Abstract
Background
Dose-escalation to above 80 Gy during external beam radiotherapy for localised prostate cancer leads to improved oncological outcomes but also substantially increased rectal toxicity. The aim of this study was to demonstrate the safety and efficacy of escalating the dose to 82 Gy following insertion of a peri-rectal hydrogel spacer (HS) prior to radiotherapy.
Methods
This was a single arm, open-label, prospective study of men with localised prostate cancer who were prescribed a course of intensity modulated radiotherapy escalated to 82 Gy in 2 Gy fractions following insertion of the SpaceOAR™ HS (Boston Scientific, Marlborough, MA). Patients were prescribed a standard course of 78 Gy in 2 Gy fractions where rectal dose constraints could not be met for the 82 Gy plan. The co-primary endpoints were the rate of grade 3 gastrointestinal (GI) and genitourinary (GU) adverse events (CTCAE, v4), and patient-reported quality of life (QoL) (EORTC QLQ-C30 and PR25 modules), up to 37.5 months post-treatment.
Results
Seventy patients received treatment on the study, with 64 (91.4%) receiving an 82 Gy treatment course. The median follow-up time post-treatment was 37.4 months. The rate of radiotherapy-related grade 3 GI and GU adverse events was 0% and 2.9%, respectively. There were 2 (2.9%) grade 3 adverse events related to insertion of the HS. Only small and transient declines in QoL were observed; there was no clinically or statistically significant decline in QoL beyond 13.5 months and up to 37.5 months post-treatment, compared to baseline. No late RTOG-defined grade ≥ 2 GI toxicity was observed, with no GI toxicity observed in any patient at 37.5 months post-treatment. Nine (12.9%) patients met criteria for biochemical failure within the follow-up period.
Conclusions
Dose-escalation to 82 Gy, facilitated by use of a hydrogel spacer, is safe and feasible, with minimal toxicity up to 37.5 months post-treatment when compared to rates of rectal toxicity in previous dose-escalation trials up to 80 Gy. Trials with longer follow-up of oncological and functional outcomes are required to robustly demonstrate a sustained widening of the therapeutic window.
Trial registration Australian New Zealand Clinical Trials Registry, ACTRN12621000056897, 22/01/2021. Retrospectively registered.
Similar content being viewed by others
Background
Dose-escalated radiotherapy up to 78 Gy with conventional fractionation (1.8–2 Gy/fraction), and more recently, moderately hypofractionated radiotherapy (2.5–4 Gy/fraction) are the recommended forms of external beam radiotherapy (EBRT) for low to intermediate risk localised prostate cancer (PCa) [1]. Several randomised trials have demonstrated that dose-escalation reduces biochemical, local and distant failure compared to total doses less than 74 Gy [2,3,4]. Additional dose-escalation to 80 Gy and above can further reduce the rate of biochemical failure and distant metastases [5, 6] and may improve overall survival for men with high-risk disease [7].
Although improving oncological outcomes, dose-escalated EBRT also increases the rate of late gastrointestinal (GI) and genitourinary (GU) toxicity [2], even when intensity modulated radiotherapy (IMRT) is used [4]. A large randomised trial of EBRT for localised PCa found that rates of grade 2 or higher GI and GU toxicity were 12% and 21%, respectively for the dose-escalated 79.2 Gy arm, versus 7% and 15%, respectively, for the 70.2 Gy arm [4].
The rectum is the dose-limiting organ at risk during dose-escalated EBRT to the prostate [8]. To mitigate the increased risk of rectal toxicity, several methods of increasing the physical separation of the prostate and rectum have been investigated. These strategies include the implantation of a bio-degradable balloon [9] or injectable spacers composed of hyaluronic acid [10] or hydrogel [11, 12], which have been shown to reduce rectal dose [13, 14].
A recent systematic review and meta-analysis found a 66% reduction in the volume of the rectum receiving 70 Gy or more, a 77% reduction in the risk of late grade 2 or higher rectal toxicity and better long-term bowel-related quality of life (QoL) in men with peri-rectal hydrogel spacers implanted prior to dose-escalated prostate radiotherapy [15]. However, there is very limited evidence for the efficacy of peri-rectal hydrogel spacers when the dose is escalated above 80 Gy, with only one retrospective study presenting data following a treatment regimen of 81 Gy in 1.8 Gy fractions [16].
The primary aim of this trial was to evaluate adverse events and QoL up to three years following EBRT to the prostate when escalated to 82 Gy in 2 Gy fractions, following insertion of a hydrogel spacer to minimise rectal dose.
Methods
Setting and patients
This is a single centre, single arm, prospective phase II cohort study of dose-escalated IMRT for men with localised PCa following insertion of the SpaceOAR™ hydrogel spacer (HS) (Boston Scientific, Marlborough, MA). The study was approved by the Epworth HealthCare (611-13) and Monash Health (RES-19-0000-167E) human research ethics committees, respectively. All patients provided written informed consent.
