ambulance is dispatched to the field in some cases. However, REBOA is rarely performed in pre-hospital settings and is often performed after arrival at the emergency department. Moreover, blood transfusion is rarely performed in pre-hospital settings.
This study complied with the principles of the 1964 Declaration of Helsinki and its amendments and was approved by the Ethics Committee of Tsuchiura Kyodo General Hospital (approval number: 2022FY10). The requirement for informed consent from each patient was waived because of the study’s retrospective nature. We used the opt-out method, which provides opportunities to refuse to participate in the study through online information disclosure in our hospital. The study was conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting statement.
Study participants
The study included all cases for which REBOA was used between 2004 and 2021.
Measurements
We collected the following patient information from the JTDB: age; sex; year of injury; trauma classification (blunt or penetrating); pre-hospital vital signs [systolic blood pressure (SBP), heart rate (HR), respiratory rate (RR), and percutaneous oxygen saturation (SpO2)]; Glasgow coma scale (GCS) score; time from emergency medical service dispatch to emergency department (ED) arrival; vital signs at ED arrival [SBP, HR, RR, and SpO2, body temperature, and GCS, abbreviated injury scale (AIS) score for each region, injury severity score (ISS), revised trauma score (RTS), status at hospital discharge (survival or death)]; lactic acid level; focused assessment with sonography in trauma (FAST) results; number of REBOA cases, cases of cardiac arrest on arrival, and ACC cases; and probability of survival based on the trauma and injury severity score (TRISS-Ps).
Definitions and outcomes
The AIS was calculated based on AIS 98 until 2018 and AIS 2008 after 2019 in accordance with the change in JTDB registration rule. Data for pre-hospital GCS score, SpO2, and lactic acid levels on ED arrival were only available after 2019 in the JTDB. Cardiac arrest was characterized by a recorded SBP of 0 mmHg based on the registration instructions of the JTDB. The primary outcome was survival at hospital discharge.
Statistical analysis
The trend of the number, characteristics, and outcomes of patients treated with REBOA and the number of facilities where REBOA was used, according to admission year, was described. Trends in hospital mortality were also compared among specific subgroups, including all patients with trauma, patients treated with REBOA, patients treated with REBOA without severe head or spine injuries defined by AIS ≥ 3, patients treated with REBOA with shock upon hospital arrival (SBP < 80 mmHg), and patients treated with REBOA without shock upon hospital arrival.
Patient characteristics were described using median and interquartile range (IQR) for continuous variables and number and percentage (%) for categorical variables. The chi-square test was used with a significance level of 0.05 to test the association of variables. We conducted a single regression analysis to show the changes in annual mortality rates across some subgroups: all patients with trauma in the database, all cases in which REBOA was used, the REBOA group without severe head or spine injury of AIS ≥ 3, cases with SBP < 80 mmHg among patients for whom REBOA was used, and patients with SBP ≥ 80 mmHg among patients for whom REBOA was used. We conducted a logistic regression analysis for the annual mortality rate adjusted by TRISS-Ps. All statistical analyses were performed using R software version 4.3.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
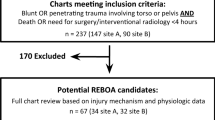
A total of 427,561 patients were registered with the JTDB between 2004 and 2021. Of them, 2557 patients were treated with REBOA and were deemed eligible for inclusion. Table 1 presents the baseline patient characteristics. Overall, the median age of the participants was 55 years, with male patients constituting 65.3% of the study population. Blunt trauma accounted for approximately 93.0% of the cases. The median transport time was 37 min. The median SBP at ED arrival was 70 mm Hg. The thoracic region had the highest median AIS score. FAST-positive cases accounted for 45.9% of the cases. The median ISS and RTS values were 34.0 and 4.7, respectively. The median TRISS-Ps was 0.35. The overall mortality rate was 59.7%, and 16.9% of the patients experienced cardiac arrest upon arrival. ACC was performed in 16.7% of the cases. The number of REBOA cases was 24 in 2004, which increased to 262 in 2019. The number of REBOA cases declined from 2020 to 167 by 2021. The in-hospital mortality rate decreased from 91.3 to 50.9% during the observation period.
