Abstract
Background
Using self-expanding metal stents (SEMS) and decompression tubes (DT) as a bridge-to-surgery (BTS) treatment may avoid emergency operations for patients with colorectal cancer-caused obstructions. This study aimed to evaluate the efficacy and safety of the two approaches.
Methods
We systematically retrieved literature from January 1, 2000, to May 30, 2023, from the PubMed, Embase, Web of Science, SinoMed, Wanfang Data, Chinese National Knowledge Infrastructure, and Cochrane Central Register of Clinical Trials databases. Randomized controlled trials (RCTs) or cohort studies of SEMS versus DT as BTS in colorectal cancer obstruction were selected. Risks of bias were assessed for RCTs and cohort studies using the Cochrane Risk of Bias tool version 2 and Risk of Bias in Nonrandomized Studies of Interventions. Certainty of evidence was determined using the Graded Recommendation Assessment. Odds ratio (OR), mean difference (MD), and 95% confidence interval (95% CI) were used to analyze measurement data.
Results
We included eight RCTs and eighteen cohort studies involving 2,061 patients (SEMS, 1,044; DT, 1,017). Pooled RCT and cohort data indicated the SEMS group had a significantly higher clinical success rate than the DT group (OR = 1.99, 95% CI 1.04, 3.81, P = 0.04), but no significant difference regarding technical success (OR = 1.29, 95% CI 0.56, 2.96, P = 0.55). SEMS had a shorter postoperative length of hospital stays (MD = − 4.47, 95% CI − 6.26, − 2.69, P < 0.00001), a lower rates of operation-related abdominal pain (OR = 0.16, 95% CI 0.05, 0.50, P = 0.002), intraoperative bleeding (MD = − 37.67, 95% CI − 62.73, − 12.60, P = 0.003), stoma creation (OR = 0.41, 95% CI 0.23, 0.73, P = 0.002) and long-term tumor recurrence rate than DT (OR = 0.47, 95% CI 0.22, 0.99, P = 0.05).
Conclusion
SEMS and DT are both safe as BTS to avoid emergency surgery for patients with colorectal cancer obstruction. SEMS is preferable because of higher clinical success rates, lower rates of operation-related abdominal pain, intraoperative bleeding, stoma creation, and long-term tumor recurrence, as well as a shorter postoperative length of hospital stays.
Trial registration CRD42022365951.
Similar content being viewed by others
Background
According to the latest global cancer burden data released by the International Agency for Research on Cancer of the World Health Organization in 2020, incidence of colorectal cancer ranks third in terms of incidence among all cancers, accounting for approximately 10% of new cancer cases globally. Moreover, it has escalated to the second leading cause of cancer-related deaths worldwide, accounting for approximately 9.4% of all cancer-related deaths [1]. Obstruction is one of the most common complications of colorectal cancer, with a prevalence as high as 29%. It also constitutes a significant percentage of emergency department admissions, as this critical condition often requires emergency interventions [2]. Recent studies have shown an alarmingly high postoperative mortality rate among patients with obstruction caused by colorectal cancer, with a 30-day mortality rate exceeding 50% [3, 4]. Additionally, the risk of perioperative morbidity is increased by the generally poor systemic condition of patients, e.g., electrolyte and acid base imbalances, intestinal congestion and edema [5]. Consequently, any surgical approach to treating these patients may significantly increase the risk of mortality, as well as escalate hospitalization costs and prolong the recovery [6].
In recent years, the endoscopic placement of self-expanding metal stents (SEMS) and decompression tubes (DT) has emerged as a bridge to surgery (BTS), allowing for the rapid relief of obstruction symptoms in patients and avoiding emergency surgery. This approach creates conditions for radical resection, thus improving the overall survival rate of patients. In 1991, Dohmoto et al. [7] first reported the use of endoscopically placed SEMS as a palliative treatment for rectal and sigmoid colon cancers. With the advancement of endoscopic techniques, SEMS can also be used as a transitional tool before radical colorectal cancer resection. Several studies have reported the role of SEMS in relieving obstruction due to colorectal cancer [8,9,10,11]. SEMS not only reduces the stoma rate and length of postoperative hospital stay but also decreases the mortality rate in patients with colorectal cancer obstruction [12]. The European Society of Gastrointestinal Endoscopy (ESGE) and the American Society for Gastrointestinal Endoscopy recommend SEMS as an option for palliation and relief of malignant bowel obstruction [13, 14]. The ESGE suggests that SEMS can be used as an alternative to emergency surgery for potentially curable colorectal cancer obstruction.
In 1940, Abbott et al. [15] developed DT, which alleviates intestinal obstruction by repeatedly flushing the intestinal lumen upon reaching the site of obstruction. Studies have demonstrated the safety and efficacy of DT [16,17,18,19]. Prior to the healthcare policy reforms in Japan, DT was often the preferred treatment modality for malignant colonic obstruction [20].
Both endoscopically placed SEMS and DT have high technical and clinical success rates [21, 22]. However, the differential effects of SEMS and DT in patients with colorectal cancer obstruction remain controversial. This study aimed to evaluate the effectiveness and safety of SEMS and DT as BTS in relieving colorectal cancer obstruction, as well as to compare the short- and long-term outcomes of subsequent radical resection.
