Abstract
Background
This study was conducted to evaluate the efficiency and accuracy of the daily patient setup for breast cancer patients by applying surface-guided radiation therapy (SGRT) using the Halcyon system instead of conventional laser alignment based on the skin marking method.
Methods and materials
We retrospectively investigated 228 treatment fractions using two different initial patient setup methods. The accuracy of the residual rotational error of the SGRT system was evaluated by using an in-house breast phantom. The residual translational error was analyzed using the couch position difference in the vertical, longitudinal, and lateral directions between the reference computed tomography and daily kilo-voltage cone beam computed tomography acquired from the record and verification system. The residual rotational error (pitch, yaw, and roll) was also calculated using an auto rigid registration between the two images based on Velocity. The total setup time, which combined the initial setup time and imaging time, was analyzed to evaluate the efficiency of the daily patient setup for SGRT.
Results
The average residual rotational errors using the in-house fabricated breast phantom for pitch, roll, and yaw were 0.14°, 0.13°, and 0.29°, respectively. The average differences in the couch positions for laser alignment based on the skin marking method were 2.7 ± 1.6 mm, 2.0 ± 1.2 mm, and 2.1 ± 1.0 mm for the vertical, longitudinal, and lateral directions, respectively. For SGRT, the average differences in the couch positions were 1.9 ± 1.2 mm, 2.9 ± 2.1 mm, and 1.9 ± 0.7 mm for the vertical, longitudinal, and lateral directions, respectively. The rotational errors for pitch, yaw, and roll without the surface-guided radiation therapy approach were 0.32 ± 0.30°, 0.51 ± 0.24°, and 0.29 ± 0.22°, respectively. For SGRT, the rotational errors were 0.30 ± 0.22°, 0.51 ± 0.26°, and 0.19 ± 0.13°, respectively. The average total setup times considering both the initial setup time and imaging time were 314 s and 331 s, respectively, with and without SGRT.
Conclusion
We demonstrated that using SGRT improves the accuracy and efficiency of initial patient setups in breast cancer patients using the Halcyon system, which has limitations in correcting the rotational offset.
Similar content being viewed by others
Background
In recent years, surface-guided radiation therapy (SGRT), which uses the three-dimensional (3D) surface of the patient in real-time using optical imaging, has been widely adopted as a patient setup and monitoring method [1,2,3,4,5,6,7,8,9]. Because the accuracy of radiation therapy is closely related to the patient setup, it is important to verify that between the simulation and treatment, the patient position is consistent [10]. SGRT provides real-time six degrees of freedom (6-DOF) surface information in the treatment room for a reference body contour acquired from treatment planning CT [1, 2, 5, 6]. The 6-DOF information without an additional imaging dose can be used to monitor the intra-fractional motion during treatment and provide the necessary correction information for the patient’s reference position. In particular, SGRT allows for more accurate positioning compared with conventional laser alignment based on skin marking (LAS) and could reduce the extent of daily imaging in some cases [4]. In addition, it is an effective method for reducing the overall setup time, which can minimize the time required for image registration [7]. LAS, which is routinely used as a reference for the initial patient setup for treatment as well as for simulation in our hospital, has the advantage of being a simple and non-invasive method. However, it is primarily based on the therapist’s perspective, thus making the initial patient setup method user-dependent and inaccurate. In some cases, it corrects according to the skin rather than the position of the entire body because of the elasticity of human skin [5, 6].
With an increasing number of patients undergoing hypo-fractionated whole breast radiotherapy (WBRT) or accelerated partial breast irradiation (APBI), the use of intensity-modulated radiation therapy (IMRT) or volumetric modulated arc therapy (VMAT), which can achieve highly conformal dose distributions, has increased [11, 12]. However, uncertainties related to the patient setup may lead to inaccuracies in dose delivery; in particular, because of the steep dose gradient, the efficacy of IMRT and VMAT can be limited and the patient outcomes for both local tumor control and normal tissue complications can be affected [13]. In particular, because breast tissue is highly deformable, reproducing the patient setup is often challenging in patients with breast cancer. Several studies have shown SGRT to be a useful method for improving the accuracy and efficiency of the patient setup compared to conventional tattoo/laser-based method with the potential to reduce the frequency of routine image guided radiation therapy [1,2,3,4,5,6,7,8,9, 14,15,16,17,18,19,20,21,22].