The number of facilities using REBOA in 2004 increased from 10 to 105 in 2019. The number of facilities using REBOA has decreased since 2020, reaching 62 by 2021 (Fig. 1). Although RTS changed substantially from 2004 to 2006, the median and IQR for both RTS (Fig. 2) and ISS (Fig. 3) were similar after these periods.
Univariate regression analysis was conducted in various subgroups to compare the trends in mortality rates (Fig. 4). The REBOA group without severe head or spine injury of AIS ≥ 3 had greater improvement in mortality than that of all-patient group using REBOA and all-trauma patient group. The greatest improvement in mortality was observed in patients with SBP ≥ 80 mmHg among all patients for whom REBOA was performed.
Mortality rate in subgroups and overall trauma over time. Single regression analysis was conducted in various subgroups to compare the trends in mortality rates. The black line shows the REBOA group without severe head or spine injury of AIS ≥ 3. The red lines show the cases in which REBOA was used. The blue line indicates trauma cases in the database. The purple line shows cases with SBP < 80 mmHg among those where REBOA was used. The green line shows cases with SBP ≥ 80 mmHg among cases where REBOA was used. Abbreviations REBOA, resuscitative endovascular balloon of the aorta; AIS, Abbreviated injury scale; SBP, systolic blood pressure
Logistic regression analysis for the outcome of annual mortality indicated steadily declined mortality even after adjusting for TRISS-Ps (Fig. 5).
Discussion
A retrospective observational study analyzing data from the Japanese nationwide trauma registry over the past 18 years was conducted on 2,557 patients who underwent REBOA. A consistently decreasing trend in mortality was observed. The physiological and anatomical severities of the patients were similar over the years, and a reduction in mortality was observed, regardless of the severity of their conditions.
Several previous studies evaluated the mortality rate associated with REBOA, ranging from 34 to 70.8% [10,11,12,13]. Aoki et al. showed that the mortality rate of patients undergoing REBOA decreased between 2004 and 2015 [14]. Our study further enriched these results by adding 6 years of data, demonstrating changes over time in the number of cases in which REBOA was used, number of facilities using REBOA, and analysis of specific subgroups. The results of the present study revealed that mortality continued improving after 2016. The increase in the use of REBOA and the number of facilities implementing it until 2019 may be attributed to the growing recognition of the procedure. The introduction of hybrid emergency room system in Japan in 2011 partially could have contributed to this trend [15, 16].
Furthermore, 7 Fr narrow-diameter balloons were approved for clinical use in 2013. They were shown to reduce complications related to REBOA [17], including lower extremity ischemia. This technical progress in REBOA may have resulted in its increased number of REBOA uses. The decrease in the number of patients and facilities after 2020 could be attributed to the COVID-19 pandemic. Given that the RTS and ISS remained similar over the years, it was suggested that the indications for REBOA were consistent over 18 years.
While trauma-related mortality has decreased over the years [18], the mortality rate of patients treated with REBOA was further reduced compared to that of the all-trauma cohort [18]. There are several possible explanations for this. It is possible that the REBOA insertion technique has been partially improved by disseminating off-the-job REBOA training courses in Japan [8, 19]. Among the cases of REBOA, a significant reduction in mortality was observed in patients with an SBP of 80 mmHg or higher, indicating that REBOA had a particularly significant effect on improving outcomes in bleeding patients with relatively stable conditions. The UK-REBOA randomized clinical trial suggested that there may be more deaths in the REBOA group, which may have been influenced by the longer time to hemostasis in the REBOA group. Furthermore, the improvement in the mortality rate of patients without severe head or spine trauma was lower than that of patients treated with REBOA. These findings indicate that the progress in the hemostatic strategy, including damage control resuscitation, contributed to the favorable outcome of the patients who underwent REBOA.
This study has some limitations. Because this was retrospective registry-based study, some important information was missing, namely when, where, and how REBOA was performed. Since information on changes in vital signs after arrival at hospital was not available, the patients’ condition just before REBOA was unclear. The zone, extent, duration of the REBOA inflation, and the method used to confirm the placement of the REBOA catheter was unclear. The expertise level of the individual performing REBOA was unknown. Detailed information on the preparation and operation of hemostatic procedures, such as the availability of trauma surgeons and operating theaters at each facility, is unavailable in the JTDB.