Methods
This systematic evaluation adheres to the guidelines outlined by Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), and our research plan has been registered with PROSPERO (CRD42022365951).
Search strategy
The literature search was conducted independently by two researchers (WM and J-CZ) using the following databases: PubMed, Embase, Web of Science, SinoMed, Wanfang Data, Chinese National Knowledge Infrastructure, and the Cochrane Central Register of Clinical Trials. The search covered the period from January 1, 2000, to May 1, 2023. The inclusion criteria for the literature were studies published in English or Chinese. The search terms were combined using Boolean logic and connected with "AND/OR" and the search strategies of the mentioned databases can be found in Additional file 1: Table S1.
Inclusion and exclusion criteria
After importing all the retrieved literature into a reference management software, duplicate articles were removed. Subsequently, two independent researchers (WM and J-CZ) reviewed the titles and abstracts of the remaining articles based on the basis of the inclusion and exclusion criteria to identify potentially relevant studies. The inclusion criteria consisted of the following: (1) randomized controlled trials (RCTs) and cohort studies; (2) participants diagnosed with obstruction caused by colorectal cancer confirmed by abdominal computed tomography (CT) or endoscopic biopsy; (3) interventions involving SEMS and DT; and (4) studies providing relevant indicators, including (a) operation-related outcomes such as technical success, clinical success, and operation-related complications; (b) surgery-related outcomes such as intraoperative bleeding, stoma rate, length of hospital stay, and surgery-related complications; and (c) long-term outcomes such as survival, tumor recurrence, and tumor metastasis. Exclusion criteria included the following: (1) case reports, systematic reviews, and meta-analyses; (2) interventions other than SEMS or DT; and (3) studies lacking the reporting of the aforementioned relevant indicators. When the reviewers disagreed regarding the inclusion of an article, its full text was read to discuss its inclusion. If a consensus could not be reached between the two researchers, the final decision was made by a third researcher (HJ) of the review team.
Outcome definition
Technical success was defined as the achievement of instrument placement. Clinical success was defined as the resolution of obstructive symptoms. Other outcomes were defined in accordance with the respective definitions of each included study.
Data extraction
Two independent researchers (WM and J-CZ) assessed the eligibility of selected articles and extracted the following information: study characteristics (first author’s name, publication year, country, and study design), patient characteristics (age, sex sample size, clinical stage, tumor location, and device type), operation-related outcomes (technical success, clinical success, and operation-related complications), surgery-related outcomes (intraoperative bleeding, stoma rate, length of hospital stay, and surgery-related complications), and long-term outcomes (survival, tumor recurrence, and tumor metastasis rate). To minimize data entry errors, all data were entered by the two independent researchers and checked by a third researcher (HJ), with any discrepancies resolved through discussion.
Assessment of risk of bias
Two independent researchers (J-CZ and KL) independently assessed the risk of bias in the included studies. The risk of bias assessment for RCTs was conducted using the Cochrane Risk of Bias tool version 2 (RoB 2), which evaluates six domains of bias: (1) randomization process, (2) deviations from intended interventions, (3) missing outcome data, (4) measurement of outcomes, (5) selection of reported results, and (6) overall bias [23]. Risk Of Bias in Non-randomized Studies—of Interventions (ROBINS-I), a tool for evaluating the risk of bias in cohort studies [24], includes seven domains: (1) bias due to confounding, (2) bias in participant selection, (3) bias in classification of interventions, (4) bias due to deviations from intended interventions, (5) bias due to missing data, (6) bias in measurements of outcomes, and (7) bias in selection of the reported results. Any discrepancies between the two researchers were resolved by a third researcher (HJ).
Certainty of evidence
The certainty of the evidence was evaluated by two independent researchers (J-CZ and KL) using the Graded Recommendations Assessment, Development, and Evaluation (GRADE) through the GRADE Pro online website tool [25, 26]. We assessed the quality of the evidence and the confidence in the effect estimates based on study design, risk of bias, inconsistency, indirectness, imprecision, and risk of publication bias. For each outcome, the overall quality of the evidence was described as "high," "moderate," "low," or "very low." Any discrepancies between the two researchers were resolved by a third researcher (HJ).
Statistical analysis
Methods for assessing heterogeneity in included studies comprised visual inspection and statistical tests. When heterogeneity was absent, a fixed effect model was applied to pool data. If the heterogeneity existed, then a random effect model was applied. Visual inspection often employed a forest plot, where an elevated level of homogeneity could be inferred if the confidence intervals (CIs) overlapped and there were no apparent outliers in the point estimates. Statistical tests, such as the Q test and I2 statistic, were also utilized. An I2 value ≥ 75% indicates high heterogeneity among the included studies, 50% ≤ I2 < 75% suggests moderate heterogeneity, and 25% ≤ I2 < 50% indicates low heterogeneity [27]. For indicators with > ten articles, a funnel plot was utilized to evaluate publication bias in the included literature.