The Halcyon™ linear accelerator (LINAC) (Varian Medical System, Palo Alto, CA, USA) is a bore-enclosed LINAC that corrects the patient setup position in every fraction using kV or MV imaging systems. Unlike the C-type LINAC, the patient’s initial setup is performed in the virtual isocenter, which is approximately 58 cm away from the treatment isocenter in the longitudinal direction, and the patient is then moved into the bore of the treatment isocenter. After moving to the treatment isocenter, the patient’s position is corrected by moving the couch value in terms of the difference value obtained by image registration between the reference imaging and daily imaging. However, it is difficult to correct for rotational errors because the couch in the Halcyon device only allows for translational movement [14, 15]. If a rotational error occurs during the initial setup, the additional imaging dose and the overall setup time increase because the patient must be manually repositioned. Therefore, the initial patient setup in the virtual isocenter is critical since it affects the accuracy and efficiency of the overall treatment. In this study, the accuracy to measure the residual rotational error of the SGRT system was evaluated using in-house breast phantom. Also, unlike most previous studies comparing two group using different initial setup methods, CBCTs obtained from each patient using both initial setup methods were analyzed to evaluate the accuracy and efficiency of SGRT compared with LAS method using Halcyon system. [3,4,5,6,7, 14,15,16]
Methods and materials
After receiving institutional review board approval, a retrospective study was conducted on 38 breast cancer patients treated with the Halcyon LINAC in our hospital. The treatment simulation was performed with a Brilliance CT Big Bore (Philips, Cleveland, OH, USA) using a slice thickness of 2.5 mm and a breast board was used for immobilization and to achieve reproducibility of the patient’s position. The Halcyon LINAC, which contains a 6 MV flattening filter free (FFF) and a dual-layer multi-leaf collimator (MLC), allows fast and accurate IMRT and VMAT based on a kV cone beam CT imaging (kV CBCT) system. Because it is necessary to move from the virtual isocenter to the treatment isocenter after the initial setup, 2D or 3D images should be acquired for every fraction to ensure that the positioning is accurate. Compared with the C-type LINAC, the patient setup for Halcyon Linac can be corrected with only translational error because the treatment couch has 3-DOF. The daily initial setup for each patient was performed by aligning skin markings with room laser for three fractions and by using SGRT for three fractions. In the LAS method, after marking the skin with ink at the reference isocenter during CT simulation, the patients were aligned to the marked locations and were manually shifted by the therapists. For the SGRT method, body surfaces were reconstructed using an imaging system that was used to match the body contours acquired from the reference CT image. After acquiring 6 CBCTs (3 CBCTs with LAS method, 3 CBCTs with SGRT) per patient, a total of 228 CBCTs were analyzed.
SGRT implementation
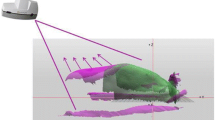
In our study, the AlignRT image-guided system (Version 6.2, Vision RT Ltd., London, UK) was used for SGRT implementation. As shown in Fig. 1, AlignRT, consisting of a three-camera pod system, was installed on the ceiling and aligned to the virtual isocenter to monitor the patient’s initial setup out of the bore. System calibration was performed on the virtual isocenter owing to the area blocked by the O-ring type design. The daily QA for the SGRT system was performed using a plate with a circular pattern before treatment. When the maximum root mean square values representing the average discrepancy of the camera positions between the daily QA and system calibration exceeded 0.8 mm, the system was calibrated. While the initial setup of the patient was performed at the virtual isocenter, the reference body contour generated by the reference CT had the coordinates of the treatment isocenter; therefore, a dummy plan with a couch position without delta couch shift was generated using the Eclipse Scripting API. The region of interest (ROI) for breast cancer patients, which includes breast tissues, ribs, and the lateral aspect of the left and right breast to the midcoronal plane, was generated to monitor the difference in body contour quantitatively. The thresholds for the translational error (vertical, longitudinal, and lateral) and rotational error (pitch, roll, and yaw) were set to 3 mm and 3°, respectively. If the difference in the 6-DOF was within the thresholds, the couch was moved to the treatment isocenter for kV CBCT imaging.
