Abstract
Background
Radiomics is a new technology to noninvasively predict survival prognosis with quantitative features extracted from medical images. Most radiomics-based prognostic studies of non-small-cell lung cancer (NSCLC) patients have used mixed datasets of different subgroups. Therefore, we investigated the radiomics-based survival prediction of NSCLC patients by focusing on subgroups with identical characteristics.
Methods
A total of 304 NSCLC (Stages I–IV) patients treated with radiotherapy in our hospital were used. We extracted 107 radiomic features (i.e., 14 shape features, 18 first-order statistical features, and 75 texture features) from the gross tumor volume drawn on the free breathing planning computed tomography image. Three feature selection methods [i.e., test–retest and multiple segmentation (FS1), Pearson's correlation analysis (FS2), and a method that combined FS1 and FS2 (FS3)] were used to clarify how they affect survival prediction performance. Subgroup analysis for each histological subtype and each T stage applied the best selection method for the analysis of All data. We used a least absolute shrinkage and selection operator Cox regression model for all analyses and evaluated prognostic performance using the concordance-index (C-index) and the Kaplan–Meier method. For subgroup analysis, fivefold cross-validation was applied to ensure model reliability.
Results
In the analysis of All data, the C-index for the test dataset is 0.62 (FS1), 0.63 (FS2), and 0.62 (FS3). The subgroup analysis indicated that the prediction model based on specific histological subtypes and T stages had a higher C-index for the test dataset than that based on All data (All data, 0.64 vs. SCCall, 060; ADCall, 0.69; T1, 0.68; T2, 0.65; T3, 0.66; T4, 0.70). In addition, the prediction models unified for each T stage in histological subtype showed a different trend in the C-index for the test dataset between ADC-related and SCC-related models (ADCT1–ADCT4, 0.72–0.83; SCCT1–SCCT4, 0.58–0.71).
Conclusions
Our results showed that feature selection methods moderately affected the survival prediction performance. In addition, prediction models based on specific subgroups may improve the prediction performance. These results may prove useful for determining the optimal radiomics-based predication model.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Non-small-cell lung cancer (NSCLC) accounts for approximately 85% of lung cancers [1], which makes it the leading cause of cancer mortality worldwide [2]. Although treatment decisions and prognostic of lung cancer have significantly improved over the years, a parallel improvement in terms of global survival rate has lagged [3]. Currently, the tumor-node-metastasis (TNM) staging system is the most reliable prognostic factor for lung cancer [4]. However, survival rates may vary between patients included in the same disease stage [5]. Therefore, new prognostic approaches are urgently needed to achieve a personalized medical treatment to improve disease outcome [6]. Personalized cancer treatment is now largely based on medical imaging [7] because it offers the advantages of being noninvasive, reproducible, and relatively easy to implement in clinical practice [8]. Of particular interest is the work of Aerts et al. [9], who showed that features extracted from computed tomography (CT) may be useful for predicting the outcome of NSCLC patients.
Radiomics is a high-throughput technique to quantify phenotypic features in medical images [9, 10]. These features may help predict survival prognosis, preoperative distant metastasis, and histological subtype classification [9, 11, 12]. In recent years, there have been several reports showing high accuracy of radiomics in predicting histological classification of NSCLC. Liu et al. [13] established a multi-subtype classification model for the four major histological subtypes of NSCLC [i.e., squamous cell carcinoma (SCC), adenocarcinoma (ADC), large cell carcinoma (LCC), and not otherwise specified (NOS)] and investigated their classification performance and generalization ability. They showed an average classification accuracy of 0.89 on the training set and a classification accuracy of 0.86 on the test set. Zhu et al. [14] sought to distinguish SCC and ADC based on a radiomic signature. Their results showed an area under the curve (AUC) of 0.905 for the training cohort and an AUC of 0.893 for the validation cohort, which indicated good performance of the radiomic signature in distinguishing between ADC and SCC. These studies that classified the histological subtypes of NSCLC showed that texture features representing heterogeneity were essential in classifying each subtype. This is synonymous with the fact that each subtype has a different trend in radiomic features (especially texture features), i.e., the way the tumor looks in the CT image. In addition to differences in radiomic features, significant differences in prognosis have been reported for each histological subtype [15, 16]. Abel et al. showed that, compared to ADC, SCC was highly associated with local recurrence rates and was an independent negative predictor of overall survival [15]. Thus, histological subtypes vary widely in all aspects, including phenotype, heterogeneity, and prognosis.