When the outcome measures were binary variables, the effect size was evaluated using odds ratios (ORs) and their corresponding 95% CIs. For continuous numerical variables, the effect size was assessed using mean differences (MDs) and their corresponding 95% CIs. If the data were reported in formats other than the mean and standard deviation (e.g., in the case of median and range), we applied the method developed by Hozo et al. [28] to transform them. The statistical significance of the pooled effect size was determined using the Z-test. Unless stated otherwise, a P-value < 0.05 was considered statistically significant. Meta-analysis was conducted using the Review Manager 5.4 software.
Results
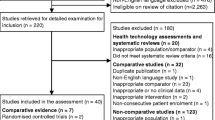
According to the above-mentioned search strategy, a total of 2,242 articles were retrieved from electronic databases spanning January 1, 2000, to May 30, 2023. Detailed insights into the selection process and exclusion rationale are presented through the PRISMA diagram (Fig. 1). Eight RCTs and eighteen cohort studies fulfilled the inclusion criteria, enlisting a cumulative 2,061 participants (Table 1). All eight RCTs originated in China, with seven cohort studies from China and eleven from Japan. Notably, among the studies, eighteen focused on left-sided colon cancer obstructions, while one centered on right-sided colon cancer obstructions, and seven studies covered obstructions in any part of the colon. Sample sizes ranged from 31 to 206 participants, with 1,044 in the SEMS group and 1,017 in the DT group. Participant ages spanned 56.1 to 76.0 years. Diverse SEMS models, encompassing Niti-S, WallFlex, Hanaro, and Naturfit, were adopted, while DT models included Create Medic and Dennis. Further comprehensive trial characteristics are summarized in Additional file 2: Table S2.
Quality assessment results
Within the eight RCTs analyzed, seven were defined at high bias risk, utilizing the Cochrane RoB-2 tool, for inadequate random sequence generation detail (Figs. 2, 3). Due to the study's unique nature, allocation concealment feasibility was limited. All literature sources presented complete, non-selective outcome data. Regarding the eighteen cohort studies, four articles failed to define participant inclusion and exclusion criteria, thus posing significant bias risk based on ROBINS-I assessment (Additional file 3: Fig. S1; Additional file 4: Fig. S2).
Operation-related outcomes
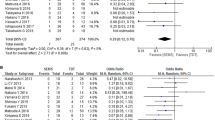
Seven RCTs and fifteen cohort studies reported on SEMS and DT procedural technical success, encompassing 906 SEMS and 903 DT participants (Fig. 4). A random-effects model was applied to pool data. Results indicated no significant difference between the two groups (OR = 1.29, 95% CI 0.56, 2.96, P = 0.55). Subgroup analyses were conducted, stratified by study type. DT exhibited superior technical success over SEMS in the RCT subgroup (OR = 0.13, 95% CI 0.05, 0.39, P = 0.0003) and SEMS demonstrated superior than DT in the cohort study subgroup (OR = 2.25, 95% CI 1.30, 5.02, P = 0.007).
Five RCTs and fifteen cohort studies reported clinical success rates for SEMS and DT, with 830 SEMS and 703 DT participants (Fig. 5). The results revealed a significantly higher rate of clinical success in the SEMS group than the DT group (OR = 1.99, 95% CI 1.04, 3.81, P = 0.04). Stratifying by study type, RCT subgroup revealed higher clinical success rates for DT than SEMS (OR = 0.38, 95% CI 0.16, 0.88, P = 0.02). Conversely, in the cohort study subgroup, SEMS was superior over DT (OR = 1.99, 95% CI 1.04, 3.81, P = 0.04).
Three cohort studies reported on operation-related abdominal pain post SEMS and DT placement, the SEMS group encompassed 102 participants, while the DT group included 52 (Additional file 5: Fig. S3). Results signified significantly reduced abdominal pain incidence in the SEMS group compared to the DT group (OR = 0.16, 95% CI 0.05, 0.50, P = 0.002).
Surgery-related outcomes
Among seven cohort studies comparing intraoperative bleeding, SEMS comprised 255 participants and DT comprised 285 (Fig. 6a). Outcomes revealed significantly less intraoperative bleeding in the SEMS group (MD = − 37.67, 95% CI − 62.73, − 12.60, P = 0.003). For post-surgery stoma creation, nine cohort studies included 462 SEMS participants and 498 DT participants (Fig. 6b). Outcomes indicated a lower stoma creation rate in the SEMS group compared to the DT group (OR = 0.41, 95% CI 0.23, 0.73, P = 0.002).
Thirteen cohort studies were included to compared SEMS and DT groups postoperative hospital stay (Fig. 7a). The SEMS group included 599 participants, while the DT group 565. Outcomes indicated a shorter postoperative length of hospital stays in the DT group compared to the SEMS group (MD = − 4.47, 95% CI − 6.26, − 2.69, P < 0.00001).
Long-term outcomes
Tumor recurrence was reported in one RCT and four cohort studies, including 174 SEMS participants and 110 DT participants (Fig. 7b). The result indicated reduced tumor recurrence rates in the SEMS group compared to the DT group (OR = 0.47, 95% CI 0.22, 0.99, P = 0.05).