Accuracy verification for rotational error
The accuracy of the residual rotational error of the SGRT system was evaluated by using an in-house breast phantom. An anthropomorphic phantom (Model 702 Adult ATOM Female, CIRS Inc., Norfolk, VA), which is sectional in design with traditional 25 mm thick sections, was scanned with a 1.5 mm slice thickness. A phantom designed with a thickness of 25 mm has dosimetric capabilities, but it is difficult to obtain reproducible surface imaging. Therefore, to be suitable for the SGRT system, a phantom with an opaque/matte, light-colored surface that reflects the projected light pattern was fabricated using 3D printing. The body contours were converted into the standard tessellation language format for 3D printing. The phantom was manufactured from amorphous thermoplastic material using a Zortrax M300 3D printer (Zortrax, Olsztyn, Poland). After CT scanning the 3D printed breast phantom, the body contour was used as reference in the same way as the patient cases. The phantom on the baseplate was set to a virtual isocenter, and rotational errors from − 1.5° to 1.5° in steps of 0.5°were induced for pitch, yaw, and roll using the baseplate, as shown in Fig. 2. The induced rotational errors were acquired using an SGRT system. Then, the rotational error was estimated by matching the body contour imported from Eclipse and acquired surface images using AlighRT, and the kV CBCT scans were acquired. The kV CBCTs were imported into Velocity™ (Version 4.1, Varian Medical Systems Inc.) to verify the residual rotational error using auto rigid registration between the kV CBCT and reference CT.
Data acquisition and analysis
A total of 228 fractions including three fractions with LAS methods and three fractions with the SGRT for each patient acquired from thirty-eight patients prescribed dose of 43.2 Gy in 16 fractions were investigated. Twenty-nine of the patients underwent breast-conserving surgery and nine underwent mastectomy. The accuracy of the initial setup in terms of translational error was quantified by retrospectively analyzing the couch shifts between the reference CT and kV CBCT images. Because the Halcyon couch only moves the translational shift, both the kV CBCT and reference CT were exported into Velocity™ to compare the residual rotational error. The ROI was set to the appropriate dimensions in all three planes (axial, sagittal, and coronal) to include the chest wall and ribs to be fused. After fusing the two images, the rotational errors for the pitch, roll, and yaw were obtained from the automatic registration results. The setup efficiency was analyzed by comparing the initial setup and imaging times. The initial setup times were acquired by measuring the timestamp of the record and verification (R&V) system, starting from the instant the patient was loaded into the system and ending when the images were acquired. The imaging time was defined as from start of kV beam irradiation until after couch shift performed by the auto-and manual image registration by measuring the timestamps of R&V system. Patient data were analyzed by calculating mean, median, maximum, and quartile distributions. A paired t-test was used to establish the statistical significance of the results at P < 0.05.
Results
Accuracy verification for rotational error
Figure 3 presents the results for the residual rotational error of the SGRT using an in-house phantom. These rotational errors indicate good agreement between SGRT and induced rotational error, compared with the rigid registration of the daily kV CBCT and reference CT. The mean residual rotational errors in the SGRT for pitch, yaw, and roll were 0.14°, 0.29°, and 0.13°, respectively. The largest error between the two systems was for yaw and the smallest difference was for roll. The maximum difference between the induced and SGRT systems in all directions was 0.40°.
Initial setup accuracy
A comparison of the kV CBCT translational and rotational errors with and without SGRT is presented in Table 1. The average translational errors for the vertical, longitudinal, and lateral directions in the case of the LAS methods were 0.27 mm, 0.2 mm, and 0.21 mm, respectively. Compared with the LAS method, the average translational error using SGRT showed vertical and lateral improvements in the patient setup. However, it was confirmed that the translational error significantly decreased longitudinally using the LAS method. The average rotational errors for pitch, yaw, and roll using the LAS method were 0.32°, 0.51°, and 0.29°, respectively. By contrast, the average rotational difference for roll was significantly reduced using SGRT; however, yaw was similar to that of the LAS method. The respective average rotational errors for pitch, roll, and yaw using the SGRT were 0.3, 0.51, and 0.19.
