Abstract
Background
Tourniquets (TQ) have been increasingly adopted in pre-hospital settings recently. This study examined the effectiveness and safety of applying TQ in the pre-hospital settings for civilian patients with traumatic vascular injuries to the extremities.
Materials and methods
We systematically searched the Ovid Embase, PubMed, and Cochrane Central Register of Controlled Trials databases from their inception to June 2023. We compared pre-hospital TQ (PH-TQ) use to no PH-TQ, defined as a TQ applied after hospital arrival or no TQ use at all, for civilian vascular extremity trauma patients. The primary outcome was overall mortality rate, and the secondary outcomes were blood product use and hospital stay. We analyzed TQ-related complications as safety outcomes. We tried to include randomized controlled trials (RCTs) and non-randomized studies (including non-RCTs, interrupted time series, controlled before-and-after studies, cohort studies, and case-control studies), if available. Pooled odds ratios (ORs) were calculated and the certainty of evidence was assessed using Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology.
Results
Seven studies involving 4,095 patients were included. In the primary outcome, pre-hospital TQ (PH-TQ) use significantly decrease mortality rate in patients with extremity trauma (odds ratio [OR], 0.48, 95% confidence interval [CI] 0.27–0.86, I2 = 47%). Moreover, the use of PH-TQ showed the decreasing trend of utilization of blood products, such as packed red blood cells (mean difference [MD]: -2.1 [unit], 95% CI: -5.0 to 0.8, I2 = 99%) or fresh frozen plasma (MD: -1.0 [unit], 95% CI: -4.0 to 2.0, I2 = 98%); however, both are not statistically significant. No significant differences were observed in the lengths of hospital and intensive care unit stays. For the safety outcomes, PH-TQ use did not significantly increase risk of amputation (OR: 0.85, 95% CI: 0.43 to 1.68, I2 = 60%) or compartment syndrome (OR: 0.94, 95% CI: 0.37 to 2.35, I2 = 0%). The certainty of the evidence was very low across all outcomes.
Conclusion
The current data suggest that, in the pre-hospital settings, PH-TQ use for civilian patients with vascular traumatic injury of the extremities decreased mortality and tended to decrease blood transfusions. This did not increase the risk of amputation or compartment syndrome significantly.
Similar content being viewed by others
Background
In emergency situations, tourniquets (TQ) are used to control severe bleeding by applying pressure on a limb or body part to restrict blood flow to the area. However, while it is useful intervention for controlling extremity hemorrhage [1,2,3], prolonged application poses inherent risks of complications [4, 5]. In the past, TQs were primarily utilized in military settings; however, recently, this intervention has been increasingly adopted in civilian settings [6,7,8].
The latest United States national guidelines for field triage of injured patients incorporate the identification of active bleeding, referring TQ as one of the criteria for recognizing a high risk of serious injury [9]. Surgical intervention is commonly indicated for patients who require TQs, and a higher mortality rate is observed in cases where timely TQ placement is not implemented [10]. However, only a few studies have investigated the efficacy of TQs in civilian settings. In military environments, where immediate life-saving measures are often crucial and medical resources may be limited, TQs are more readily employed as first-line interventions for severe extremity bleeding. In contrast, healthcare providers in civilian settings may have a more nuanced approach, aiming to balance the need for hemorrhage control with the potential risks and associated complications. In addition, the threshold for TQ use in civilian settings may be influenced by local protocols and the expertise of the healthcare providers involved. Several studies have not reported survival benefits associated with the use of pre-hospital TQs [11,12,13]. Therefore, we aimed to perform a systematic review to investigate the effectiveness of pre-hospital TQ application in patients with traumatic vascular injuries of the extremities.
Materials and methods
Eligibility criteria and outcome measures
This systematic review was conducted and reported in accordance with the checklist of PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [14]. We included studies that examined the impact of pre-hospital TQ (PH-TQ) utilization on survival outcomes in patients with vascular extremity injuries caused by trauma in a civilian setting. PH-TQ refer to pneumatic or mechanical TQ applied to patients before hospital arrival, while no PH-TQ use was defined as a TQ applied after hospital arrival (late TQ) or no TQ use at all.