However, no statistically significant differences were observed between the utilization of SEMS and DT in the context of colorectal cancer obstruction, with respect to operation-related perforation (OR = 0.56, 95% CI 0.29, 1.05, P = 0.07), device migration (OR = 0.56, 95% CI 0.23, 1.37, P = 0.20), postoperative anastomotic leakage (OR = 1.11, 95% CI 0.61, 2.00, P = 0.74), postoperative infection (OR = 0.77, 95% CI 0.42, 1.41, P = 0.39), postoperative 30-day mortality (OR = 0.62, 95% CI 0.20, 1.91, P = 0.40), overall survival rate (OR = 0.91, 95% CI 0.40, 2.04, P = 0.81), recurrence-free rates (OR = 1.32, 95% CI 0.81, 2.17, P = 0.27), and tumor metastasis (OR = 0.46, 95% CI 0.20, 1.08, P = 0.07). Further details are available in the Additional file 6.
Sensitivity analysis
A sensitivity analysis evaluated the robustness of SEMS and DT meta-analysis results concerning intraoperative bleeding (I2 = 91%) and postoperative hospital stay duration (I2 = 93%), with high study heterogeneity. A literature exclusion approach was employed. Sequentially excluding individual studies resulted in unchanged outcomes, validating meta-analysis reliability.
GRADE evidence
Outcome indicators were graded individually for RCTs and cohort studies, aligned with GRADE evidence levels (Table 2). Due to blinding challenges, outcomes require cautious interpretation. Among RCT-derived indicators, technical success and clinical success evidence levels were moderate, while operation-related perforation, postoperative anastomotic leakage, and infection evidence levels were low. Cohort study-derived indicators showcased low tumor metastasis evidence levels, and very low evidence levels for technical success, clinical success, operation-related perforation, operation-related abdominal pain, device migration, intraoperative bleeding, postoperative stoma creation, postoperative hospital stays, postoperative anastomotic leakage, postoperative infection, postoperative 30-day mortality, overall survival, recurrence-free rate, and tumor recurrence.
Discussion
This systematic review and meta-analysis enrolled twenty-six studies involving 2,061 participants with colorectal cancer obstruction. The results of the analysis indicated that SEMS had advantages over DT in several aspects of managing colorectal cancer obstruction, such as clinical success, operation-related abdominal pain, intraoperative bleeding, stoma creation, length of postoperative hospital stay, and long-term tumor recurrence rate. However, the two methods were not significantly different in terms of technical success, operation-related perforation, device migration, postoperative anastomotic leakage, postoperative infection rate, 30-day mortality rate, survival rate, recurrence-free rate, and tumor metastasis.
SEMS are delivered via a stent placement system to the lesion to dilate the intestine and relieve the obstruction. The internal diameter of a dilated SEMS is in the range of 18–25 mm [53]. DT, with an internal diameter of about 7 mm, is fixed by an inflated balloon catheter before the obstructive lesion [54]. The application of SEMS or DT as a BTS effectively relieves symptoms in patients with colorectal cancer obstruction, avoiding the need for emergency surgery. In this study, SEMS had a higher clinical success rate than that of DT (98.3% vs. 77.8%, P = 0.009). Xu et al. [55] reached the same conclusion on the effectiveness of SMES and DT for left-sided colon obstruction. There are fewer clinical studies of SEMS and DT for the treatment of patients with right-sided colon cancer obstruction. In a study by Yoshiyuki Suzuki et al. [45]. the technical and clinical success rates for SEMS for right-sided colon cancer obstruction were 94.7% and 89.5%, respectively, and for DT 90.5% and 85.7%, respectively, which were not significantly difference. Analyzing the subgroups according to the different sites of obstruction, we found that the clinical success rate of SEMS was higher than DT for obstructions in any part of the colon and showed a trend to be higher than DT in the left-side group. Therefore, for left-sided colon cancer obstruction, it is more advantageous to use SEMS as a bridge to surgery.
However, sub-group analyses based on different study designs indicate that the effects are different between pooled RCTs and cohort studies. The underlying cause may potentially be attributed to the temporal orientation of the data derived from the RCTs, before the year 2014. During this period, DT was notably more prevalent for addressing colorectal cancer obstructions. There is a substantial change in 2012, when SEMS was included in the reimbursement list in Japan and the relevant researches surged. At the same time, the evolution in endoscopic technology and stent material bolstered the effectiveness of SEMS in colorectal cancer obstructions. Therefore, we performed further analyses based on the timing of the studies and found that there was no significant difference between the clinical success rates of SEMS and DT before 2014 (OR = 0.75, 95% CI 0.23, 2.42, P = 0.63), whereas SEMS was superior than DT after 2014 (OR = 2.97, 95% CI 1.61, 5.50, P = 0.0005). Possible reasons for these observations are: (1) the larger internal diameter of the SEMS makes it easier for feces to pass; (2) the smaller diameter of the DT is prone to blockage, which affects obstruction relief; and (3) after placement of the DT, it requires medical professionals for long-term maintenance to flush and drain it, and the risk of artificially caused decompression failure is high.
