Abstract
Background
Accelerated partial breast irradiation (APBI) is an alternative breast-conserving therapy approach where radiation is delivered in less time compared to whole breast irradiation (WBI), resulting in improved patient convenience, less toxicity, and cost savings. This prospective randomized study compares the external beam APBI with commonly used moderate hypofractionated WBI in terms of feasibility, safety, tolerance, and cosmetic effects.
Methods
Early breast cancer patients after partial mastectomy were equally randomized into two arms– external APBI and moderate hypofractionated WBI. External beam technique using available technical innovations commonly used in targeted hypofractionated radiotherapy to minimize irradiated volumes was used (cone beam computed tomography navigation to clips in the tumor bed, deep inspiration breath hold technique, volumetric modulated arc therapy dose application, using flattening filter free beams and the six degrees of freedom robotic treatment couch). Cosmetics results and toxicity were evaluated using questionnaires, CTCAE criteria, and photo documentation.
Results
The analysis of 84 patients with a median age of 64 years showed significantly fewer acute adverse events in the APBI arm regarding skin reactions, local and general symptoms during a median follow-up of 37 months (range 21–45 months). A significant difference in favor of the APBI arm in grade ≥ 2 late skin toxicity was observed (p = 0.026). Late toxicity in the breast area (deformation, edema, fibrosis, and pain), affecting the quality of life and cosmetic effect, occurred in 61% and 17% of patients in WBI and APBI arms, respectively. The cosmetic effect was more favorable in the APBI arm, especially 6 to 12 months after the radiotherapy.
Conclusion
External APBI demonstrated better feasibility and less toxicity than the standard regimen in the adjuvant setting for treating early breast cancer patients. The presented study confirmed the level of evidence for establishing the external APBI in daily clinical practice.
Trial registration
NCT06007118.
Similar content being viewed by others
Background
The preferred treatment option for most patients with early breast cancer (BC) is breast-conserving therapy (BCT) [1], consisting of partial mastectomy and subsequent breast irradiation. Conventionally fractionated whole-breast irradiation (WBI) with or without an additional tumor bed dose, time burdening patients, usually taking 5–7 weeks, was standard for decades. Large phase III trials have proved that overall irradiation time could be reduced using hypofractionated WBI without compromising local control and warranting a good safety profile [2, 3].
Partial-breast irradiation (PBI) has been introduced as an alternative approach for adjuvant radiotherapy (RT) after partial mastectomy in selected low-risk early BC patients. Compared with WBI, estimated advantages of PBI include shorter overall treatment time when RT is accelerated (APBI, accelerated partial breast irradiation), improved safety profile, and potential cost reduction [4]. Several large phase III trials demonstrated the noninferiority of PBI versus WBI in terms of local recurrence (LR) and similar or reduced toxicity at five years [5,6,7,8,9]. Recommendations for APBI have been published by both the American Society for Radiation Oncology and the Groupe Européen de Curiethérapie-European Society for Radiotherapy Oncology [10,11,12].
There are several technical possibilities for APBI, such as interstitial or intracavitary brachytherapy (BRT) or external beam irradiation. Three-dimensional conformal radiotherapy (3D-CRT) has been associated with a higher risk of skin reactions and worse cosmetic results [13,14,15], particularly because of the need to accommodate extra safety margins to compensate for inaccuracies during irradiation. APBI, based on the principles of hypofractionation, has the advantages of being less invasive and faster due to focusing on the target, using a higher radiation dose per fraction, and reducing the dose to the surrounding normal tissues. Moreover, it improves the accuracy of treatment through the different currently available machine devices, such as image-guided radiotherapy (IGRT) aimed at clips in the tumor bed using CT devices on the platform of linear accelerator (cone beam computed tomography, CBCT); [16] irradiation in deep inspiration breath hold (DIBH technique) [17, 18] to stop breast movements during breathing; fast and accurate dose application using arc therapy (volumetric modulated arc therapy, VMAT) [19]; radiation beams without a homogenizing filter with a high dose rate (flattening filter free beams, FFF) [20] or correction of the patient’s position with six degrees of freedom robotic treatment couch (6DoF couch) [21].
The aim of this prospective randomized single-institution study conducted by the Department of Radiation Oncology at Masaryk Memorial Cancer Institute (MMCI) in Brno, Czechia, was to compare APBI (5 fractions) of the early BC patients with the currently more commonly used moderate hypofractionated WBI regimen (20 fractions) [22]. The main objective was to evaluate the feasibility, safety, tolerance, and cosmetic effects of APBI and, thus, to increase the evidence for establishing this technique in indicated patients into daily clinical practice.
Methods
Patients and study design
Patients with early-stage BC referred for adjuvant RT were randomly assigned to the following two treatment arms: APBI arm (irradiation of tumor bed, 30 Gy in 5 fractions, referred as study arm) or WBI arm (moderate hypofractionated irradiation of the whole breast with a boost to the tumor bed, 40 Gy in 15 fractions followed by 10 Gy in 5 fractions). Written informed consent was received from each patient prior to enrolment. The study was approved by the Ethical Board of Masaryk Memorial Cancer Institute (MMCI; approval No. 2017/1889/MOU) and registered at ClinicalTrials.gov (NCT06007118).
