Abstract
Acute mesenteric ischemia (AMI) is a group of diseases characterized by an interruption of the blood supply to varying portions of the intestine, leading to ischemia and secondary inflammatory changes. If untreated, this process may progress to life-threatening intestinal necrosis. The incidence is low, estimated at 0.09–0.2% of all acute surgical admissions, but increases with age. Although the entity is an uncommon cause of abdominal pain, diligence is required because if untreated, mortality remains in the range of 50%. Early diagnosis and timely surgical intervention are the cornerstones of modern treatment to reduce the high mortality associated with this entity. The advent of endovascular approaches in parallel with modern imaging techniques is evolving and provides new treatment options. Lastly, a focused multidisciplinary approach based on early diagnosis and individualized treatment is essential. Thus, we believe that updated guidelines from World Society of Emergency Surgery are warranted, in order to provide the most recent and practical recommendations for diagnosis and treatment of AMI.
Similar content being viewed by others
Background
Acute mesenteric ischemia (AMI) is caused by sudden interruption of blood supply to the intestine, leading to cellular damage, intestinal necrosis, and commonly patient death if untreated [1]. AMI may be occlusive or non-occlusive (NOMI), with the primary etiology further defined as mesenteric arterial embolism (50%), mesenteric arterial thrombosis (15–25%), or mesenteric venous thrombosis (5–15%) [2, 3]. The overall incidence is low (0.09–0.2% of all acute admissions to emergency departments), representing an infrequent cause of abdominal pain [4,5,6], but a common cause of emergent intestinal resection. Prompt diagnosis and intervention are essential to reduce the mortality rates that exceed 50% [7,8,9,10].
Traditionally, AMI has been treated with open surgery. Over the past two decades, the rapid development of endovascular techniques has made this approach an important alternative for patients with occlusion of the superior mesenteric artery (SMA). Some studies have shown that endovascular therapy is associated with lower rates of mortality and bowel resection than the traditional, open approach [11,12,13].
The assessment and therapy carried out by an interdisciplinary team should keep the time-to-reperfusion interval as short as possible. In addition, advances in postoperative care have improved outcome for patients with short bowel syndrome [14, 15]. Both in-hospital care and further bowel rehabilitation lead to increase survival and better long-term outcome with acceptable quality of life [16, 17].
Introducing a clinical pathway and centers of excellence results in higher awareness of AMI, more appropriate imaging, less delays, increased number of revascularizations, and, therefore, lower mortality [18, 19].
Accordingly, the present paper aims to provide an update with recommendations based on the most currently accepted concepts in the management of AMI [20].
Methods
The World Society of Emergency Surgery (WSES) endorsed a team of experts to develop specific questions about diagnosis and management of AMI. This group performed a thorough literature review and presented its findings during the WSES World Congress, September 2021 in Edinburg, Scotland. The quality of the evidence available was evaluated according to the GRADE methodology, and recommendations were classified into two levels: strong recommendation in favor or against; weak recommendation (suggestion) in favor or against. [21,22,23,24]
During the Congress, the Board of the Society approved the proposed statements. After the acceptance, the update of the guidelines was further discussed by the Board of the WSES and approved.
Pathophysiology and epidemiology
Acute mesenteric arterial embolism
Half of cases of AMI are due to acute SMA embolism [2, 3]. Mesenteric emboli can originate from the left atrium (e.g., atrial fibrillation), left ventricle (e.g., left ventricular dysfunction with poor ejection fraction), or cardiac valves (e.g., endocarditis). Occasionally emboli are generated from an atherosclerotic aorta. Emboli typically lodge at points of normal anatomic artery narrowing. The SMA is particularly vulnerable because of its relatively large diameter and low takeoff angle from the aorta. The majority of emboli lodge 3–10 cm distal to the origin of the SMA, thus sparing the proximal jejunum and colon. More than 20% of SMA emboli are associated with concurrent emboli to another arterial bed including the spleen and kidney [25].
Acute mesenteric arterial thrombosis
Thrombosis of the SMA (approximately 25% of cases) is usually associated with pre-existing chronic atherosclerotic disease leading to stenosis. Many of these patients have a history consistent with chronic mesenteric ischemia (CMI), including postprandial pain, weight loss, or “food fear.” A detailed medical history is important when evaluating a patient suspected to have AMI. Thrombosis usually occurs at the origin of visceral arteries. An underlying plaque in the SMA usually progresses eventually to a critical stenosis resulting in collateral beds. Accordingly, symptomatic SMA thrombosis most often accompanies celiac occlusion [26]. SMA thrombosis may also occur due to vasculitis, mesenteric dissection, or mycotic aneurysm. Involvement of the ileocolic artery will result in necrosis of the proximal colon.
Acute non-occlusive mesenteric ischemia
NOMI occurs in approximately 20% of cases, and is usually a consequence of SMA vasoconstriction associated with low splanchnic blood flow [27]. The compromised SMA blood flow also affects the proximal colon due to involvement of the ileocolic artery. Patients with NOMI typically suffer from severe coexisting illness, commonly cardiac failure which may be precipitated by sepsis. Hypovolemia and the use of vasoconstrictive agents may precipitate NOMI.
Mesenteric venous thrombosis
Mesenteric venous thrombosis (MVT) accounts for less than 10% of cases of mesenteric infarction. Thrombosis is attributed to a combination of Virchow’s triad; stagnant blood flow, hypercoagulability, and endothelial damage. In young patients, 36% of MVT occurs without an obvious cause [28]. An inflammatory process around the superior mesenteric vein (SMV) due to acute pancreatitis or inflammatory bowel disease may cause thrombosis. Surgical trauma such as splenectomy or bariatric surgery may also provoke SMV thrombosis. Hypercoagulability may be due to inherited disease such as Factor V Leiden, prothrombin mutation, protein S deficiency, protein C deficiency, antithrombin deficiency, and antiphospholipid syndrome. Additionally, recent work suggests that fibrinolysis shutdown (resistance to tissue plasminogen activator—tPA) is a significant risk factor for hypercoagulability [29]. Thrombophilia may also be acquired due to malignancies, hematologic disorders, and oral contraceptives [30].
Recent trends: prevalence, pathophysiology
The prevalence of AMI has changed in recent decades. The prevalence of acute mesenteric occlusion among patients with an acute abdomen may vary from 17.7% in emergency laparotomy and 31.0% in laparotomy for elderly non-trauma patients [31].
Mesenteric arterial embolism decreased to 25% of cases [3, 32]. Mesenteric arterial thrombosis was the second most common cause of mesenteric ischemia, which historically accounted for 20–35% and recently increased to 40% [32]. NOMI accounts for 25% of cases [3], which is also increasing, compared to the historical cohort, because of increased number of critically ill patients and overall improvement of intensive care. Although the mechanism is still unknown, heart failure, renal failure, cardiac surgery using cardiopulmonary bypass, and the use of catecholamine are reported as risk factors [33].
The etiology of AMI has changed over the years with increasing percentages of acute arterial thrombosis due to atherosclerosis which may in part be explained by modern anticoagulant therapy used for the treatment of atrial fibrillation.
The incidence of AMI increases exponentially with age. In patients aged 75 years or older, AMI is a more prevalent cause of acute abdomen than appendicitis [1]. The incidence of AMI in an 80-year-old is roughly tenfold that of a 60-year-old patient [34].
Abdominal compartment syndrome with very high intraabdominal pressure may cause bowel ischemia that is complicated with ischemia–reperfusion injury when decompression laparotomy is performed [35].
AMI has been described in patients with coronavirus disease (COVID -19), probably related to large vessel thromboembolic events as well as to small vessel thrombosis linked to hypercoagulability and fibrinolysis shutdown [36].
-
1.
Severe abdominal pain out of proportion to physical examination findings should be assumed to be AMI until disproven. (Strong recommendation based on low-quality evidence 1C)
The key to early diagnosis is a high level of clinical suspicion.
The clinical scenario of a patient complaining of excruciating abdominal pain with an unrevealing abdominal examination is classic for early AMI [37]. The reason for the pain being disproportionate to the clinical findings is that ischemia starts from the mucosa toward the serosa. That is why initially there is severe pain without clinical findings.
If the physical examination demonstrates signs of peritonitis, there is likely irreversible intestinal ischemia with bowel necrosis. In a study on AMI, 95% of patients presented with abdominal pain, 44% with nausea, 35% with vomiting, 35% with diarrhea, and 16% with blood per rectum [38]. Approximately, one-third of patients present with the triad of abdominal pain, fever, and hemoccult-positive stool. Other patients, particularly those with delayed diagnosis, may present in extremis with septic shock. Clinical signs of peritonitis may be subtle. Accordingly, one must have a high index of suspicion, because such findings are predictive of intestinal infarction.
The classic presentation of AMI, i.e., “severe, poorly localized abdominal pain that is out of proportion to the physical examination,” is becoming less common, while the “acute on chronic” presentations of mesenteric ischemia are more typical, and probably underdiagnosed [39]. Patients presenting with symptomatic chronic mesenteric ischemia are at high risk of developing in-hospital AMI.
Severe COVID-19 infection and AMI have a poor prognosis, delay in diagnosis, and intervention [40,41,42]. AMI should be suspected in patients with COVID-19 who present with nausea, vomiting, diarrhea, abdominal pain, and abdominal distension because of hypercoagulability and hypoperfusion. Blood tests will not aid in the diagnosis of AMI, though essential in patient management. CTA is the diagnostic modality of AMI along with clinical correlation.
-
2.
Clinical scenario and risk factors differentiate AMI as mesenteric arterial emboli, mesenteric arterial thrombosis, NOMI, or mesenteric venous thrombosis. (Weak recommendation based on low-quality evidence 1C)
Types of AMI
A careful medical history is important because distinct clinical scenarios are associated with the pathophysiological form of AMI [43]. Patients with mesenteric arterial thrombosis often have a history of chronic postprandial abdominal pain, progressive weight loss, and previous revascularization procedures for mesenteric arterial occlusion. Patients with NOMI have pain that is generally more diffuse and episodic associated with poor cardiac performance. These patients are more likely to have suffered from cardiac failure, and recent surgery. Several other smaller cohorts also reported hemodialysis as a risk factor of NOMI [44, 45]. Furthermore, NOMI represents a cause of secondary worsening in septic shock, particularly in septic patients treated with high-dose vasoactive drugs.