Eligible patients were men with pathologically confirmed clinical stage T1 to T3 adenocarcinoma with no evidence of locoregional or distant metastatic disease. Clinical disease stage was determined via digital rectal examination and pre-biopsy magnetic resonance imaging (MRI). Neo-adjuvant or concurrent androgen deprivation therapy (ADT) was permitted at clinician discretion, with the duration of ADT being 6 months and 18 months for patients with intermediate-risk and high-risk disease, respectively. Patients receiving radiotherapy to the pelvic nodes, or who had active inflammatory bowel disease, an active bleeding disorder, or any other malignancy (either active or within 5 years prior to enrolment) except for non-melanoma skin cancer, were excluded from the study.
Procedures
A baseline computed tomography (CT) scan was performed prior to insertion of the HS. Patients were scanned in a supine position and were required to have a full bladder and empty bowel.
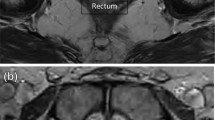
The insertion of the HS took place via a transperineal route under brief general anaesthesia and with antibiotic prophylaxis. The retro-prostatic space was hydro-dissected and 10 mL of the hydrogel was injected into the peri-rectal space under ultrasound guidance using a technique previously described [17]. Three gold-seed fiducials were also inserted into the prostate gland at the time of the HS insertion to facilitate image-guided radiotherapy, as per the standard of care for this cohort.
Planning CT and MRI scans were conducted a minimum of seven days following HS insertion. The prostate, seminal vesicles, HS and organs at risk were delineated following rigid registration of the CT and MRI datasets in the Eclipse™ (Varian Medical Systems, Palo Alto, CA) treatment planning system. High- (82 Gy) and low-dose (59 Gy) planning target volumes (PTV) were defined as 7 mm isotropic expansions of the prostate and seminal vesicles, respectively, except in the posterior direction where a 5 mm margin was applied. The extent of the rectal contour was 1 cm superior and inferior to the PTV.
A seven-field intensity modulated radiotherapy (IMRT) technique was used for treatment planning. Dose objectives for the prostate included mean dose ≥ 82 Gy (100%) and minimum dose ≥ 77.9 Gy (95% of the prescription dose). Dose constraints for the rectum were volume receiving 78 Gy (V78Gy) = 0%, V75Gy < 10%, V70Gy < 20%, V60Gy < 30%, V50Gy < 50% and V30Gy < 60%. Patients were prescribed and treated to 82 Gy unless dose objectives were not met and in that instance they were treated to 78 Gy.
An additional 78 Gy plan using the pre-insertion CT data was generated for each patient for the purpose of comparison to the 82 Gy post-insertion plan with the HS present. The same treatment planning technique was used for both the pre- and post-insertion plans.
Prior to the delivery of each daily fraction, target position and adequacy of bladder (full) and rectal (empty) preparation was verified using a combination of dual orthogonal 2D planar imaging (daily) or 3D volumetric imaging via cone beam CT (weekly at minimum). Image matching was performed based on the position of the three intra-prostatic gold seed fiducials.
Post-EBRT follow-up with clinical assessment, adverse event scoring, serum prostate-specific antigen (PSA) testing, and administration of patient-reported outcome questionnaires was scheduled for 6 weeks post-treatment, three-monthly for 18 months, then at six-month intervals until the final study visit at 37.5 months following the end of treatment.
Endpoints
Two primary endpoints were evaluated: (1) the incidence of grade 3 or higher GI and GU toxicity, defined by the Common Terminology Criteria for Adverse Events (v4.0), up to 37.5 months following radiotherapy, and (2) patient-reported changes in disease-specific QoL, measured by the European Organisation for Research and Treatment of Cancer (EORTC) Quality-of-life Questionnaire (QLQ) core (C30) [18] and prostate cancer (PR25) [19] modules. Secondary endpoints were the rate of local and biochemical control, respectively. Biochemical failure was defined as a PSA rise of ≥ 2 ng/mL from the post-EBRT nadir [20] or a rising PSA level and radiological evidence of disease progression.
In addition, radiotherapy-related GI toxicity was retrospectively graded according to Radiation Therapy Oncology Group (RTOG) acute and late toxicity criteria. To complement this, the proportion of post-insertion 82 Gy plans with a normal tissue complication probability (NTCP) for late grade ≥ 2 rectal toxicity or rectal bleeding equal to or lower than the corresponding pre-insertion 78 Gy plan was evaluated. NTCP calculation was performed using a previously validated tool [21] and based on the Lyman-Kutcher-Burman model using model parameters defined by QUANTEC [22].