The inclusion criteria were: age ≥ 50 years; Karnofsky index > 70; breast-conserving surgery; DCIS G1/2 ≤ 25 mm with negative margins (≥ 3 mm) or invasive (non-lobular) luminal-like HER2 negative carcinoma ≤ 20 mm with negative margins (≥ 2 mm) without LVI; performing of axillary dissection (≥ 6 negative lymph nodes) or negative sentinel node biopsy. The exclusion criteria were: prior chest or breast surgery; absence of surgical clips in tumor bed; multifocal or multicentric involvement; factors contraindicating RT; known BRCA1/2 or other mutation in high penetrating genes; neoadjuvant therapy; prior RT; adjuvant chemotherapy.
Randomization
A stratified permuted block randomization scheme with a block size of four was used to assign patients to arms in a 1:1 ratio. The treatment group assignment was not blinded. Stratification factors were (1) surgery bed size measured by the longest distance of surgery clips placed for radiotherapy navigation (< 30 mm or ≥ 30 mm), and (2) phototype (light (phototype I/II) or dark (phototype III/IV)).
Treatment
Safety and accuracy of treatment were achieved by ensuring reliable and reproducible immobilization (frameless fixation with Orfit Industries and CIVCO Medical Solutions vacuum-formable mattresses) and using all technical machine devices described above (cone beam computed tomography navigation to clips in the tumor bed, deep inspiration breath hold technique, volumetric modulated arc therapy dose application, using flattening filter free beams and the six degrees of freedom robotic treatment couch). CT scans with 2 mm thick slices, including the curve of respiratory movements, were sent to the radiotherapy planning system. For WBI, the clinical target volume (CTV) was defined by the residual parenchyma of the gland. The planning target volume (PTV) was created by expanding CTV by 10 mm in all directions. For both arms, tumor bed CTV encompasses the excision cavity with a 10 mm margin. Visible cavity and clips placed to the cavity borders during surgery were used to define the CTV. The CTV did not include the chest wall and pectoralis muscles and was limited to 5 mm from the skin surface. In the APBI arm, PTV was delineated with a 3-mm extent in all directions from CTV to accommodate possible set-up errors. The PTV was also limited to 5 mm from the skin surface. The prescribed radiation dose was planned for this final PTV.
The WBI arm patients were irradiated with a moderate hypofractionated mode within 20 working days [3]. The whole breast was irradiated with 40.05 Gy in 15 fractions, followed by a boost to the tumor bed with 10 Gy in 5 fractions. The APBI arm patients received a total dose of 30 Gy administered in 5 fractions over five consecutive days, allowing for a potential break over the weekend, provided that there were at least two consecutive fractions before or after the weekend break. The dose distribution and beam arrangement of APBI are presented in Supplementary Fig. 1. Treatment plans were created using Eclipse planning system version 15.6 (Varian Medical Systems, Palo Alto CA) using the AAA algorithm. VMAT technique (2–3 partial arcs) and a high dose rate 6 MV beam without a homogenization filter (FFF) were used [19, 20, 23]. Adequate target coverage was achieved when the prescribed dose covered 95% of the PTV. A dose gradient was also assessed, and the treatment plans should meet the number of organs at risk dose-volume constraints [24,25,26,27] based on published studies (Supplementary Table 1). The treatment was delivered by the linear accelerator Varian TrueBeam STX v. 2.5.(Varian Medical Systems, Palo Alto CA).
Follow-up and outcomes
Evaluation and study assessments were scheduled prior to RT (B, baseline), at the end of RT (M0), and in 1 (M1), 3 (M3), 6 (M6), 9 (M9), 12 (M12) months after RT, in the second year every four months and then every six months.
The primary endpoint of the study was toxicity evaluated by CTCAE (Common Terminology Criteria for Adverse Events). Acute toxicity was defined as adverse reactions occurring within three months after RT, and late toxicity occurs during the next follow-up. The grades presented are the patient’s worst toxicity at any time point. Secondary endpoints were quality of life (Qol) measured with the official Czech translation of EORTC QoL questionnaires [28,29,30] (EORTC QLQ-C30), including a special module for patients with BC (Breast QLQ-BR45); cosmetic effect independently evaluated by patient, physician, and nurse scored using Harvard scale (4-point Likert scale) [31]; change in breast appearance (photographic) assessed on a 3-point graded scale (none, mild, marked); and economy burden of patients evaluated at the end of RT by a 4-point graded scale (none, mild, middle, significant). For future evaluation of subsequent endpoints (recurrence-free survival, disease-specific survival, ipsilateral breast-recurrence rate, distant disease-free interval, and overall survival), patients will be followed up according to standards of care. Six months after RT, pulmonary toxicity was assessed based on clinical examination and computed tomography (CT) scan in the treatment position.
Sample size and statistical analysis
The study was designed to assess the noninferiority of APBI to relative WBI in terms of the grade ≥ 2 late skin toxicity involving events between 6 months and two years after RT. Assuming an incidence of late skin toxicity in the WBI arm of 15% and an expected incidence in APBI of 5%, and based on two proportion z-test with a noninferiority margin of 10%, one-sided significance level of 5%, test power of 90%, and 10% dropout rate, 84 patients (42 in each arm) were required.
Patient and treatment characteristics were described using the standard summary statistics, i.e., median and interquartile range (IQR) for continuous variables and numbers and percentages for categorical variables. Depending on the nature of the data, Fisher’s exact or chi-square test for categorical variables and nonparametric Mann-Whitney test for continuous variables were used to compare arms. A significance level of 5% was considered for all statistical tests, and R statistical software version 4.3.1 [32] was used.