Patients with MVT present with a mixture of nausea, vomiting, diarrhea, and abdominal cramping. Gastrointestinal bleeding occurs in 10% [46].
Nearly 50% of patients presenting with embolic AMI have atrial fibrillation, and approximately one-third of patients have a prior history of arterial embolus with preexisted peripheral vascular disease [38].
Risk factors for specific phenotypes of AMI are presented in Table 1..
-
3.
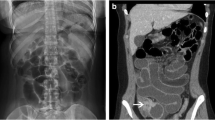
Plain X-ray is not recommended in evaluating patients for intestinal ischemia. (Strong recommendation based on moderate-quality evidence 1B)
A radiograph is usually the initial test ordered in patients with acute abdominal pain but has a limited role in the diagnosis of mesenteric ischemia, especially in the early setting. A negative radiograph does not exclude mesenteric ischemia [47]. Plain radiography only becomes positive when bowel infarction has developed and intestinal perforation manifests as free intraperitoneal air.
-
4.
There are no laboratory parameters that are sufficiently accurate to conclusively identify the presence or absence of ischemic or necrotic bowel, although elevated l-lactate, leukocytosis, and D-dimer may assist. (Weak recommendation based on moderate-quality evidence 2B)
Although laboratory results are not definitive, they may help to corroborate clinical suspicion. More than 90% of patients will have an abnormally elevated leukocyte count [48]. The second most commonly encountered abnormal finding is metabolic acidosis with elevated lactate level, which occurs in 88% [49].
Patients may present with lactic acidosis due to dehydration and decreased oral intake. Thus, differentiation of early ischemia versus irreversible bowel injury based upon the lactate level alone is not reliable unless accompanied by other clinical evidence. Elevated serum lactate levels > 2 mmol/l is associated with irreversible intestinal ischemia hazard ratio: 4.1 (95% CI: 1.4–11.5; p < 0.01) in case of AMI [50].
It should be emphasized that the presence of lactic acidosis in combination with abdominal pain when the patient may not otherwise appear clinically ill should lead to consideration of early CTA.
Based on the current literature, no accurate biomarkers have been identified to diagnose AMI [51, 52]. D-dimer has been reported to be an independent risk factor for intestinal ischemia [52], reflecting ongoing clot formation and endogenous degradation via fibrinolysis. No patient presenting with a normal D-dimer had intestinal ischemia and D-dimer > 0.9 mg/L had a specificity, sensitivity, and accuracy of 82%, 60%, and 79%, respectively [53]. Thus, D-dimer may be useful in the early assessment.
Elevated amylase has been reported in roughly a half of patients with AMI. [54] This is important to note to as patient may be misdiagnosed as having acute pancreatitis, and delay in critical interventions could impact survival outcomes.
Other biomarkers reported to be of use in the diagnosis of AMI include intestinal fatty acid-binding protein (I-FABP), serum alpha-glutathione S-transferase (alpha-GST), and cobalt–albumin binding assay (CABA) [55, 56]. A cross-sectional diagnostic study of 129 patients admitted for acute abdominal pain found that the three most promising circulating biomarkers for AMI—citrulline, I-FABP, and d-lactate—were neither sensitive nor specific enough for the differential diagnosis of AMI [57].
These results, however, contrast with other published reports [56, 58]. This could be explained by selection bias (established severe AMI cases were included) leading to an overestimated performance of the studied biomarkers.
-
5.
Computed tomography angiography (CTA) should be performed without delay in any patient with suspicion for AMI. (Strong recommendation based on high-quality evidence 1A)
Delay in diagnosis is the dominant factor that accounts for high mortality rates of 30–70% despite increased knowledge of this entity [59, 60]. Every 6 h of delay in diagnosis (actually—delay in CTA) doubles mortality [61]. The multidetector CTA has replaced formal angiography as the diagnostic study of choice. Volume rendering is now a semiautomatic workflow component of many CT machines. These can aid remote communities with less experienced staff.
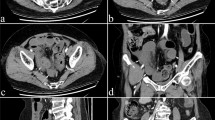
In the presence of advanced AMI, the CTA findings reflect irreversible ischemia (intestinal dilatation and thickness, reduction or absence of visceral enhancement, pneumatosis intestinalis, and portal venous gas, especially the combination of all) and free intraperitoneal air [62].
Comprehensive biphasic CTA includes the following important steps:
-
(a)
Pre-contrast scans to detect vascular calcification, hyper-attenuating intravascular thrombus, and intramural hemorrhage.
-
(b)
Arterial and venous phases to demonstrate thrombus in the mesenteric arteries and veins, abnormal enhancement of the bowel wall, and the presence of embolism or infarction of other organs.
-
(c)
Multiplanar reconstructions (MPR) to assess the origin of the mesenteric arteries [63].
The oral contrast is not indicated and even harmful. CTA should be performed despite the presence of acute kidney injury, as the consequences of delayed or missed diagnosis are far more detrimental for patients than exposure to the iodinated contrast agent. A recent study found that in 27 of 28 patients (96.4%) MDCT correctly diagnosed AMI (specificity of 97.9%) [27, 64]. A sensitivity of 93%, specificity of 100%, and positive and negative predictive values of 100% and 94%, respectively, were achieved [65, 66].
Six radiological findings (bowel loop dilatation, pneumatosis intestinalis, SMV thrombosis, free intraperitoneal fluid, portal vein thrombosis, and splenic vein thrombosis) were found to be predictors of bowel necrosis in patients with AMI [67]. The clinical significance of pneumatosis intestinalis as a single radiological finding remains the challenge. In a biggest multicentral retrospective study, 60% of patients had benign disease [68].
In NOMI, CTA may demonstrate bowel ischemia and free fluid in the face of patent mesenteric vessels. In MVT, the most common positive radiological finding on venous phase CTA is thrombus in the superior mesenteric vein described as the target sign [69].
Associated findings that suggest MVT include bowel wall thickening, pneumatosis, splenomegaly, and ascites [69]. Portal or mesenteric venous gas strongly suggests the presence of bowel infarction.
Diagnostic angiography can differentiate occlusive, embolic, and thrombotic from non-occlusive AMI.
Duplex ultrasonography has a limited role in this entity, but may be helpful if obtained early in chronic cases [47]. It could be useful to monitor the bowel’s peristalsis or the amount of free peritoneal fluid especially in NOMI.
MRA is an established technique in the evaluation of the mesenteric arterial and venous vasculature in patients with suspected AMI. It has been well accepted for chronic mesenteric ischemia cases and functional assessment of bowel insufficiency as a result of SMA pathology [70]. Nevertheless, its use is limited in the emergency setting.
-
6.
Non-occlusive mesenteric ischemia (NOMI) should be suspected in critically ill patients with abdominal pain or distension requiring vasopressor support and evidence of multiorgan dysfunction. (Weak recommendation based on low-quality evidence 2C)
Clinical examination and routine laboratory tests are of only little value in reaching an early and reliable diagnosis of NOMI. Unexplained abdominal distension or gastrointestinal bleeding may be the only signs of acute intestinal ischemia in NOMI and may be undetectable in sedated patients in the ICU in approximately 25% of cases [71, 72]. Patients surviving cardiopulmonary resuscitation who develop bacteremia and diarrhea should be suspected of having NOMI, regardless of presence or absence of abdominal pain. Right-sided abdominal pain associated with the passage of maroon or bright red blood in the stool is highly suggestive of NOMI.
Gastrointestinal perfusion is often impaired early in critical illnesses, major surgery, or trauma, all of which are characterized by increased demands on the circulation to maintain tissue oxygen delivery [73].
Most of the symptoms listed in this section are often not clinically apparent in a critically ill and ventilated patients. Accordingly, any negative changes in a patient's physiology, including new onset of organ failure, increase in vasoactive support, and nutrition intolerance, should raise the suspicion of AMI.
Experimental and observational studies suggest that the use of vasopressors such as norepinephrine and epinephrine might result in impaired mucosal perfusion [74, 75]. Other pharmacological agents such as vasopressin and digoxin [76] as well as acute profound hypovolemia could also worsen ischemia.
Lastly, the role of enteral nutrition in critically ill patients on development of intestinal ischemia is controversial. In general, enteral and parenteral nutrition is complementary to meet patient’s daily caloric requirements. In the recent randomized controlled trial “NUTRIREA 2” [77], enteral nutrition was compared to parenteral nutrition: Mortality did not differ between the two groups, but a significantly higher rate of bowel ischemia was reported in the enteral group.
-
7.
When the diagnosis of AMI is made, fluid resuscitation should commence immediately to enhance visceral perfusion. Electrolyte abnormalities should be corrected, and nasogastric decompression initiated. (Strong recommendation based on moderate-quality evidence 1B)
Fluid resuscitation with crystalloid and blood products is essential for the management of the patient with suspected AMI. Preoperative resuscitation is important to prevent cardiovascular collapse on induction of anesthesia. To guide effective resuscitation, early hemodynamic monitoring should be implemented [78]. Assessment of electrolyte levels and acid–base status should be performed. This is especially true in patients with AMI, where severe metabolic acidosis and hyperkalemia may result from underlying bowel infarction and reperfusion [79]. Vasopressors should be used with caution. Dobutamine, low-dose dopamine, and milrinone to improve cardiac function have been shown to have less impact on mesenteric blood flow [80, 81]. The fluid volume requirement in these patients may be high, due to extensive capillary leakage, but the infusion of large volume of crystalloid should be utilized carefully to optimize bowel perfusion [82]. The goals of therapy should address physiologic levels of oxygen delivery with continued monitoring of lactate level as an indication of perfusion improvement. Supra-physiologic level of oxygen delivery was suggested in the past which is not supported by the current evidence [83].
-
8.