Statistical analysis
Proportions are presented as percentages with Clopper-Pearson 95% confidence intervals (CI) [23]. Time to biochemical and local progression was analysed using Kaplan–Meier curves.
Baseline health-related QoL scores for selected QLQ-C30 (global quality of life, physical functioning, constipation, diarrhoea) and QLQ-PR25 (urinary function, bowel function) sub-scales were compared to 7.5-, 13.5-, 19.5-, 25.5-, 31.5- and 37.5-month follow-up time-points using linear regression allowing for clustering by time within patients, employing a robust estimator [24, 25]. The linear effect of time between baseline and 36 months post-treatment was analysed for each sub-scale.
In addition, the trajectory of QoL scores (mean and 95% CI) for each sub-scale was presented graphically at the six time-points from baseline up to 37.5 months post-treatment. Clinically important differences in QoL scores between baseline and each time-point were presented and assessed according to sub-scale specific thresholds for the QLQ-C30 [26]. A 10-point threshold was used for the QLQ-PR25 to determine clinically important changes in QoL from baseline, as has been used previously [27]. All statistical analyses were conducted using Stata version 17 (Stata Corporation, College Station, Texas, 2021). The QLQ-C30 was scored within Stata [28], the QLQ-PR25 was scored using R 4.1 (R Foundation for Statistical Computing, Vienna, Austria, 2021) [29]. A p value < 0.05 was considered statistically significant.
Results
Demographics
Seventy-one patients were enrolled into the study between November 2013 and September 2016. One patient withdrew from the trial prior to receiving treatment. Baseline characteristics for the cohort of 70 men receiving treatment are shown in Table 1. Sixty-four out of the 70 treated patients (91.4% [95% CI: 82.3–96.8%]) completed an 82 Gy treatment course. Six patients received a total dose of 78 Gy; rectal dose constraints could not be met for the 82 Gy plan for five patients and one patient who was prescribed 82 Gy had dose-limiting urinary toxicity and treatment was halted at 78 Gy. The median (25th to 75th percentile) length of follow-up for the cohort was 37.4 months (36.1–38 months).
Adverse events
No grade 3 or higher radiotherapy-related GI adverse events were observed. Two (2.9% [95% CI: 0.35–9.9%]) radiotherapy-related GU grade 3 adverse events were reported; one patient with urinary incontinence at 13.5 months and one patient who had a urinary tract obstruction at 4.5 months, however, the latter had undergone a transurethral resection of the prostate prior to radiotherapy.
Two patients (2.9% [95% CI: 0.35–9.9%]) manifested grade 3 adverse events attributable to the HS. One patient reported mild rectal discomfort approximately 3 weeks following HS insertion with pain increasing intermittently over the course of 4 months. MRI findings were unremarkable and symptoms resolved completely by 6 weeks following radiotherapy. One patient reported rectal pain, increasing following insertion of the HS, and was diagnosed with a rectal ulcer two weeks following radiotherapy. This was managed with a drainage catheter with full resolution of symptoms within 2 months.
QoL
There were no statistically significant changes in bowel related QoL up to 37.5 months following treatment. Constipation and diarrhoea symptom scores transiently exceeded the small clinically important difference threshold (5 and 3 points, respectively) at 13.5 and 7.5 months, respectively, with resolution of QoL scores by the next 6-monthly follow-up time-point for both sub-scales (Fig. 1). No clinically important declines in bowel related QoL beyond 13.5 months post-treatment were observed. Scores for the bowel symptom sub-scale of the QLQ-PR25 did not exceed the clinically important difference threshold within the follow-up period (Fig. 1F).
Quality of life trajectory up to 37.5 months following treatment measured by QLQ-C30 (A–D) and QLQ-PR25 (E and F) sub-scales. For the QLQ-C30, the blue and pink regions indicate a small and medium clinically important worsening of quality of life, respectively, as previously defined by Cocks et al. 2011 [26]. For the QLQ-PR25, pink regions indicate a minimum 10-point clinically important worsening of quality of life. Small and transient clinically important reductions in global health status (A) and physical functioning (B) were observed at 7.5 months post-treatment as well as small increases in constipation (C) and diarrhoea (D) symptom scores at 13.5 and 7.5 months, respectively. No clinically important changes from baseline were observed for overall urinary (E) or bowel (F) sub-scales
The mean Physical Functioning score for the cohort was significantly lower than baseline at 7.5 months post-treatment (− 5.1 [95% CI − 9.5 to − 0.8], p = 0.022) and 31.5 months (− 4.8 [95% CI − 7.9 to − 1.7], p = 0.003). However, only the 7.5-month score exceeded the five-point threshold for a small clinically important difference (Fig. 1B). There was a transient but statistically significant decline in Global Health Status score at 7.5 months (− 6.3 [95% CI − 12.0 to − 0.6], p = 0.032) which exceeded the threshold for a small clinically important difference of 4 points (Fig. 1A).