The study types included randomized controlled trials (RCTs) and non-randomized studies, which comprised non-RCTs, interrupted time series, controlled before-and-after studies, cohort studies, and case-control studies. Unpublished studies, including conference abstracts or articles, letters, editorials, comments, and case reports, were excluded. In this review, the primary outcome was overall mortality, and the secondary outcomes were the volume of infused blood components and possible TQ-related complications. The study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) in 2023 (CRD42023448057).
Information sources and search strategy
We searched studies in PubMed, Ovid EMBASE, and the Cochrane Central Register of Controlled Trials (CENTRAL). The detailed search strategy is shown in the Supplementary Materials (Supplementary 1). Our search strategy included all years since database inception and all languages, provided that an English-language abstract is available. The final date of this study was set as June 30, 2023. The reference lists of identified studies were checked for additional relevant articles.
Study selection
Following the removal of duplicates, titles were independently screened by the reviewers (YCK and TYT), and irrelevant results were removed. The process was followed by title and abstract screening, and a full-text assessment was conducted if the article was deemed potentially relevant. Additional reviewers (MJH and TPL) were invited and a discussion was initiated to reach a consensus regarding any concerns encountered during the selection process.
Data collection process, data items, and quality assessment
After the final set of included articles was determined, a spreadsheet specifically adapted for this review was created to record the data extracted from the articles. The spreadsheet consisted of various details, including author(s), publication year, country, study design, participant characteristics, intervention type, and key outcomes. The risk of bias in individual studies was independently reviewed by two authors (YCK and KWL). The RoB 2 tool was planned to be used to assess the quality of randomized controlled studies and the ROBINS-I tool for nonrandomized controlled studies [15, 16]. The certainty of evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology [17].
Data synthesis and analysis
The treatment effects for dichotomized outcomes were evaluated using the odds ratio (OR); continuous outcomes were summarized as the mean difference (MD). Zero-count cells in the dichotomized outcomes were handled using the Yate’s correction approach, which added 0.5 to the cells containing 0 (zero events) [18]. Meta-analyses were conducted to combine the outcome data, and the weighted means of the ORs and their corresponding 95% confidence intervals (CIs) were calculated using random effects models (DerSimonian-Laird method) [19]. Sensitivity analysis for primary outcome was conducted by performing a meta-analysis using data from nonrandomized studies with adjusted ORs. To clarify the impact of using PH-TQ on secondary outcomes and to understand whether reducing heterogeneity among studies would affect the research findings, another sensitivity analysis using data from studies comparing PH-TQ use and no TQ use was also conducted. For the article providing median and interquartile range (IQR), the mean and standard deviation (SD) was converted using the formula: mean ≈ median, and SD ≈ IQR / 1.35. To assess the statistical heterogeneity across studies, we calculated I2 statistics, with I2 > 50%, assuming the presence of significant heterogeneity [20, 21]. The analyses were performed using R (version 4.3.0; R Foundation for Statistical Computing, Vienna, Austria), and the meta-analysis was performed using the meta package. A p-value < 0.05 was considered statistically significant.
Result
Search results, study characteristics, and quality assessment
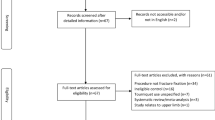
A flow diagram of the included studies is shown in Fig. 1. After the literature search, 691 records were identified. A total of 109 duplicates and 554 irrelevant articles, were removed after screening the titles and abstracts, resulting to 28 reports for full-text review that were considered potentially relevant. Overall, 7 articles met the inclusion criteria and were included in our study [8, 10,11,12,13, 22, 23]. All studies included in our analysis were nonrandomized cohort studies conducted in the North America between 2014 and 2022, comprising six studies from the United States [8, 10,11,12,13, 23] and one study from Canada [22]. The reasons for the exclusion of studies were as follows: no comparison group (n = 14); for military purpose (n = 3); lacks outcome of interest (n = 2); and no related intervention (n = 2).
