Abstract
Objective
The purpose of this study was to evaluate the efficacy of postoperative adjuvant radiotherapy for patients with upper tract urothelial carcinoma (UTUC) who underwent kidney-sparing surgery (KSS).
Methods
We retrospectively reviewed the clinical records of 31 patients with primary UTUC who underwent kidney-sparing surgery (KSS) and who were treated with adjuvant radiotherapy at our center between October 1998 and May 2017. Statistical analyses were performed with SPSS 23.0. The primary endpoints of this study included overall survival (OS) and local recurrence-free survival (LRFS); the secondary endpoints were disease-free survival (DFS) and treatment-related toxicity.
Results
The median follow-up was 58.4 months (range, 12.7-185.3 months), and the median local recurrence time was 59.0 months (range, 7.0-185 months). All of the patients completed radiotherapy on schedule, and no grade 3–4 late-stage reaction was observed. The estimated 5-year and 10-year OS, DFS and LRFS rates of the patients were 64.0%, 61.1%, 69.6% and 48.0%, 40.9%, 64.6%, respectively. Univariate analysis showed that age (χ2 = 4.224, P = 0.040), R0 resection (χ2 = 3.949, P = 0.047), and early stage (I + II) (χ2 = 6.515, P = 0.011) were associated with good OS; DFS benefit in early stage patients (χ2 = 6.151, P = 0.013) and age<70 years old (χ2 = 5.091, P = 0.024). Patients with distal ureteral segments had better LRFS than patients with proximal ureteral cancer (χ2 = 5.248, P = 0.022). However, multivariate analysis showed that age was the only factor of OS (χ2 = 4.099, P = 0.043).
Conclusion
Adjuvant radiotherapy is safe and tolerated, and LRFS was superior in middle and distal ureteral cancer than in proximal ureteral cancer.
Similar content being viewed by others
Introduction
Upper tract urothelial carcinoma (UTUC) is an uncommon cancer accounting for approximately 5–10% of all urothelial carcinomas [1]. Nearly 60% of UTUC patients have invasive disease, and approximately 25% of patients have regional metastasis at the time of diagnosis. Radical nephroureterectomy (RNU) with bladder-cuff removal is the gold standard treatment for high-risk UTUC with a good outcome for early-stage patients [2]. However, postoperative adjuvant therapies are limited due to the significant loss of renal function after removal of a renal unit during RNU, and administration of adjuvant chemotherapy is challenging. It has been reported that the 5-year cancer-specific survival rate for patients with pT2/pT3 tumors is less than 50%, and it is less than 10% for patients with T4 or N + disease [3]. Recently, for patients with low-risk UTUC, including the following factors: unifocal disease, tumor size < 2 cm, low-grade cytology, low-grade ureteroscopic biopsy and no invasion on CT urography (CTU), there has been an increasing tendency toward kidney-sparing surgery (KSS), including segmental ureterectomy (SU) [4]. A meta-analysis showed that there was no difference in HR for cancer-specific survival (CSS) or overall survival (OS) between RNU and SU [5], but the risk of local and bladder recurrence remains relatively high. In consideration of a 30–50% local recurrence rate even when postoperative chemotherapy is conducted [6,7,8], it is necessary to initiate new strategies to improve efficacy.
Postoperative radiotherapy can significantly improve the local control rate in many carcinomas [9]. However, the efficacy of postoperative radiotherapy in UTUC is unclear due to the rarity of the disease. Recent studies have shown that adjuvant radiotherapy can decrease the 3-year local recurrence rate (LRR) from 39 to 11% and improve overall survival [10, 11]. Liu et al. explored the potential safety and effectiveness of radiotherapy as a curative treatment for UTUC patients who cannot undergo surgery for several reasons, such as unresectable disease, old age, and multiple comorbidities [12]. Because of the high risk of local and bladder recurrence, vigilant radiographic and endoscopic surveillance of the bladder and the ipsilateral upper tract are required after KSS [4]. However, the efficacy and safety of postoperative adjuvant radiotherapy in patients with KSS have not been reported. Meanwhile, previous research results in our center and with a small sample study showed that there was no significant difference in OS between patients treated with postoperative radiotherapy in the non-RNU group and RNU group, so we think that patients with KSS may benefit from postoperative adjuvant radiotherapy [13]. In this article, we further investigated the efficacy of postoperative adjuvant radiotherapy for patients with UTUC who suffered from KSS.