Results
From September 2019 to June 2021, 87 patients were enrolled and randomized. Of these, three were excluded from the final evaluation due to insufficient follow-up (Fig. 1). In the analyzed cohort, 42 patients were assigned to the APBI arm and 42 to the WBI arm. Median follow-up was 37 months (range 21–45 months). No recurrence, regional or distant relapse of the disease was detected in all patients during follow-up.
Baseline patients’ characteristics are summarized in Table 1. No significant difference was observed between arms. The majority of enrolled patients had NST tumors (79%), up to 10 mm (50%), of nuclear grade G1 (59%), with low Ki67 status (55%). The median negative resection margin was 5 and 5.5 mm in the APBI and WBI groups, respectively. 74% of patients had concurrent endocrine therapy.
Baseline dose-volume characteristics are summarized in Table 2. The CTV volume median in the study arm was 58.5 cc (range 25.7–141.0), and the PTV volume median was 86.5 cc (range 40.9–189.9). In the control group, the median size of the CTV boost was 14.5 cc (range 4.2–59.4), and PTV boost was 69.0 cc (range 33.9–167.7).
The radiation toxicities at acute and late periods are presented in Table 3. Significantly fewer acute adverse events were observed in the APBI arm regarding skin reactions and local and general symptoms (p < 0.001 for all). Skin side effects of grade ≥ 2 were significantly less often in the APBI arm in terms of erythema (p < 0.001), hyperpigmentation (p = 0.002), and desquamation (p = 0.012).
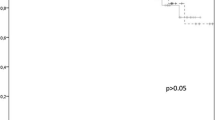
In the WBI arm, important late toxicity was worse and fading over time. A significant difference in favor of the study arm in skin dryness, edema, hyperpigmentation (p < 0.001 for all), and tenderness (p = 0.002) was observed. Grade ≥ 2 late skin toxicity developed in 5 (12%) patients in the WBI arm and none in the APBI arm (2-sided equality test: p = 0.026, noninferiority test with margin of 10%: p < 0.001). Late toxicity in the breast area (deformation, edema, fibrosis, and pain), affecting Qol and the cosmetic effect of the treatment, occurred in 61% of patients for any grade and 7.3% for grade ≥ 2 in the WBI arm and 17% for any grade in the APBI group (p < 0.001). Selected toxicities over time are shown in Fig. 2. More pronounced toxicity in the WBI arm is presented in all toxicity domains. Notably, grade ≥ 2 toxicities are minimal in the study arm. Fibrosis and breast deformation adverse events were common immediately after surgery and gradually disappeared over time, faster in the APBI arm, whereas in the WBI arm, reappeared after RT.
Based on CT scans six months after RT, radiographic signs of pneumonitis/fibrosis were less common in the APBI than in the WBI arm (1 patient, 2.4% vs. 26 patients, 63%, p < 0.001). One patient in WBI simultaneously had clinical symptoms of pneumonitis.
Cosmetic effects evaluated at different periods are summarized in Table 4. The cosmetic effect was more favorable in the APBI group, especially 6 to 12 months after the RT. A significant difference in the occurrence of cosmetic changes appeared between arms throughout the first year after irradiation. Major cosmetic changes (clear and severe differences) were noted mainly from the patient’s point of view (p = 0.003 at M0-M3 and p = 0.055 at M6-M12).
Discussion
This prospective randomized study of early BC patients is, together with the slightly earlier initiated HYPAB trial [33], the first to evaluate the efficacy and side effects of five-fractions ABPI (30 Gy in 5 fractions) compared to moderate hypofractionated, currently most used, WBI regimen (40 Gy in 15 fractions). The conclusions of our study and the HYBAB trial are consistent and help to increase the evidence for using this fractionation and technique in routine APBI practice. In contrast to the other trials using the same fractionation [6, 24], a dose of 30 Gy was administered in 5 consecutive daily fractions, VMAT technique and FFF beams were used for dose application.
Thanks to more precise irradiation using all available modern technologies and procedures used in targeted hypofractionated and stereotactic RT (surgical clips, CBCT, DIBH, VMAT, FFF, 6DoF couch), it was possible to reduce the volume of the PTV and thereby avoid the increased toxicity described in the oldest external APBI studies [13,14,15]. Therefore, the 3-mm PTV margin is supposed to be large enough to accommodate possible set-up errors in this setting. This is in line with the trend of modern radiotherapy, where safety margins can be reduced thanks to new technologies, thereby reducing side effects and improving the quality of life of oncology patients. Based on our findings, APBI is highly tolerable in regards to both toxicity and cosmetic effects, ultimately providing definite benefits to patients. As a result, the technique of external APBI may be used more often in clinical practice in the future. We are aware that confirmation of the oncological effectiveness of this technique and the appropriateness of using a 3-mm PTV margin requires a longer follow-up. However, the indication is that at the time of analysis, no local, regional, or distant recurrence of the disease was detected in both arms of patients.
Other randomized trials dealing with external APBI compared this technique with standard fractionated WBI (50 Gy in 25 fractions) [24, 34]. Comparing different fractionation schedules is also crucial. Studies involving twice-daily irradiation of patients reported increased toxicity and more adverse cosmetic effects [7, 8, 15]. Furthermore, our study demonstrated that consecutive irradiation yields favorable cosmetic outcomes with minimal toxicity, so irradiating every other day may not be necessary [35,36,37].
