Abstract
Introduction
Laparoscopic colectomy is rarely performed for ischemic colitis. The aim of this propensity score-matched study was to compare preoperative characteristics, intraoperative details and short-term outcomes for emergent laparoscopic colectomy versus the traditional open approach for patients with ischemic colitis.
Methods
Retrospective review of 96 patients who underwent emergent colectomy for ischemic colitis between January 2011 and December 2020 (39 via laparoscopy, 57 via laparotomy) was performed. We compared short-term outcomes after using a one-to-one ratio and nearest-neighbor propensity score matching to obtain similar preoperative and intraoperative parameters in each group.
Results
Patients in the open group experienced more surgical site complications (52.6% vs. 23.0%, p = 0.004), more intra-abdominal abscesses (47.3% vs. 17.9%, p = 0.003), longer need for ventilator support (20 days vs. 0 days, p < 0.001), more major complications (77.2% vs. 43.5%, p = 0.001), higher mortality (49.1% vs. 20.5%, p = 0.004), and longer hospital stay (32 days vs. 19 days, p = 0.001). After propensity score matching (31 patients in each group), patients undergoing open (vs. laparoscopy) had more surgical site complications (45.1% vs. 19.4%, p = 0.030) and required longer ventilator support (14 vs. 3 days, p = 0.039). After multivariate analysis, Charlson Comorbidity Index (p = 0.024), APACHE II score (p = 0.001), and Favier’s classification (p = 0.023) were independent predictors of mortality.
Conclusions
Laparoscopic emergent colectomy for ischemic colitis is feasible and is associated with fewer surgical site complications and better respiratory function, compared to the open approach.
Similar content being viewed by others
Introduction
Ischemic colitis (IC), characterized by insufficient blood supply and oxygen delivery to the colon, is the most common form of bowel ischemia [1]; the incidence of IC ranges from 4.5 to 44 cases per 100,000 person years [2]. The severity of IC depends on the degree of parietal involvement, ranging from superficial mucosa inflammation, amenable to conservative or medical treatment, to full-thickness transmural necrosis, a life-threatening condition that requires surgery [3,4,5,6]. The mortality rate after surgery is high, up to 60% [7], usually related to transmural bowel necrosis and patient comorbidity [8].
The benefits of laparoscopy have been well described for elective [9, 10] and more recently, for emergent colorectal surgery [11,12,13,14]. However, publications on the laparoscopic approach for IC are rare; most patients undergo laparotomy [15,16,17,18]. The aim of this study is to report the short-term outcomes of laparoscopic management of patients with IC, compared to open colectomy, in propensity score-matched groups.
Patients and methods
From January 2011 to December 2020, all consecutive patients in China Medical Hospital (Taichung, Taiwan) who underwent emergent surgery for IC confirmed by pathology reports were included in this study (Fig. 1). The study was approved by the departmental and institutional ethical committees of the China Medical University Hospital, Taichung, Taiwan (Registered NO: CMUH110-REC3-067). Baseline characteristics, laboratory, operative, postoperative outcome data were retrospectively reviewed and analyzed. Indications for the minimal access approach depended on surgeon discretion. Patients who initially underwent laparoscopy but who were converted to open surgery were analyzed in the laparoscopic group (intention-to-treat). The extent of colon resection, the performance of anastomosis, and/or stoma was determined on a case-by-case basis, according to surgeons’ judgment, degree of bowel ischemia, and patient clinical status. We categorized ischemia according to Favier’s classification: type I (transient and mild mucosal ischemia), type II (mucosal and muscularis ischemia, generally considered reversible but possibly linked to multiple organ failure), or type III (nonreversible transmural ischemia) [3].
The Charlson Comorbidity Index (CCI) was calculated for each patient [19]. The Acute Physiology and Chronic Health Evaluation II (APACHE II) score was used to evaluate severity of sepsis before operation [20]. Delayed surgery was defined as surgical intervention performed ≥ 3 days after the initial symptoms appeared [21]. The etiology of IC was individualized as postoperative IC (within 15 days postoperative) or not, and among the latter, as occlusive and non-occlusive [17, 22]. Duration of ventilator support and hospital stay were counted starting from the day of emergency colectomy for IC. Deceased patients were excluded from statistical analyses of these two parameters. Morbidity and mortality were recorded at 30 days after the second operation or during the same hospital stay if the patient was hospitalized longer. Complications were graded using the Clavien–Dindo classification [23]. Major complications were defined as grade III or greater. Intra-abdominal or deep surgical site abscess was defined as abscess formations visualized on computerized tomography (CT) scan. Prolonged ileus was defined as non-emission of flatus ≥ 7 days [24].
