Abstract
Background
This study aimed to investigate the effect of abdominal compression on tumour motion and target volume and to determine suitable planning target volume (PTV) margins for patients treated with lung stereotactic body radiotherapy (SBRT) based on four-dimensional computed tomography (4DCT).
Methods
Twenty-three patients diagnosed to have a peripheral pulmonary tumour were selected and divided into an all lesions group (group A), an upper middle lobe lesions group (group B), and a lower lobe lesions group (group C). Two 4DCT scans were performed in each patient, one with and one without abdominal compression. Cone beam computed tomography (CBCT) was performed before starting treatment. The gross target volumes (GTVs) were delineated and internal gross target volumes (IGTVs) were defined. IGTVs were generated using two methods: (1) the maximum intensity projections (MIPs) based on the 4DCT were reconstructed to form a single volume and defined as the IGTVMIP and (2) GTVs from all 10 phases were combined to form a single volume and defined as the IGTV10. A 5-mm, 4-mm, and 3-mm margin was added in all directions on the IGTVMIP and the volume was constructed as PTVMIP5mm, PTVMIP4mm, and PTVMIP3mm.
Results
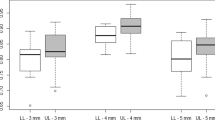
There was no significant difference in the amplitude of tumour motion in the left–right, anterior–posterior, or superior-inferior direction according to whether or not abdominal compression was applied (group A, p = 0.43, 0.27, and 0.29, respectively; group B, p = 0.46, 0.15, and 0.45; group C, p = 0.79, 0.86, and 0.37; Wilcoxon test). However, the median IGTVMIP without abdominal compression was 33.67% higher than that with compression (p = 0.00), and the median IGTV10 without compression was 16.08% higher than that with compression (p = 0.00). The median proportion of the degree of inclusion of the IGTVCBCT in PTVMIP5mm, PTVMIP4mm, and PTVMIP3mm ≥ 95% was 100%, 100%, and 83.33%, respectively.
Conclusions
Abdominal compression was useful for reducing the size of the IGTVMIP and IGTV10 and for decreasing the PTV margins based on 4DCT. In IGTVMIP with abdominal compression, adding a 4-mm margin to account for respiration is feasible in SBRT based on 4DCT.
Similar content being viewed by others
Background
Lung cancer has high incidence and mortality rates in both men and women worldwide [1,2,3], with a 5-year overall survival rate of 68.5–83% in patients with T1N0M0 disease and 53.8–65% in those with T2N0M0 disease [4]. Therefore, there is a good deal of clinical interest in improving early detection and treatment rates [5,6,7]. Surgical resection is the gold standard treatment for stage T1N0M0 and T2N0M0 non-small cell lung cancer. However, some of these patients have severe cardiovascular disease and poor lung function, and the National Comprehensive Cancer Network guidelines recommend stereotactic body radiotherapy (SBRT) as a standard treatment for those with good local control. SBRT is also suitable for patients with oligometastatic lung tumours [8,9,10,11,12].
Compared with conventional fractionated radiotherapy, SBRT can deliver higher radiation doses in fewer fractions focused on small targets with better local control and survival rates. Furthermore, it protects lung function and shortens the duration of radiotherapy [8, 11,12,13]. However, the ability of SBRT to provide precise radiotherapy is limited by positional uncertainty in that the position of the targets can be affected by several factors, one of which is respiratory motion [14, 15]. SBRT delivers high radiation doses in each fraction; therefore, technological advances are needed in both imaging and management of respiratory motion to reduce the target margin and limit the risk of complications caused by radiotherapy, especially when the tumour excursion is large [12]. In clinical practice, various manoeuvres can be used to manage motion, included active breath-hold, deep inhalation breath-holding (DIBH), tracking, and abdominal compression.