Adjuvant RT after primary surgery aims to eliminate the potential microscopic residual disease in the surgery bed and/or surrounding satellites [38, 39]. Recurrences occur most often at the site of the primary lesion [40, 41]. The randomized trials [6, 11, 24, 35, 42,43,44,45,46,47] have shown noninferiority in LC and OS after the tumor bed irradiation as opposed to WBI in patients with early BC after BCT [10,11,12, 48]. Based on these results, ASTRO and ESTRO recommend APBI as an alternative to WBI for selected patients with early BC [10,11,12, 49].
Published reputable studies [6, 46, 47] using external beam RT show better toxicity profiles and cosmetic effects in APBI arms. Livi et al. [24, 35, 42] compared the same APBI fractionation scheme (30 Gy in 5 fractions, every other day) with standard WBI (50 Gy in 25 fractions + boost). There was a significant difference in both any grade and grade ≥ 2 acute toxicity in favor of the APBI arm. The most frequently observed event was skin erythema (19.9% and 66.5% in APBI and WBI arms, respectively). Concerning late side effects, no grade ≥ 2 toxicity was observed in the APBI group. The most represented event was skin fibrosis in both arms (4.5% and 11.2% in APBI and WBI arms, respectively). The trial showed not only a significantly better toxicity profile but also the functional status and Qol after treatment and after 2 years were better in the APBI group, which is consistent with our study findings. We observed disappeared differences in cosmetic effects between WBI and APBI with longer follow-up. This may be due to the subjectivity of the assessment or the fact that patients have grown accustomed to the condition of their breast.
Some studies used 10 fractions in 5 days, i.e., twice daily irradiation [7, 8, 15], for external APBI. Data on patient preferences are limited, but both patients and physicians consider twice-daily radiation to be complicated and not optimal [50, 51]. The Canadian phase III RAPID study demonstrated the noninferiority of APBI in LC and acute toxicity. However, late toxicity and cosmetic results favored WBI. The authors concluded that the six-hour interval between fractions is too short for reparation. The APBI dose regimen used in our study (30 Gy in 5 fractions) is satisfactory for adjuvant irradiation. Qi et al. [52] described the α/β ratio (basic radiobiological parameter) of breast tumors to be relatively low (α/β = 2.88), and therefore high-dose RT can be very beneficial in the same way. Using a linear quadratic model and assuming an α/β ratio of 3 or 2.5, the prescribed dose used in our APBI study is equivalent to 54 or 56.7 Gy when using standard fractionation.
Since ASTRO and ESTRO recommendations were strictly followed [10,11,12, 48], only low-risk patients were included in APBI studies. Treatment results may be impaired if patients with a higher risk of recurrence (larger tumors, smaller surgical margins, hormone non-dependency, or lymph node involvement) are included. In the NSABP B-39/RTOG 0413 [8] study, enrolling patients with the nodal disease (pN1mic or pN1), criteria for noninferiority of the APBI were not reached in the number of ipsilateral recurrences (although the absolute difference was 0.7%).
The crucial factor affecting toxicity is the size of the target volume. Clinical trials using the 3D-CRT technique were associated with higher skin reactions and worse cosmetic results, particularly because of the need to accommodate extra safety margins to compensate for all inaccuracies during irradiation, including breast movements during breathing. The median PTV volumes in the published 3D-CRT studies were 269 cc, 296 cc, and 185 cc, respectively [53]. Livi et al. [24], as also mentioned above, used intensity modulated radiation therapy (IMRT) and showed no significant difference between PBI and WBI in ipsilateral breast tumor recurrence and survival rates at ten years, with significantly improved outcomes in treatment-related toxic effects and cosmetic results in favor of the APBI arm. The mean PTV volume in their trial was 139 cc (range 55–259). In our APBI trial, the VMAT technique was used for its accuracy and fast rate of dose application [19]. The median PTV volume in the APBI arm was 86.5 cc (range 40.9–189.9). The data presented from all the mentioned studies indicates that PTV volumes up to 150–180 cc are safe for applying the dose of 30 Gy in 5 fractions. Moreover, two studies used the same dose fractionation for WBI and PBI and showed that reducing the irradiated volume alone reduced late toxicity [6, 54].
A growing interest in ultra-hypofractionated regimens emerged during the COVID-19 pandemic [55]. A one-week hypofractionated WBI regimen has become standard in the UK. For local disease control, the WBI schedule of 26 Gy in 5 fractions over one week is non-inferior to 40 Gy in 15 fractions over three weeks [55,56,57]. Although it seems safe in terms of normal tissue effects for up to 5 years, this regimen has not been tested within a PBI phase 3 trial. In this context, the schedule of 30 Gy in 5 fractions represents an appealing treatment option that is both safe and effective [24, 34, 35, 37].
We are aware of the study’s limitations. The first is the relatively small number of patients, although sufficient for the statistical power of the considered objective. During the interim follow-up, there was no recurrence, regional or distant dissemination, or death of patients, but a longer follow-up for secondary objectives analysis is necessary. Second, the boost dose applied in our study is not necessary in light of current knowledge and recommendations and means certain overtreatment [58, 59]. When the study began, such a procedure was part of the treatment protocols at our institution. Also, most of the above-described studies used boost irradiation in the control arms. Recently, a boost may not be indicated in older patients with sufficient resection margins. This may have worsened the observed toxicity parameters in some patients and thus highlighted the differences between the arms. Our study was designed to confirm the non-inferiority of APBI compared to WBI. However, we observed that APBI patients experienced even significantly less toxicity.