Surgical technique of laparoscopic colectomy for ischemic colitis
All patients underwent skin prep and were draped for surgery in the lithotomy position. The first 12 mm trocar was inserted peri-umbilically by the open method. After examination of the entire abdomen, the extent of IC was confirmed and additional trocars were inserted: two on the right and two on the left. The colon was mobilized lateral to medial and then divided proximally and distally with endo-GIA staplers to remove the ischemic segment (Fig. 2). The corresponding mesentery transection was performed using Ligasure (Fig. 2). The ischemic colonic specimen was extracted via the umbilical surgical site or planned stoma site (Fig. 2). Primary anastomosis or Hartmann’s procedure was performed depending on patient clinical status and surgeon experience. Finally, the entire abdomen was abundantly lavaged and an abdominal drain placed.
Surgical steps of emergent laparoscopic colectomy for ischemia colitis. a Colonic mobilization from lateral side; b Endo-GIA was applied at distal and proximal edges of the ischemic colon; c Mesentery division with Ligasure; and d Specimen was extracted via the umbilicus surgical site or planned stoma site
Categorical data are presented as percentages, and continuous data are expressed as median (with range). Fisher’s exact test or chi-squared test was used for categorical data. Student’s t test was used for normally distributed metric data and Mann–Whitney U test for non-normally distributed data. A propensity score analysis was performed to obtain a one-to-one match by using the nearest-neighbor matching method. Multiple logistic regression was used to derive propensity scores regarding the probability that a patient would undergo a laparoscopic or open method. Patients in whom the propensity score was not applicable were excluded from further analysis. The following covariates were matched: ASA, APACHE II score, Favier classification, and extent of bowel ischemia. Variables with p values < 0.05 from univariate analysis were included in a stepwise multivariate logistic regression analysis to evaluate the probability of mortality. Receiver operating characteristic (ROC) curve analysis was performed to identify the optimal cutoff value of APACHE II score for mortality according to the area under the ROC curve (AUC). All statistical analyses were performed with SPSS for Windows (version 25.0; IBM-SPSS Inc., Armonk, NY).
Results
From January 2011 to December 2020, 96 patients underwent emergent colectomy for IC, 39 via laparoscopy, 57 via laparotomy (Fig. 1). Before propensity score matching, statistically significant differences between laparoscopic and open groups included higher ASA (ASA 4: 64.9% vs. 38.4%, p = 0.024) and higher APACHE II score (19 vs. 13, p < 0.001) for the open group compared to the laparoscopic group, respectively (Table 1). There was no statistically significant difference in CCI (open vs. laparoscopic: 5 vs. 6, p = 0.772). All patients were Favier II or III: There were more patients in the open group who were Favier III (75.4% vs. 51.3%, p = 0.014) and had total colonic ischemia (19.4% vs. 5.1%, p = 0.004) (vs. laparoscopic group) (Table 2). There was no statistically significant difference in the proportion of patients with bowel perforation (open vs. laparoscopic: 45.6% vs. 41%, p = 0.656). After propensity score matching, none of the variables were statistically significantly different in the two (open and laparoscopic) groups of 31 patients each.
Perioperative results and short-term morbidity are summarized in Table 3. Before propensity score matching, patients in the open group had more surgical site complications (52.6% vs. 23.0%, p = 0.004), higher proportion of intra-abdominal abscess (47.3% vs. 17.9%, p = 0.003), longer ventilator support (20 days vs. 0 days, p < 0.001), more major complications (77.2% vs. 43.5%, p = 0.001), higher mortality (49.1% vs. 20.5%, p = 0.004), and longer hospital stay (32 days vs. 19 days, p = 0.001). After propensity score matching, patients undergoing open (vs. laparoscopy) had more surgical site complications (45.1% vs. 19.4%, p = 0.030) and required longer ventilator support (14 days vs. 3 days, p = 0.039), whereas there was no statistically significant difference in rates of major complications (64.5% vs. 48.3%, p = 0.200) or mortality (38.7% vs. 25.8%, p = 0.277). However, there was a trend toward fewer intra-abdominal abscess (38.7% vs. 19.4%, p = 0.093) and shorter hospital stay (32 days vs. 20 days, p = 0.061).