Setup efficiency
Table 2 summarizes the initial setup and imaging times of the two setup methods. The average initial setup times were 185 s and 187 s using the LAS method and SGRT, respectively. No significant differences were observed in the initial setup time. However, the imaging time was reduced by approximately 13% using SGRT, which was statistically significant. The average total setup times considering both the initial setup time and imaging time were 314 s and 331 s with and without SGRT, respectively. It was confirmed that the efficiency of the total setup time in the SGRT was significantly improved by approximately 5% compared to that of the LAS method.
Discussion
The accuracy and efficiency of using SGRT implemented on the recently installed Halcyon LINAC were evaluated based on both the phantom and patients. Many studies have reported the advantages of SGRT for various sites such as the head and neck, breast, abdomen, and pelvis [2,3,4,5,6,7,8,9, 14,15,16,17,18,19,20,21,22]. In particular, Fores-Martinez et al. reported that the use of SGRT on Halcyon allowed for a reduction of additional imaging during patient setup in non-SRS intracranial treatment, more accurate and faster initial setups for breast patients by reducing both re-alignment and repeat imaging [15]. Nguyen et al. [14] showed that the SGRT decrease the translational setup error significantly by up to 2.1 cm compared with tattoos and rotational error by approximately 35%. Most of these studies compared patient groups using two different methods, while this study compared the results of using both methods (LAS vs. SGRT) for one patient, showing that using SGRT can reduce total setup time as well as initial setup error. [1,2,3,4,5,6,7,8,9, 14,15,16,17,18,19,20,21,22]
To establish a reference for SGRT accuracy in measuring rotational error, using 3D printing, we fabricated an in-house breast phantom and a base plate capable of applying arbitrary rotational error. Unlike previous studies, because the inside of the phantom used in our study did not employ high-density material, auto rigid registration was mainly performed by matching the phantom surface, which had a relatively high contrast [14, 17]. Therefore, it was considered more suitable for evaluating the systematic accuracy of the rotational error for SGRT using only surface information. The maximum difference between the SGRT and auto rigid registration for pitch, roll, and yaw was 0.4° in our study, which is comparable to the results of a study by Mancosu et al., who reported an estimated maximum rotational error of ± 0.3° for SGRT [17].
Flores‐Martinez et al. [15] reported that there was a significant decrease in residual rotational error in pitch, but not in yaw and roll, for the patient setup in Halcyon with SGRT. By contrast, in our study, the average residual rotational error for roll was significantly decreased using SGRT. There was a slight decrease in the average residual rotational error in pitch, but it was not statistically significant, and yaw remained the same with and without the SGRT. Nguyen et al. reported that SGRT significantly reduced setup errors compared with tattoos in all translational directions in patients with breast cancer [14]. They also showed that additional information acquired by the SGRT system can improve the positioning accuracy of breast cancer patients compared with the laser-based setup [14]. However, our study showed that only the average residual translational error in the vertical direction decreased significantly, but increased in the longitudinal direction. The average longitudinal translational error was larger for both tattoos and SGRT in the study by Cravo et al. [18]. This errors are affected by respiratory induced chest wall motion, and a larger longitudinal difference was observed in our study. This is probably because the longitudinal direction, which is limited in accuracy by the flatness of the body surface, caused larger error in SGRT due to combination of respiratory induced motion [22].
Most studies have reported that SGRT offered a reduced average setup time compared with the tattoo or LAS methods [1,2,3,4,5,6,7,8,9]. However, SGRT increased the average initial setup time by approximately 2 s. It may take relatively more time to reach the initial setup because the initial setup should be performed within the tolerance for the quantitative value of 6-DOF. This allows therapists to use more information during the initial setup to create a more accurate patient setup. However, it was confirmed that the imaging time and the overall setup time were significantly reduced. Because the accuracy of the initial setup using SGRT was better, it could be shorter to match the reference image and daily kV CBCT image than LAS method. In particular, the imaging time can be reduced through the result of the better initial setup accuracy by reducing rotational error in Halcyon couch which is difficult to correct rotational error. Breast tissue, for which it is difficult to ensure setup reproducibility because it is soft and non-rigid, limits the accuracy of setups when using the tattoo or LAS methods. Sometimes, because PTV for breast cancer patient which include the supraclavicular lymph node is large and complex, SGRT which uses quantitative information of 6DOF is more suitable for breast cancer patient. In addition, as the 6-DOF information shown by the SGRT system can reduce inter-therapist variation, the reproducibility of the patient setup can be improved.