Methods
We retrospectively reviewed the clinical records of patients with primary UTUC who suffered from KSS treated with adjuvant radiotherapy at our center between October 1998 and May 2017. The eligibility criteria were as follows: KSS was conducted and postoperative histologically confirmed UTUC; no distant metastasis; and complete follow-up data were available. Pretreatment evaluation included complete history and physical examination, blood count, renal and liver function, chest and abdomen CT, pelvic magnetic resonance imaging (MRI) and transrectal ultrasound.
Treatment
All patients received a CT simulation (16-slice Philips Brilliance BigBore CT, Netherland) in the supine position with oral and intravenous contrast agents. The gross tumor volume (GTV) and clinical target volume (CTV) were contoured on axial CT slices. The GTV included the primary tumor (GTV-T), which indicated pathological R1 (microscopic positive margins), and the involved lymph nodes (GTV-N). CTV covered GTV-T, GTV-N (if any), and pelvic lymph node regions (including common iliac, internal iliac, external iliac and obturator lymph nodes on the same side of the lesion). When the tumor was located in the upper ureter, the CTV covered the primary tumor, and when the tumor was located in the middle and distal ureter, the field of CTV was extended, including the adjacent ureteral passage region and the bladder or the lymphatic drainage region. Different radiotherapy regimens were given according to the patients’ condition. The planning target volume (PTV) consisted of the CTV with a 5 mm margin expansion. For R1 or lymph node metastasis, a boost of 4 to 20 Gy at 2 Gy per fraction was considered.
Follow-up and evaluation of toxicities
The patients were followed up every 3 months within 2 years after radiotherapy, once every 6 months after 2 years, and once every 5 years after 5 years. The review items included computed tomography (CT), B-scan ultrasonography, and magnetic resonance urography (MRU). Other examinations, including routine blood examination, voided urine cytology, chest radiography, and cystoscopic examination, were also performed during follow-up. Patients with acute and chronic radiotherapy toxicity were evaluated according to the National Cancer Institute Common Toxicity Criteria for Adverse Events (CTCAE), version 5.0.
Statistics
The primary endpoints of this study included overall survival (OS), local recurrence-free survival (LRFS), disease-free survival (DFS), and treatment-related toxicity. OS was defined as the time to death or the last follow-up from the beginning of treatment; DFS was defined as the time to recurrence, metastasis or last follow-up from the beginning of treatment; LRFS was defined as the time to recurrence of the primary tumor (including bladder) or the last follow-up from the beginning of treatment. Survival curves were calculated by the Kaplan‒Meier method and compared using the log-rank test. The Cox proportional hazards model was used to determine the independent factors affecting endpoints based on the variables selected by the univariate analysis. The chi-square test was used for comparisons between groups. Statistical analyses were performed with SPSS 23.0 for Windows (SPSS, Inc., Chicago, IL). P values < 0.05 were considered statistically significant.
Results
The last follow-up was December 31, 2020. Two patients lost to follow-up within one year after radiotherapy were excluded, and a total of 31 patients were enrolled in this study. The median age was 65 years old (range 39–81 years). There were 11 patients ≥ 70 years old, including 6 patients over 75 years old. Two patients had a previous history of bladder cancer of more than 5 years. One patient had a history of colon cancer surgery, and 6 patients had pathological R1. According to the AJCC 8th edition [14], there were 20 (64.5%) and 11 (35.5%) patients with stage I-II and stage III-IV disease, respectively. The major histological types were well-differentiated transitional epithelial cell carcinoma. There were two cases of rare pathological types, including poorly differentiated adenocarcinoma and poorly differentiated squamous cell carcinoma. Most tumors (83.9%) were located in the middle and distal ureter. Renal pelvis involvement occurred in 3 patients, bladder involvement in 4 patients and multifocal disease involvement in 3 patients. Detailed clinical data of these patients are detailed in Table 1.
Treatment and acute toxicities
A total of 4 patients received postoperative chemotherapy due to high-risk pollution. The median time from the operation to the onset of radiation therapy was 41 days (13–229 days), with a median treatment time of 36 days (32–62 days). Three-dimensional conformal radiotherapy (3D-CRT) was conducted in 11 patients, and intensity-modulated radiotherapy (IMRT) was conducted in 20 patients. The median radiotherapy dose was 50 Gy (range 30-61.52 Gy, 1.8 ~ 2.0 Gy/fraction). For 21 patients with distal ureter tumors, 13 of the patients (52%) had the field of CTV that covered the middle ureter and bladder. During the treatment period, there were 8 cases of grade 1–2 acute hematological toxicity, 6 cases of grade 1–2 gastrointestinal toxicity, 10 cases of grade 1–2 urinary system toxicity, and 1 case of concurrent chemotherapy with grade 3 myelosuppression. All of the patients completed radiotherapy on schedule, and no grade 3–4 late-stage reaction was observed.