Conclusions
While there was no significant change in patient severity, mortality of patients treated with REBOA decreased over time. Further research is required to determine the reasons for these improvements in trauma care.
Data availability
The data that supported the findings of this study are available from the Japan Trauma Data Bank, but the availability of these data is restricted.
Abbreviations
- REBOA:
-
Resuscitative endovascular balloon occlusion of the aorta
- ACC:
-
aortic cross-clamping
- SBP:
-
systolic blood pressure
- HR:
-
heart rate
- RR:
-
respiratory rate
- SpO2:
-
percutaneous oxygen saturation
- GCS:
-
Glasgow coma scale
- ED:
-
emergency department
- AIS:
-
abbreviated injury scale
- ISS:
-
injury severity score
- RTS:
-
revised trauma score
- FAST:
-
focused assessment with sonography in trauma
- TRISS-Ps:
-
trauma and injury severity score
- IQR:
-
interquartile range; percentage, %
References
Perkins JG, Cap AP, Weiss BM, Reid TJ, Bolan CD. Massive transfusion and nonsurgical hemostatic agents. Crit Care Med. 2008;36(7). https://doi.org/10.1097/CCM.0b013e31817e2ec5. ;Suppl:S325–39.
Haruta K, Endo A, Shiraishi A, Otomo Y. Usefulness of resuscitative endovascular balloon occlusion of the aorta compared to aortic cross-clamping in severely injured trauma patients: analysis from the Japan Trauma Data Bank. Acute Med Surg. 2023;10:e830. https://doi.org/10.1002/ams2.830.
DuBose JJ, Scalea TM, Brenner M, Skiada D, Inaba K, Cannon J, et al. The AAST prospective aortic occlusion for resuscitation in Trauma and Acute Care surgery (AORTA) registry: data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). J Trauma Acute Care Surg. 2016;81:409–19. https://doi.org/10.1097/TA.0000000000001079.
Cralley AL, Vigneshwar N, Moore EE, Dubose J, Brenner ML, Sauaia A, et al. Zone 1 endovascular balloon occlusion of the aorta vs resuscitative thoracotomy for patient resuscitation after severe hemorrhagic shock. JAMA Surg. 2023;158:140–50. https://doi.org/10.1001/jamasurg.2022.6393.
Kinslow K, Shepherd A, McKenney M, Elkbuli A. Resuscitative endovascular balloon occlusion of aorta: a systematic review. Am Surg. 2022;88:289–96. https://doi.org/10.1177/0003134820972985.
Joseph B, Zeeshan M, Sakran JV, Hamidi M, Kulvatunyou N, Khan M, et al. Nationwide analysis of resuscitative endovascular balloon occlusion of the aorta in civilian trauma. JAMA Surg. 2019;154:500–8. https://doi.org/10.1001/jamasurg.2019.0096.
Jansen JO, Hudson J, Cochran C, MacLennan G, Lendrum R, Sadek S, et al. Emergency department resuscitative endovascular balloon occlusion of the aorta in trauma patients with exsanguinating hemorrhage: the UK-REBOA randomized clinical trial. JAMA. 2023;330:1862–71. https://doi.org/10.1001/jama.2023.20850.
Birrenbach T, Wespi R, Hautz WE, Berger J, Schwab PR, Papagiannakis G, et al. Development and usability testing of a fully immersive VR simulation for REBOA training. Int J Emerg Med. 2023;16:67. https://doi.org/10.1186/s12245-023-00545-6.
Sykes AG, Sisson WB, Wang LJ, Martin MJ, Thangarajah H, Naheedy J, et al. Balloons for kids: anatomic candidacy and optimal catheter size for pediatric resuscitative endovascular balloon occlusion of the aorta. J Trauma Acute Care Surg. 2022;92:743–7. https://doi.org/10.1097/TA.0000000000003521.
Gupta BK, Khaneja SC, Flores L, Eastlick L, Longmore W, Shaftan GW. The role of intra-aortic balloon occlusion in penetrating abdominal trauma. J Trauma. 1989;29:861–5. https://doi.org/10.1097/00005373-198906000-00026.