Observed and predicted rectal toxicity
Rates of acute and late RTOG-defined GI toxicity over the course of the follow-up period are shown in Fig. 2A. GI toxicity was most prevalent at 6 weeks post-treatment, with 15 (21.4% [12.5–32.9%]) and 3 (4.3% [0.9–12.0%]) patients manifesting grade 1 and 2 acute toxicity, respectively, which resolved almost universally across the cohort by 4.5 months post-treatment. Late grade 2 or higher GI toxicity was not observed, and no patient had any GI toxicity at the time of last follow-up.
Observed (A) and predicted (B) GI toxicity up to 37.5 months post-treatment. GI toxicity was most common at 6 weeks post-treatment but resolved almost completely by 4.5 months (A). No late grade ≥ 2 toxicity GI toxicity was observed. Sixty-five (95.6% [95% CI: 87.6–99.1%]) of sixty-eight evaluable patients had a reduction in rectal NTCP (late grade ≥ 2 toxicity or rectal bleeding) after insertion of the hydrogel spacer with a prescription dose of 82 Gy compared to a prescription of 78 Gy but with no HS (B). The median decrease in NTCP was 11.3%. (95% CI: 9.5–13.0%). The three patients with an increase in rectal NTCP (shown in red) had sub-optimal placement of the spacer at the time of insertion
The NTCP for corresponding pre-insertion 78 Gy and post-insertion 82 Gy plans are shown in Fig. 2B. The NTCP for late grade ≥ 2 rectal toxicity or rectal bleeding was lower for the post-insertion 82 Gy plan for 65 out of 68 (95.6% [95% CI: 87.6–99.1%]) evaluable patients. The increase in NTCP in three cases was attributable to sub-optimal placement of the HS. The median NTCP was 14.3% (95% CI: 12.6–17.2%) and 0.6% (95% CI: 0.3–1.3%), for the pre-insertion 78 Gy and post-insertion 82 Gy plans, respectively, with a median reduction in NTCP between corresponding plans of 11.3% (95% CI: 9.5–13.0%).
Biochemical and local progression
Nine (12.9% [95% CI: 6.1–23.0%]) and three (4.3% [95% CI: 0.9–12.0%]) patients met the criteria for biochemical and local progression, respectively, at three years following treatment (Fig. 3). Five of the nine patients who had progressed biochemically had International Society of Urological Pathology (ISUP) grade group ≥ 4 disease at baseline.
Discussion
To our knowledge, this is the first study to evaluate outcomes of prostate EBRT to an escalated dose of at least 82 Gy (2 Gy per fraction) following insertion of a peri-rectal HS. Principally, this study found that dose escalation to 82 Gy was safe, with minimal radiotherapy-related rectal toxicity and only small, transient increases in bowel-specific QoL symptom scores. Two (2.9%) grade 3 GU adverse events were reported and no late grade 2 or higher GI toxicities were observed. Dose-escalation to 82 Gy was feasible following HS insertion, with a high rate (95.6%) of reduction in rectal NTCP compared to a standard 78 Gy plan with no HS, and a high rate (91.4%) of patients being prescribed and subsequently completing the 82 Gy treatment course.
Previous studies using conventionally fractionated doses ≥ 80 Gy report relatively high rates of clinically significant acute and late GI toxicity in the absence of a rectal spacer. Petrongari et al. [30] (86 Gy in 2 Gy fractions, IMRT) report rates of grade 2 acute GI toxicity and late rectal bleeding of 44% and 18%, respectively, in addition to a 2.5% rate of late grade 3 and 4 GI toxicity. In the GETUG 06 phase III trial, the rate of late grade ≥ 2 GI toxicity in the arm receiving 80 Gy was 19.5% [2]. Even with dose-escalation to only 70–78 Gy, rates of late grade ≥ 2 GI toxicity are reported to be in the order of 5–20% [4, 31, 32], underscoring the efficacy of the HS observed in the current study where no late grade 2 GI toxicities were observed. These findings are consistent with the long-term results of a phase III trial (79.2 Gy in 1.8 Gy fractions, IMRT) which reported 0% versus 5.7% 3-year incidence of late grade ≥ 2 GI toxicity in the HS versus no-HS arms, respectively [33].
The use of a HS during dose-escalated prostate EBRT has previously been shown to result in long-term preservation of bowel-specific QoL. Hamstra et al. [33] reported that patients with a HS had better bowel QoL compared to patients without a HS 3 years following treatment (79.2 Gy in 1.8 Gy fractions, IMRT), with this difference being clinically meaningful. In a retrospective study, Pinkawa et al. [34] found that the group patients treated with a HS had a significantly lower rate of moderate to big problems with bowel urgency and had numerically smaller increases in bowel bother score up to 5 years following treatment (76 or 78 Gy in 2 Gy fractions, IMRT). The current study builds on these observations by demonstrating that preservation of long-term bowel QoL is possible when doses are escalated even further to 82 Gy, if a HS spacer is used.