Finally, several patients with a low-risk BC treated in the APBI trials may have been suitable candidates for the complete omission of adjuvant RT. Published meta-analyses established that forgoing WBI does not impact overall survival in selected patients but is associated with a significantly higher rate of LR [60,61,62]. This procedure is chosen mainly for patients with worse clinical conditions or comorbidities when a significant benefit from reducing the risk of ipsilateral disease recurrence using RT is not expected. On the other hand, the second pillar of early BC patient care is ET, which may negatively influence Qol of patients [63] due to its detrimental action on the cardiovascular system, bone density, sexuality, and cognition. Therefore, the oncological community is investigating [64] whether APBI could safely replace ET in very low-risk early BC (i.e., older age, luminal-A disease). In such a case, the double advantage of partial breast irradiation– a significant shortening of the total radiation time and less toxicity compared with WBI and the abolition of long-term toxicity of ET if omitted - would favorably affect QoL.
Conclusion
The technique of external APBI using the principles of targeted hypofractional RT was found to be very well tolerated, easy to perform, and safe. External beam APBI schedule of 30 Gy in 5 fractions represents an attractive treatment option that is both safe and effective. Our study indicated that this technique may be a more feasible and less toxic option in the adjuvant setting for treating early BC patients compared to hypofractionated WBI, thus contributing to increasing its evidence for use in clinical practice. In the long term, short-course, once-daily external beam schedule will emerge as the favored approach to balance efficacy, convenience, and toxicity for those patients who proceed with adjuvant partial breast radiation.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- APBI:
-
Accelerated partial breast irradiation
- WBI:
-
Whole breast irradiation
- BC:
-
Breast cancer
- BCT:
-
Breast-conserving therapy
- PBI:
-
Partial-breast irradiation
- RT:
-
Radiotherapy
- LR:
-
Local recurrence
- BRT:
-
Brachytherapy
- 3D-CRT:
-
Three-dimensional conformal radiotherapy
- IGRT:
-
Image-guided radiotherapy
- CBCT:
-
Cone beam computed tomography
- DIBH:
-
Deep inspiration breath hold
- VMAT:
-
Volumetric modulated arc therapy
- FFF:
-
Flattening filter free beams
- MMCI:
-
Masaryk Memorial Cancer Institute
- CTV:
-
Clinical target volume
- PTV:
-
Planning target volume
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- Qol:
-
Quality of life
- CT:
-
Computed tomography
- IQR:
-
Interquartile range
- DCIS:
-
Ductal Carcinoma In Situ
- NST:
-
Non-specified tumor histology
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- IA:
-
Aromatase inhibitor
References
Darby S, McGale P, Correa C, Taylor C, Arriagada R, Clarke M, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378:1707–16.
Haviland JS, Owen JR, Dewar JA, Agrawal RK, Barrett J, Barrett-Lee PJ, et al. The UK standardisation of breast radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trials. Lancet Oncol. 2013;14:1086–94.
Whelan TJ, Pignol J-P, Levine MN, Julian JA, MacKenzie R, Parpia S, et al. Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med. 2010;362:513–20.
Greenup RA, Camp MS, Taghian AG, Buckley J, Coopey SB, Gadd M, et al. Cost comparison of radiation treatment options after lumpectomy for breast cancer. Ann Surg Oncol. 2012;19:3275–81.
Strnad V, Polgár C, Ott OJ, Hildebrandt G, Kauer-Dorner D, Knauerhase H, et al. Accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy compared with whole-breast irradiation with boost for early breast cancer: 10-year results of a GEC-ESTRO randomised, phase 3, non-inferiority trial. Lancet Oncol. 2023;24:262–72.
Coles CE, Griffin CL, Kirby AM, Titley J, Agrawal RK, Alhasso A, et al. Partial-breast radiotherapy after breast conservation surgery for patients with early breast cancer (UK IMPORT LOW trial): 5-year results from a multicentre, randomised, controlled, phase 3, non-inferiority trial. Lancet. 2017;390:1048–60.
Whelan TJ, Julian JA, Berrang TS, Kim DH, Germain I, Nichol AM, et al. External beam accelerated partial breast irradiation versus whole breast irradiation after breast conserving surgery in women with ductal carcinoma in situ and node-negative breast cancer (RAPID): a randomised controlled trial. Lancet. 2019;394:2165–72.
Vicini FA, Cecchini RS, White JR, Arthur DW, Julian TB, Rabinovitch RA, et al. Long-term primary results of accelerated partial breast irradiation after breast-conserving surgery for early-stage breast cancer: a randomised, phase 3, equivalence trial. Lancet. 2019;394:2155–64.
Haussmann J, Budach W, Corradini S, Krug D, Jazmati D, Tamaskovics B et al. Comparison of adverse events in partial- or whole breast radiotherapy: investigation of cosmesis, toxicities and quality of life in a meta-analysis of randomized trials. Radiat Oncol. 2023;18.
Correa C, Harris EE, Leonardi MC, Smith BD, Taghian AG, Thompson AM, et al. Accelerated partial breast irradiation: executive summary for the update of an ASTRO evidence-based Consensus Statement. Pract Radiat Oncol. 2017;7:73–9.