Pattern of failure and survival
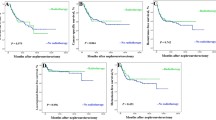
The median follow-up was 58.4 months (range, 12.7-185.3 months), and the median local recurrence time was 59.0 months (range, 7.0-185 months). A second malignant tumor occurred in 1 patient with adenolymphoma of the parotid gland. Twelve patients (38.7%) died due to disease progression. Distant metastasis occurred in 17 patients (54.8%), and local recurrence occurred in 10 patients (32.3%), including 4 patients (12.9%) with bladder recurrence. The estimated 5-year and 10-year OS, DFS and LRFC rates of patients were 64.0%, 61.1%, and 69.6% and 48.0%, 40.9%, and 64.6%, respectively. The OS and LC rate curves are shown in Fig. 1. Univariate analysis showed that age (χ2 = 4.224, P = 0.040), R0 resection (χ2 = 3.949, P = 0.047), and early stage (I + II) (χ2 = 6.515, P = 0.011) were associated with good OS; DFS benefit in early stage patients (χ2 = 6.151, P = 0.013) and age<70 years old (χ2 = 5.091, P = 0.024). Patients with distal ureteral segments had a better LRFC than patients with proximal ureteral cancer (χ2 = 5.248, P = 0.022). The analysis of prognostic factors is shown in Table 2. However, multivariate analysis showed that age was the only factor of OS (χ2 = 4.099, P = 0.043).
Discussion
UTUC is a rare urinary system tumor, accounting for only 5% of all urinary system tumors in the Western population. The incidence in the Asian population has increased slightly as a result of taking traditional Chinese medicines containing aristolochic acid. UTUC accounts for 20–25% of all urinary system tumors. The prognosis of primary ureteral carcinoma is poor. This may be due to the thin wall of the ureter, which allows the tumor to pass through the basal layer easily, and the rich lymph around the ureter is prone to local invasion and metastasis. Good results can be obtained by a simple operation in patients with early ureteral carcinoma. Hall et al. reported that the 5-year disease-free survival rates of patients with pTa, pT1, pT2, pT3 and pT4 were 100%, 91.7%, 72.6%, 40.5% and 0%, respectively. However, a number of studies have shown that for patients with tumors above stage III, the OS rate of more than 5 years ranges from 12 to 64% [2, 11, 15, 16].
In UTUC, due to the significant loss of renal function after removal of a rental unit during RNU, administration of adjuvant chemotherapy is challenging [17, 18]. Recent large-scale evidence from the National Cancer Database (NCDB) showed that patients with locally advanced or node-positive disease could benefit from adjuvant treatment (HR 0.77). However, no studies have shown that adjuvant chemotherapy had a survival benefit for patients with KSS [19]. In our study, only 4 (11.1%) patients were treated with postoperative chemotherapy, and there was no significant difference in OS and DFS due to the small sample size.
The effectiveness of postoperative adjuvant radiotherapy for UTUC has been controversial. Chen et al. [11] and Fan K et al. [20] showed that postoperative radiotherapy could improve the OS of patients with T3-4 tumors. Li HZ et al.’s [21] studies showed that adjuvant radiotherapy significantly improved 5-year RFS compared with partial ureterectomy alone, and partial ureterectomy combined with adjuvant radiotherapy did not significantly improve 5-year RFS compared with radical nephroureterectomy. Jwa E et al. [10] showed that adjuvant radiotherapy could improve the local control rate and could reduce the bladder recurrence rate but did not improve OS or PFS. Chang YH et al.’s [22] study yielded similar results. However, a KSS approach is advocated for low-risk tumors or for high-risk tumors when there is an imperative indication (renal insufficiency or solitary functioning kidney), and whether postoperative adjuvant radiotherapy is beneficial in patients with KSS has not been studied. In our respective study, the estimated 5-year OS, DFS and LC rates of patients were 64.0%, 61.1%, and 69.6%, respectively. The effective rates were higher than those of patients who underwent surgery alone reported in the literature [23, 24] and similar to those of postoperative radiotherapy groups [11, 25]. Bladder recurrence is common postoperatively in patients with UTUC and a risk factor for a poor prognosis [26]. The bladder recurrence rate can reach 27 to 47% [27, 28] after surgery, as described in the literature. In our study, the bladder recurrence rate was 12.9%, much lower than that in previous reports.