The study characteristics are summarized in Table 1. The analyzed studies involved 4,095 patients, of whom 1,692 and 2,403 received and did not receive PH-TQ, respectively. The studies compared the effect of PH-TQ, with no TQ in five studies [8, 11, 13, 22, 23]; PH-TQ vs. late-TQ in one study [10]; and PH-TQ vs. (late-TQ + no-TQ) in one study [12]. The study participants were mostly males with an average age < 45 years. The participant characteristics in each study are shown in Supplementary 2. All analyzed studies provided crude numbers of mortality, whereas only four [8, 11, 13, 23] controlled for confounders using matching or regression approaches. Three types of blood products were analyzed for infusion: packed red blood cells (pRBCs), platelets, and plasma. Blood transfusion in the first 24 h was reported in five studies [8, 11, 12, 22, 23], blood transfusion in the first hour was reported in one study [10], and the total amount of blood products required in another study [13]. All the analyzed studies documented various side effects following TQ use. These included amputation in all studies [8, 10,11,12,13, 22, 23], compartment syndrome in four [10, 11, 13, 22], thromboembolic complication in two [13, 23], nerve palsy in two [12, 13], and infection in two [13, 23]. Individual studies have reported other complications in the pulmonary, cardiac, musculoskeletal, and renal system [11, 13, 23]. The outcomes and potential complications associated with TQ use reported in each study are shown in Supplementary 3. The overall risk of bias varied from moderate to critical, and most of the included studies were subject to a serious to critical risk of bias owing to the risk of confounding factors. The results of the risk of bias assessment are shown in Fig. 2.
Quantitative synthesis
The results are summarized in Fig. 3, and detailed information on each outcome is provided in the Supplementary Appendix. For the primary outcome, the pooled results demonstrated applying PH-TQ (compared to those who did not receive PH-TQ) was associated with a significantly lower mortality rate (OR, 0.48; 95% CI 0.27–0.86; I2, 47%) (Fig. 3 and Supplementary 4). In the sensitivity analysis of primary outcome, the results remained statistically significant when using only adjusted outcomes in four studies (aOR, 0.34, 95% CI 0.19–0.59, I2, 0%) (Supplementary 5). For secondary outcomes, the use of PH-TQ is not associated with reduced use of blood products such as pRBC (MD, -2.09 [unit]; 95% CI -5.00–0.82, I2, 99%) or FFP (MD, -1.0 [unit]; 95% CI -4.0–2.0; I2, 98%) (Fig. 3, Supplementary 6–7) No significant difference was observed regarding the length of hospital stay (MD, -0.80 [day]; 95% CI -2.90–1.30, I2, 66%) or intensive care unit length of stay (MD, -0.51 [day]; 95% CI -2.08–1.06; I2, 92%) (Fig. 3, Supplementary 8–9).
For the safety outcomes, the use of PH-TQ is not associated with increased amputation (OR, 0.85; 95% CI 0.43–1.68; I2, 60%) and compartment syndrome (OR, 0.94; 95% CI, 0.37–2.35; I2, 0%) (Fig. 3, Supplementary 10–11). The sensitivity analysis utilizing data from studies comparing PH-TQ use and no TQ use revealed that, despite a reduction in heterogeneity among studies, the utilization of PH-TQ is not significantly associated with secondary outcomes, including safety outcomes (Supplementary 12–17). The funnel plot, which exhibit asymmetry, is shown in Supplementary 18. Because of the limited number of studies included (n < 10), the Egger’s test was not performed. The certainty of evidence (CoE) using the GRADE method for the treatment recommendations of individual endpoints is summarized in Table 2. The CoE was downgraded by domains in the risk of bias and inconsistency owing to the high proportion of studies with a serious risk of bias and high heterogeneity across studies. An asymmetric funnel plot for mortality outcomes was observed. Although only seven studies were included in the review, the publication bias domain was downgraded as concerns arose. In summary, the overall CoE showed very low quality of evidence across all reported endpoints.