Active breath-hold is an effective way of reducing the necessary margin due to respiratory motion [16]. Using this procedure, the system is activated when the patient reaches the specified lung volume and stage of the breathing cycle, and the valve is inflated to hold the patient’s breath [14]. DIBH reduces motion in two ways, namely, by deep inspiration, which reduces lung density, and by breath-holding, which prevents movement of the tumour by immobilisation [17]. Patients require respiratory training before receiving this treatment; therefore, it is a hypothesis that poor control of motion using the active breath-hold and DIBH methods could be attributed to poor compliance and respiratory function. Tracking the motion of gold fiducial markers implanted near the tumour is an obvious way of evaluating tumour motion. Using this method, gold spheres or electromagnetic beacons with a diameter of 2 mm are implanted in or near the tumour. The position of each fiducial is tracked in three dimensions several times per second using an imaging system with automatic detection software. The linear accelerator delivers radiation when each fiducial is within an acceptable range of the desired simulation position [14]. However, implantation of fiducials is an invasive procedure for the patient, and assessment of the range of tumour motion is labour-intensive for the clinician [15]. In contrast, the abdominal compression technique requires no respiratory training or open surgery. It simply entails use of a compression plate/belt worn on the abdomen, which adjusts the pressure to a level that is comfortable for the patient and provides an easy-to-use method for complex SBRT setups. Although there have been many studies of the ability of abdominal compression to reduce tumour motion and decrease the target volume for upper abdominal tumours [18,19,20,21,22,23], several authors have mentioned that abdominal compression sometimes causes interfractional variations and marked respiratory motion.
The aim of this study was to investigate the ability of abdominal compression to reduce tumour motion and the target volume in patients treated with lung SBRT based on four-dimensional computed tomography (4DCT) and to determine the repeatability and conformability of target volumes during SBRT.
Methods
Patient characteristics
Twenty-three patients with 32 lesions who received SBRT between August 2018 and March 2020 were prospectively selected in the study if they had the following: a diagnosis of peripheral primary non-small cell lung cancer staged as T1N0M0; (b) a diagnosis of peripheral oligometastatic pulmonary disease that was controlled after initial systemic therapy and a lesion diameter of ≤ 4 cm; (c) an inoperable tumour that was strongly recommended for radiation therapy by a multidisciplinary team; (d) performance status 0–1 and able to breathe freely with abdominal compression; and no thoracic radiotherapy before treatment. Written informed consent was obtained in all cases. The patients were divided into an all lesions group (group A), an upper middle lobe lesions group (group B), and a lower lobe lesions group (group C). The patient and tumour characteristics are listed in Table 1.
CT simulation and image acquisition
During computed tomography (CT) simulation, all patients were immobilised using an abdominal compression system (Body Pro-Lok™; CIVCO Radiotherapy, Orange City, IA, USA) in the horizontal supine position. The respiratory plate places pressure at the level of the diaphragm to assist in restricting respiratory movement. The degree of pressure provided by the plate was as high as the patient could tolerate. Each patient underwent one helical three-dimensional CT (3DCT) and two 4DCT scanning sessions in a Big Bore simulated CT system (Philips Medical Systems, Bensalem, PA, USA). The 3DCT was performed with free-breathing. The first 4DCT was performed with abdominal compression and the second without abdominal compression when free-breathing was restored after removal of the respiratory plate. The patient was asked to breathe freely and rhythmically during both the 3DCT and 4DCT scanning procedures. During acquisition of the 4DCT data, the patient's abdominal surface was tracked using the Sentinel™ system (C-Rad, Uppsala, Sweden) and used as a surrogate for respiratory motion. The respiratory cycle was divided into 10 phases based on classical phase-binning, and reconstructed CT images were defined as CT0, CT10, CT20 through to CT90, where CT0 represents the dataset from end-inhalation and CT50 represents the dataset from end-exhalation during one respiratory cycle. The maximum intensity projection (MIP) was reconstructed from all 10 4DCT phases, referred to as MIPcom and MIPnon-com for images obtained with abdominal compression and free-breathing, respectively. All patients were treated using a linear accelerator (VitalBeam™, Varian Medical Systems, Palo Alto, CA, USA). Before treatment, cone beam CT (CBCT) of the chest was performed based on the position described earlier for the CT simulation. CT and CBCT images were acquired from the cricothyroid membrane to 5 mm beneath the diaphragm with a thickness of 3 mm. All images were transferred to the treatment planning system (MIM software version 6.7.6; MIM Software Inc., Cleveland, OH, USA).
Target definition
To eliminate interobserver variation, the target volumes were delineated on the CT images by the same physician using the MIM software. The gross target volumes (GTVs) were delineated on images from all phases of 4DCT with or without compression (GTV4DCTcom and GTV4DCTnon-com, respectively) in the same window width of 1600 HU with a window level of − 600 HU. [24] The GTVs delineated with and without abdominal compression are shown in Fig. 1. The internal gross target volume (IGTV) was generated using two methods: (1) MIPs based on the 4DCT were combined to form a single volume (IGTVMIP) and (2) GTVs from all 10 phases were combined to form a single volume (IGTV10).