At present, there is no consensus on the radiation range of postoperative radiotherapy for UTUC. In most centers, CTV covers only the tumor bed area, the regional lymph node drainage area, and the retroperitoneal lymph node drainage areas with definite or suspected lymph node metastasis [20, 22, 25, 29]. However, in 2011, Chen’s study clearly defined the irradiation range, which included the renal pelvis, the full length of the ureter, the whole bladder and the retroperitoneal lymph node drainage area, in 53 patients – the most extensive group examined among all known studies. Chen et al. also mentioned that radiotherapy reduces the incidence of bladder recurrence (38.7–13.2%, p < 0.001) and recommended that the target area of radiotherapy include the whole bladder [11]. Belhadj Y found that bladder recurrence could occur anywhere in postoperative patients with UTUC [30], which also supports whole bladder irradiation. However, the rate of acute bladder toxicity (grades 1 and 2) was 58.2%, and the rate of grade 3 or above toxicity was 3%. Meanwhile, the literature showed that patients with lower ureteral tumors had a higher prevalence of deaths (HR = 2.227) than patients with upper ureteral tumors [31]. Therefore, in our study, the target volume covering the bladder was carried out for patients with middle and distal ureteral tumors, and a better LRFC was observed (χ2 = 5.248, P = 0.022). In most studies, tumor stage, grade or other variables, including age, tumor location, lymph node involvement, multifocality, and tumor architecture, were considered the most important prognostic factors for UTUC [32,33,34]. In this study, univariate analysis showed that R0 resection (χ2 = 4.098, P = 0.043), early stage (I + II) (χ2 = 6.485, P = 0.011) and low-risk population (χ2 = 4.079, P = 0.043) were associated with good OS, but multivariate analysis showed that age was the only factor of OS, perhaps due to the percentage of patients aged ≥ 75 years accounting for 22.2% (8/36). Therefore, for patients with kidney protection requirements (especially older patients), postoperative adjuvant radiotherapy may be a feasible choice.
Conclusion
Adjuvant radiotherapy is safe and tolerated, and LRFS was superior in middle and distal ureteral cancer than in proximal ureteral cancer. With the development of immune checkpoint inhibitors in ureteral cancer, whether OS can be improved in KSS patients by immune combination with radiotherapy needs to be further explored.
Availability of supporting data
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33.
Roupret M, Babjuk M, Burger M, Capoun O, Cohen D, Comperat EM, Cowan NC, Dominguez-Escrig JL, Gontero P, Hugh Mostafid A, et al. European Association of Urology Guidelines on Upper urinary tract Urothelial Carcinoma: 2020 update. Eur Urol. 2021;79(1):62–79.
Abouassaly R, Alibhai SM, Shah N, Timilshina N, Fleshner N, Finelli A. Troubling outcomes from population-level analysis of surgery for upper tract urothelial carcinoma. Urology. 2010;76(4):895–901.
Lucca I, Klatte T, Roupret M, Shariat SF. Kidney-sparing surgery for upper tract urothelial cancer. Curr Opin Urol. 2015;25(2):100–4.
Zhang J, Yang F, Wang M, Niu Y, Chen W, Xing N. Comparison of Radical Nephroureterectomy and Partial Ureterectomy for the Treatment of Upper Tract Urothelial Carcinoma. Biomed Res Int 2018, 2018:2793172.
Zigeuner RE, Hutterer G, Chromecki T, Rehak P, Langner C. Bladder tumour development after urothelial carcinoma of the upper urinary tract is related to primary tumour location. BJU Int. 2006;98(6):1181–6.
Elawdy MM, Osman Y, Taha DE, Zahran MH, El-Halwagy S, Garba ME, Harraz AM. Risk factors and prognosis of intravesical recurrence after surgical management of upper tract urothelial carcinoma: a 30-year single centre experience. Arab J Urol. 2017;15(3):216–22.
Terakawa T, Miyake H, Muramaki M, Takenaka A, Hara I, Fujisawa M. Risk factors for intravesical recurrence after surgical management of transitional cell carcinoma of the upper urinary tract. Urology. 2008;71(1):123–7.