Two spacer-related grade 3 adverse events were observed in this this study, the nature of which were consistent with previous safety reports for SpaceOAR™. Serious adverse events, including occurrences of rectal ulceration, perforation and fistula have been documented previously [35,36,37]. A recent trial of carbon ion versus proton therapy for prostate cancer reported that two (2.2%) of 92 patients who had a HS inserted were diagnosed with a grade 3 rectal fistula [38]. In addition the rate of low to moderate grade adverse events related to HS insertion has been reported to be up to 10% [15]. Given that the risk of significant HS-related toxicity is non-zero, the use of a HS should be considered in the context of the projected benefits to QoL and the treatment toxicity profile, for example, where dose-fractionation schemes with equivalent dose in 2 Gy fractions (EQD2) > 80 Gy are used. The potential benefit of a HS for a given patient also depends on individual patient anatomy [39] and clinical risk factors [40], which can be used on a prospective basis to select the patients most suitable for HS insertion prior to treatment.
The rationale for dose-escalation above EQD2 80 Gy is improved biochemical progression free survival, with benefits proportional to dose [5]. For patients with ISUP grade group ≥ 4 disease, dose-escalation to ≥ 80 Gy is also associated with lower risks of biochemical failure, distant metastases and overall survival [7]. In this study, the overall rate of 3-year biochemical failure (Phoenix definition) was 12.9%, and 16.7% in the sub-group of patients who had disease with ISUP grade group ≥ 4. While the length of follow-up in this study is limited, this rate of biochemical failure is likely to be consistent with the reports of other dose-escalation trials, including GETUG 06 which reported a 23.5% 5-year rate of biochemical failure in the 80 Gy arm [2]. Of note, the proportion of patients with ISUP grade group ≥ 4 (42.9%) and clinical stage T3 disease (30%) in this study was higher than the 80 Gy arm of GETUG 06 (6.5% and 13%, respectively). The observation that oncological outcomes following dose-escalation to 82 Gy are comparable with other contemporary dose-escalation trials, but rates of late GI toxicity substantially lower with the use of a HS, is suggestive of a clinically significant widening of the therapeutic ratio. Long-term studies (> 5 year) of dose-escalation above EQD2 80 Gy, whether via conventional or hypofractionated regimens, and with the use of a HS, are therefore warranted.
While this study was conducted in the twilight of the conventional fractionation era for PCa the findings are informative for the application of rectal spacers in the setting of hypofractionation. There has been a paradigm shift towards the use of moderately hypofractionated (2.5–4 Gy/fraction) or ultra-hypofractionated (> 4 Gy/fraction) regimens to reduce patient burden, capitalise on advances in both treatment planning and dose-delivery technologies and exploit the radiobiological characteristics of PCa. Trials of hypofractionated regimens report conflicting results regarding differences in late GI sequelae compared to conventional fractionation [41,42,43], with some studies reporting higher rates of late GI toxicity following hypofractionation [42, 43]. In the HYPRO trial, higher rates of patient-reported late rectal sequelae (including rectal bleeding, mucous discharge and faecal incontinence) were reported following hypofractionated treatment, with a post-hoc analysis finding a significant local dose–effect relationship between these late GI sequelae and regions of the rectal wall receiving intermediate to high doses [42]. This suggests that the application of a HS in the setting of hypofractionation could be highly effective for the minimisation of late GI toxicity. The use of a HS during prostate radiotherapy has also been shown to reduce intra-fraction prostate motion [44]. This could further reduce the risk of morbidity during the delivery of ultra-hypofractionated regimens, however, long-term clinical outcome data is still maturing [45].
The defined scope of this study was to assess safety and feasibility of dose escalation to 82 Gy with the use of a HS, and therefore the main limitations are a relatively short follow-up for oncological outcomes and the lack of a control arm to assess treatment efficacy. In addition, the rate of QoL completion was relatively poor. However, the objective endpoints of radiotherapy-related adverse events and RTOG-defined acute and late GI toxicity provide robust safety data.
Conclusions
This study demonstrates for the first time the feasibility and safety of escalating the dose to 82 Gy for intact prostate EBRT when a HS is used. Rates of radiotherapy-related adverse events and toxicity were minimal, with no late grade 2 GI toxicity reported during the 3-year follow-up period and no long-term detrimental impact on QoL. Future studies should prospectively assess whether long-term oncological and functional outcomes of dose-escalation to EQD2 > 80 Gy with use of a HS results in a sustainable widening of the therapeutic ratio for this cohort of patients particularly with the increasing deployment of moderately and ultra-hypofractionated schedules.