Operation-related abdominal pain is one of the common complications after endoscopic placement of SEMS and DT. In a study by Chen et al. [36] on intestinal stents and intestinal obstruction tubes for acute left-sided colorectal cancer obstruction, the incidence of abdominal pain in the DT group was as high as 72.7% (8/11) compared with 18.2% (4/22) in the SEMS group. The occurrence of abdominal pain caused by intestinal obstruction tubes might be due to the following: (1) during maintenance, it is necessary to dilute the stool by injecting water and other solvents through the tube into the obstructed intestinal lumen, which briefly causes an increase in pressure in the intestinal lumen; (2) because one end of the tube is fixed to the obstructing lesion and the other end is connected to a suction device, a mechanical force pulls the intestinal wall; and (3) after the successful placement of the intestinal obstruction tube, the tip of the tube protrudes and compresses the intestinal wall, which increases the probability of abdominal pain, and in severe cases, ischemic necrosis of the intestinal wall may occur, causing intestinal perforation. Perforation is the most common and serious complication of endoscopic operations and often requires emergency surgery. In this study, the incidence rates of operation-related perforations were 1.9% and 4.6% for SEMS and DT, respectively (P = 0.07). The risk of stent-related perforation is significantly increased in patients receiving adjunctive chemotherapy, particularly anti-angiogenic agents, with those receiving bevacizumab therapy having a higher risk than that of patients not receiving chemotherapy [57].
With the development of laparoscopic technology, laparoscopic surgery has become the preferred method for the treatment of colorectal cancer because of its advantages such as accurate identification of the lesion site, small surgical trauma, and fast postoperative recovery. However, laparoscopic surgery should be avoided for patients with severe intestinal dilation and edema [58, 59]. In a study conducted by Sato et al. [50] on the treatment of obstructive colorectal cancer with SEMS and DT, the rates of laparoscopic surgery were 100% (60/60) and 44.4% (8/18), respectively (P < 0.001). Matsuda et al. [33] reported a laparoscopic surgery rate of 96.4% (27/28) in the SEMS group, whereas the DT group had a rate of only 2.2% (1/45) (P < 0.001). These results suggest that SEMS is more effective in relieving intestinal obstruction and bowel preparation, improving bowel dilation and edema, and is suitable for laparoscopic surgery, resulting in less intraoperative bleeding, lower incidence of stoma creation, and shorter length of postoperative hospital stay.
The long-term impact of SEMS and DT as a BTS for patients with obstructive colorectal cancer remains unclear. In a retrospective study by Takahashi et al. [60] comparing the differences in tumor biology between SEMS and DT as a BTS for obstructive colorectal cancer, the SEMS group showed significantly higher plasma concentrations of cell-free DNA than did the DT group (992 vs. 308 ng/mL, P = 0.005). Similarly, circulating tumor DNA was higher in the SEMS group than in the DT group (83% vs. 22%, P = 0.002). However, in a study by Okuda et al. [52], no significant differences in 5-year survival and 5-year disease-free survival in patients with stage II/III non-right colorectal cancer were found between SEMS and DT placement (83.7% vs. 86.4%, P = 0.822 and 64.7% vs 66.4%, P = 0.854, respectively). In the current study, the long-term outcomes of survival rate, recurrence-free rate, and tumor metastasis were also not significantly different. However, the tumor recurrence rate was lower in the SEMS group than in the DT group. Given the small sample size and retrospective nature of the included studies, further large-scale, multicenter, high-quality RCTs are needed to validate these findings.
The limitations of this study are as follows. (1) We included twenty-six eligible studies, all of which were from Asian countries. This geographical variation may introduce clinical heterogeneity and affect the generalizability of our results. (2) The included studies involved participants with different types of obstructions caused by colorectal cancer, with one study focusing on right-sided obstructions, six studies on obstructions in any part of the colon, and the remaining studies on left-sided obstructions. This variation in patient characteristics may have resulted in baseline differences among the patients. (3) The included studies used different SEEMS/DT models, which may serve as a confounding factor in our study. (4) Owing to significant bias, the certainty level of the evidence is not very high.
Conclusion
Both SEMS and DT are effective as BTS when treating obstructions due to colorectal cancer. However, the analysis results indicate that SEMS is better than DT at managing colorectal cancer obstruction, such as clinical success, operation-related abdominal pain, intraoperative bleeding, stoma creation, length of postoperative hospital stay, and long-term tumor recurrence. Therefore, as a BTS, SEMS should be the preferred option for patients with colorectal cancer obstruction. Further large-scale international clinical trials are still needed to verify the efficacy of both SEMS and DT for colorectal cancer obstruction in different countries.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- BTS:
-
Bridge to surgery
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- DT:
-
Decompression tube
- ESGE:
-
European Society of Gastrointestinal Endoscopy
- GRADE:
-
Graded Recommendations Assessment, Development, and Evaluation
- MD:
-
Mean difference
- OR:
-
Odds ratio
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT:
-
Randomized controlled trial
- RoB 2:
-
Cochrane Risk of Bias tool version 2
- ROBINS-I:
-
Risk of Bias in Nonrandomized Studies of Interventions
- SEMS:
-
Self-expanding metal stent
References
International Agency for Research on Cancer. Latest global cancer data: cancer burden rises to 19.3 million new cases and 10.0 million cancer deaths in 2020. https://www.iarc.fr/fr/news-events/latest-global-cancer-data-cancer-burden-rises-to-19-3-million-new-cases-and-10-0-million-cancer-deaths-in-2020. Accessed 16 Dec 2020.