Discussion
This systematic review identified seven cohort studies investigating the benefits of PH-TQ use in patients with vascular extremity injuries and demonstrated that early placement of TQ in the pre-hospital setting may confer a survival benefit for patients with vascular injuries in the extremities. The analysis did not reveal any significant differences in the transfusion of blood products, ICU and hospital lengths of stay, or the occurrence of potential complications associated with the intervention. Substantial heterogeneity was noted across the pooled effect estimates.
A previous meta-analysis conducted by Latina et al., which included four articles comparing the clinical effectiveness of pneumatic or mechanical tourniquets, did not find conclusive evidence regarding the impact of emergency PH-TQ placement on overall mortality and utilization of blood products [24]. Moreover, three included studies reported adjusted results on overall mortality [11, 13, 23]. Only two studies employing case-control matching of participants were included in the meta-analysis [11, 13], and one study was excluded because of unclear reporting of the effect estimate [23]. For comparison, the meta-analysis in our study was conducted using ORs as the effect measures. Although not all crude data were provided in a case-control manner, we assumed that the severity of the intervention group would not be less serious than that of the control group. In the sensitivity analysis, four of seven included studies that provided adjusted ORs (aOR) were used for the meta-analysis. The result was away from null, and the heterogeneity statistic I2 decreased from 47 to 0%, as we estimated the effect. Furthermore, our study used patients who did not receive PH-TQ, including no TQ application and hospital TQ application, as our control group, which was different from the previous study. We pooled the controls because vascular extremity trauma cases are regarded as time-sensitive [25] and adverse outcomes might occur when the intervention is delayed, possibly even when it is administered upon arrival at hospitals [10]. For component therapy, the heterogeneity across the studies was high, and different variable measurements (e.g., blood products needed in the first hour and first day, or the total amount of blood products needed), were reported. Our study did not identify any supporting evidence indicating that the use of PH-TQs led to a reduction in the need for blood product transfusion. Each study identified in the systematic review reported different TQ-related adverse events. However, the diagnosis of complications has not been clearly reported across studies, making comparisons difficult. Although some of the included studies utilized various statistical methods to address confounding factors, most of them were subject to serious or critical risks, and co-intervention in addition to TQ use may have led to bias. The inherent limitations associated with the retrospective cohort study design may constrain the interpretation of the present meta-analytical findings, highlighting the need for a well-designed clinical trial of better quality.
The utilization of PH-TQ varies within each emergency medical service (EMS) system and its use is influenced by local protocols. A previous study conducted in the United States reported an estimated incidence of 0.2 PH-TQ applications per 1000 EMS activations [7], and this trend was increasing, especially in urban areas [6]. However, although the idea of using TQ is becoming more prevalent in specific communities, we should be aware that the procedure may result in complications and that not every TQ is being used properly [26]. Extremity injuries encompass a wide spectrum ranging from severe deformities to subtle injuries that can be challenging to diagnose. Based on limited experience in using PH-TQ, the importance of adequate training for healthcare providers or first responders and more consistent protocols cannot be overemphasized. Furthermore, in trauma cases, time plays a critical role because the timing of interventions and treatments can substantially influence patient outcomes. It is crucial for practitioners not only to possess the skills and knowledge to correctly apply TQ but also recognize the importance of swiftly using them.
The adverse events reported in the included studies did not show a significant increase in complications related to the use of TQs, and none of the studies reported a direct association with the interventions. Adverse events may have contributed to the injury itself rather than the use of TQs. The severity of injuries tended to be lower in civilian settings than in military settings [27]. It was anticipated that pre-hospital stays for civilians would be shorter and that the likelihood of complications resulting from prolonged TQ application would be reduced. However, both civilian and military settings were composed mostly of young male-injured individuals; the potential complications to the older population or special population needed to be deliberate, considering that these populations are prone to cardiovascular or other adverse events.