Availability of data and materials
Non-identifiable datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADT:
-
Androgen deprivation therapy
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- EBRT:
-
External beam radiation therapy
- EORTC:
-
European Organisation for Research and Treatment of Cancer
- EQD2:
-
Equivalent dose in 2 Gy fractions
- GI:
-
Gastro-intestinal
- GU:
-
Genitourinary
- HS:
-
Hydrogel spacer
- IMRT:
-
Intensity modulated radiation therapy
- ISUP:
-
International Society of Urological Pathology
- MRI:
-
Magnetic resonance imaging
- NTCP:
-
Normal tissue complication probability
- PCa:
-
Prostate cancer
- PSA:
-
Prostate-specific antigen
- PTV:
-
Planning target volume
- QoL:
-
Quality of life
- QLQ-C30:
-
Quality of life questionnaire core module
- QLQ-PR25:
-
Quality of life questionnaire prostate cancer module
- QUANTEC:
-
Quantitative Analyses of Normal Tissue Effects in the Clinic
- RTOG:
-
Radiation Therapy Oncology Group
- SD:
-
Standard deviation
- VXX Gy:
-
Proportion of structure receiving a minimum of XX Gy
References
Mottet N, van den Bergh RCN, Briers E, den Broeck TV, Cumberbatch MG, Santis MD, et al. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer—2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2021;79:243–62.
Beckendorf V, Guerif S, Le Prisé E, Cosset JM, Bougnoux A, Chauvet B, et al. 70 Gy versus 80 Gy in localized prostate cancer: 5-year results of GETUG 06 randomized trial. Int J Radiat Oncol. 2011;80:1056–63.
Kuban DA, Tucker SL, Dong L, Starkschall G, Huang EH, Cheung MR, et al. Long-term results of the M. D. Anderson randomized dose-escalation trial for prostate cancer. Int J Radiat Oncol Biol Phys. 2008;70:67–74.
Michalski JM, Moughan J, Purdy J, Bosch W, Bruner DW, Bahary JP, et al. Effect of standard vs dose-escalated radiation therapy for patients with intermediate-risk prostate cancer: the NRG Oncology RTOG 0126 randomized clinical trial. JAMA Oncol. 2018;4: e180039.
Eade TN, Hanlon AL, Horwitz EM, Buyyounouski MK, Hanks GE, Pollack A. What dose of external-beam radiation is high enough for prostate cancer? Int J Radiat Oncol Biol Phys. 2007;68:682–9.
Zelefsky MJ, Pei X, Chou JF, Schechter M, Kollmeier M, Cox B, et al. Dose escalation for prostate cancer radiotherapy: predictors of long-term biochemical tumor control and distant metastases-free survival outcomes. Eur Urol. 2011;60:1133–9.
Pahlajani N, Ruth KJ, Buyyounouski MK, Chen DYT, Horwitz EM, Hanks GE, et al. Radiotherapy doses of 80 Gy and higher are associated with lower mortality in men with Gleason score 8 to 10 prostate cancer. Int J Radiat Oncol Biol Phys. 2012;82:1949–56.
Pinkawa M. Spacer application for prostate cancer radiation therapy. Future Oncol. 2014;10:851–64.
Gez E, Cytron S, Ben Yosef R, London D, Corn BW, Alani S, et al. Application of an interstitial and biodegradable balloon system for prostate-rectum separation during prostate cancer radiotherapy: a prospective multi-center study. Radiat Oncol. 2013;8:96.
Prada PJ, Fernández J, Martinez AA, de la Rúa A, Gonzalez JM, Fernandez JM, et al. Transperineal injection of hyaluronic acid in anterior perirectal fat to decrease rectal toxicity from radiation delivered with intensity modulated brachytherapy or EBRT for prostate cancer patients. Int J Radiat Oncol Biol Phys. 2007;69:95–102.
Eckert F, Alloussi S, Paulsen F, Bamberg M, Zips D, Spillner P, et al. Prospective evaluation of a hydrogel spacer for rectal separation in dose-escalated intensity-modulated radiotherapy for clinically localized prostate cancer. BMC Cancer. 2013;22(13):27.
Uhl M, Herfarth K, Eble MJ, Pinkawa M, van Triest B, Kalisvaart R, et al. Absorbable hydrogel spacer use in men undergoing prostate cancer radiotherapy: 12 month toxicity and proctoscopy results of a prospective multicenter phase II trial. Radiat Oncol. 2014;9:96.