When SGRT was applied to the treatment of breast cancer patients in the Halcyon system, which has a limitation in correcting the rotational error, similarly to the other studies, our results showed its advantage in terms of accuracy and efficiency of patient setup. In addition, many studies have emphasized SGRT as a convenient and effective tool for initial patient setup and comfort because tattoos or markings were not applied to the patient's skin [3, 21]. Compared to the LAS method, patients were satisfied with the absence of marking within the skin; in particular, the additional task of therapists could be reduced because they did not need to reapply the skin marking. However, it is currently impossible for an SGRT system installed in Halcyon to monitor patient motion in the treatment isocenter located in the bore during treatment. Therefore, monitoring using an in-bore camera, which enables intra-fractional motion monitoring using the treatment camera, will be performed in a future study.
Conclusion
The use of SGRT was confirmed to be valuable for reducing the daily setup error compared to the patient’s daily setup using ink-based skin marking. In SGRT, a more accurate patient setup can be effected by reducing the rotational errors that are difficult to correct owing to the lack of capacity for couch movement in Halcyon systems. In addition, it was confirmed that the imaging time could be reduced by using SGRT, and that treatment efficiency increased owing to a reduction in the total setup time. SGRT for breast cancer patients using Halcyon systems can facilitate efficient and accurate setups compared with the conventional ink-marking method.
Availability of data and materials
The datasets supporting the study conclusions are included within this manuscript.
Abbreviations
- SGRT:
-
Surface-guided radiation therapy
- 3D:
-
Three-dimensional
- 6-DOF:
-
Six degrees of freedom
- LAS:
-
Laser alignment based on skin marking
- WBRT:
-
Whole breast radiotherapy
- APBI:
-
Accelerated partial breast irradiation
- IMRT:
-
Intensity-modulated radiation therapy
- FFF:
-
Flattening filter free
- MLC:
-
Multi-leaf collimator
- kV CBCT:
-
KV cone beam CT
- VMAT:
-
Volumetric modulated arc therapy
- R&V:
-
Record and verification
References
Al-Hallaq HA, et al. AAPM task group report 302: surface-guided radiotherapy. Med Phys. 2022;49(4):e82–112.
Leong B, Padilla L. Impact of use of optical surface imaging on initial patient setup for stereotactic body radiotherapy treatments. J Appl Clin Med Phys. 2019;20(12):149–58.
Stanley DN, McConnell KA, Kirby N, Gutiérrez AN, Papanikolaou N, Rasmussen K. Comparison of initial patient setup accuracy between surface imaging and three point localization: a retrospective analysis. J Appl Clin Med Phys. 2017;18(6):58–61.
Kügele M, Mannerberg A, Nørring Bekke S, Alkner S, Berg L, Mahmood F, Ceberg S. Surface guided radiotherapy (SGRT) improves breast cancer patient setup accuracy. J Appl Clin Med Phys. 2019;20(9):61–8.
Wiant DB, et al. Surface imaging-based analysis of intrafraction motion for breast radiotherapy patients. J Appl Clin Med Phys. 2014;15(6):147–59.
Naidoo W, Leech M. Feasibility of surface guided radiotherapy for patient positioning in breast radiotherapy versus conventional tattoo-based setups-a systematic review. Tech Innov Patient Support Radiat Oncol. 2022;22:39–49.
Jimenez RB, et al. Tattoo free setup for partial breast irradiation: a feasibility study. J Appl Clin Med Phys. 2019;20(4):45–50.
Padilla L, et al. A survey of surface imaging use in radiation oncology in the United States. J Appl Clin Med Phys. 2019;20(12):70–7.
Kost S, Shah CS, Xia P, Guo B. Setup time and positioning accuracy in breast radiation therapy using surface guided radiation therapy. Int J Radiat Oncol. 2018;102(3):e481–2.