Broad-spectrum antibiotics should be immediately administered. (Strong recommendation based on moderate-quality evidence 1C)
The high risk of infection among patients with AMI outweighs the risks of acquired antibiotic resistance, and therefore, broad-spectrum antibiotics should be administered early in the course of treatment [84]. Intestinal ischemia leads to early loss of the mucosal barrier, which facilitates bacterial translocation and the risk of septic complications. Antibiotic therapy should be administered for at least 4 days in immunocompetent stable patients with consideration given to a longer duration of therapy for signs of ongoing infection [85]. As soon as possible, antibiotic regimen should be tailored according to the microbial isolation. Prolonged course of empiric antibiotics, if clinically deemed necessary, should be guided in accordance with local antibiotic stewardship team.
-
9.
Prompt laparoscopy/laparotomy should be done for patients with an overt peritonitis. (Strong recommendation based on low-quality evidence 1C)
When physical findings suggestive of an acute intraabdominal catastrophe are present, bowel infarction has already occurred, and the chance of survival in this patient population with significant associated comorbidity is reduced dramatically. Peritonitis secondary to bowel necrosis mandates surgery without delay.
The goal of surgical intervention for AMI includes:
-
1)
Re-establishment of the blood supply to the ischemic bowel.
-
2)
Resection of all non-viable regions.
-
3)
Preservation of all viable bowel.
Intestinal viability is the most important factor influencing outcome in patients with AMI. Non-viable intestine, if unrecognized, results in multisystem organ dysfunction and ultimately death. Prompt laparotomy allows for direct assessment of bowel viability.
Emergency laparotomy
After initial resuscitation, midline laparotomy should be performed, followed by the assessment of all areas of the intestine with decisions for resection of all frankly necrotic areas. The SMA is easily palpated by placing fingers behind the root of the mesentery. The SMA is identified as a firm tubular structure, which may have or not a palpable pulse. Otherwise, the SMA can also be reached by following the middle colic artery where it enters the SMA at the mesentery. Direct sharp dissection, exposing the artery from its surrounding mesenteric tissue, is required for proper exposure to perform revascularization. In cases where there is diagnostic uncertainty, arteriogram is the study of choice. It can be done intraoperatively especially in hybrid suites. Intraoperative duplex is a simple, rapid, repeatable, and often definitive alternative diagnostic modality.
Re-establishment of the blood supply to the ischemic bowel
Revascularization when relevant has an essential role in the multidisciplinary approach to AMI. As an example, among the 104 patients who did not undergo revascularization, 64 (62%) died within 30 days compared to 36 out of 85 (42%) patients who were re-vascularized (p = 0.01) [86].
Different techniques of blood flow restoration are used depending on the AMI pathophysiology. Embolectomy and angioplasty are a well-established definitive treatment for SMA emboli. On the other hand, thrombosis of the SMA at the origin of the aorta (a common pathology in diffuse atherosclerosis) will require a bypass procedure. Bypass may be performed in either an antegrade fashion from the supraceliac aorta or retrograde fashion from the infrarenal aorta or common iliac arteries. Single-vessel revascularization (SMA) is usually sufficient in the acute setting. However, it increases the magnitude of the procedure and may require prosthetics in the presence of contaminated field. Nowadays endovascular procedures reduce the requirement for surgical bypasses. Thus, multidisciplinary collaborative approach including specialists from multiple disciplines is integral for good clinical outcomes.
Temporary SMA shunting may spare considerable bowel. For patients in extremis, or where the necessary technical skillset is not available, temporary SMA shunting should be considered.
Neither NOMI nor MVT typically requires vascular repair. Full-dose anticoagulation should be initiated on all patients prior to the surgical procedure. Unfractionated heparin is effective and easy to manage, especially in patients with acute kidney failure.
Intraoperative bowel viability assessment
There are limited intraoperative tools to help surgeons in decision making regarding bowel viability, especially in circumstances in which the bowel appears to be “dusky” or threatened but not clearly ischemic. In this case, a temporary abdominal closure via a negative pressure wound therapy device or temporary dressing (custom made with plastic sheets, gauzes, and drains) is convenient in order to provide an opportunity for a second-look surgery. Clear documentation of bowel length is crucial in every operation note.
In addition to traditional surgical inspection of the bowel, available techniques of intraoperative assessment of bowel viability rely on bowel oxygenation, myoelectric activity, and perfusion. The intraoperative absence of any one of these criteria is a sufficient predictor of bowel non-viability.
Many surgeons use their hands and eyes to look for the presence or absence of peristalsis or mesenteric pulsation to evaluate whether blood flow is adequate.
Doppler ultrasonography (DUS) is a safe and noninvasive technique to measure blood flow and is popular for its easiness of use and relatively low cost [87].
Flowmetry with fluorescein dye is currently part of the accepted standard of clinical care for intraoperative assessment of bowel viability. Fluorescein can therefore be used to visualize perfusion in open laparotomies using a Woods Lamp or laparoscopically using an endoscope with appropriate filters [88, 89].
Indocyanine Green (ICG) is a near-infrared (NIR) fluorophore with an emission peak of 832 nm in whole blood [90]. It has been used in the same way as fluorescein, but primarily in the elective surgical setting [91]. ICG utilization in the emergent setting, particularly in AMI, has not been well investigated to date, although early animal models, isolated cases, and cohort studies show promise.
The potential for combining modalities for intraoperative bowel assessment warrants further studies [92].
Laparoscopy in AMI
Diagnostic laparoscopy is feasible as a bedside procedure in the intensive care unit (ICU) with the advantage of avoiding time delay for awaiting operating room availability and preventing adverse events during critically ill patients transfer. However, the routine use of diagnostic laparoscopy in AMI has not been generally adopted [6].
When a second-look surgery is indicated, second-look laparoscopy may be a useful alternative to conventional surgery, because it prevents critically ill patients from the trauma and risks of relaparotomy and can be performed as an ICU bedside operation. In one study, only 20% of patients underwent a second-look laparoscopy within first 72 h, but this did not change the outcome and complication rate [93]. In another case series, non-therapeutic laparotomy was avoided in 9/20 patients with NOMI [94].
The European Association for Endoscopic Surgery (EAES) consensus for the laparoscopic approach to the acute abdomen states that there is no published data demonstrating advantages in the diagnosis and treatment of acute bowel ischemia by laparoscopy [95]. However, laparoscopy can be useful in confirming the diagnosis in doubtful cases, evaluate the extension of the ischemic small bowel segment, and offer a treatment option in cases of segmental necrosis.
In addition, post-cardiac surgery patients admitted to the ICU have a relatively high rate of NOMI, where the CT-scan can be equivocal. In these cases, bedside diagnostic laparoscopy may be a safe and effective procedure that avoids needless laparotomy and can direct further management steps [96].
-
10.
Endovascular revascularization procedures are the primary option in cases of arterial occlusion when sufficient expertise is available. (Strong recommendation based on low-quality evidence 1C)
Endovascular techniques have become popular in revascularization of the SMA. No randomized control trial has been performed to assess and compare open surgery to an endovascular approach, as patients with AMI are very heterogenic and physiologically different [97]. Much controversy surrounds the use of endovascular techniques as primary management of AMI [98]. Some studies report lesser need for laparotomy, less bowel resection, and significantly lower mortality rate with endovascular techniques compared to surgery [99].
Open surgery is effective in assessing the viability of the bowel and hence preventing delay in revascularization especially when an endovascular approach is unavailable [1].
Different endovascular procedures are summarized in Table 2.
Comparison of endovascular intervention and surgery
Publications related to endovascular treatment of AMI have been evolving since 2010 [11, 12]. Several observational studies and meta-analyses comparing the outcomes of endovascular interventions and surgery have been published [13, 107,108,109,110].
All studies have shown a benefit for endovascular therapy compared to open surgery in terms of lower bowel resection rates and lower 30-day mortality rates.
The latest study using the National Inpatient Sample database included 4665 patients who underwent interventional treatment (24% endovascular and 76% open revascularization) from 2005 through 2009 showed that endovascular intervention is associated with lower mortality compared to open surgery (24.9% vs 39.3%) [111]. Another meta-analysis including nineteen observational studies also showed that endovascular intervention was associated with a lower prevalence of bowel resection (OR 0.45, 95%CI 0.34–0.59) and 30-day mortality (OR 0.45, 95%CI 0.34–0.59) compared with open surgery [112].
The Guidelines of the European Society of Vascular Surgery showed a pooled overall 30-day mortality rate after endovascular therapy of 17.2% (367/2131), compared to 38.5% after open surgery (1582/4111) [113].
It is important to note that all studies that were focused on endovascular revascularization have high levels of heterogeneity. It is possible that patients undergoing open repair have more advanced disease resulting in long-segment bowel resection rates and poorer outcome. The 5-year survival following endovascular treatment and open vascular surgery was 40% and 30%, respectively [108].
The pooled estimate of technical success of endovascular intervention was 94%, based on a recent meta-analysis [100]. On the other hand, the pooled estimate of the unplanned surgery rate of endovascular therapy was 40%.
In patients with acute embolic SMA occlusion, there are no data suggesting a superiority of open versus endovascular treatment [114].
Aspiration embolectomy with thrombolytic treatment should be considered in patients with no clinical signs of acute peritonitis. In a study that analyzed the Swedish Vascular Registry (SWEDVASC) between 1987 and 2009, 34 patients that received thrombolysis for acute SMA occlusion were identified. In-hospital mortality was 26%, and technical success was 88%. Patients who needed explorative laparotomy after lysis had an in-hospital mortality rate of 38% [102].
Hybrid approach: endovascular intervention and surgery
Retrograde open mesenteric stenting (ROMS) is an emerging hybrid technique utilized in cases of AMI. This procedure includes a laparotomy and retrograde endovascular revascularization of the superior mesenteric artery [115]. One of the advantages of this method over vascular bypass is significantly shorter operative time. One of the major concerns after stenting is patency. However, patency rates similar to bypass were reported (76–88%) [116].
Theoretically, if technical capabilities and infrastructure for hybrid procedures are available, ROMS may be a good treatment option for patients who require laparotomies. It is possible that ROMS may avoid the need for second-look surgeries.
Centers of excellence equipped with hybrid operating rooms may provide further data supporting the use of an endovascular strategy [117]. The raised awareness of AMI, low threshold for suspicion, immediate CTA with real-time radiology report, and early involvement of senior staff members are increase rapid access and utilization of hybrid operating rooms.
-
11.