Schaue D, McBride WH. Opportunities and challenges of radiotherapy for treating cancer. Nat Rev Clin Oncol. 2015;12(9):527–40.
Jwa E, Kim YS, Ahn H, Kim CS, Lee JL, Kim SO. Adjuvant radiotherapy for stage III/IV urothelial carcinoma of the upper tract. Anticancer Res. 2014;34(1):333–8.
Chen B, Zeng ZC, Wang GM, Zhang L, Lin ZM, Sun LA, Zhu TY, Wu LL, Zhang JY, Ji Y. Radiotherapy may improve overall survival of patients with T3/T4 transitional cell carcinoma of the renal pelvis or ureter and delay bladder tumour relapse. BMC Cancer. 2011;11:297.
Liu MZ, Gao XS, Qin SB, Li XY, Ma MW, Xie M, Lyu F, Wang D. Radiation therapy for nonmetastatic medically inoperable upper-tract urothelial carcinoma. Transl Androl Urol. 2021;10(7):2929–37.
Hu K, Hou XR,Shen J, Lian XSun, Sh,Zhang. FQ.Treatment results and prognostic analysis of 47 patients with urethral transitional cell carcinoma treated with post-operative adjuvant radiotherapy. Chin J Radiat Oncol. 2012;19(3):247–9.
Trotti A, Byhardt R, Stetz J, Gwede C, Corn B, Fu K, Gunderson L, McCormick B, Morrisintegral M, Rich T, et al. Common toxicity criteria: version 2.0. An improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys. 2000;47(1):13–47.
Chang YH, Hsiao PJ, Chen GH, Lin CC, Chang CH, Wu HC, Huang CP, Yang CR, Yeh SP. Outcomes of stage II-IV upper-tract urothelial carcinoma and adjuvant chemotherapy for locally advanced cancer. Oncol Lett. 2019;17(1):1341–8.
Margulis V, Shariat SF, Matin SF, Kamat AM, Zigeuner R, Kikuchi E, Lotan Y, Weizer A, Raman JD, Wood CG, et al. Outcomes of radical nephroureterectomy: a series from the Upper Tract Urothelial Carcinoma collaboration. Cancer. 2009;115(6):1224–33.
Galsky MD, Stensland KD, Moshier E, Sfakianos JP, McBride RB, Tsao CK, Casey M, Boffetta P, Oh WK, Mazumdar M, et al. Effectiveness of Adjuvant Chemotherapy for locally advanced bladder Cancer. J Clin Oncol. 2016;34(8):825–32.
Kaag MG, O’Malley RL, O’Malley P, Godoy G, Chen M, Smaldone MC, Hrebinko RL, Raman JD, Bochner B, Dalbagni G, et al. Changes in renal function following nephroureterectomy may affect the use of perioperative chemotherapy. Eur Urol. 2010;58(4):581–7.
Freifeld Y, Krabbe LM, Clinton TN, Woldu SL, Margulis V. Therapeutic strategies for upper tract urothelial carcinoma. Expert Rev Anticancer Ther. 2018;18(8):765–74.
Fan KH, Chen YC, Leung WM, Chuang CK, Pang ST, Hong JH. Adjuvant and salvage radiotherapy for urothelial cell carcinoma of the upper urinary tract: experience in a single institution. Chang Gung Med J. 2012;35(3):247–54.
Li HZ, Li X, Gao XS, Qi X, Ma MW, Qin S. Oncological outcomes of adjuvant radiotherapy for partial ureterectomy in Distal Ureteral Urothelial Carcinoma Patients. Front Oncol. 2021;11:699210.
Huang YC, Chang YH, Chiu KH, Shindel AW, Lai CH. Adjuvant radiotherapy for locally advanced upper tract urothelial carcinoma. Sci Rep. 2016;6:38175.
Ozsahin M, Zouhair A, Villa S, Storme G, Chauvet B, Taussky D, Gouders D, Ries G, Bontemps P, Coucke PA, et al. Prognostic factors in urothelial renal pelvis and ureter tumours: a multicentre Rare Cancer Network study. Eur J Cancer. 1999;35(5):738–43.
Hall MC, Womack S, Sagalowsky AI, Carmody T, Erickstad MD, Roehrborn CG. Prognostic factors, recurrence, and survival in transitional cell carcinoma of the upper urinary tract: a 30-year experience in 252 patients. Urology. 1998;52(4):594–601.