Tumour motion and volume
The excursion of the GTVs was compared. The coordinates of the centre-of-mass of the target volume calculated using GTV4DCTcom and GTV4DCTnon-com were recorded to analyse the motion amplitudes of GTVs in different modes using the following formula:
where ΔX, ΔY, and ΔZ are defined as the movement in the left–right (LR), anterior–posterior (AP), and superior-inferior (SI) directions, respectively. The IGTVMIP and IGTV10 values with and without compression were compared.
Target consistency
The PTVMIP5mm, PTVMIP4mm, and PTVMIP3mm were created by addition of a 5-mm, 4-mm, and 3-mm margin, respectively, to the IGTVMIPcom in the LR, AP, and SI directions. The degree of inclusion (DI) between IGTVCBCT and PTVMIPcom was used to define the repeatability and conformability of PTVMIPcom relative to IGTVCBCT.
The formula used to calculate DI was as follows:
X ∩ Y is defined as the overlap between the IGTV and PTV values (MIM software, 6.7.6).
Assuming volume X to be the reference for the standard volume, if the treatment planning was based on volume Y, 1-DI (X in Y) of volume X would be irradiated unnecessarily and 1-DI (X in Y) of volume Y would miss irradiation [24]. And in this study, X = IGTVCBCT and Y = PTVMIPcom.
Statistical analysis
The target motion and volume data were not normally distributed. Therefore, the Wilcoxon test was used to compare the target motion and volume. The statistical analysis was performed using SPSS for Windows version 23.0 (IBM Corp., Armonk, NY, USA). A p value < 0.05 was considered statistically significant.
Results
Table 2 shows the GTV excursion at different sites in the lungs. When compared with non-compression, the median GTV excursion with compression increased by 6.67% in the LR direction but decreased by 6.45% in the AP direction and by 29.41% in the SI direction in group A, increased by 71.43% in the LR direction and reduced by 7.69% and 40.00% in the AP and SI directions, respectively, in group B, and did not change in the LR direction but increased by 5.56% in the AP direction and decreased by 54.69% in the SI direction in group C. There was no statistically significant between-group difference in GTV excursion according to whether or not compression was applied. The median 3D GTV motion with compression and non-compression was 3.15 mm (range 0.05–11.10) and 4.56 mm (range 0.41–12.92), respectively, in group A, 3.02 mm (range 0.05–7.38) and 2.92 mm (range 0.41–12.92), respectively, in group B, and 5.40 mm (range 2.12–11.10) and 6.65 mm (range 4.01–11.28), respectively, in group C; there was no significant difference between compression and non-compression in the three groups (Z = −1.16, − 1.17, − 0.65, respectively; p = 0.25, and 0.24, 0.52). In group B, comparing compression with non-compression, there was an obvious increase for 7 (35%), 6 (30%),8 (40%), and 7 (35%) of the 20 targets in the LR, AP, and SI directions and the 3D vector, respectively; a clear reduction for 11 (55%), 11 (55%), 10 (50%), and 12 (60%) of the 20 targets in the LR, AP, and SI directions and the 3D motion, respectively; and no change in the target motion amplitude of the 20 targets in the LR, AP, or SI direction or in the 3D motion for the 2 (10%), 3(15%), 2 (10%), and 1 (5%) remaining targets. In group C, comparing abdominal compression with non-compression, there was an obvious increase for 2 (17%), 5 (42%), 4 (33%), and 5 (42%) of the 12 targets in the LR, AP, and SI directions and in the 3D motion, respectively; an obvious reduction for 3 (25%), 4 (33%), 5 (42%), and 4 (33%) of the 12 targets in the LR, AP, and SI directions, and in the 3D motion, respectively; and no change in the target motion amplitude for the 7 (58%), 3 (25%), 3 (25%), and 3 (25%) remaining targets in the LR, AP, or SI direction or in the 3D motion.
The median IGTVMIPcom and IGTVMIPnon-com volumes in group A were 4.01 cm3 (range 0.39–34.84) and 5.36 cm3 (range 0.41–41.90), respectively; the difference was statistically significant (Z = −3.45, p = 0.00; Wilcoxon test). The median IGTV10com and IGTV10non-com volumes in group B were 6.59 cm3 (range 0.45–36.89) and 7.65 cm3 (range 0.43–46.46), respectively, and also significantly different (Z = −3.14, p = 0.00; Wilcoxon test).