Damage control surgery (DCS) with temporary abdominal closure is an important adjunct for patients who require intestinal resection allowing reassessment of bowel viability and in situations of severe abdominal sepsis. (Strong recommendation based on low-quality evidence 1B)
The damage control laparotomy strategy (abbreviated laparotomy) is an accepted technique in trauma care for the past 30 years. It is an important option in the patient with AMI [118]. Damage control is the surgical modality of choice in the critically ill patient with AMI for physiological and technical reasons. The decision to utilize DCS should be made early based upon the response to resuscitation [119]. Advanced age is not a contraindication to DCS as good outcomes have been observed in the elderly [120].
Planned second-look techniques are required after restoration of SMA flow, with or without resection of ischemic bowel (and no anastomosis or stoma) following resuscitation in the ICU [120, 121]. If there is an uncertainty regarding bowel viability, the stapled off bowel ends should be left in discontinuity and re-inspected after a period of continued ICU resuscitation to restore physiological balance. Often, bowel which is borderline ischemic at the initial exploration will improve after restoration of blood supply and physiologic stabilization. Multiple adjuncts have been suggested to assess intestinal viability, but none have proven to be uniformly reliable [122, 123].
Most often, re-exploration should be accomplished within 24–48 h and decisions regarding anastomosis, stoma, or additional resection can be made with plans for sequential abdominal closure.
In a review of 43 patients undergoing open mesenteric revascularization, the authors noted that 11 of the 23 patients undergoing a second-look operation required bowel resection [32]. The bowel in these patients is often very swollen and poses a high risk for anastomotic leak. Recent studies suggest that careful hand sewn techniques are preferable to staples use in this group [124, 125].
These patients often suffer from acidosis, hypothermia, and coagulopathy, which require prompt and ongoing correction. Physiologic restoration is multifactorial and includes careful and limited crystalloid infusion to avoid abdominal compartment syndrome, frequent monitoring of lactate clearance and central venous oxygen saturation, and the use of viscoelastic techniques (TEG, ROTEM) to assess coagulation status and guide ongoing blood product administration. Recent evidence suggests that direct peritoneal resuscitation techniques can be useful in this scenario [126, 127].
-
12.
Mesenteric venous thrombosis can often be successfully treated with a continuous infusion of unfractionated heparin. (Strong recommendation based on moderate-quality evidence 1B)
MVT has a distinctive clinical finding on CTA scan, and when noted in a patient without findings of peritonitis, non-operative management should be considered. The first line treatment for mesenteric venous thrombosis is anticoagulation. Systemic thrombolytic therapy is rarely indicated. When clinical signs demand operative intervention, one should resect only obviously necrotic bowel utilizing damage control techniques since anticoagulation therapy may improve the clinical picture over the ensuing 24–48 h. Early use of heparin has been associated with improved survival [128].
Patients with peritonitis require emergency surgery. Intraoperative management is dictated by the surgical findings ranging from a segmental infarction of small bowel to necrosis of the entire bowel, with or without perforation. The aim of resection is to conserve as much bowel as possible. Second-look laparotomy, 24–48 h later, may avoid the resection of potentially viable bowel. A second-look procedure is mandatory in patients who have extensive bowel involvement.
There are no high-quality studies suggesting that endovascular therapy has a proven role in the treatment of MVT but may be an option in selected patients not responding to anticoagulation therapy. Most published data on interventional radiological treatments for MVT refer to small case series. The use of systemic intravenous tPA has been successfully reported [129]. Thrombolysis via the SMA is ineffective and associated with an increased risk of bleeding [130]. The role of open surgical thrombectomy in modern practice is uncertain [131].
Supportive measures include nasogastric suction, fluid resuscitation, and bowel rest.
-
13.
When NOMI is suspected, the focus is to correct the underlying cause and improve mesenteric perfusion. Infarcted bowel should be resected promptly. (Strong recommendation based on low-quality evidence 1C).
The central principle of NOMI management is the treatment of the underlying precipitating cause. Fluid resuscitation, optimization of cardiac output, and elimination of vasopressors remain important primary measures. Additional treatment may include systemic anticoagulation (heparin) and the use of catheter-directed infusion of vasodilatory and antispasmodic agents, most commonly papaverine hydrochloride [132]. The decision to intervene surgically is based on the presence of peritonitis, perforation, or overall worsening of the patient’s condition [81].
If a patient presents with peritoneal signs, an exploratory laparotomy is required for resection of frankly necrotic bowel. Unfortunately, these patients are often in critical condition and the mortality remains very high (50–85%) [9]. Damage control surgery is an important adjunct, given the critical state of these patients.
Direct vasodilator treatment is not commonly used in real-world practice. Despite several clinical guidelines mentioning vasodilator therapy for NOMI [133,134,135], only a few small studies have been published [136, 137]. Direct vasodilator infusion of papaverine into the SMA showed reduced mortality associated with AMI [138]. Another study demonstrated that early treatment with continuous IV prostaglandin E1 (PGE1) reduced mortality in patients with NOMI [136].
A nationwide study from Japan focused on vasodilator therapy using papaverine, and/or PGE1 in NOMI patients (161 patients vs. 1676 in control group) showed vasodilator therapy was associated with significantly lower in-hospital mortality and need for abdominal surgery [139]. This was a highly selected patient cohort with mild disease.
-
14.
Postoperative intensive care of AMI patients is directed toward the improved intestinal perfusion and the prevention of a multiple organ failure. (Strong recommendation based on low-quality evidence 1C)
Release of toxic products following bowel resection and restoration of blood flow induce inflammatory processes that can lead to multiorgan failure (MOF) even in the absence of necrotic bowel. Capillary leakage resulting from reperfusion injury leads to volume sequestration into the third space. Systemic hypotension often requires catecholamine administration.
In such a scenario, depending on cardiac output and peripheral vascular resistance, a combination of noradrenaline and dobutamine rather than vasopressin should be considered to minimize the possible negative impact on the intestinal microcirculation [140]. Renal replacement therapy, which is often required in case of acute kidney injury, may contribute to hemodynamic stabilization and facilitate optimization of fluid balance. Because of the potential bacterial translocation from the injured gut, broad-spectrum antibacterial treatment according to current guidelines should be continued after surgery based upon the degree of contamination and culture results [141]. Systemic heparin is administered postoperatively (with activated partial thromboplastin time (aPTT) between 40 and 60) in all patients. Low-molecular weight heparin (LMWH) in therapeutic doses is a good alternative if no surgical interventions are planned. Enteral feeding is preferred, but some patients may need parenteral nutrition for a prolonged time due to short bowel and intestinal failure.
-
15.
Treatment of AMI is optimal in a dedicated center using a focused care bundle and a multidisciplinary team. (Strong recommendation based on low-quality evidence 1C)
Recent published evidence suggests that treatment of occlusive AMI in “intestine stroke centers” using a multidisciplinary approach improves outcomes [142, 143]. Improving survival rates can be obtained if mesenteric ischemia is diagnosed and treated early. The goal of multidisciplinary approach is to keep the time to reperfusion as short as possible. The team often includes general surgeon (preferably an emergency surgery specialist), vascular surgeon, interventional radiologist, and intensivist. The concept of “intestinal stroke centers” has been promulgated in France and in China [144, 145].
Dedicated “intestinal stroke centers” have highlighted the effectiveness of a multidisciplinary approach focusing on: (1) removal of non-viable ischemic bowel, (2) preservation of intestine with revascularization, and (3) intensive care treatment to prevent progression to multiorgan failure. Utilizing this approach, Corcos et al. reported a 30-day survival of 95% in a small single-center study involving 18 patients presenting with occlusive AMI [146].
Recently, an implemented pathway and care bundle for patients with suspected AMI was introduced in Meilahti Helsinki University Hospital [18]. The key aspects of the “bundle” were elevated awareness, rapid diagnostics, and interventions including hybrid OR with endovascular treatment capacity. Patients treated under the bundle protocol were more often diagnosed with CT, had shorter mean in-hospital delay to operating room (median 3 h), and had revascularization done more often. The thirty-day mortality was lower in this group [17 (25%) compared with 23 (51%), p = 0.001] [18].
Well-designed multidisciplinary teams tend to optimize perioperative care for all involved patients. This includes patients with non-favorable prognosis. Efforts to improve surgical care should employ multidisciplinary teams to promote both quality and cost-effective care.
The management of patients with AMI is summarized in Fig. 1
-
16.
Patients with short bowel syndrome following extensive bowel resection should have restoration of digestive continuity in association with hormonal therapy to optimize absorptive function and achieve nutritional autonomy. (Weak recommendation, low-quality evidence 1C)
The loss of large amounts of small bowel due to AMI can result in short bowel syndrome (SBS) and intestinal failure. SBS is associated with poor quality of life and a morbidity, which increases with age and comorbidities [147]. Management of patients with SBS can be challenging, especially in case of ostomies with associated large fluid losses and electrolyte imbalances [148]. Studies have shown that sparing the ileocecal valve and the colon is associated with nutritional independency in adults with SBS.
Recently, the use of synthetic growth agents such as the Glucagon-like peptide-2 (GLP-2) analog teduglutide has substantially changed the management of intestinal failure [149]. Multiple studies have shown that the use of a GLP-2 analog allowed a significant reduction of total parenteral nutrition (TPN) dependence and improved quality of life in patients with intestinal failure [150, 151].
Restoration of bowel continuity following extensive resection will improve functional outcome. If gastrointestinal tract reconstruction is not feasible, patients should be referred early for intestinal transplantation.
-
17.
In case of massive gut necrosis, a careful assessment of the patients underlying comorbidities and advanced directives is advisable to find the optimal therapeutic strategy which could include palliation. (Weak recommendation, low-quality evidence 1C)
In cases of extensive infarction of most of the small bowel with or without a portion of the colon, the surgeon could face an ethical decision whether to do anything. Resection of the entire involved bowel will result in SBS with serious consequences.
The group from the Massachusetts General Hospital observed a decrease in the percentage of patients who underwent operative management of AMI over the last 25 years. This was correlated with an increase in the number of documented increased rates of “comfort measures only” status prior to surgical intervention from 50 to 70% [86].