Noh YY, Kim TH, Kang SH, Kim DS, Cho MS, Kim KH, Suh TS. Development of a room laser based real-time alignment monitoring system using an array of photodiodes. Phys Med. 2016;32(10):1284–91.
Fiorentino A, Ruggieri R, Giaj-Levra N, Sicignano G, Di Paola G, Naccarato S, Alongi F. Three-dimensional conformal versus intensity modulated radiotherapy in breast cancer treatment: is necessary a medical reversal? Radiol Med. 2017;122(2):146–53.
Kang SH, Chung JB, Kim KH, Kang SW, Eom KY, Song C, Kim JS. Comparison of dosimetrical and radiobiological parameters on three VMAT techniques for left-sided breast cancer. Prog Med Phys. 2019;30(1):7–13.
Kang S, Li J, Ma J, Zhang W, Liao X, Qing H, Orlandini LC. Evaluation of interfraction setup variations for postmastectomy radiation therapy using EPID-based in vivo dosimetry. J Appl Clin Med Phys. 2019;20(10):43–52.
Nguyen D, Farah J, Josserand-Pietri F, Barbet N, Khodri M. Benefits and challenges of standard ceiling-mounted surface guided radiotherapy systems for breast treatments on Halcyon™. Radioprotection. 2021;6:e235.
Flores-Martinez E, Cerviño LI, Pawlicki T, Kim GY. Assessment of the use of different imaging and delivery techniques for cranial treatments on the Halcyon linac. J Appl Clin Med Phys. 2020;21(1):53–61.
Hattel SH, Andersen PA, Wahlstedt IH, et al. Evaluation of setup and intrafraction motion for surface guided whole-breast cancer radiotherapy. J Appl Clin Med Phys. 2019;20(6):39–44.
Mancosu P, Fogliata A, Stravato A, Tomatis S, Cozzi L, Scorsetti M. Accuracy evaluation of the optical surface monitoring system on EDGE linear accelerator in a phantom study. Med Dosim. 2016;41(2):173–9.
Sá AC, Fermento A, Neves D, Ferreira S, Silva T, Coelho CM, Bonnarens E. Radiotherapy setup displacements in breast cancer patients: 3D surface imaging experience. Rep Pract Oncol Radiother. 2018;23(1):61–7.
Ma Z, Zhang W, Su Y, Liu P, Pan Y, Zhang G, Song Y. Optical surface management system for patient positioning in interfractional breast cancer radiotherapy. Biomed Res Int. 2018;2018:6415497.
Kost S, Guo B, Xia P, Shah C. Assessment of setup accuracy using anatomical landmarks for breast and chest wall irradiation with surface guided radiation therapy. Pract Radiat Oncol. 2019;9(4):239–47.
Batista V, Meyer J, Kügele M, Al-Hallaq H. Clinical paradigms and challenges in surface guided radiation therapy: where do we go from here? Radiother Oncol. 2020;153:34–42.
Laaksomaa M, et al. AlignRT® and Catalyst™ in whole‐breast radiotherapy with DIBH: Is IGRT still needed? J Appl Clin Med Phys. 2019;20(3):97–104.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grants funded by the Korea government (MSIT) (Nos. 2020R1C1C100936611 and 2020M2D9A1093990).
Author information
Authors and Affiliations
Contributions
JK and CHC supervised the project, had given valuable advices on the proceeding of this work, and designed the concept and the experiment method of the research. JHC, BSJ and KHS supported on data collection and the characterization of the sample. SK and HJ performed the experiment and data analysis. SK wrote the paper and prepared Figures and Tables. JK and CHC revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving a human participants was in accordance with the ethical standards of the institutional research committee. For this type of study, formal consent is not required.
Consent for publication
Not applicable.
Competing interests
S Kang, H Jin, JH Chang, BS Jang, KH Shin, CH Choi, J Kim declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kang, S., Jin, H., Chang, J.H. et al. Evaluation of initial patient setup methods for breast cancer between surface-guided radiation therapy and laser alignment based on skin marking in the Halcyon system. Radiat Oncol 18, 60 (2023). https://doi.org/10.1186/s13014-023-02250-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-023-02250-3