Strnad V, Major T, Polgar C, Lotter M, Guinot JL, Gutierrez-Miguelez C, et al. ESTRO-ACROP guideline: interstitial multi-catheter breast brachytherapy as accelerated partial breast irradiation alone or as boost - GEC-ESTRO breast Cancer Working Group practical recommendations. Radiother Oncol. 2018;128:411–20.
Strnad V, Krug D, Sedlmayer F, Piroth MD, Budach W, Baumann R, et al. DEGRO practical guideline for partial-breast irradiation. Strahlenther Onkol. 2020;196:749–63.
Hepel JT, Tokita M, MacAusland SG, Evans SB, Hiatt JR, Price LL, et al. Toxicity of three-dimensional conformal radiotherapy for accelerated partial breast irradiation. Int J Radiat Oncol Biol Phys. 2009;75:1290–6.
Jagsi R, Ben-David MA, Moran JM, Marsh RB, Griffith KA, Hayman JA, et al. Unacceptable cosmesis in a protocol investigating intensity-modulated radiotherapy with active breathing control for accelerated partial-breast irradiation. Int J Radiat Oncol Biol Phys. 2010;76:71–8.
Olivotto IA, Whelan TJ, Parpia S, Kim DH, Berrang T, Truong PT, et al. Interim cosmetic and toxicity results from RAPID: a randomized trial of accelerated partial breast irradiation using three-dimensional conformal external beam radiation therapy. J Clin Oncol. 2013;31:4038–45.
Purdie TG, Bissonnette JP, Franks K, Bezjak A, Payne D, Sie F, et al. Cone-beam computed tomography for on-line image guidance of lung stereotactic radiotherapy: localization, verification, and intrafraction tumor position. Int J Radiat Oncol Biol Phys. 2007;68:243–52.
Bergom C, Currey A, Desai N, Tai A, Strauss JB. Deep Inspiration Breath Hold: Techniques and Advantages for Cardiac Sparing During Breast Cancer Irradiation. Front Oncol. 2018;8 APR.
Latty D, Stuart KE, Wang W, Ahern V. Review of deep inspiration breath-hold techniques for the treatment of breast cancer. J Med Radiat Sci. 2015;62:74–81.
Otto K. Volumetric modulated arc therapy: IMRT in a single gantry arc. Med Phys. 2008;35:310–7.
Yan Y, Yadav P, Bassetti M, Du K, Saenz D, Harari P, et al. Dosimetric differences in flattened and flattening filter-free beam treatment plans. J Med Phys. 2016;41:92–9.
Schmidhalter D, Fix MK, Wyss M, Schaer N, Munro P, Scheib S et al. Evaluation of a new six degrees of freedom couch for radiation therapy. Med Phys. 2013;40.
Haviland JS, Hopwood P, Mills J, Sydenham M, Bliss JM, Yarnold JR. Do patient-reported outcome measures agree with clinical and photographic assessments of normal tissue effects after breast Radiotherapy? The experience of the standardisation of breast radiotherapy (START) trials in early breast Cancer. Clin Oncol (R Coll Radiol). 2016;28:345–53.
Ong CL, Verbakel WFAR, Cuijpers JP, Slotman BJ, Lagerwaard FJ, Senan S. Stereotactic radiotherapy for peripheral lung tumors: a comparison of volumetric modulated arc therapy with 3 other delivery techniques. Radiother Oncol. 2010;97:437–42.
Livi L, Meattini I, Marrazzo L, Simontacchi G, Pallotta S, Saieva C, et al. Accelerated partial breast irradiation using intensity-modulated radiotherapy versus whole breast irradiation: 5-year survival analysis of a phase 3 randomised controlled trial. Eur J Cancer. 2015;51:451–63.
Piroth MD, Baumann R, Budach W, Dunst J, Feyer P, Fietkau R et al. Heart toxicity from breast cancer radiotherapy: current findings, assessment, and prevention. Strahlenther Onkol. 2019;195.
Lee BM, Chang AS, Kim SY et al. Risk of radiation pneumonitis following individualized modern radiotherapy with IMRT, a breath-holding technique, and prone positioning for breast cancer. Abstract selected for 2018 Best of ASTRO (November 30-December 1, 2018) from ASTRO’s 60th Annual Meeting (October 21–24, 2018).
Obayomi-Davies O, Kole TP, Oppong B, Rudra S, Makariou EV, Campbell LD et al. Stereotactic Accelerated Partial Breast Irradiation for Early-Stage Breast Cancer: Rationale, Feasibility, and Early Experience Using the CyberKnife Radiosurgery Delivery Platform. Front Oncol. 2016;6 MAY:23.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Sprangers MA, Groenvold M, Arraras JI, Franklin J, te Velde A, Muller M, et al. The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. J Clin Oncol. 1996;14:2756–68.
Bjelic-Radisic V, Cardoso F, Cameron D, Brain E, Kuljanic K, da Costa RA, et al. An international update of the EORTC questionnaire for assessing quality of life in breast cancer patients: EORTC QLQ-BR45. Ann Oncol. 2020;31:283–8.
Haloua MH, Marianna N, Krekel A, Johannes G, Jacobs A, Zonderhuis B et al. Cosmetic Outcome Assessment following breast-conserving therapy: a comparison between BCCT.core Software and Panel evaluation. Int J Breast Cancer. 2014;2014.