Baer C, Menon R, Bastawrous S, Bastawrous A. Emergency presentations of colorectal cancer. Surg Clin North Am. 2017;97:529–45.
Frago R, Ramirez E, Millan M, Kreisler E, del Valle E, Biondo S. Current management of acute malignant large bowel obstruction: a systematic review. Am J Surg. 2014;207:127–38.
Alcántara M, Serra-Aracil X, Falcó J, Mora L, Bombardó J, Navarro S. Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left-sided colonic cancer. World J Surg. 2011;35:1904–10.
Pisano M, Zorcolo L, Merli C, et al. 2017 WSES guidelines on colon and rectal cancer emergencies: obstruction and perforation. World J Emerg Surg. 2018;13:36. https://doi.org/10.1186/s13017-018-0192-3.
Yang L, Li SX, Lv JJ, Jin YL. Contrast endoscopic colorectal stenting and endoscopic ileus tube in preoperative therapy for acute low malignant colorectal obstruction. China J Endosc. 2010;16:169–71.
Dohmoto M. New method-endoscopic implantation of rectal stent in palliative treatment of malignant stenosis. Endosc Dig. 1991;3:1507–12.
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M. Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol. 2004;99:2051–7.
Zhao XD, Cai BB, Cao RS, Shi RH. Palliative treatment for incurable malignant colorectal obstructions: a meta-analysis. World J Gastroenterol. 2013;19:5565–74.
Liang TW, Sun Y, Wei YC, Yang DX. Palliative treatment of malignant colorectal obstruction caused by advanced malignancy: a self-expanding metallic stent or surgery? A system review and meta-analysis. Surg Today. 2014;44:22–33.
Takahashi H, Okabayashi K, Tsuruta M, Hasegawa H, Yahagi M, Kitagawa Y. Self-expanding metallic stents versus surgical intervention as palliative therapy for obstructive colorectal cancer: a meta-analysis. World J Surg. 2015;39:2037–44.
Harris GJ, Senagore AJ, Lavery IC, Fazio VW. The management of neoplastic colorectal obstruction with colonic endolumenal stenting devices. Am J Surg. 2001;181:499–506.
van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Götz M, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline–Update 2020. Endoscopy. 2020;52:389–407.
ASGE Standards of Practice Committee; Harrison ME, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, et al. The role of endoscopy in the management of patients with known and suspected colonic obstruction and pseudo-obstruction. Gastrointest Endosc. 2010;71:669–79.
Abbott WO, Karr WG, Glenn PM, Warren R. Intubation studies of the human small intestine. 14. The absorption of glucose from the duodenum. Am J Med Sci. 1940;200:532–6.
Araki Y, Isomoto H, Matsumoto A, Kaibara A, Yasunaga M, Hayashi K, et al. Endoscopic decompression procedure in acute obstructing colorectal cancer. Endoscopy. 2000;32:641–3.
Horiuchi A, Maeyama H, Ochi Y, Morikawa A, Miyazawa K. Usefulness of Dennis Colorectal Tube in endoscopic decompression of acute, malignant colonic obstruction. Gastrointest Endosc. 2001;54:229–32.
Tanaka T, Furukawa A, Murata K, Sakamoto T. Endoscopic transanal decompression with a drainage tube for acute colonic obstruction: clinical aspects of preoperative treatment. Dis Colon Rectum. 2001;44:418–22.
Yokohata K, Sumiyoshi K, Hirakawa K. Merits and faults of transanal ileus tube for obstructing colorectal cancer. Asian J Surg. 2006;29:125–7.
Horiuchi A, Nakayama Y, Kajiyama M, Kamijima T, Kato N, Ichise Y, et al. Endoscopic decompression of benign large bowel obstruction using a transanal drainage tube. Colorectal Dis. 2012;14:623–7.
An Y. Efficacy of drainage tube and self-expanding metallic stent acute left malignant colorectal obstruction. Zhong Guo Medical University; 2018.
Jiang H, Sun MW, Hefright B, Chen W, Lu CD, Zeng J. Efficacy of hypocaloric parenteral nutrition for surgical patients: a systematic review and meta-analysis. Clin Nutr. 2011;30:730–7.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in andomized trials. BMJ. 2019;366:l4898.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Ansari MT, Tsertsvadze A, Moher D. Grading quality of evidence and strength of recommendations: a perspective. PloS Med. 2009;6:e1000151.
Brozek JL, Akl EA, Alonso-Coello P, Lang D, Jaeschke R, Williams JW, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64:669–77.