Surgery may not be the best solution especially in elderly frail patients unable to tolerate long-term parenteral nutrition. In this regard, a preoperative discussion with the patient and their family is essential in guiding clinical decisions [152]. Shared decision making is very appropriate for this situation.
-
18.
Patients undergoing revascularization should have surveillance imaging and long-term anticoagulation. (Strong recommendation based on moderate-quality evidence 1B)
The majority of patients treated for AMI will require lifelong anticoagulant/antiplatelet therapy to prevent relapse. In patients following endovascular stent placement, clopidogrel is administered for 6 months and acetylsalicylic acid as lifelong maintenance treatment. However, there is no scientific data on dual antiplatelet therapy after SMA stenting and the recommendation is based on experience from coronary interventions. When recovered following acute illness, most patients can switch to direct oral anticoagulants (DOACs) or vitamin K antagonists (VKA). Anticoagulation is given for 6 months, but most patients with underlying hypercoagulability should be considered for lifelong anticoagulation [113].
Continued surveillance for stent or graft restenosis is important, as AMI after mesenteric revascularization accounts for 6–8% of late deaths [153].
Patients undergoing revascularization should have surveillance imaging obtained via CTA or duplex ultrasound within 6 months, with frequent follow-up to enable early intervention for recurrent disease [135]. Current Society for Vascular Surgery guidelines recommend duplex ultrasonography at 1, 6, and 12 months after the intervention, and then annually thereafter [154].
Long-term care should be focused on the patient’s underlying medical comorbidities in order to minimize the risk of relapse. Lifestyle modification as well as management of hyperlipidemia, hypertension, and diabetes is necessary.
All established statements and recommendations are presented in Additional file 1: Table S3.
Conclusions
AMI is a serious surgical emergency. The most important message is to have a high index of suspicion based on the combination of history of abrupt onset of abdominal pain, acidosis, and organ failure. This clinical scenario should prompt imaging (CTA) in order to establish the diagnosis. In parallel with rapid resuscitation and after careful assessment of the CTA, the patient should be explored to assess bowel viability, re-establish vascular flow, and resect non-viable bowel.
In the operating room, a focus on revascularization should take priority.
Classically open revascularization approaches have been used and described, in combination with damage control laparotomy. Recent developments, with improvement in early diagnosis, have allowed endovascular techniques to be implemented. Although evidence for the impact of endovascular interventions is limited at this time, they have apparent advantages over open surgery in some patients.
Preliminary evidence suggests that treatment of AMI in especially dedicated centers using a multidisciplinary approach improves outcomes. The evaluation and treatment of these patients by an interdisciplinary team reduce the time to reperfusion as short as possible.
Availability of data and materials
Not applicable.
Abbreviations
- AMI:
-
Acute mesenteric ischemia
- NOMI:
-
Non-occlusive mesenteric ischemia
- WSES:
-
World Society of Emergency Surgery
- CTA:
-
Computed tomography angiography
- SMA:
-
Superior mesenteric artery
- CMI:
-
Chronic mesenteric ischemia
- MVT:
-
Mesenteric venous thrombosis
- SMV:
-
Superior mesenteric vein
- VTE:
-
Venous thromboembolism
- tPA:
-
Tissue plasminogen activator
- I-FABP:
-
Intestinal fatty acid-binding protein
- alpha-GST:
-
Serum alpha-glutathione S-transferase
- CABA:
-
Cobalt–albumin binding assay
- MDCT:
-
Multidetector computed tomography
- MPR:
-
Multiplanar reconstructions
- DUS:
-
Doppler ultrasonography
- ICG:
-
Indocyanine green
- NIR:
-
Near-infrared fluorophore
- ICU:
-
Intensive care unit
- ROMS:
-
Retrograde open mesenteric stenting
- DCS:
-
Damage control surgery
- TEG, ROTEM:
-
Viscoelastic techniques
- PGE1:
-
Prostaglandin E1
- MOF:
-
Multiorgan failure
- aPTT:
-
Activated partial thromboplastin time
- LMWH:
-
Low-molecular weight heparin
- SBS:
-
Short bowel syndrome
- GLP-2:
-
Glucagon-like peptide-2
- TPN:
-
Total parenteral nutrition
- DOACs:
-
Direct oral anticoagulants
- VKA:
-
Vitamin K antagonists
References
Patel A, Kaleya RN, Sammartano RJ. Pathophysiology of mesenteric ischemia. Surg Clin North Am. 1992;72:31–41.
Acosta S. Mesenteric ischemia. Curr Opin Crit Care. 2015;21:171–8.
Clair DG, Beach JM. Mesenteric ischemia. N Engl J Med. 2016;374:959–68.
Acosta S, Bjorck M. Acute thrombo-embolic occlusion of the superior mesenteric artery: a prospective study in a well-defined population. Eur J Vasc Endovasc Surg. 2003;26:179–83.
Duran M, Pohl E, Grabitz K, Schelzig H, Sagban TA, Simon F. The importance of open emergency surgery in the treatment of acute mesenteric ischemia. World J Emerg Surg. 2015;26(10):45.
Stoney RJ, Cunningham CG. Acute mesenteric ischemia. Surgery. 1993;114:489–90.
Chang RW, Chang JB, Longo WE. Update in management of mesenteric ischemia. World J Gastroenterol. 2006;12:3243–7.
Horton KM, Fishman EK. Multidetector CT angiography in the diagnosis of mesenteric ischemia. Radiol Clin North Am. 2007;45:275–88.
Schoots IG, Koffeman GI, Legemate DA, Levi M, van Gulik TM. Systematic review of survival after acute mesenteric ischaemia according to disease aetiology. Br J Surg. 2004;91:17–27.
Beaulieu RJ, Arnaoutakis KD, Abularrage CJ, Efron DT, Schneider E, Black JH. Comparison of open and endovascular treatment of acute mesenteric ischemia. J Vasc Surg. 2014;59:159–64.
Naazar AA, Omair A, Chu SH, Keane KG, Weber DG. A shifting trend towards endovascular intervention in the treatment of acute mesenteric ischemia. Cureus. 2021;13(10):e18544. https://doi.org/10.7759/cureus.18544.
Acosta-Mérida MA, Marchena-Gómez J, Saavedra-Santana P, Silvestre-Rodríguez J, Artiles-Armas M, Callejón-Cara MM. Surgical outcomes in acute mesenteric ischemia: has anything changed over the years? World J Surg. 2020;44(1):100–7.
Arthurs ZM, Titus J, Bannazadeh M, Eagleton MJ, Srivastava S, Sarac TP, et al. A comparison of endovascular revascularization with traditional therapy for the treatment of acute mesenteric ischemia. J Vasc Surg. 2011;53(3):698–704.
Massironi S, Cavalcoli F, Rausa E, Invernizzi P, Braga M, Vecchi M. Understanding short bowel syndrome: current status and future perspectives. Dig Liver Dis. 2020;52(3):253–61.
Kelly DG, Tappenden KA, Winkler MF. Short bowel syndrome. J Parenter Enteral Nutr. 2013;38:427–37.
Mizushima T, Udagawa E, Hasegawa M, Tazuke Y, Okuyama H, Fernandez J, Nakamura S. Etiologies and treatments of chronic intestinal failure-short bowel syndrome (SBS) in Japanese adults: a real-world observational study. Surg Today. 2022. https://doi.org/10.1007/s00595-022-02469-9.
Harpain F, Schlager L, Hütterer E, Dawoud C, Kirchnawy S, Stift J, Krotka P, Stift A. Teduglutide in short bowel syndrome patients: a way back to normal life? JPEN J Parenter Enteral Nutr. 2022;46(2):300–9. https://doi.org/10.1002/jpen.2272.
Tolonen M, Lemma A, Vikatmaa P, Peltola E, Mentula P, Björkman P, Leppäniemi A, Sallinen V. The implementation of a pathway and care bundle for the management of acute occlusive arterial mesenteric ischemia reduced mortality. J Trauma Acute Care Surg. 2021;91(3):480–8.
Tran LM, Andraska E, Haga L, Sridharan N, Chaer RA, Eslami MH. Hospital-based delays to revascularization increase risk of postoperative mortality and short bowel syndrome in acute mesenteric ischemia. J Vasc Surg. 2022;75(4):1323–33. https://doi.org/10.1016/j.jvs.2021.09.033.
Bala M, Kashuk J, Moore EE, Kluger Y, Biffl W, Gomes CA, Ben-Ishay O, Rubinstein C, Balogh ZJ, Civil I, Coccolini F, Leppaniemi A, Peitzman A, Ansaloni L, Sugrue M, Sartelli M, Di Saverio S, Fraga GP, Catena F. Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery. World J Emerg Surg. 2017;7(12):38. https://doi.org/10.1186/s13017-017-0150-5.
Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberati A, Schunemann HJ, Group GW. Going from evidence to recommendations. BMJ. 2008;336:1049–51
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P,Schunemann HJ, Group GW. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Ceresoli M, Coccolini F, Biffl WL, Sartelli M, Ansaloni L, Moore EE, Di Saverio S, Kluger Y, Catena F. WSES guidelines updates. World J Emerg Surg. 2020;15(1):39. https://doi.org/10.1186/s13017-020-00318-z.
Bala M, Kashuk J, Moore EE, Catena F, Leppaniemi A, Ansaloni L, Biffl W, Coccolini F, Peitzman A, Sartelli M, Sugrue M, Fraga GP, Di Saverio S, Kluger Y. Establishing position papers by the WSES. World J Emerg Surg. 2018;15(13):1. https://doi.org/10.1186/s13017-018-0163-8.
Acosta S, Ogren M, Sternby NH, Bergqvist D, Björck M. Clinical implications for the management of acute thromboembolic occlusion of the superior mesenteric artery: autopsy findings in 213 patients. Ann Surg. 2005;241:516–22.
Kärkkäinen JM, Acosta S. Acute mesenteric ischemia (part I) -incidence, etiologies, and how to improve early diagnosis. Best Pract Res Clin Gastroenterol. 2017;31:15–25.
Aschoff AJ, Stuber G, Becker BW, Hoffmann MH, Schmitz BL, Schelzig H, et al. Evaluation of acute mesenteric ischemia: accuracy of biphasic mesenteric multi-detector CT angiography. Abdom Imaging. 2009;34:345–57.