R Core Team. _R: A Language and Environment for Statistical Computing_. R Foundation for Statistical Computing, Vienna, Austria. 2023. https://www.r-project.org/. Accessed 15 Feb 2023.
Franceschini D, Loi M, Chiola I, Arculeo S, Marzo M, Fernandes B et al. Preliminary results of a Randomized Study on Postmenopausal Women with early stage breast Cancer: adjuvant hypofractionated whole breast irradiation Versus Accelerated partial breast irradiation (HYPAB Trial). Clin Breast Cancer. 2021;21.
Meattini I, Saieva C, Miccinesi G, Desideri I, Francolini G, Scotti V, et al. Accelerated partial breast irradiation using intensity modulated radiotherapy versus whole breast irradiation: Health-related quality of life final analysis from the Florence phase 3 trial. Eur J Cancer. 2017;76:17–26.
Meattini I, Marrazzo L, Saieva C, Desideri I, Scotti V, Simontacchi G, et al. Accelerated partial-breast irradiation compared with whole-breast irradiation for early breast Cancer: long-term results of the Randomized Phase III APBI-IMRT-Florence Trial. J Clin Oncol. 2020;38:4175–83.
Colciago RR, La Rocca E, Giandini C, Rejas Mateo A, Bedini N, Capri G, et al. One-week external beam partial breast irradiation: survival and toxicity outcomes. J Cancer Res Clin Oncol. 2023;149:10965–74.
Marrazzo L, Meattini I, Simontacchi G, Livi L, Pallotta S. Updates on the APBI-IMRT-Florence Trial (NCT02104895) technique: from the Intensity Modulated Radiation Therapy Trial to the Volumetric Modulated Arc Therapy Clinical Practice. 2023. https://doi.org/10.1016/j.prro.2022.05.010.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), Darby S, McGale P, Correa C, Taylor C, Arriagada R, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10 801 women in 17 randomised trials. Lancet. 2011;378:1707–16.
Bartelink H, Horiot J-C, Poortmans P, Struikmans H, Van den Bogaert W, Barillot I, et al. Recurrence rates after treatment of breast cancer with standard radiotherapy with or without additional radiation. N Engl J Med. 2001;345:1378–87.
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–41.
Veronesi U, Marubini E, Mariani L, Galimberti V, Luini A, Veronesi P, et al. Radiotherapy after breast-conserving surgery in small breast carcinoma: long-term results of a randomized trial. Ann Oncol. 2001;12:997–1003.
Meattini I, Saieva C, Marrazzo L, Di Brina L, Pallotta S, Mangoni M, et al. Accelerated partial breast irradiation using intensity-modulated radiotherapy technique compared to whole breast irradiation for patients aged 70 years or older: subgroup analysis from a randomized phase 3 trial. Breast Cancer Res Treat. 2015;153:539–47.
Schäfer R, Strnad V, Polgár C, Uter W, Hildebrandt G, Ott OJ, et al. Quality-of-life results for accelerated partial breast irradiation with interstitial brachytherapy versus whole-breast irradiation in early breast cancer after breast-conserving surgery (GEC-ESTRO): 5-year results of a randomised, phase 3 trial. Lancet Oncol. 2018;19:834–44.
Polgár C, Ott OJ, Hildebrandt G, Kauer-Dorner D, Knauerhase H, Major T, et al. Late side-effects and cosmetic results of accelerated partial breast irradiation with interstitial brachytherapy versus whole-breast irradiation after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: 5-year results of a randomised, controlled, phase 3 trial. Lancet Oncol. 2017;18:259–68.
Ott OJ, Strnad V, Hildebrandt G, Kauer-Dorner D, Knauerhase H, Major T, et al. GEC-ESTRO multicenter phase 3-trial: accelerated partial breast irradiation with interstitial multicatheter brachytherapy versus external beam whole breast irradiation: early toxicity and patient compliance. Radiother Oncol. 2016;120:119–23.
Rodríguez N, Sanz X, Dengra J, Foro P, Membrive I, Reig A, et al. Five-year outcomes, cosmesis, and toxicity with 3-dimensional conformal external beam radiation therapy to deliver accelerated partial breast irradiation. Int J Radiat Oncol Biol Phys. 2013;87:1051–7.
Meduri B, Baldissera A, Galeandro M, Donini E, Tolento G, Giacobazzi P, et al. OC-0568: Accelerated PBI VS standard radiotherapy (IRMA trial): interim cosmetic and toxicity results. Radiother Oncol. 2017;123:303.
Meattini I, Becherini C, Boersma L, Kaidar-Person O, Marta GN, Montero A, et al. European Society for Radiotherapy and Oncology Advisory Committee in Radiation Oncology Practice consensus recommendations on patient selection and dose and fractionation for external beam radiotherapy in early breast cancer. Lancet Oncol. 2022;23:e21–31.
Shaitelman SF, Anderson BM, Arthur DW, Bazan JG, Bellon JR, Bradfield L, et al. Partial breast irradiation for patients with early-stage invasive breast Cancer or Ductal Carcinoma in situ: an ASTRO Clinical Practice Guideline. Pract Radiat Oncol. 2023. https://doi.org/10.1016/J.PRRO.2023.11.001.
Bonin K, McGuffin M, Presutti R, Harth T, Mesci A, Feldman-Stewart D, et al. Breast Cancer patients’ preferences for Adjuvant Radiotherapy Post Lumpectomy: whole breast irradiation vs. partial breast irradiation-single institutional study. J Cancer Educ. 2018;33:37–43.