When a 5-mm margin was added to the IGTVMIPcom to form the PTVMIPcom, the median DI of the IGTVCBCT in the PTVMIP5mm was 100%. When 4-mm and 3-mm margins were added, the median proportions of the DI in IGTVCBCT in PTVMIP4mm and PTVMIP3mm ≥ 95% were 100% and 83.33%, respectively.
Discussion
SBRT is a highly conformal and hypo-fractionated type of radiotherapy used to treat lung cancer with high‐dose radiation that can be focally administered and with exquisite dose fall-off [8, 25]. The main limiting factor for lung SBRT is respiration, which can lead to larger PTVs during treatment and an excessive risk of radiation‐induced complications. The tumour tissue and normal tissue treated with SBRT would receive different radiation doses under different breathing conditions [26]; therefore, management of respiratory movement could increase the benefit of radiotherapy for tumours in the lungs and other organs that are markedly affected by respiratory motion. Accurate measurement of tumour excursion is an essential component of management of respiratory movement in patients with lung tumours. In these patients, the effect of amplitude of respiratory movement depends on many factors, including the location of the tumour. Different measurement methods could also lead to different results. Therefore, there is considerable variation in the findings reported in the literature [27, 28]. Takao et al. [27] reported that the amplitude of baseline shift/drift of lung tumours in the craniocaudal direction was 1.65 mm using a real-time tumour-tracking radiation therapy system in 68 patients treated using SBRT with free-breathing. In a study that included 20 lesions, Negoro et al. [28] found that the average tumour excursion was 7.7 mm in the craniocaudal direction under free respiration using X-ray fluoroscopy simulation. In the present study, we calculated that the median excursion was 3.4 mm (2.5 mm for the upper middle lobe and 6.4 mm for the lower lobe) in the SI direction under free respiration using 4DCT.
Management of respiratory movement during lung SBRT aims to eliminate or minimise the target excursion caused by respiratory motion and to decrease the IGTV. Although abdominal compression has been considered to be an effective method for reducing respiratory movement, its effects on tumour excursion had not been consistent in the published reports [29,30,31,32]. Negoro et al. [28] reported that abdominal compression achieved a significant reduction in movement of tumours in the lower lobe from a range of 8–20 to 2–11 mm using fluoroscopic X-ray simulation. Bouihol et al. [29] found a reduction in tumour excursion in 82% of cases, with a reduction of 3.5 mm in the lower lobe and 0.8 mm in the upper middle lobe; however, case analysis indicated that the tumour excursion increased under abdominal compression in five cases using 4DCT. Mampuya et al. [30] reported that compression could reduce tumour excursion in the craniocaudal direction from 19.9 ± 7.3 to 12.4 ± 5.8 mm for tumours with excursion > 8 mm when measured using CBCT. Javadi et al. [31] reported tumour excursion of 6.1 mm with compression and 6.0 mm without compression in patients treated with lung SBRT, which suggested that abdominal compression could not reduce tumour excursion. Their finding is in accordance with that in a study by Rasheed et al. [32] who reported that tumour excursion was reduced in three patients, increased in five, and remained the same in nine. Overall, in that study, abdominal compression did not have any significant effect in reducing tumour excursion. The authors suggested that the effect of compression may be patient-specific and that the lobe in which the tumour was located did not predetermine the efficacy of compression. In our study, there was no statistically significant difference in the effect of compression on tumour excursion according to whether the tumour was in an upper middle lobe or a lower lobe. However, in numerical terms, the excursion in the SI direction decreased with abdominal compression regardless of tumour location, and this change in the tumour excursion pattern may explain the difference in IGTV.
Compared with non-compression, we found that abdominal compression could significantly reduce the IGTV, specifically, IGTVMIPcom < IGTVMIPnon-com (median reduction of 1.35 cm3) and IGTV10com < IGTV10non-com (median reduction of 1.06 cm3). Bouihol et al. [29] showed that abdominal compression could reduce the internal target volume (ITV) of tumours by approximately 1.3 cm3 for lung SBRT, which is consistent with our present findings. The reduction in IGTV (ITV) might reduce the incidence of radiation-induced lung injury [30]; therefore, abdominal compression may be beneficial for lung SBRT.