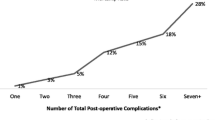
In univariate analysis, ASA class (p = 0.005), CCI (p = 0.009), APACHE II score (p < 0.001), laparoscopy approach (p = 0.006), aorta-related surgery (p = 0.017), Favier’s classification (p = 0.017), and transparietal colonic ischemia (p = 0.004) were statistically significant associated with mortality. After multivariate analysis, CCI (p = 0.024), APACHE II score (p = 0.001), Favier’s classification (p = 0.023) were independent predictors of mortality (Table 4). With regard to the evaluation of the cutoff point of APACHE II score for mortality, the area under the curve (AUC) was 86.0% (95% CI 77.9–94.1, p < 0.001). The cutoff point for the APACHE II score was 20.5 (optimal sensitivity and specificity were 66.7% and 93.3%, respectively) (Fig. 3).
Discussion
This propensity score matching comparison of emergent open versus laparoscopic colonic resection for IC confirmed that surgical site complications and duration of ventilation support were statistically significantly reduced after the laparoscopic approach. Of note, there was no statistically significant difference found in hospital stay, major complications, or mortality. After multivariate analysis, CCI (OR = 1.29, p = 0.024), APACHE II score (OR = 1.25, p = 0.001), and Favier’s classification (OR = 9.02, p = 0.023) remained statistically significant predictors of mortality (Table 4).
While randomized clinical trials are universally accepted as the gold-standard methodology for measuring the “causal” effects of management on outcomes [25], they are not always possible or adequately powered because they are time-consuming, costly, and may have ethical or practical constraints [26, 27]. Moreover, IC is rare; therefore, the accrual period for a randomized trial would be long and costly. Propensity score matching has gained in popularity in observational studies because potential biases in pretreatment characteristics between treatment groups are minimized [28].
Perioperative mortality can be as high as 60% after surgery and is most likely multifactorial, including degree of parietal involvement, location of ischemia, patient comorbidities, and physiological status [7]. However, after propensity-score matching, there was no statistically significant difference in patient variables thought to be associated with surgical outcomes in our study. Intraoperative findings (Favier’s classification, location of ischemia) were also included in propensity-score matching, even though these variables cannot be known precisely before operation, because they reflect severity of disease and technical difficulty. However, in 2011, Reissfelder et al. presented a risk score that predicts postoperative mortality of patients undergoing surgery for IC; perioperative variables included non-occlusive IC, acute renal failure, extent of bowel ischemia, serum lactate, and duration of catecholamine therapy [29]. As some of these factors were not included in our matching, they could eventually be part of a selection bias for treating patients with IC using an open or laparoscopic approach.
While laparoscopy is widely practiced in elective colorectal surgery, it is much less popular for emergency settings, although its feasibility and safety have been shown [11] and, ideally, should provide a smoother and less complicated postoperative course. Moreover, laparoscopy can be used with diagnostic intent in suspected IC, especially when colonoscopy is deemed dangerous [30] or for post-ischemic stenosis [15] and has the advantage of visualizing the entire colon, but is infrequently indicated for colectomy after acute ischemia and in particular in patients with IC. In the ACS-NSQIP database study, only 125 of 4548 (4.3%) colectomies for IC were performed laparoscopically [31]. Most published studies on the laparoscopic approach in patients with acute colorectal disease have focused on perforated diverticulitis, colorectal anastomosis leakage, or inflammatory colitis [12,13,14, 32,33,34,35,36]. All these studies showed that the laparoscopic approach could decrease the surgical site complication rate in the emergent setting but were not conclusive regarding overall complications, mortality, or hospital stay. This is in line with our results: The surgical site complication rate was lower in the laparoscopic group after propensity score matching. Furthermore, duration of ventilator support was shorter in the laparoscopic group after propensity score matching. Although there was a statistical trend toward shorter hospital stay, larger series are needed to demonstrate the advantages of the laparoscopy approach, and in particular in patients with severe disease or poor physiological status.