Al-Hilaly MA, Abu-Zidan FM. Mesenteric vein thrombosis: is it one disease? Eur J Vasc Endovasc Surg. 1995;9(1):103–6.
Moore HB, Moore EE, Lawson PJ, Gonzalez E, Fragoso M, Morton AP, Gamboni F, Chapman MP, Sauaia A, Banerjee A, Silliman CC. Fibrinolysis shutdown phenotype masks changes in rodent coagulation in tissue injury versus hemorrhagic shock. Surgery. 2015;158:386–92.
Cohn DM, Roshani S, Middeldorp S. Thrombophilia and venous thromboembolism: implications for testing. Semin Thromb Hemost. 2007;33:573–81.
Khan A, Hsee L, Mathur S, Civil I. Damage-control laparotomy in nontrauma patients: review of indications and outcomes. J Trauma Acute Care Surg. 2013;75(3):365–8.
Marchena-Gómez J, Saavedra-Santana P, Silvestre-Rodríguez J, Artiles-Armas M, Callejón-Cara MM. Surgical outcomes in acute mesenteric ischemia: has anything changed over the years? World J Surg. 2020;44:100–7.
Sakamoto T, Fujiogi M, Matsui H, Fushimi K, Yasunaga H. Clinical features and outcomes of nonocclusive mesenteric ischemia after cardiac surgery: a retrospective cohort study. Heart Vessels. 2020;35:630–6.
Kärkkäinen JM, Lehtimäki TT, Manninen H, et al. Acute mesenteric ischemia is a more common cause than expected of acute abdomen in the elderly. J Gastrointest Surg. 2015;19(8):1407–14.
Smit M, Buddingh KT, Bosma B, Nieuwenhuijs VB, Hofker HS, Zijlstra JG. Abdominal compartment syndrome and intra-abdominal ischemia in patients with severe acute pancreatitis. World J Surg. 2016;40(6):1454–61.
Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan Italy. Thromb Res. 2020;191:9–14. https://doi.org/10.1016/j.thromres.2020.04.024.
Carver TW, Vora RS, Taneja A. Mesenteric ischemia. Crit Care Clin. 2016;32:155–71.
Park WM, Gloviczki P, Cherry KJ Jr, Hallett JW Jr, Bower TC, Panneton JM, Schleck C, Ilstrup D, Harmsen WS, Noel AA. Contemporary management of acute mesenteric ischemia: factors associated with survival. J Vasc Surg. 2002;35:445–52.
Kärkkäinen JM. Acute mesenteric ischemia in elderly patients. Expert Rev Gastroenterol Hepatol. 2016;10(9):985–8.
Kerawala AA, Das B, Solangi A. Mesenteric ischemia in COVID-19 patients: a review of current literature. World J Clin Cases. 2021;9(18):4700–8.
Patel S, Parikh C, Verma D, Sundararajan R, Agrawal U, Bheemisetty N, Akku R, Sánchez-Velazco D, Waleed MS. Bowel ischemia in COVID-19: a systematic review. Int J Clin Pract. 2021;75(12):e14930. https://doi.org/10.1111/ijcp.14930.
Fransvea P, Costa G, Pepe G, La Greca A, Magalini S, Puccioni C, d’Agostino L, Altieri G, Borello A, Cozza V, Sganga G. Acute intestinal ischemia in patients with COVID-19: single-centre experience and literature review. Eur Rev Med Pharmacol Sci. 2022;26(4):1414–29.
Acosta-Merida MA, Marchena-Gomez J, Hemmersbach-Miller M, Roque-Castellano C, Hernandez-Romero JM. Identification of risk factors for perioperative mortality in acute mesenteric ischemia. World J Surg. 2006;30:1579–85.
Endean ED, Barnes SL, Kwolek CJ, Minion DJ, Schwarcz TH, Mentzer RM Jr. Surgical management of thrombotic acute intestinal ischemia. Ann Surg. 2001;233:801–8.
Zeier M, Wiesel M, Rambausek M, Ritz E. Non-occlusive mesenteric infarction in dialysis patients: the importance of prevention and early intervention. Nephrol Dial Transplant. 1995;10:771–3.
Morasch MD, Ebaugh JL, Chiou AC, Matsumura JS, Pearce WH, Yao JS. Mesenteric venous thrombosis: a changing clinical entity. J Vasc Surg. 2001;34:680–4.
Oliva IB, Davarpanah AH, Rybicki FJ, Desjardins B, Flamm SD, Francois CJ, Gerhard-Herman MD, Kalva SP, Ashraf Mansour M, Mohler ER 3rd, Schenker MP, Weiss C, Dill KE. ACR appropriateness criteria ® imaging of mesenteric ischemia. Abdom Imaging. 2013;38:714–9.
Kärkkäinen JM. Acute mesenteric ischemia: a challenge for the acute care surgeon. Scand J Surg. 2021;110(2):150–8.
Kougias P, Lau D, El Sayed HF, Zhou W, Huynh TT, Lin PH. Determinants ofmortality and treatment outcome following surgical interventions for acutemesenteric ischemia. J Vasc Surg. 2007;46:467–74.
Nuzzo A, Maggiori L, Ronot M, Becq A, Plessier A, Gault N, Joly F, Castier Y, Vilgrain V, Paugam C, Panis Y, Bouhnik Y, Cazals-Hatem D, Corcos O. Predictive factors of intestinal necrosis in acute mesenteric ischemia: prospective study from an intestinal stroke center. Am J Gastroenterol. 2017;112:597–605.
Evennett NJ, Petrov MS, Mittal A, Windsor JA. Systematic review and pooled estimates for the diagnostic accuracy of serological markers for intestinal ischemia. World J Surg. 2009;33:1374–83.
Powell A, Armstrong P. Plasma biomarkers for early diagnosis of acuteintestinal ischemia. Semin Vasc Surg. 2014;27:170–5.
Block T, Nilsson TK, Björck M, Acosta S. Diagnostic accuracy of plasma biomarkers for intestinal ischaemia. Scand J Clin Lab Invest. 2008;68:242–8.
Wilson C, Imrie CW. Amylase and gut infarction. Br J Surg. 1986;73:219–21.
Matsumoto S, Sekine K, Funaoka H, Yamazaki M, Shimizu M, Hayashida K, Kitano M. Diagnostic performance of plasma biomarkers in patients with acute intestinal ischaemia. Br J Surg. 2014;101:232–8.
Treskes N, Persoon AM, van Zanten ARH. Diagnostic accuracy of novel serological biomarkers to detect acute mesenteric ischemia: a systematic review and meta-analysis. Intern Emerg Med. 2017;12:821–36.
Nuzzo A, Guedj K, Curac S, Hercend C, Bendavid C, Gault N, Tran-Dinh A, Ronot M, Nicoletti A, Bouhnik Y, Castier Y, Corcos O, Peoc’h K. SURVI (structure d’URgences Vasculaires Intestinales) research group (French intestinal stroke center) accuracy of citrulline, I-FABP and D-lactate in the diagnosis of acute mesenteric ischemia. Sci Rep. 2021;11(1):18929. https://doi.org/10.1038/s41598-021-98012-w.
Peoc’h K, Nuzzo A, Guedj K, Paugam C, Corcos O. Diagnosis biomarkers in acute intestinal ischemic injury: so close, yet so far. Clin Chem Lab Med. 2018;56:373–85.
Bradbury AW, Brittenden J, McBride K, Ruckley CV. Mesenteric ischaemia: a multidisciplinary approach. Br J Surg. 1995;82:1446–59.
Kassahun WT, Schulz T, Richter O, Hauss J. Unchanged high mortality rates from acute occlusive intestinal ischemia: six year review. Langenbecks Arch Surg. 2008;393:163–71.
Paes E, Vollmar JF, Hutschenreiter S, Schoenberg MH, Schölzel E. Diagnostik und Therapie des akuten Mesenterialinfarktes. Chir Gastroenterol. 1990;6:473–80.
Kirkpatrick ID, Kroeker MA, Greenberg HM. Biphasic CT with mesenteric CTangiography in the evaluation of acute mesenteric ischemia: initial experience. Radiology. 2003;229:91–8.
Furukawa A, Kanasaki S, Kono N, Wakamiya M, Tanaka T, Takahashi M, Murata K. CT diagnosis of acute mesenteric ischemia from various causes. Am J Roentgenol. 2009;192:408–16.
Menke J. Diagnostic accuracy of multidetector CT in acute mesenteric ischemia: systematic review and meta-analysis. Radiology. 2010;256:93–101.
Hagspiel KD, Flors L, Hanley M, Norton PT. Computed tomography angiography and magnetic resonance angiography imaging of the mesenteric vasculature. Tech Vasc Interv Radiol. 2015;18:2–13.
Oliva IB, Davarpanah AH, Rybicki FJ, et al. ACR appropriateness criteria imaging of mesenteric ischemia. Abdom Imaging. 2013;38:714–9.
Emile SH, Khan SM, Barsoum SH. Predictors of bowel necrosis in patients with acute mesenteric ischemia: systematic review and meta-analysis. Updates Surg. 2021;73(1):47–57.
DuBose JJ, Lissauer M, Maung AA, Piper GL, O'Callaghan TA, Luo-Owen X, Inaba K, Okoye O, Shestopalov A, Fielder WD, Ferrada P, Wilson A, Channel J, Moore FO, Paul DB, Johnson S; EAST Pneumatosis Study Group. Pneumatosis intestinalis predictive evaluation study (PIPES): a multicenter epidemiologic study of the Eastern association for the surgery of Trauma. J Trauma Acute Care Surg. 2013;75(1):15–23.
David RA, Erben Y, Kalra M. Clinical presentation, etiology, and diagnostic considerations. In: Oderich G, editor. Mesenteric vascular disease. Springer; 2015. p. 199–209.
Collins JD. MR imaging of the mesenteric vasculature. Radiol Clin North Am. 2020;58(4):797–813.
Daviaud F, Grimaldi D, Dechartres A, Charpentier J, Geri G, Marin N, Chiche JD, Cariou A, Mira JP, Pène F. Timing and causes of death in septic shock. Ann Intensive Care. 2015;5:16.