Li SJ, Jiang H, Yang H, Chen W, Peng J, Sun MW, et al. The dilemma of heterogeneity tests in meta-analysis: a challenge from a simulation study. PLoS ONE. 2015;10:e0127538.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Xing Z, Zhao Y, Zhu J, et al. Contrast ileus tube through anus and endoscopic colorectal stent in pre-operative therapy for lower position malignant colorectal obstruction. Yinanbing Zazhi. 2013;12:200–2.
Chen SJ, Huang ZH, Guo CS. Colorectal stenting vs ileus tube drainage for treatment of acute malignant colorectal obstruction. Shijie Huaren Xiaohua Zazhi. 2014;22:4036–40.
Chen Z, Wang XM, Yin ZZ, et al. The clinical efficacy of acute obstructive left-sided colorectal cancer treated by colonoscopic metal stenting and ileus tube catheterization. Tianjin Yiyao. 2014;42:481–4.
Li H, Li Z, You Z. The application of stent and transanal ileus tube in laparoscopic treatment of obstructive colorectal cancer. J Laparosc Surg. 2015;20:179–82.
Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Takahashi G, Matsutani T, et al. Comparison between metallic stent and transanal decompression tube for malignant large-bowel obstruction. J Surg Res. 2016;205:474–81.
Kojima K, Toda N, Kurosaki S, et al. Self-expandable metallic stent as bridge to surgery is superior to transanal drainage tube at quality of life for the patients with primary malignant colorectal obstruction. United Eur Gastroenterol J. 2016;4:A75–6.
Takeyama H, Kitani K, Wakasa T, Tsujie M, Fujiwara Y, Mizuno S, et al. Self-expanding metallic stent improves histopathologic edema compared with transanal drainage tube for malignant colorectal obstruction. Dig Endosc. 2016;28:456–64.
Chen JJ, Lai YD, Li DS, et al. Intestinal stent, and intestinal obstruction catheter for acute left hemi-colorectal cancerous obstruction. Chin J Dig Endose. 2016;33:252–4.
Yang KH, Wang K. Treatment analysis of stent and obstruction catheter in laparoscopic surgery for left colorectal cancer patients complicated with intestinal obstruction. Zhonghua Putong Waikexue Wenxian Dianziban. 2016;10:291–3.
Chen SQ. Effectiveness of intestinal stents and intestinal obstruction catheters in patients with obstructive colorectal cancer undergoing laparoscopic surgery. Dangdai Yiyao Luncong. 2017;15:75–7.
Liu W, Li L, Guo JM. The effect of intestinal stent and ileus tube in laparoscopic surgery in treatment of obstructive colorectal cancer. Shiyong Aizheng Zazhi. 2017;32:1716–8.
Kagami S, Funahashi K, Ushigome M, Koike J, Kaneko T, Koda T, et al. Comparative study between colonic metallic stent and anal tube decompression for Japanese patients with left-sided malignant large bowel obstruction. World J Surg Oncol. 2018;16:210.
Kawachi J, Kashiwagi H, Shimoyama R, Isogai N, Fukai R, Miyake K, et al. Comparison of efficacies of the self-expandable metallic stent versus transanal drainage tube and emergency surgery for malignant left-sided colon obstruction. Asian J Surg. 2018;41:498–505.
Chang XD, Deng WS, Huang J. Transanal ileus tube decompression and intestinal stent implantation decompression laparoscopic surgery comparative observation on treatment of obstructive colorectal cancer. Linchang He Shiyan Zazhi. 2018;17:1425–7.
Zhang S, Xu J, Shi L, et al. Comparison between self-expandable metallic colonic stent and transanal decompression tube for leftsided malignant colorectal obstruction. Zhongguo Zhongxiyi Jiehe Waike Zazhi. 2018;24:550–5.
Sato R, Oikawa M, Kakita T, Okada T, Oyama A, Abe T, et al. Comparison of the long-term outcomes of the self-expandable metallic stent and transanal decompression tube for obstructive colorectal cancer. Ann Gastroenterol Surg. 2019;3:209–16.
Suzuki Y, Moritani K, Seo Y, Takahashi T. Comparison of decompression tubes with metallic stents for the management of right-sided malignant colonic obstruction. World J Gastroenterol. 2019;25:1975–85.
Yin C. Effectiveness of stents and intestinal obstruction catheters in laparoscopic surgery for obstructive colorectal cancer. Zhongguo Yiliao Qixie Xinxi. 2019;25:84–5.
Xu YS, Fu YF, Li DC, Song T. Preoperative colonic decompression with decompression tube insertion versus stent insertion in patients with malignant left colonic obstruction. Surg Laparosc Endosc Percutan Tech. 2020;30:183–6.
Inoue H, Arita T, Kuriu Y, Shimizu H, Kiuchi J, Yamamoto Y, et al. Emergency management of obstructive colorectal cancer—a retrospective study of efficacy and safety in self-expanding metallic stents and trans-anal tubes. In Vivo. 2021;35:2289–96.
Kondo A, Kumamoto K, Kobara H, Nagahara T, Wato M, Shibatoge M, et al. Outcomes of patients with left-sided obstructive colorectal cancer: comparison between self-expandable metallic stent and other treatment methods. Dig Surg. 2022;39:117–24.