Symptoms of IC are often nonspecific, vague, and the diagnosis can be challenging at an early stage. In a review of 364 patients, peritoneal signs were present in only 7.4 percent of patients [1]. Furthermore, it is often difficult to identify symptoms in patients who are unconscious and debilitated, those in intensive care, or who are cognitively impaired, such as those with delirium or dementia. Therefore, IC must be suspected if a patient in an intensive care unit cannot tolerate a normal diet within a couple of days or has signs of infection. As ischemia in IC is initially mucosal, laparoscopic visualization of the serosa may seem normal, but conversely, as transmural ischemia can exist with minimal clinical signs, laparoscopic examination could be an early diagnostic tool for severe IC and lead to earlier surgical intervention.
When we compared the surgical delay between the laparoscopic and open groups, we found that the delay was longer in the open group than in the laparoscopic group (59.6% vs. 43.5%, p = 0.121; after propensity, 67.7% vs. 48.3%, p = 0.123). Although the difference was not statistically significant, this finding might further support the role of laparoscopy as an early diagnostic tool of the acute abdomen (EAES Symposium) [30, 37].
Our overall operation times (open: 200 min, laparoscopy: 180 min, p = 0.693) were comparable to those in another study [18]. However, in contrast to studies that focused on diverticulitis [12, 13], the operation time in the laparoscopy group was not statistically significantly longer than the open group. One reason might be that surgery for IC might have been more complex in the open group compared to laparoscopy group in spite of propensity score matching. Secondly, surgeons take more time to close a laparotomy compared to smaller laparoscopic surgical sites. Thirdly, all surgeries were performed by experienced hands in our institution. Based on our experience, we think laparoscopy should not prolong the operation time in the emergent cases and might even decrease the operation time in experienced hands.
Ischemic colitis is rare. The 2016 Premier Perspectives national inpatient database analysis indicated that only 12/945 (1.5%) laparoscopic colectomies were performed for noninfectious enteritis and colitis [38]. We agree with the authors that emergency laparoscopy has its place in emergency settings such as IC and there is a need to enlarge the indications [38]. Maggiori and Panis found that laparoscopic surgery for severe acute colitis was associated with a similar (or improved) short-term outcome compared with an open approach [39]. Sampietro et al. reported on 145 patients who underwent laparoscopic emergency subtotal colectomy for ulcerative colitis or Crohn’s disease stating that it was safe and feasible for acute severe colitis in IBD [40]. Our colectomy procedure is standardized, and all surgeons in our unit follow it. We believe that standardization of the surgical procedure could avoid mistakes especially when there are anatomical alterations and tissue inflammatory changes in the emergent setting. Finally, a laparoscopic second look is preferable to laparotomy. The timing of the second look is variable but usually should be within 72 h [41, 42].
While the causes that initiate ischemia may be variable, and even multiple, it is widely thought that these patients have vascular anomalies that enhance the onset: These can be constitutional or acquired. Among the former, there is no or a contentious connection between the middle colic and left colic arteries (Griffith’s point) in up to 48% of patients, or between the most distal sigmoid artery and the superior rectal artery (Sudeck’s point) in 5–15% of patients [43]. Previous colectomy or aortic surgery can further modify the vascular supply to the colon [43, 44]. Anastomosis after segmental colectomy for IC under these conditions might need specific maneuvers such as retroileal transmesenteric anastomosis (Toupet technique) or the Deloyers technique [45].
Previous studies have found various laboratory parameters to be associated with mortality, such as LDH > 450 U/l, blood urea nitrogen (BUN) (> 28 mg/dl), Hb < 12 g/dl, and hyponatremia (Na < 136 mEq/l) [46]. In our study, we used the APACHE II score to determine the general physical status of patients with IC. In multivariate regression analysis, APACHE II score (OR: 1.25, 95% CI 1.10–1.41, p = 0.001) was identified as an independent predictive factor for mortality. Furthermore, the APACHE II score model exhibited a high accuracy for the prediction of mortality, with an AUC of 0.86 (77.9–94.1, p < 0.001), comparable to that found by Peixoto et al. where the AUC was 0.89 [46]. In a large series of open colectomy, emergency surgery for IC was associated with high postoperative mortality [22]. In this study, preoperative lactates level, delay to surgery > 12 h, and the occurrence of postoperative acute kidney injury were independent predictors of postoperative mortality. Conversely, the specific cause of IC did not seem to impact postoperative mortality. These authors underlined the key role of prompt diagnosis and surgical intervention in the management of severe IC [22].