CBCT is an effective way of confirming the effect of respiratory management techniques on SBRT. At present, 4DCT and CBCT are widely used in SBRT for lung tumours. Calculating the DI of IGTVCBCTcom in PTVMIPcom could confirm the repeatability and consistency of the target during radiotherapy [33,34,35]. The American Association of Physicists in Medicine proposed differential margins for the PTV in all three dimensions during lung tumour SBRT [15]; undoubtedly, the excessive target volume increased the amount of unnecessary irradiation delivered to the surrounding normal lung tissue. [36] Therefore, lung tumour SBRT is usually expanded by 5 mm from the IGTV to construct the PTV. The results of our study indicate that an IGTVMIPcom with a 4-mm margin to account for respiration is reasonable for patients treated with SBRT under abdominal compression. Of course, the reduction in the PTV expansion boundary was based on positioning error and online position correction based on CBCT; therefore, automatic registration, positioning error correction, and manual registration based on soft tissue landmarks must be carried out before each CBCT-based treatment. If based only on bony automatic registration, abdominal compression is not recommended for lung SBRT because it can lead to uncorrected interfractional motion [29, 37], adversely affect local control of the tumour, and reduce patient survival [20].
We found that when patients with peripheral lung tumours were treated with SBRT, abdominal compression did not significantly change the tumour excursion in any of the three dimensions or the overall motion vector of the lung tumour and that the respiratory pattern changed in all lobe locations. Patients tend to breathe with the upper thoracic region when the lower region is immobilised; therefore, when abdominal breathing is suppressed, chest breathing is enhanced, which leads to changes in the excursion of tumours in different directions of the lung [29, 31]. Our results are more meaningful in terms of the efficacy of compression on target volumes. Abdominal compression reduced the IGTV, increased the DI of IGTVCBCTcom in PTVMIPcom, and reduced the PTV margins based on 4DCT.
The main limitation of this study was its small sample size, especially in the group of patients with tumours in the lower lobes, which led to smaller tumour excursions. Further studies with larger case numbers are needed to confirm our findings.
Conclusions
Use of abdominal compression did not decrease the motion of peripheral lung tumours in this study. When compared with non-compression, the GTV motion was not significantly decreased in any of the three directions measured or in the 3D vector regardless of the site of the tumour in the lung. While there was a change in the respiratory pattern with compression, it was related to the lung lobes in that the excursions increased in the LR direction and decreased in the AP and SI directions for the upper middle lobes but did not change in the LR direction, increased in the AP direction, and decreased in the SI direction for the lower lobes. A substantially smaller IGTV was seen for peripheral pulmonary tumours, and compression could increase the DI of IGTVCBCTcom in PTVMIPcom to minimise the external extension boundary of peripheral pulmonary tumours treated with SBRT based on 4DCT.
Availability of data and materials
All data generated or analyzed during this study are included in this published article. The authors in this article insure the availability of supporting data.
Abbreviations
- 4DCT:
-
Four-dimensional computed tomography
- AP:
-
Anterior–posterior
- CBCT:
-
Cone beam computed tomography
- DI:
-
Degree of inclusion
- DIBH:
-
Deep inhalation breath-holding
- GTV:
-
Gross target volume
- IGTV:
-
Internal gross target volume
- ITV:
-
The internal target volume
- LR:
-
Left–right
- MIP:
-
Maximum intensity projection
- PTV:
-
Planning target volume
- SBRT:
-
Stereotactic body radiotherapy
- SI:
-
Superior–inferior
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Torre LA, Siegel RL, Jemal A. Lung cancer statistics. Adv Exp Med Biol. 2016;893:1–19.
Hirsch FR, Scagliotti GV, Mulshine JL, Kwon R, Curran WJ, Wu YL, et al. Lung cancer: current therapies and new targeted treatments. Lancet. 2017;389:299–311.
Nesbitt JC, Putnam JB Jr, Walsh GL, Roth JA, Mountain CF. Survival in early-stage non-small cell lung cancer. Ann Thorac Surg. 1995;60:466–72.
Raghavan D, Wheeler M, Doege D, Doty JD 2nd, Levy H, Dungan KA, Davis LM, et al. Initial results from mobile low-dose computerized tomographic lung cancer screening unit: improved outcomes for underserved populations. Oncologist. 2020;25:e777–81.