Hoopes DJ, Kaziska D, Chapin P, Weed D, Smith BD, Hale ER, et al. Patient preferences and physician practice patterns regarding breast radiotherapy. Int J Radiat Oncol Biol Phys. 2012;82:674–81.
Qi XS, White J, Li XA. Is α/β for breast cancer really low? Radiother Oncol. 2011;100:282–8.
Bentzen SM, Yarnold JR. Reports of unexpected late side-effects of accelerated partial breast irradiation– radiobiological considerations. Int J Radiat Oncol Biol Phys. 2010;77:969.
Thomsen MS, Alsner J, Nielsen HM, Jakobsen EH, Nielsen MH, Møller M, et al. Volume matters: breast induration is associated with irradiated breast volume in the Danish breast Cancer Group phase III randomized partial breast irradiation trial. Radiother Oncol. 2022;177:231–5.
Coles CE, Aristei C, Bliss J, Boersma L, Brunt AM, Chatterjee S, et al. International guidelines on Radiation Therapy for breast Cancer during the COVID-19 pandemic. Clin Oncol. 2020;32:279–81.
Murray Brunt A, Haviland JS, Wheatley DA, Sydenham MA, Alhasso A, Bloomfield DJ, et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5-year efficacy and late normal tissue effects results from a multicentre, non-inferiority, randomised, phase 3 trial. Lancet. 2020;395:1613–26.
Vicini F, Broughman J, Halima A, Mayo Z, Obi E, Al-Hilli Z et al. Delivery of Adjuvant Radiation in 5 days or less after lumpectomy for breast Cancer: a systematic review. https://doi.org/10.1016/j.ijrobp.2021.11.026.
Smith BD, Bellon JR, Blitzblau R, Freedman G, Haffty B, Hahn C et al. Radiation therapy for the whole breast: executive summary of an American Society for Radiation Oncology (ASTRO) evidence-based guideline. 2018. https://doi.org/10.1016/j.prro.2018.01.012.
Bartelink H, Maingon P, Poortmans P, Weltens C, Fourquet A, Jager J, et al. Whole-breast irradiation with or without a boost for patients treated with breast-conserving surgery for early breast cancer: 20-year follow-up of a randomised phase 3 trial. Lancet Oncol. 2015;16:47–56.
Matuschek C, Bölke E, Haussmann J, Mohrmann S, Nestle-Krämling C, Gerber PA et al. The benefit of adjuvant radiotherapy after breast conserving surgery in older patients with low risk breast cancer- a meta-analysis of randomized trials. Radiat Oncol. 2017;12.
Chesney TR, Yin JX, Rajaee N, Tricco AC, Fyles AW, Acuna SA, et al. Tamoxifen with radiotherapy compared with tamoxifen alone in elderly women with early-stage breast cancer treated with breast conserving surgery: a systematic review and meta-analysis. Radiother Oncol. 2017;123:1–9.
Kunkler IH, Williams LJ, Jack WJL, Cameron DA, Dixon JM. Breast-conserving surgery with or without irradiation in early breast Cancer. N Engl J Med. 2023;388:585–94.
Crivellari D, Spazzapan S, Puglisi F, Fratino L, Scalone S, Veronesi A. Hormone therapy in elderly breast cancer patients with comorbidities. Crit Rev Oncol Hematol. 2010;73:92–8.
Meattini I, Poortmans PMP, Marrazzo L, Desideri I, Brain E, Hamaker M, et al. Exclusive endocrine therapy or partial breast irradiation for women aged ≥ 70 years with luminal A-like early stage breast cancer (NCT04134598 - EUROPA): Proof of concept of a randomized controlled trial comparing health related quality of life by patient reported outcome measures. J Geriatr Oncol. 2021;12:182–9.
Funding
This research was supported by the Ministry of Health of the Czech Republic — conceptual development of research organization (MMCI, 00209805), by the project NV19-03-00354, by the project National Institute for Cancer Research (Programme EXCELES, ID Project No. LX22NPO5102)— Funded by the European Union — Next Generation EU, by the LRI projects CZECRIN (no. LM2023049) and BBMRI.cz (no. LM2023033) and by European Regional Development Fund (project no. CZ.02.1.01/0.0/0.0/16_013/0001674).
Author information
Authors and Affiliations
Contributions
PB, TK, and MS were responsible for the conception and design of the study. PB, MS, MV, OC, KP, and PM collected the patient data. IS performed a formal analysis. MV and KP provided provide technical support. PB, IS, MS, MH, and TK interpreted the data. PB, IS, MS, MH, and TK were major contributors to the manuscript’s draft. TK and PS supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethical Board of Masaryk Memorial Cancer Institute (MMCI; approval No. 2017/1889/MOU). Written informed consent was received from each patient prior to enrolment.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplement Material 1. Supplementary Table 1
: Dose constraints and plan optimization. Supplementary Figure 1: Dose distribution and beam arrangement for APBI arm
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Burkon, P., Selingerova, I., Slavik, M. et al. Toxicity of external beam accelerated partial-breast irradiation (APBI) in adjuvant therapy of early-stage breast cancer: prospective randomized study. Radiat Oncol 19, 17 (2024). https://doi.org/10.1186/s13014-024-02412-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-024-02412-x