Saito N, Matsumoto H, Yagi T, Hara Y, Hayashida K, Motomura T, et al. Evaluation of the safety and feasibility of resuscitative endovascular balloon occlusion of the aorta. J Trauma Acute Care Surg. 2015;78:897–903. https://doi.org/10.1097/TA.0000000000000614. discussion 4.
Irahara T, Sato N, Moroe Y, Fukuda R, Iwai Y, Unemoto K. Retrospective study of the effectiveness of Intra-aortic Balloon Occlusion (IABO) for traumatic haemorrhagic shock. World J Emerg Surg. 2015;10:1. https://doi.org/10.1186/1749-7922-10-1.
Moore LJ, Brenner M, Kozar RA, Pasley J, Wade CE, Baraniuk MS, et al. Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage. J Trauma Acute Care Surg. 2015;79:523–30. https://doi.org/10.1097/TA.0000000000000809. discussion 30–2.
Aoki M, Abe T, Hagiwara S, Saitoh D, Oshima K. Resuscitative endovascular balloon occlusion of the aorta may contribute to improved survival. Scand J Trauma Resusc Emerg Med. 2020;28:62. https://doi.org/10.1186/s13049-020-00757-2.
Watanabe H, Shimojo Y, Hira E, Kuramoto S, Muronoi T, Oka K, et al. First establishment of a new table-rotated-type hybrid emergency room system. Scand J Trauma Resusc Emerg Med. 2018;26:80. https://doi.org/10.1186/s13049-018-0532-z.
Kinoshita T, Yamakawa K, Matsuda H, Yoshikawa Y, Wada D, Hamasaki T, et al. The survival benefit of a novel trauma workflow that includes immediate whole-body computed tomography, surgery, and interventional radiology, all in one trauma resuscitation room: a retrospective historical control study. Ann Surg. 2019;269:370–6. https://doi.org/10.1097/SLA.0000000000002527.
Teeter WA, Matsumoto J, Idoguchi K, Kon Y, Orita T, Funabiki T, et al. Smaller introducer sheaths for REBOA may be associated with fewer complications. J Trauma Acute Care Surg. 2016;81:1039–45. https://doi.org/10.1097/TA.0000000000001143.
Endo A, Shiraishi A, Matsui H, Hondo K, Otomo Y. Assessment of progress in early trauma care in Japan over the past decade: achievements and areas for future improvement. J Am Coll Surg. 2017;224:191–e1985. https://doi.org/10.1016/j.jamcollsurg.2016.10.051.
Thabouillot O, Boddaert G, Travers S, Dubecq C, Derkenne C, Kedzierewicz R, et al. Effectiveness of short training in resuscitative endovascular balloon occlusion of the aorta (REBOA) by emergency physicians: the applied course for internal aortic clamping on field mission. J Spec Oper Med. 2021;21:36–40. https://doi.org/10.55460/NYAW-F69L.
Acknowledgements
The authors would like to thank Editage (www.editage.com) for the English language editing.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
H.H. drafted and revised the manuscript, developed the study concept and design and was involved in statistical analysis and data interpretation. H.H. also takes responsibility for the research, final approval, and study supervision. A.E. assisted in manuscript revision, study concept and design development, and data interpretation and assumed responsibility for research conduct and final approval. R.Y., K.Y., K.S., and T.A. were involved in data acquisition and manuscript revision and accepted responsibility for the research conduct and final approval. K.M. contributed to manuscript revision and data interpretation and took responsibility for conducting the research and obtaining final approval. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Tsuchiura Kyodo General Hospital (approval number: 2022FY10). The requirement for informed consent from each patient was waived because of the study’s retrospective nature. We used the opt-out method, which provides opportunities to refuse to participate in the study through online information disclosure in our hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hoshi, H., Endo, A., Yamamoto, R. et al. Use of resuscitative endovascular balloon occlusion of the aorta (REBOA) for trauma and its performance in Japan over the past 18 years: a nationwide descriptive study. World J Emerg Surg 19, 19 (2024). https://doi.org/10.1186/s13017-024-00548-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-024-00548-5