Mariados N, Sylvester J, Shah D, Karsh L, Hudes R, Beyer D, et al. Hydrogel spacer prospective multicenter randomized controlled pivotal trial: dosimetric and clinical effects of perirectal spacer application in men undergoing prostate image guided intensity modulated radiation therapy. Int J Radiat Oncol Biol Phys. 2015;92:971–7.
Melchert C, Gez E, Bohlen G, Scarzello G, Koziol I, Anscher M, et al. Interstitial biodegradable balloon for reduced rectal dose during prostate radiotherapy: results of a virtual planning investigation based on the pre- and post-implant imaging data of an international multicenter study. Radiother Oncol. 2013;106:210–4.
Miller LE, Efstathiou JA, Bhattacharyya SK, Payne HA, Woodward E, Pinkawa M. Association of the placement of a perirectal hydrogel spacer with the clinical outcomes of men receiving radiotherapy for prostate cancer: a systematic review and meta-analysis. JAMA Netw Open. 2020;3: e208221.
Te Velde BL, Westhuyzen J, Awad N, Wood M, Shakespeare TP. Late toxicities of prostate cancer radiotherapy with and without hydrogel SpaceAOR insertion. J Med Imaging Radiat Oncol. 2019;63:836–41.
Hatiboglu G, Pinkawa M, Vallée JP, Hadaschik B, Hohenfellner M. Application technique: placement of a prostate-rectum spacer in men undergoing prostate radiation therapy. BJU Int. 2012;110:E647-652.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
van Andel G, Bottomley A, Fosså SD, Efficace F, Coens C, Guerif S, et al. An international field study of the EORTC QLQ-PR25: a questionnaire for assessing the health-related quality of life of patients with prostate cancer. Eur J Cancer. 2008;44:2418–24.
Roach M, Hanks G, Thames H, Schellhammer P, Shipley WU, Sokol GH, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006;65:965–74.
Chang JH, Gehrke C, Prabhakar R, Gill S, Wada M, Joon DL, et al. RADBIOMOD: a simple program for utilising biological modelling in radiotherapy plan evaluation. Phys Med. 2016;32:248–54.
Michalski JM, Gay H, Jackson A, Tucker SL, Deasy JO. Radiation dose–volume effects in radiation-induced rectal injury. Int J Radiat Oncol Biol Phys. 2010;76(Suppl):123–9.
Armitage P, Berry G, Matthews JNS. Statistical methods in medical research. 4th ed. Oxford: Wiley-Blackwell; 2002.
Huber PJ. The behavior of maximum likelihood estimates under nonstandard conditions. Proc Fifth Berkeley Symp Math Stat Probab. 1967;5(1):221–34.
White H. Maximum likelihood estimation of misspecified models. Econometrica. 1982;50:1–25.
Cocks K, King MT, Velikova G, Martyn St-James M, Fayers PM, Brown JM. Evidence-based guidelines for determination of sample size and interpretation of the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. J Clin Oncol. 2011;29:89–96.
Duchesne GM, Woo HH, King M, Bowe SJ, Stockler MR, Ames A, et al. Health-related quality of life for immediate versus delayed androgen-deprivation therapy in patients with asymptomatic, non-curable prostate cancer (TROG 03.06 and VCOG PR 01–03 [TOAD]): a randomised, multicentre, non-blinded, phase 3 trial. Lancet Oncol. 2017;18:1192–201.
Bascoul-Mollevi C, Castan F, Azria D, Gourgou-Bourgade S. EORTC QLQ-C30 descriptive analysis with the qlqc30 command. Stata J. 2015;15:1060–74.
Anota A, Hamidou Z, Paget-Bailly S, Chibaudel B, Bascoul-Mollevi C, Auquier P, et al. Time to health-related quality of life score deterioration as a modality of longitudinal analysis for health-related quality of life studies in oncology: do we need RECIST for quality of life to achieve standardization? Qual Life Res. 2015;24:5–18.
Petrongari MG, Landoni V, Saracino B, Gomellini S, Arcangeli S, Iaccarino G, et al. Dose escalation using ultra-high dose IMRT in intermediate risk prostate cancer without androgen deprivation therapy: preliminary results of toxicity and biochemical control. J Exp Clin Cancer Res. 2013;32:103.
Aluwini S, Pos F, Schimmel E, Krol S, van der Toorn PP, de Jager H, et al. Hypofractionated versus conventionally fractionated radiotherapy for patients with prostate cancer (HYPRO): late toxicity results from a randomised, non-inferiority, phase 3 trial. Lancet Oncol. 2016;17:464–74.
Jolnerovski M, Salleron J, Beckendorf V, Peiffert D, Baumann AS, Bernier V, et al. Intensity-modulated radiation therapy from 70Gy to 80Gy in prostate cancer: six- year outcomes and predictors of late toxicity. Radiat Oncol. 2017;12:99.