Czito B, Zietman A, Kaufman D, Skowronski U, Shipley W. Adjuvant radiotherapy with and without concurrent chemotherapy for locally advanced transitional cell carcinoma of the renal pelvis and ureter. J Urol. 2004;172(4 Pt 1):1271–5.
Elawdy MM, Osman Y, Taha DE, El-Halwagy S. Muscle-invasive bladder and urethral cancer recurrence after surgical management of upper tract urothelial carcinoma: a review of 305 patients. Turk J Urol. 2018;44(3):213–20.
O’Brien T, Ray E, Singh R, Coker B, Beard R. British Association of Urological Surgeons section of O: Prevention of bladder tumours after nephroureterectomy for primary upper urinary tract urothelial carcinoma: a prospective, multicentre, randomised clinical trial of a single postoperative intravesical dose of mitomycin C (the ODMIT-C trial). Eur Urol. 2011;60(4):703–10.
Guan B, Cao ZP, Peng D, Li YF, Zhan YH, Liu LB, He SM, Xiong GY, Li XS, Zhou LQ. [Prognostic factors of patients with T2N0M0 upper tract urothelial carcinoma: a single-center retrospective study of 235 patients]. Beijing Da Xue Xue Bao Yi Xue Ban. 2017;49(4):603–7.
Hahn AW, Giri S, Pathak R, Bhatt VR, Martin MG. Effect of Adjuvant Radiotherapy on Survival in patients with Locoregional Urothelial Malignancies of the Upper urinary tract. Anticancer Res. 2016;36(8):4051–5.
Belhadj Y, Grande P, Seisen T, Gobert A, Gomez FD, Cussenot O, Roupret M. Bladder mapping of tumour recurrence after radical nephroureterectomy for upper tract urothelial carcinoma and its influence on oncological outcomes. BJU Int. 2019;123(4):618–23.
Inamoto T, Matsuyama H, Komura K, Ibuki N, Fujimoto K, Shiina H, Sakano S, Nagao K, Mastumoto H, Miyake M, et al. Tumor Location based segmentation in Upper-Tract Urothelial Carcinoma Impacts on the Urothelial recurrence-free survival: a multi-institutional database study. Curr Urol. 2020;14(4):183–90.
Lucca I, Kassouf W, Kapoor A, Fairey A, Rendon RA, Izawa JI, Black PC, Fajkovic H, Seitz C, Remzi M, et al. The role of adjuvant chemotherapy for lymph node-positive upper tract urothelial carcinoma following radical nephroureterectomy: a retrospective study. BJU Int. 2015;116(1):72–8.
Li X, Cui M, Gu X, Fang D, Li H, Qin S, Yang K, Zhu T, Li X, Zhou L, et al. Pattern and risk factors of local recurrence after nephroureterectomy for upper tract urothelial carcinoma. World J Surg Oncol. 2020;18(1):114.
Kluth LA, Xylinas E, Kent M, Hagiwara M, Kikuchi E, Ikeda M, Matsumoto K, Dalpiaz O, Zigeuner R, Aziz A, et al. Predictors of survival in patients with disease recurrence after radical nephroureterectomy. BJU Int. 2014;113(6):911–7.
Acknowledgements
This work was supported by the Key Project of the National Natural Science Foundation of China (U19A2064).
Author information
Authors and Affiliations
Contributions
Professor Ke Hu and Jing Zhao concepted and designed of the study,as well as responsible for the administration. Hui Guan and Guangyu Wang generated, collected, assembled and analysis of data. Weiping Wang, Yuncan Zhou, Zhikai Liu, Xiaorong Hou, Junfang Yan, Shuai Sun took part in this study for technological supporting. Jing Zhao drafted the manuscript and all authors approved of the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval and Consent to participate
We performed a retrospective review of data from patients at Peking Union Medical College Hospital under a study approved by the ethics committee of Peking Union Medical College Hospital, Beijing, China, in accordance with the guidelines of the Declaration of Helsinki (S-K899). Informed consent was obtained from all patients.
Consent for publication
All authors have approved the manuscript for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guan, H., Wang, G., Wang, W. et al. Postoperative adjuvant radiotherapy for patients with upper tract urothelial carcinoma (UTUC) who underwent kidney-sparing surgery (KSS): a single-center study. Radiat Oncol 18, 120 (2023). https://doi.org/10.1186/s13014-023-02303-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-023-02303-7