Our review has several limitations. First, we included only a limited number of available studies, and no RCTs were identified. This limitation may have affected the overall strength of the evidence and ability to draw solid conclusions. However, it is not possible to perform RCTs in the real-world. To avoid confounding factors, we performed a sensitivity analysis using aORs and led to the same conclusion. Furthermore, cases of TQ application may be deemed more serious, and the efficacy might be underestimated, as all of the reported aORs in the included studies consistently deviated significantly from the null value. Second, we did not compare our method with other hemostasis methods such as manual arterial compression, hemostatic agents, or other hemostatic medical devices. Future studies should incorporate comparative analyses to provide a more comprehensive evaluation of the effectiveness of an intervention. In addition to hemostatic devices, comprehensive approaches for managing traumatic injuries are required. Third, the study did not incorporate time-related factors, such as the time of injury, time to arrival at the hospital, or time to tourniquet application. Time plays a crucial role in trauma cases because the timing of interventions and treatments can significantly affect patient outcomes. Hence, a standardized trauma registry should be established. In addition to data collection and longitudinal follow-up, the registry can serve as a tool for quality improvement initiatives, strengthening each component of acute care for trauma cases.
Conclusion
The meta-analysis revealed that early placement of a TQ in the pre-hospital setting may provide a survival advantage for patients with vascular injuries in the extremities and decrease the use of blood products. There was no increase in the risk of amputation or compartment syndrome. Further large-scale prospective studies are needed to verify these findings.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Beekley AC, Sebesta JA, Blackbourne LH, et al. Prehospital tourniquet use in Operation Iraqi Freedom: Effect on hemorrhage control and outcomes. J Trauma. 2008;64:28–S37. discussion S37.
Kotwal RS, Montgomery HR, Kotwal BM, et al. Eliminating preventable death on the battlefield. Arch Surg. 2011;146:1350–8.
Kragh JF Jr., Walters TJ, Baer DG, et al. Practical use of emergency tourniquets to stop bleeding in major limb trauma. J Trauma. 2008;64:38–S49. discussion S49–50.
Inaba K, Siboni S, Resnick S, et al. Tourniquet use for civilian extremity trauma. J Trauma Acute Care Surg. 2015;79:232–7. ;quiz 332.
Pillgram-Larsen J, Mellesmo S. [Not a tourniquet, but compressive dressing. Experience from 68 traumatic amputations after injuries from mines]. Tidsskr nor Laegeforen. 1992;112:2188–90.
BenÍtez CY, Ottolino P, Pereira BM, et al. Tourniquet use for civilian extremity hemorrhage: systematic review of the literature. Rev Col Bras Cir. 2021;48:e20202783.
El Sayed MJ, Tamim H, Mailhac A, Mann NC. Trends and predictors of limb tourniquet use by civilian emergency medical services in the United States. Prehosp Emerg Care. 2017;21:54–62.
Henry R, Matsushima K, Ghafil C, et al. Increased use of prehospital tourniquet and patient survival: Los Angeles countywide study. J Am Coll Surg. 2021;233:233–239e2.
Newgard CD, Fischer PE, Gestring M, et al. National guideline for the field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2021. J Trauma Acute Care Surg. 2022;93:e49–e60.
Scerbo MH, Holcomb JB, Taub E, et al. The trauma center is too late: major limb trauma without a pre-hospital tourniquet has increased death from hemorrhagic shock. J Trauma Acute Care Surg. 2017;83:1165–72.
McNickle AG, Fraser DR, Chestovich PJ, et al. Effect of prehospital tourniquets on resuscitation in extremity arterial trauma. Trauma Surg Acute Care Open. 2019;4:e000267.
Schroll R, Smith A, Alabaster K, et al. AAST multicenter prospective analysis of prehospital tourniquet use for extremity trauma. J Trauma Acute Care Surg. 2022;92:997–1004.