Guillaume A, Pili-Floury S, Chocron S, Delabrousse E, De Parseval B, Koch S, Samain E, Capellier G, Piton G. Acute mesenteric ischemia among post-cardiac surgery patients presenting with multiple organ failure. Shock. 2016;47:296.
Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N. Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities. World J Gastrointest Pathophysiol. 2016;7:125–30.
De Backer D, Creteur J, Silva E, Vincent JL. Effects of dopamine, norepinephrine, and epinephrine on the splanchnic circulation in septic shock: which is best? Crit Care Med. 2003;31:1659–67.
Krychtiuk KA, Richter B, Lenz M, Hohensinner PJ, Huber K, Hengstenberg C, Wojta J, Heinz G, Speidl WS. Epinephrine treatment but not time to ROSC is associated with intestinal injury in patients with cardiac arrest. Resuscitation. 2020;155:32–8.
Bourcier S, Klug J, Nguyen LS. Non-occlusive mesenteric ischemia: diagnostic challenges and perspectives in the era of artificial intelligence. World J Gastroenterol. 2021;27(26):4088–103.
Reignier J, Boisramé-Helms J, Brisard L, Lascarrou JB, Ait Hssain A, Anguel N, Argaud L et al Clinical Research in Intensive Care and Sepsis (CRICS) group. Enteral versus parenteral early nutrition in ventilated adults with shock: a randomised, controlled, multicentre, open-label, parallel group study (NUTRIREA-2). Lancet 2018; 391: 133–43
Wyers MC. Acute mesenteric ischemia:diagnostic approach and surgical treatment. Semin Vasc Surg. 2010;23:9–20.
Corcos O, Nuzzo A. Gastro-intestinalvascular emergencies. Best Pract Res Clin Gastroenterol. 2013;27:709–25.
Tendler DA, LaMont JT. Acute mesenteric ischemia. Uptodate. 2013. http://www.uptodate.com/contents/acute-mesentericischemia. Accessed 13 Aug 2016.
Sise MJ. Mesenteric ischemia: the whole spectrum. Scand J Surg. 2010;99:106–10.
Oldenburg WA, Lau LL, Rodenberg TJ, Edmonds HJ, Burger CD. Acute mesentericischemia: a clinical review. Arch Intern Med. 2004;164:1054–62.
Helmerhorst HJ, Schultz MJ, van der Voort PH, de Jonge E, van Westerloo DJ. Bench-to-bedside review: the effects of hyperoxia during critical illness. Crit Care. 2015;19:284.
Sartelli M, Coccolini F, Kluger Y, et al. WSES/GAIS/SIS-E/WSIS/AAST global clinical pathways for patients with intra-abdominal infections. World J Emerg Surg. 2021;16:49. https://doi.org/10.1186/s13017-021-00387-8.
Global Alliance for Infections in Surgery Working Group. A global declaration on appropriate use of antimicrobial agents across the surgical pathway. Surg Infect (Larchmt). 2017;18(8):846–53.
Chou EL, Wang LJ, McLellan RM, Feldman ZM, Latz CA, LaMuraglia GM, Clouse WD, Eagleton MJ, Conrad MF. Evolution in the presentation, treatment, and outcomes of patients with acute mesenteric ischemia. Ann Vasc Surg. 2021;74:53–62.
Ballard JL, Stone WM, Hallett JW, Pairolero PC, Cherry KJ. A critical analysis of adjuvant techniques used to assess bowel viability in acute mesenteric ischemia. Am Surg. 1993;59(5):309–11.
Paral J, Ferko A, Plodr M, et al. Laparoscopic diagnostics of acute bowel ischemia using ultraviolet light and fluorescein dye: an experimental study. Surg Laparosc EndoscPercutan Tech. 2007;17(4):291–5.
McGinty JJJ, Hogle N, Fowler DL. Laparoscopic evaluation of intestinal ischemia using fluorescein and ultraviolet light in a porcine model. Surg Endosc. 2003;17(7):1140–3.
Mordon S, Devoisselle JM, Soulie-Begu S, Desmettre T. Indocyanine green: physicochemical factors affecting its fluorescence in vivo. Microvasc Res. 1998;55(2):146–52.
Liot E, Assalino M, Buchs NC, et al. Does near-infrared (NIR) fluorescence angiography modify operative strategy during emergency procedures? Surg Endosc. 2018;32(10):4351–6.
Bryski MG, Frenzel-Sulyok LG, Kaplan L, Singhal S, Keating JJ. Techniques for intraoperative evaluation of bowel viability in mesenteric ischemia: a review. Am J Surg. 2020. https://doi.org/10.1016/j.amjsurg.2020.01.042.
Yanar H, Taviloglu K, Ertekin C, Ozcinar B, Yanar F, Guloglu R, Kurtoglu M. Planned second-look laparoscopy in the management of acute mesenteric ischemia. World J Gastroenterol. 2007;13(24):3350–3.
Cocorullo G, Mirabella A, Falco N, Fontana T, Tutino R, Licari L, Salamone G, Scerrino G, Gulotta G. An investigation of bedside laparoscopy in the ICU for cases of non-occlusive mesenteric ischemia. World J Emerg Surg. 2017;18(12):4. https://doi.org/10.1186/s13017-017-0118-5.
Agresta F, Ansaloni L, Baiocchi GL, Bergamini C, Campanile FC, Carlucci M, Cocorullo G, Corradi A, Franzato B, Lupo M, Mandalà V, Mirabella A, Pernazza G, Piccoli M, Staudacher C, Vettoretto N, Zago M, Lettieri E, Levati A, Pietrini D, Scaglione M, De Masi S, De Placido G, Francucci M, Rasi M, Fingerhut A, Uranüs S, Garattini S. Laparoscopic approach to acute abdomen from the consensus development conference of the Società Italiana di Chirurgia Endoscopica e nuove tecnologie (SICE), Associazione Chirurghi Ospedalieri Italiani (ACOI), Società Italiana di Chirurgia (SIC), Società Italiana di Chirurgia d’Urgenza e del Trauma (SICUT), Società Italiana di Chirurgia nell’Ospedalità Privata (SICOP), and the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2012;26:2134–64.
Bergamini C, Alemanno G, Giordano A, Pantalone D, Fontani G, Di Bella AM, Iacopini V, Prosperi P, Martellucci J. The role of bed-side laparoscopy in the management of acute mesenteric ischemia of recent onset in post-cardiac surgery patients admitted to ICU. Eur J Trauma Emerg Surg. 2020. https://doi.org/10.1007/s00068-020-01500-3.
Orr NT, Endean ED. Part two: against the motion. an endovascular first strategy is not the optimal approach for treating acute mesenteric ischemia. Eur J Vasc Endovasc Surg. 2015;50:276–9. https://doi.org/10.1016/j.ejvs.2015.04.026.
Smith SF, Gollop ND, Klimach SG, Murray PJ. Is open surgery or endovascular therapy best to treat acute mesenteric occlusive disease? Int J Surg. 2013;11:1043–7. https://doi.org/10.1016/j.ijsu.2013.10.003.
Zhang Z, Wang D, Li G, Wang X, Wang Y, Li G, Jiang T. Endovascular treatment for acute thromboembolic occlusion of the superior mesenteric artery and the outcome comparison between endovascular and open surgical treatments: a retrospective study. Biomed Res Int. 2017;2017:1964765. https://doi.org/10.1155/2017/1964765.
Heiss P, Loewenhardt B, Manke C, Hellinger A, Dietl KH, Schlitt HJ, et al. Primary percutaneous aspiration and thrombolysis for the treatment of acute embolic superior mesenteric artery occlusion. Eur Radiol. 2010;20(12):2948–58.
Raupach J, Lojik M, Chovanec V, Renc O, Strycek M, Dvorak P, et al. Endovascular management of acute embolic occlusion of the superior mesenteric artery: a 12-year single-centre experience. Cardiovasc Intervent Radiol. 2016;39(2):195–203.
Bjornsson S, Bjorck M, Block T, Resch T, Acosta S. Thrombolysis for acute occlusion of the superior mesenteric artery. J Vasc Surg. 2011;54(6):1734–42.
Dias NV, Acosta S, Resch T, Sonesson B, Alhadad A, Malina M, et al. Mid-term outcome of endovascular revascularization for chronic mesenteric ischaemia. Br J Surg. 2010;97(2):195–201.
Wyers MC, Powell RJ, Nolan BW, Cronenwett JL. Retrograde mesenteric stenting during laparotomy for acute occlusive mesenteric ischemia. J Vasc Surg. 2007;45(2):269–75.
Blauw JT, Meerwaldt R, Brusse-Keizer M, Kolkman JJ, Gerrits D, Geelkerken RH, et al. Retrograde open mesenteric stenting for acute mesenteric ischemia. J Vasc Surg. 2014;60(3):726–34.
Chen Y, Zhu J, Ma Z, Dai X, Fan H, Feng Z, et al. Hybrid technique to treat superior mesenteric artery occlusion in patients with acute mesenteric ischemia. Exp Ther Med. 2015;9(6):2359–63.
Schermerhorn ML, Giles KA, Hamdan AD, Wyers MC, Pomposelli FB. Mesenteric revascularization: management and outcomes in the United States, 1988–2006. J Vasc Surg. 2009;50(2):341–8.
Block TA, Acosta S, Bjorck M. Endovascular and open surgery for acute occlusion of the superior mesenteric artery. J Vasc Surg. 2010;52(4):959–66.
Ryer EJ, Kalra M, Oderich GS, Duncan AA, Gloviczki P, Cha S, et al. Revascularization for acute mesenteric ischemia. J Vasc Surg. 2012;55(6):1682–9.
Beaulieu RJ, Arnaoutakis KD, Abularrage CJ, Efron DT, Schneider E, Black JH. Comparison of open and endovascular treatment of acute mesenteric ischemia. J Vasc Surg. 2014;59(1):159–64.
Arnaoutakis KD, Abularrage CJ, Efron DT, Schneider E, Black JH 3rd. Comparison of open and endovascular treatment of acute mesenteric ischemia. J Vasc Surg. 2014;59:159–64.