Huang H, Luo W, Ni Y, Sun S, Wang C, Zhang L. The diagnostic efficiency of seven autoantibodies in lung cancer. Eur J Cancer Prev. 2020;29:315–20.
Ji P, Diederichs S, Wang W, Böing S, Metzger R, Schneider PM, et al. MALAT-1, a novel noncoding RNA, and thymosin beta4 predict metastasis and survival in early-stage non-small cell lung cancer. Oncogene. 2003;22:8031–41.
Ouyang W, Yu J, Nuerjiang S, Li Z, Wang D, Wang X, et al. Stereotactic body radiotherapy improves the survival of patients with oligometastatic non-small cell lung cancer. Cancer Med. 2019;8:4605–14.
Al-Shafa F, Arifin AJ, Rodrigues GB, Palma DA, Louie AV. A review of ongoing trials of stereotactic ablative radiotherapy for oligometastatic cancers: where will the evidence lead? Front Oncol. 2019;9:543.
Li H, Shen Y, Wu Y, Cai S, Zhu Y, Chen S, et al. Stereotactic body radiotherapy versus surgery for early-stage non-small-cell lung cancer. J Surg Res. 2019;243:346–53.
Shintani T, Matsuo Y, Iizuka Y, Mitsuyoshi T, Mizowaki T. A retrospective long-term follow-up study of stereotactic body radiation therapy for non-small cell lung cancer from a single institution: incidence of late local recurrence. Int J Radiat Oncol Biol Phys. 2018;100:1228–36.
Dunne EM, Fraser IM, Liu M. Stereotactic body radiation therapy for lung, spine and oligometastatic disease: current evidence and future directions. Ann Transl Med. 2018;6:283.
Whyte RI, Crownover R, Murphy MJ, Martin DP, Rice TW, DeCamp MM Jr, et al. Stereotactic radiosurgery for lung tumors: preliminary report of a phase I trial. Ann Thorac Surg. 2003;75:1097–101.
Benedict SH, Yenice KM, Followill D, Galvin JM, Hinson W, Kavanagh B. Stereotactic body radiation therapy: the report of AAPM Task Group 101. Med Phys. 2010;37:4078–101.
Keall PJ, Mageras GS, Balter JM, Emery RS, Forster KM, Jiang SB, et al. The management of respiratory motion in radiation oncology report of AAPM Task Group 76. Med Phys. 2006;33:3874–900.
Wong JW, Sharpe MB, Jaffray DA, Kini VR, Robertson JM, Stromberg JS, et al. The use of active breathing control (ABC) to reduce margin for breathing motion. Int J Radiat Oncol Biol Phys. 1999;44:911–9.
Rosenzweig KE, Hanley J, Mah D, Mageras G, Hunt M, Toner S, et al. The deep inspiration breath-hold technique in the treatment of inoperable non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2000;48:81–7.
Wunderink W, Méndez Romero A, de Kruijf W, de Boer H, Levendag P, Heijmen B. Reduction of respiratory liver tumor motion by abdominal compression in stereotactic body frame, analyzed by tracking fiducial markers implanted in liver. Int J Radiat Oncol Biol Phys. 2008;71:907–15.
West K, Russo M, Brown E, Barry T, Hargrave C, Pryor D. Evaluation of kidney motion with and without a pneumatic abdominal compression belt: considerations for stereotactic radiotherapy. J Med Imaging Radiat Oncol. 2018;62:128–32.
Mampuya WA, Matsuo Y, Ueki N, Nakamura M, Mukumoto N, Nakamura A, et al. The impact of abdominal compression on outcome in patients treated with stereotactic body radiotherapy for primary lung cancer. J Radiat Res. 2014;55:934–9.
Raphael JC, Varghese MK, Gopu PG, Venkatesan K, Jimson AD, Febin A. Effectiveness of abdominal compression in reducing internal target motion during conformal radiotherapy for carcinoma stomach—a pilot study. Indian J Cancer. 2018;55:226–9.
Lovelock DM, Zatcky J, Goodman K, Yamada Y. The effectiveness of a pneumatic compression belt in reducing respiratory motion of abdominal tumors in patients undergoing stereotactic body radiotherapy. Technol Cancer Res Treat. 2014;13:259–67.
Eccles CL, Patel R, Simeonov AK, Lockwood G, Haider M, Dawson LA. Comparison of liver tumor motion with and without abdominal compression using cine-magnetic resonance imaging. Int J Radiat Oncol Biol Phys. 2011;79:602–8.