Hamstra DA, Mariados N, Sylvester J, Shah D, Karsh L, Hudes R, et al. Continued benefit to rectal separation for prostate radiation therapy: final results of a phase III trial. Int J Radiat Oncol Biol Phys. 2017;97:976–85.
Pinkawa M, Berneking V, Schlenter M, Krenkel B, Eble MJ. Quality of life after radiation therapy for prostate cancer with a hydrogel spacer: 5-year results. Int J Radiat Oncol Biol Phys. 2017;99:374–7.
Klotz T, Mathers MJ, Lazar Y, Gagel B. Use of hydrogel as spacer in Denovier’s space: optimization of IMRT radiotherapy of localized prostate cancer. Urologe A. 2013;52:1690–7.
Teh AYM, Ko HT, Barr G, Woo HH. Rectal ulcer associated with SpaceOAR hydrogel insertion during prostate brachytherapy. BMJ Case Rep. 2014;1:2014206931.
Aminsharifi A, Kotamarti S, Silver D, Schulman A. Major complications and adverse events related to the injection of the SpaceOAR hydrogel system before radiotherapy for prostate cancer: review of the manufacturer and user facility device experience database. J Endourol. 2019;33:868–71.
Habl G, Uhl M, Katayama S, Kessel KA, Hatiboglu G, Hadaschik B, et al. Acute toxicity and quality of life in patients with prostate cancer treated with protons or carbon ions in a prospective randomized phase II study—the IPI trial. Int J Radiat Oncol. 2016;95:435–43.
van Wijk Y, Vanneste BGL, Walsh S, van der Meer S, Ramaekers B, van Elmpt W, et al. Development of a virtual spacer to support the decision for the placement of an implantable rectum spacer for prostate cancer radiotherapy: comparison of dose, toxicity and cost-effectiveness. Radiother Oncol. 2017;125:107–12.
Vanneste BGL, Hoffmann AL, van Lin EN, Van De Voorde L, Pinkawa M, Lambin P. Who will benefit most from hydrogel rectum spacer implantation in prostate cancer radiotherapy? a model-based approach for patient selection. Radiother Oncol. 2016;121:118–23.
Catton CN, Lukka H, Gu CS, Martin JM, Supiot S, Chung PWM, et al. Randomized trial of a hypofractionated radiation regimen for the treatment of localized prostate cancer. J Clin Oncol. 2017;35:1884–90.
Heemsbergen WD, Incrocci L, Pos FJ, Heijmen BJM, Witte MG. Local dose effects for late gastrointestinal toxicity after hypofractionated and conventionally fractionated modern radiotherapy for prostate cancer in the HYPRO trial. Front Oncol. 2020;10:469.
Lee WR, Dignam JJ, Amin MB, Bruner DW, Low D, Swanson GP, et al. Randomized phase III noninferiority study comparing two radiotherapy fractionation schedules in patients with low-risk prostate cancer. J Clin Oncol. 2016;34:2325–32.
Cuccia F, Mazzola R, Nicosia L, Figlia V, Giaj-Levra N, Ricchetti F, et al. Impact of hydrogel peri-rectal spacer insertion on prostate gland intra-fraction motion during 1.5 T MR-guided stereotactic body radiotherapy. Radiat Oncol. 2020;15:178.
Alongi F, Rigo M, Figlia V, Cuccia F, Giaj-Levra N, Nicosia L, et al. Rectal spacer hydrogel in 1.5T MR-guided and daily adapted SBRT for prostate cancer: dosimetric analysis and preliminary patient-reported outcomes. Br J Radiol. 2021;94:20200848.
Acknowledgements
This study was supported by funding from the Epworth Medical Foundation and E.J. Whitten Foundation. In-kind support was provided by the Icon Cancer Foundation.
Funding
This study was supported by funding from the E.J Whitten Foundation and the Epworth Medical Foundation. The funders did not play any role in study design, collection analysis or interpretation of data, or writing the manuscript.
Author information
Authors and Affiliations
Contributions
Study conception and design: AWS, PB. Data acquisition: AWS, PB, GW, SA, NL, PL, CP, YA, LS. Recruitment and management of patients: AWS, PB, GW, SA, NL, PL. Statistical analysis: DPM, LS. Writing of manuscript: AWS, LS. Review and final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Epworth HealthCare (611-13) and Monash Health (RES-19-0000-167E) human research ethics committees, respectively. All patients provided written informed consent prior to enrolment in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
See, A.W., Bowden, P., Wells, G. et al. Dose-escalated radiotherapy to 82 Gy for prostate cancer following insertion of a peri-rectal hydrogel spacer: 3-year outcomes from a phase II trial. Radiat Oncol 17, 131 (2022). https://doi.org/10.1186/s13014-022-02103-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-022-02103-5