After propensity score matching, the conversion rate was 17/31 = 22.5%. The reasons for conversion were bowel distension, total colonic ischemia, diffuse fecal peritonitis, and/or severe adhesions. This is comparable to the literature on diverticular disease [13].
Our study has several limitations. Firstly, the sample size of this single institution case series was small (pre propensity, n = 96; post-propensity, n = 62). Secondly, as the decision to perform the operation laparoscopically was surgeon dependent, there may have been a selection bias even after propensity score matching. Thirdly, because of the retrospective design, it is not sure whether other factors may have influenced the postoperative outcomes, including intraoperative fecal spillage and bowel distension. Moreover, surgeon judgment intervened in the evaluation of the extent and degree of bowel ischemia to decide how much bowel should be resected and whether to perform primary anastomosis. In the future, intra-operative assessment by ICG might be an interesting avenue to explore [47]. Last, only known potential risk factors were matched. All confounding factors, those measured as well as those that are not measured, can only be eliminated by adequately conducted randomization. However, ischemic colitis is a rare disease, and therefore, a properly conducted and adequately powered randomized study would be difficult to perform. Finally, the inclusion time period of this study was long (2011–2020), and there have been many advances in surgical techniques and equipment, intensive care which may have impacted the surgical outcomes (such as operating time, postoperative complication rate, and hospital stay).
Conclusion
Laparoscopic emergent colectomy for IC is feasible and safe, with fewer postoperative surgical site complications and reduced duration of ventilatory support, compared to laparotomy. Major complication and mortality rates remain high, essentially because of the severity of disease and patient status. We can postulate that the advantages of laparoscopic colectomy for patients requiring surgical intervention for ischemic colitis might reduce the morbidity and mortality in this setting, but this postulate needs to be proven in larger, and ideally, randomized studies.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, William Tzu-Liang Chen, on special request.
References
Montoro MA, Brandt LJ, Santolaria S, Gomollon F, Puértolas BS, Vera J, et al. Clinical patterns and outcomes of ischaemic colitis: results of the Working Group for the Study of Ischaemic Colitis in Spain (CIE study). Scand J Gastroenterol. 2011;46:236–46.
Higgins PDR, Davis KJ, Laine L. The epidemiology of ischaemic colitis. Aliment Pharmacol Ther. 2004;19:729–38.
Favier C, Bonneau HP, Tran Minh V, Devic J. Endoscopic diagnosis of regressive ischemic colitis. Endoscopic, histologic and arteriographic correlations. Nouvelle Presse Med. 1976;5:77–9.
Trotter JM, Hunt L, Peter MB. Ischaemic colitis. BMJ. 2016;355:i6600.
Beppu K, Osada T, Nagahara A, Matsumoto K, Shibuya T, Sakamoto N, Otaka M, Terai T, Ogihara T, Watanabe S. Relationship between endoscopic findings and clinical severity in ischemic colitis. Intern Med. 2011;50:2263–7.
Fitzgerald JF, Hernandez LO. Ischemic colitis. Clin Colon Rectal Surg. 2015;28:93–8.
Ritz JP, Germer CT, Buhr HJ. Prognostic factors for mesenteric infarction: multivariate analysis of 187 patients with regard to patient age. Ann Vasc Surg. 2005;19:328–34.
Longo WE, Ward D, Vernava AM, Kaminski DL. Outcome of patients with total colonic ischemia. Dis Colon Rectum. 1997;40:1448–54.
Kulkarni N, Arulampalam T. Laparoscopic surgery reduces the incidence of surgical site infections compared to the open approach for colorectal procedures: a meta-analysis. Tech Coloproctol. 2020;24:1017–24.
Fretland ÅA, Dagenborg VJ, Bjørnelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW, et al. Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg. 2018;267:199–207.
Chand M, Siddiqui MR, Gupta A, Rasheed S, Tekkis P, Parvaiz A, et al. Systematic review of emergent laparoscopic colorectal surgery for benign and malignant disease. World J Gastroenterol. 2014;20(45):16956–63.
Turley RS, Barbas AS, Lidsky ME, Mantyh CR, Migaly J, Scarborough JE. Laparoscopic versus open Hartmann’s procedure for the emergency treatment of diverticulitis: a propensity-matched analysis. Dis Colon Rectum. 2013;56(1):72–82.