Li FX, Li JB, Zhang YJ, Liu TH, Tian SY, Xu M, et al. Comparison of the planning target volume based on three-dimensional CT and four-dimensional CT images of non-small-cell lung cancer. Radiother Oncol. 2011;99:176–80.
Yorke ED, Kutcher GJ, Jackson A, Ling CC. Probability of radiation-induced complications in normal tissues with parallel architecture under conditions of uniform whole or partial organ irradiation. Radiother Oncol. 1993;26:226–37.
Lax I, Blomgren H, Näslund I, Svanström R. Stereotactic radiotherapy of malignancies in the abdomen. Methodol Asp Acta Oncol. 1994;33:677–83.
Takao S, Miyamoto N, Matsuura T, Onimaru R, Katoh N, Inoue T, et al. Intrafractional baseline shift or drift of lung tumor motion during gated radiation therapy with a real-time tumor-tracking system. Int J Radiat Oncol Biol Phys. 2016;94:172–80.
Negoro Y, Nagata Y, Aoki T, Mizowaki T, Araki N, Takayama K, et al. The effectiveness of an immobilization device in conformal radiotherapy for lung tumor: reduction of respiratory tumor movement and evaluation of the daily setup accuracy. Int J Radiat Oncol Biol Phys. 2001;50:889–98.
Bouilhol G, Ayadi M, Rit S, Thengumpallil S, Schaerer J, Vandemeulebroucke J, et al. Is abdominal compression useful in lung stereotactic body radiation therapy? A 4DCT and dosimetric lobe-dependent study. Phys Med. 2013;29:333–40.
Mampuya WA, Nakamura M, Matsuo Y, Ueki N, Iizuka Y, Fujimoto T, et al. Interfraction variation in lung tumor position with abdominal compression during stereotactic body radiotherapy. Med Phys. 2013;40:091718.
Javadi S, Eckstein J, Ulizio V, Palm R, Reddy K, Pearson D. Evaluation of the use of abdominal compression of the lung in stereotactic radiation therapy. Med Dosim. 2019;44:365–9.
Rasheed A, Jabbour SK, Rosenberg S, Patel A, Goyal S, Haffty BG, et al. Motion and volumetric change as demonstrated by 4DCT: the effects of abdominal compression on the GTV, lungs, and heart in lung cancer patients. Pract Radiat Oncol. 2016;6:352–9.
Paddick I. A simple scoring ratio to index the conformity of radiosurgical treatment plans. J Neurosurg. 2000;93(Suppl 3):219–22.
Feuvret L, Noël G, Mazeron JJ, Bey P. Conformity index: a review. Int J Radiat Oncol Biol Phys. 2006;64:333–42.
Yaparpalvi R, Garg MK, Shen J, Bodner WR, Mynampati DK, Gafar A, et al. Evaluating which plan quality metrics are appropriate for use in lung SBRT. Br J Radiol. 2018;91:20170393.
Wu VWC, Ng APL, Cheung EKW. Intrafractional motion management in external beam radiotherapy. J Xray Sci Technol. 2019;27:1071–86.
Han C, Sampath S, Schultheisss TE, Wong JYC. Variations of target volume definition and daily target volume localization in stereotactic body radiotherapy for early-stage non-small cell lung cancer patients under abdominal compression. Med Dosim. 2017;42:116–21.
Acknowledgements
Not applicable.
Funding
This research was supported in part by the Natural Science Foundation of China (NSFC) (81201735); The Key Research and Development Projects of Shandong Province (2015GSF118011); Taishan Scholars Program of Shandong Province (NO.ts 20190982).
Author information
Authors and Affiliations
Contributions
YJQ: Data curation, Manuscript writing. JBL: Research designing, Manuscript revising. YJZ Research designing, Manuscript revising. QS, XJL, FXL, JZW, ZXL, WW: Date collection. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The ethical approval was sought from institutional ethics committee prior to commencing this study. The ethical approval ID is SDTHEC201604003.
Consent for publication
All dates in this article approval for publication.
Competing interests
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qi, Y., Li, J., Zhang, Y. et al. Effect of abdominal compression on target movement and extension of the external boundary of peripheral lung tumours treated with stereotactic radiotherapy based on four-dimensional computed tomography. Radiat Oncol 16, 173 (2021). https://doi.org/10.1186/s13014-021-01889-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-021-01889-0