El Farargy M, Abdel Hadi A, Abou Eisha M, Bashaeb K, Antoniou GA. Systematic review and meta-analysis of endovascular treatment for acute mesenteric ischaemia. Vascular. 2017;25:430–8.
Björck M, Koelemay M, Acosta S, Bastos Goncalves F, Kölbel T, Kolkman JJ, Lees T, Lefevre JH, Menyhei G, Oderich G, Esvs Guidelines Committee, Kolh P, De Borst GJ, Chakfe N, Debus S, Hinchliffe R, Kakkos S, Koncar I, Sanddal Lindholt J, Vega De Ceniga M, Vermassen F, Verzini F, Document Reviewers, Geelkerken B, Gloviczki P, Huber T, Naylor R. Editor’s Choice - Management of the Diseases of Mesenteric Arteries and Veins Clinical Practice Guidelines of the European Society of Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. 2017;53(4):460–510.
Hou L, Wang T, Wang J, Zhao J, Yuan D. Outcomes of different acute mesenteric ischemia therapies in the last 20 years: a meta-analysis and systematic review. Vascular. 2021;21:17085381211024504. https://doi.org/10.1177/17085381211024503.
Rebelo A, Partsakhashvili J, John E, Kleeff J, Ukkat J. Current concepts and evidence on open, endovascular and hybrid treatment of mesenteric ischemia: the retrograde open mesenteric stenting. Surg Pract Sci. 2020. https://doi.org/10.1016/j.sipas.2020.100022.
Oderich GS, Macedo R, Stone DH, Woo EY, Panneton JM, Resch T, Dias NV, Sonesson B, Schermerhorn ML, Lee JT, Kalra M, DeMartino RR, Sandri GA, Ramos Tenorio EJ. Low frequency vascular disease research consortium investigators. Multicenter study of retrograde open mesenteric artery stenting through laparotomy for treatment of acute and chronic mesenteric ischemia. J Vasc Surg. 2018;68:470–80.
Björck M. Part one: for the motion an endovascular first strategy is the optimal approach for treating acute mesenteric ischemia. Eur J Vasc Endovasc Surg. 2015;50:273–5.
Stone HH, Fabian TC, Turkleson ML, Jurkiewicz MJ. Management of acute full-thickness losses of the abdominal wall. Ann Surg. 1981;193(5):612–8.
Godat L, Kobayashi L, Costantini T, Coimbra R. Abdominal damage control surgery and reconstruction: world society of emergency surgery position paper. World J Emerg Surg. 2013;8:53.
Weber DG, Bendinelli C, Balogh ZJ. Damage control surgery for abdominal emergencies. Br J Surg. 2014;101:109–18.
Subramanian A, Balentine C, Palacio CH, Sansgiry S, Berger DH, Awad SS. Outcomes of damage-control celiotomy in elderly non trauma patientswith intra-abdominal catastrophes. Am J Surg. 2010;200:783–8.
Urbanavičius L, Pattyn P, de Putte DV, Venskutonis D. How to assess intestinal viability during surgery: a review of techniques. World J Gastrointest Surg. 2011;3:59–69.
Horgan PG, Gorey TF. Operative assessment of intestinal viability. Surg Clin North Am. 1992;72:143–55.
Worrell S, Mumtaz S, Tsuboi K, Lee TH, Mittal SK. Anastomotic complications associated with stapled versus hand-sewn anastomosis. J Surg Res. 2010;161:9–12.
Brundage SI, Jurkovich GJ, Hoyt DB, Patel NY, Ross SE, Marburger R, Stoner M,Ivatury RR, Ku J, Rutherford EJ, Maier RV; WTA Multi-institutional Study Group. Western trauma association. Stapled versus sutured gastrointestinal anastomoses in the trauma patient: a multicenter trial. J Trauma. 2001;51:1054–61.
Smith JW, Matheson PJ, Franklin GA, Harbrecht BG, Richardson JD, Garrison RN. Randomized controlled trial evaluating the efficacy of peritoneal resuscitation in the management of trauma patients undergoing damage control surgery. J Am Coll Surg. 2017;224:396–404.
Crafts TD, Hunsberger EB, Jensen AR, Rescorla FJ, Yoder MC, Markel TA. Direct peritoneal resuscitation improves survival and decreases inflammation after intestinal ischemia and reperfusion injury. J Surg Res. 2015;199:428–34.
Acosta S. Surgical management of peritonitis secondary to acute superior mesenteric artery occlusion. World J Gastroenterol. 2014;20:9936–41.
Hmoud B, Singal AK, Kamath PS. Mesenteric venous thrombosis. J Clin Exp Hepatol. 2014;4:257–63.
Hollingshead M, Burke CT, Mauro MA, et al. Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. J Vasc Interv Radiol. 2005;16:651–61.
Acosta S, Salim S. Management of acute mesenteric venous thrombosis: a systematic review of contemporary studies. Scand J Surg. 2021;110(2):123–9.
Meilahn JE, Morris JB, Ceppa EP, Bulkley GB. Effect of prolonged selective intramesenteric arterial vasodilator therapy on intestinal viability after acute segmental mesenteric vascular occlusion. Ann Surg. 2001;234:107–15.
American Gastroenterological Association Medical Position Statement: Guidelines on intestinal ischemia. Gastroenterology 2000;118:951–953
Rooke TW, Hirsch AT, Misra S, et al. American college of cardiology foundation task force; American heart association task force: management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American college of cardiology foundation/American heart association task force on practice guidelines. J Am Coll Cardiol. 2013;61:1555–70.
Tilsed JV, Casamassima A, Kurihara H, et al. ESTES guidelines: Acute mesenteric ischaemia. Eur J Trauma Emerg Surg. 2016;42:253–70.
Mitsuyoshi A, Obama K, Shinkura N, et al. Survival in nonocclusive mesenteric ischemia: early diagnosis by multidetector row computed tomography and early treatment with continuous intravenous high dose prostaglandin E(1). Ann Surg. 2007;246:229–35.
Klotz S, Vestring T, Rotker J, et al. Diagnosis and treatment of nonocclusive mesenteric ischemia after open heart surgery. Ann Thorac Surg. 2001;72:1583–6.
Boley SJ, Sprayregan S, Siegelman SS, et al. Initial results from an agressive roentgenological and surgical approach to acute mesenteric ischemia. Surgery. 1977;82:848–55.
Takiguchi T, Nakajima M, Ohbe H, Sasabuchi Y, Matsui H, Fushimi K, Kim S, Yokota H, Yasunaga H. Vasodilator therapy and mortality in nonocclusive mesenteric ischemia: a nationwide observational study. Crit Care Med. 2020;48(5):e356–61.
Luther B, Mamopoulos A, Lehmann C, Klar E. The ongoing challenge of acute mesenteric ischemia. Visc Med. 2018;34:217–23.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304–77.
Roussel A, Castier Y, Nuzzo A, et al. Revascularization of acute mesenteric ischemia after creation of a dedicated multidisciplinary center. J Vasc Surg. 2015;62:1251–6.
Reintam Blaser A, Acosta S, Arabi YM. A clinical approach to acute mesenteric ischemia. Curr Opin Crit Care. 2021;27(2):183–92.
Nuzzo A, Corcos O. L’ischémie mésentérique à l’ère des structures d’urgences vasculaires intestinales. Management of mesenteric ischemia in the era of intestinal stroke centers: The gut and lifesaving strategy. J Eur des Urgences et de Réanim. 2017; 38: 592–602.
Yang S, Fan X, Ding W, Liu B, Meng J, Xu D, He C, Yu W, Wu X, Li J. Multidisciplinary stepwise management strategy for acute superior mesenteric venous thrombosis: an intestinal stroke center experience. Thromb Res. 2015;135:36–45.
Corcos O, Castier Y, Sibert A, et al. Effects of a multimodal management strategy for acute mesenteric ischemia on survival and intestinal failure. Clin Gastroenterol Hepatol. 2013;11(158–65): e152.
Cruz RJ Jr, McGurgan J, Butera L, Poloyac K, Roberts M, Stein W, Minervini M, Jorgensen DR, Humar A. Gastrointestinal tract reconstruction in adults with ultra-short bowel syndrome: surgical and nutritional outcomes. Surgery. 2020;168(2):297–304.
Nightingale JM, Lennard-Jones JE, Walker ER, Farthing MJ. Jejunal efflux in short bowel syndrome. Lancet. 1990;336:765–8.
Jeppesen PB. Pharmacologic options for intestinal rehabilitation in patients with short bowel syndrome. JPEN J Parenter Enter Nutr. 2014;38:45S-52S.
Jeppesen PB, Pertkiewicz M, Messing B, et al. Teduglutide reduces need for parenteral support among patients with short bowel syndrome with intestinal failure. Gastroenterology. 2012;143(1473–1481):e1473.
O’Keefe SJ, Jeppesen PB, Gilroy R, et al. Safety and efficacy of teduglutide after 52 weeks of treatment in patients with short bowel intestinal failure. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2013;11:815–23.
Lilley EJ, Cooper Z, Schwarze ML, Mosenthal AC. Palliative care in surgery: defining the research priorities. J Palliat Med. 2017;20:702–9.
Tallarita T, Oderich GS, Gloviczki P, Duncan AA, Kalra M, Cha S, et al. Patient survival after open and endovascular mesenteric revascularization for chronic mesenteric ischemia. J Vasc Surg. 2013;57:747–55.
Zierler RE, Jordan WD, Lal BK, et al. The society for vascular Surgery practice guidelines on follow-up after vascular surgery arterial procedures. J Vasc Surg. 2018;68(1):256–84.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MB and JK wrote the main manuscript text; BDS prepared figures; MB, JK, EEM, FC, BDS, CAG, and DW are responsible for the manuscript conception and draft; all listed authors made important contributions to the conception and design of the work, have drafted the work, or substantively revised it; and all authors reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S3.
Summary of the updated 2022 guidelines for AMI: statements and recommendations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bala, M., Catena, F., Kashuk, J. et al. Acute mesenteric ischemia: updated guidelines of the World Society of Emergency Surgery. World J Emerg Surg 17, 54 (2022). https://doi.org/10.1186/s13017-022-00443-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-022-00443-x