Lee YF, Brown RF, Battaglia M, Cleary RK. Laparoscopic versus open emergent sigmoid resection for perforated diverticulitis. J Gastrointest Surg. 2020;24(5):1173–82.
Vennix S, Lips DJ, Di Saverio S, van Wagensveld BA, Brokelman WJ, Gerhards MF, et al. Acute laparoscopic and open sigmoidectomy for perforated diverticulitis: a propensity score matched cohort. Surg Endosc. 2015;30:3889–96.
Tsukada T, Nakano T, Matsui D, Sasaki S. Stenotic ischemic colitis treated with laparoscopy-assisted surgery. World J Gastrointest Surg. 2012;4(8):203–7.
Demetriou G, Nassar A, Subramonia S. The pathophysiology, presentation and management of ischaemic colitis: a systematic review. World J Surg. 2020;44(3):927–38.
Moszkowicz D, Trésallet C, Mariani A, Lefevre JH, Godiris-Petit G, Noullet S, et al. Ischaemic colitis: Indications, extent, and results of standardized emergency surgery. Dig Liver Dis. 2014;46(6):505–11.
Genstorfer J, Schäfer J, Kettelhack C, Oertli D, Rosenthal R. Surgery for ischemic colitis: outcome and risk factors for in-hospital mortality. Int J Colorectal Dis. 2014;29(4):493–503.
Charlson M, Pompei P, Ales K, MacKenzie C. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–83.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
Noh M, Yang SS, Jung SW, Park JH, Im YC, Kim KY. Poor prognostic factors in patients who underwent surgery for acute non-occlusive ischemic colitis. World J Emerg Surg. 2015;10:12 ((see correction in World J Emerg Surg. 2016 June 2; 11: 23)).
Beghdadi N, Reitano E, Cochennec F, Desgranges P, Amiot A, Sobhani I, et al. Predictors of mortality following emergency open colectomy for ischemic colitis: a single-center experience. World J Emerg Surg. 2020;15(1):40.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Artinyan A, Nunoo-Mensah JW, Balasubramaniam S, Gauderman J, Essani R, Gonzalez-Ruiz C, et al. Prolonged postoperative ileus-definition, risk factors, and predictors after surgery. World J Surg. 2008;32:1495–500.
Kapur K. Principles of biostatistics. In: Clinical and translational science; 2017. p. 243–60
Carlisle B, Kimmelman J, Ramsay T, MacKinnon N. Unsuccessful trial accrual and human subjects protections: an empirical analysis of recently closed trials. Clin Trials. 2015;12:77–83.
Chadow D, Robinson NB, Cancelli G, Soletti G, Audisio K, Rahouma M, Perezgrovas R, Gaudino M. Predictors of failure to reach target sample size in surgical randomized trials. Br J Surg. 2022;109(2):176–7.
Ali MS, Prieto-Alhambra D, Lopes LC, Ramos D, Bispo N, Ichihara MY, et al. Propensity score methods in health technology assessment: principles, extended applications, and recent advances. Front Pharmacol. 2019;10:973.
Reissfelder C, Sweiti H, Antolovic D, Rahbari NN, Hofer S, Büchler MW, Weitz J, Koch M. Ischemic colitis: who will survive? Surgery. 2011;149:585–92.
Othman M, El-Majzoub N, Khoury G, Barada K. Laparoscopy rather than colonoscopy for the diagnosis and treatment of fulminant ischemic colitis. Int J Colorectal Dis. 2014;29(11):1443–4.
Tseng J, Loper B, Jain M, Lewis AV, Margulies DR, Alban RF. Predictive factors of mortality after colectomy in ischemic colitis: an ACS-NSQIP database study. Trauma Surg Acute Care Open. 2017;2(1):e000126.
Lee CM, Huh JW, Yun SH, Kim HC, Lee WY, Park YA, et al. Laparoscopic versus open reintervention for anastomotic leakage following minimally invasive colorectal surgery. Surg Endosc. 2015;29(4):931–6.
Chen WT, Bansal S, Ke TW, Chang SC, Huang YC, Kato T, Wang HM, Fingerhut A. Combined repeat laparoscopy and transanal endolumenal repair (hybrid approach) in the early management of postoperative colorectal anastomotic leaks: technique and outcomes.