Sato K, Imaizumi K, Kasajima H, Kurushima M, Umehara M, Tsuruga Y, et al. Short- and long-term outcomes of a self-expandable metallic stent versus a transanal decompression tube for pathological stage II and III left-sided obstructive colorectal cancer: a retrospective observational study. Surg Today. 2022;52:268–77.
Zhang S, Liu G, Wu GH, Zhang SW, Zhao YJ, Xu J. Transanal decompression tube is superior to self-expandable metallic colonic stent for malignant colorectal obstruction: a retrospective study. ANZ J Surg. 2022;92:140–5.
Okuda Y, Shimura T, Uno K, Yamada T, Nukui T, Mizushima T, et al. A multicenter case-control study of self-expanding metallic stent versus trans-anal colorectal tube for stage II/III non-right-sided obstructive colon cancer. J Gastroenterol. 2023;58:217–28.
Sasaki T, Ishibashi R, Yoshida S, Fujisawa T, Shinagawa H, Gon C, et al. Comparing the mechanical properties of a self-expandable metallic stent for colorectal obstruction: proposed measurement method of axial force using a new measurement machine. Dig Endosc. 2021;33:170–8.
Ohnita K, Shikuwa S, Isomoto H, Yamaguchi N, Okamoto K, Nishiyama H, et al. A new thin endoscopic method of transanal drainage tube insertion for acute colonic obstruction due to colorectal cancer. Dig Endosc. 2009;21:252–4.
Xu J, Zhang S, Jiang T, Zhao YJ. Transanal drainage tubes vs metallic stents for acute malignant left-sided bowel obstruction: a systematic review and meta-analysis. Medicine (Baltimore). 2020;99:e18623.
Xu Y, Zhu YJ. Research Advances in Intestinal Tract Catheter and Self-Expandable Metallic Stent Treatment for Left Semicolon Cancer Combined with Obstruction. Yixue Zongshu. 2018;24(06):1087–91.
van Halsema EE, van Hooft JE, Small AJ, Baron TH, García-Cano J, Cheon JH, et al. Perforation in colorectal stenting: a meta-analysis and a search for risk factors. Gastrointest Endosc. 2014;79:970-82.e7.
Marcello PW, Milsom JW, Wong SK, Brady K, Goormastic M, Fazio VW. Laparoscopic total colectomy for acute colitis: a case-control study. Dis Colon Rectum. 2001;44:1441–5.
Ng SS, Lee JF, Yiu RY, Li JC, Leung WW, Leung KL. Emergency laparoscopic-assisted versus open right hemicolectomy for obstructing right-sided colonic carcinoma: a comparative study of short-term clinical outcomes. World J Surg. 2008;32:454–8.
Takahashi G, Yamada T, Iwai T, Takeda K, Koizumi M, Shinji S, et al. Oncological assessment of stent placement for obstructive colorectal cancer from circulating cell-free DNA and circulating tumor DNA dynamics. Ann Surg Oncol. 2018;25:737–44.
Acknowledgements
Not applicable
Funding
This work was supported by funding from the Sichuan Science and Technology Program (Grant ID: 2021YFS0378 to Hua Jiang; 2021YFH0109 to Mingwei Sun; 2020YFS0392 to Bin Cai; 2023NSFSC1475 to Kai Wang), Health Commission of Sichuan Province (Grant ID: Chuan-Gan-Yan 2023–207 to Kai Wang), Sichuan Provincial People's Hospital (Grant ID: 2021ZX01 to Kai Wang).
Author information
Authors and Affiliations
Contributions
WM was the lead author of the Cochrane review, the data on which this analysis was based. WM conceived and delineated the hypotheses, designed the study, acquired, and analyzed the data, wrote, and edited the manuscript of the previous analysis, and edited the manuscript of the present analysis. HJ and BC performed the study design and conceptualization. Mathematical modeling and meta-analysis were conducted with the help of LW and CZ. WM and J-CZ contributed to the screening of the eligible studies, data extraction, and data synthesis. J-CZ and KL contributed to the quality assessment of the publications. WM and J-CZ drafted the first version of this manuscript. All authors read and approved the final manuscript and take responsibility for its publication.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Electronic search strategies.
Additional file 2
: Table S2. Detailed information on included studies.
Additional file 3
: Fig S1. The risk of bias graph for cohort studies based on ROBINS-I.
Additional file 4
: Fig S2. The risk of bias summary for cohort studies based on ROBINS-I.
Additional file 5
: Fig S3. Forest plot of meta-analysis results regarding operation-related abdominal pain in SEMS and DT groups. SEMS, self-expanding metal stent; DT, decompression tube; CI, confidence interval; M-H, Mantel-Haenszel; df, degree of freedom.
Additional file 6
: Other research findings.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, W., Zhang, JC., Luo, K. et al. Self-expanding metal stents versus decompression tubes as a bridge to surgery for patients with obstruction caused by colorectal cancer: a systematic review and meta-analysis. World J Emerg Surg 18, 46 (2023). https://doi.org/10.1186/s13017-023-00515-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-023-00515-6