Smith AA, Ochoa JE, Wong S, et al. Prehospital tourniquet use in penetrating extremity trauma: decreased blood transfusions and limb complications. J Trauma Acute Care Surg. 2019;86:43–51.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Sterne JA, Hernán MA, Reeves BC, et al. Robins-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
The Cochrane Collaboration. Cochrane handbook for systematic reviews of interventions. Oxford: The Cochrane Collaboration; 2005.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Ioannidis JP, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007;335:914–6.
Passos E, Dingley B, Smith A, et al. Tourniquet use for peripheral vascular injuries in the civilian setting. Injury. 2014;45:573–7.
Teixeira PGR, Brown CVR, Emigh B, et al. Civilian prehospital tourniquet use is associated with improved survival in patients with peripheral vascular injury. J Am Coll Surg. 2018;226:769–76. e1 e761.
Latina R, Iacorossi L, Fauci AJ, et al. Effectiveness of pre-hospital tourniquet in emergency patients with major trauma and uncontrolled haemorrhage: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18:12861.
Newton EJ, Love J. Acute complications of extremity trauma. Emerg Med Clin North Am. 2007;25:751–61.
Duignan KM, Lamb LC, DiFiori MM, et al. Tourniquet use in the prehospital setting: are they being used appropriately? Am J Disaster Med. 2018;13:37–43.
Schroll R, Smith A, McSwain NE Jr., et al. A multi-institutional analysis of prehospital tourniquet use. J Trauma Acute Care Surg. 2015;79:10–4. discussion 14.
Acknowledgements
The authors acknowledge the assistance provided by Hsin-Ping Chiu, librarian of the National Taiwan University Medical Library, for building up the search strategy.
Funding
This study was supported by the National Taiwan University Cancer Center (NTUCCS-112-12) and Taiwan National Science and Technology Council (112-2314-B-002-222). This funding source had no role in the design of this study and had no role during its execution, analyses, interpretation of the data, or decision to submit results.
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to the design and conception of the study. Y.C.K. and T.Y.T. contributed to data acquisition. Y.C.K., T.Y.T., C.K.W. and W.C.C. analyzed the data. K.W.L., M.J.H., T.P.L. and T.M. contributed to data interpretation. Y.C.K., M.J.H. and M.H.M. drafted the article.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
13017_2024_536_MOESM1_ESM.pdf
Supplementary Material 1: Supplementary 1. Search strategy. Supplementary 2. Characteristics of participants in included studies. Supplementary 3. Outcomes and potential complications related to tourniquet use in included studies. Supplementary 4. Forest plot of overall mortality of pre-hospital tourniquets vs. no pre-hospital tourniquets. Supplementary 5. Sensitivity analysis for overall mortality of pre-hospital tourniquets versus no pre-hospital tourniquets. Supplementary 6. Forest plot of mean difference in red blood cell transfusion of prehospital tourniquets vs. no pre-hospital tourniquets. Supplementary 7. Forest plot of mean difference in fresh frozen plasma transfusion of pre-hospital tourniquets vs. no pre-hospital tourniquets. Supplementary 8. Forest plot of mean difference in length of hospital stay of prehospital tourniquets vs. no pre-hospital tourniquets. Supplementary 9. Forest plot of mean difference in intensive care unit length of stay with pre-hospital tourniquets vs. no pre-hospital tourniquets. Supplementary 10. Forest plot of amputation with pre-hospital tourniquet vs. no prehospital tourniquet. Supplementary 11. Forest plot of compartment syndrome in the pre-hospital tourniquet vs. no pre-hospital tourniquet group. Supplementary 12. Funnel plot for the included studies
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ko, YC., Tsai, TY., Wu, CK. et al. Effectiveness and safety of tourniquet utilization for civilian vascular extremity trauma in the pre-hospital settings: a systematic review and meta-analysis. World J Emerg Surg 19, 10 (2024). https://doi.org/10.1186/s13017-024-00536-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-024-00536-9