Chen YC, Fingerhut A, Tsai YY, Chang SC, Ke TW, Shen MY, Tzu-Liang C. Laparoscopic reintervention for intraperitoneal leaks after colonic surgery: do we need a routine stoma? Surg Innov. 2022.
Fowkes L, Krishna K, Menon A, Greenslade GL, Dixon AR. Laparoscopic emergency and elective surgery for ulcerative colitis. Colorectal Dis. 2008;10(4):373–8.
Panteleimonitis S, Ahmed J, Parker T, Qureshi T, Parvaiz A. Laparoscopic resection for primary and recurrent Crohn’s disease: a case series of over 100 consecutive cases. Int J Surg. 2017;47:69–76.
Sauerland S, Agresta F, Bergamzschi R, Borzellino G, Budzynski A, Champault G, et al. Laparoscopy for abdominal emergencies evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc. 2006;20:14–29.
Keller DS, Pedraza R, Flores-Gonzalez JR, et al. The current status of emergent laparoscopic colectomy: a population-based study of clinical and financial outcomes. Surg Endosc. 2016;30(8):3321–6.
Maggiori L, Panis Y. Surgical management of IBD—from an open to a laparoscopic approach. Nat Rev Gastroenterol Hepatol. 2013;10:297–306.
Sampietro GM, Colombo F, Corsi F. Sequential Approach for a Critical-View COlectomy (SACCO): a laparoscopic technique to reduce operative time and complications in IBD acute severe colitis. J Clin Med. 2020;9(10):3382.
Yanar H, Taviloglu K, Ertekin C, Ozcinar B, Yanar F, Guloglu R, et al. Planned second look laparoscopy in the management of acute mesenteric ischemia. World J Gastroenterol. 2007;13:3350–3.
Misiakos EP, Tsapralis D, Karatzas T, Lidoriki I, Schizas D, Sfyroeras GS, et al. Advents in the diagnosis and management of ischemic colitis. Front Surg. 2017;4:47.
Fingerhut A, Kurihara H, Chen WT. Vascular problems related to colectomy: habitual and variant anatomy, prevention, and tactical aspects. In: Prophylactic surgery. Springer; 2021.
Prevot F, Sabbagh C, Mauvais F, Regimbeau JM. Colectomy in patients with previous colectomy or occlusive vascular diseases: pitfalls and precautions. J Visc Surg. 2016;153:113–9.
Chen YC, Fingerhut A, Shen MY, Chen HC, Ke TW, Chang SJ, Tsai YY, Wang HM, Chen WT. Colorectal anastomosis after laparoscopic extended left colectomy: techniques and outcome. Colorectal Dis. 2020;22:1189–94.
Peixoto A, Silva M, Gaspar R, Morais R, Pereira P, Macedo G, et al. Predictive factors of short-term mortality in ischaemic colitis and development of a new prognostic scoring model of in-hospital mortality. United Eur Gastroenterol J. 2017;5(3):432–9.
Bertani C, Cassinotti E, Della Porta M, Pagani M, Boni L, Baldari L. Indocyanine green—a potential to explore: narrative review. Ann Laparosc Endosc Surg. 2022;7:9. https://doi.org/10.21037/ales-21-5.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Y-CC, T-WK, AF, and WT-LC contributed to conception and design. Y-CC, Y-YT, S-CC, H-CC, T-WK, AF, and WT-LC were involved in acquisition of data. Y-CC, T-WK, AF, and WT-LC contributed to analysis and interpretation of data. Y-CC, Y-YT, S-CC, H-CC, T-WK, AF, and WT-LC were involved in drafting the article or revising it critically for important intellectual content. YCC, Y-YT, S-CC, H-CC, T-WK, AF, and WT-LC contributed to final approval of the version to be published. All authors read and approved final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the departmental and institutional ethical committees of the China Medical University Hospital, Taichung, Taiwan (CMUH110-REC3-067). All procedures were performed in accordance with the relevant guidelines and regulations (for example, Declaration of Helsinki). Informed consent was not required due to retrospective design and granted exemption from IRB review (CMUH110-REC3-067).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, YC., Tsai, YY., Chang, SC. et al. Laparoscopic versus open emergent colectomy for ischemic colitis: a propensity score-matched comparison. World J Emerg Surg 17, 53 (2022). https://doi.org/10.1186/s13017-022-00458-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-022-00458-4