Many radiomics-based prognostic studies of NSCLC patients have used machine learning with mixed datasets of various subgroups [17,18,19]. In contrast, few studies focused on subgroups for prognostic analysis. Chaddad et al. [20] performed a prognostic analysis in each NSCLC subgroup (i.e., histological subtypes, TNM stages, and clinical stages) and obtained an AUC of 0.757, 0.703, 0.703, and 0.762 for LCC, T2, N0, and Stage I groups, respectively. In the abovementioned study, there was minimum evaluation of the improvement in prediction performance by subgroup analysis because the analysis group was too limited. Yang et al. [21] developed and validated a radiomic method by integrating tumor and lymph node radiomics for the preoperative prediction of lymph node status in gastric cancer. They performed validation using subgroups in the test dataset and showed an improvement in prediction performance compared to the validation using the whole dataset. In the abovementioned study, there was minimal subgroup analysis because the training model itself used the whole dataset rather than subgroups.
As described above, there are only studies with minimum evaluation of subgroup analysis, even though the trends of radiomic features differ in each subgroup because of differences in phenotype and heterogeneity. We hypothesized that proper training and validation using the NSCLC subgroup dataset would lead to high improvement in prognostic performance because it would eliminate differences in trends of radiomic features. Therefore, this study investigated the radiomics-based survival prediction for subgroup datasets with specific histological subtypes and T stages of NSCLC patients.
Materials and methods
Patient population and image acquisition
The dataset in this study included a total of 384 patients treated with radiotherapy for NSCLC in our hospital from January 2010 to October 2017. A subset of this dataset was classified by radiation oncologists with respect to tumor (T), lymph node (N), and metastasis (M) and classified into four standard clinical stages. In addition, the histological subtype of each patient was identified (i.e., SCC, ADC, LCC, and NOS). Further, all patients were labeled in terms of “survival,” “death,” and survival time in days from scan to death or to the date of last visit (i.e., censored). GE Light Speed RT16 (GE Medical Systems, Waukesha, WI, USA) was used at the resolution of 512 × 512 × slices to acquire CT images under free breathing, with the number of slices varying between subjects. The in-plane pixel size of the images was 0.703–1.172 × 0.703–1.172 mm2, and the slice thickness was 2.5 mm. For each scan, the gross tumor volume (GTV) was manually delineated by a radiation oncologist. Table 1 shows the demographic information of each patient. The dataset used in this study includes multiple clinical stages and chemotherapy status. This was done to reduce the bias outside of specific subgroup to evaluate the prognostic performance of specific subgroups in the subgroup analysis described below. The following patients were excluded: patients without a histological subtype report (n = 27) and with a lack of GTV contours (n = 53). The data for the remaining 304 patients were divided into training and test datasets using stratified sampling at the ratio of 80% and 20%, respectively, while maintaining a constant ratio of deaths to surviving patients.
Overall scheme
Figure 1 shows the overall scheme of this study. First, we extracted a number of radiomic features from GTV segmentation for the whole dataset. Then, we divided the whole dataset into training and test datasets and applied three independent feature selection methods to the training dataset. Next, a least absolute shrinkage and selection operator (LASSO) Cox regression model was used to construct the model of radiomic features alone (radiomic model) and the model combining radiomic and clinical features (combined model). A test dataset was adapted to the constructed model, and the concordance-index (C-index) was used to evaluate the prognostic performance. Next, specific subgroup datasets were created from the whole dataset. In the subgroup analysis, a fivefold cross-validation was applied in model validation. The training dataset was subjected to the feature selection method that showed the best performance in the analysis for All data. As with the analysis for All data, LASSO Cox regression model was used to construct the radiomic and combined models, and the model performance was validated by applying the test dataset to the constructed model.
Feature extraction
PyRadiomics [22] on 3D Slicer was used to extract radiomic features from GTV, which was resampled to 1 × 1 × 1 mm3. A total of 107 features were extracted for each patient (Additional file 1: Supplementary A), which includes 14 shape features, 18 first-order statistical features, and 75 texture features. The shape feature quantified the diameter and volume of the region of interest (ROI) and the degree of irregularity. The first-order statistical feature was used to create a histogram of pixel values and define features with respect to that histogram. The texture feature served to convert the relationships between pixel values into matrix to measure image uniformity and heterogeneity. In addition, the texture feature included gray-level co-occurrence matrix (GLCM, n = 24), gray-level dependence matrix (GLDM, n = 14), gray-level run length matrix (GLRLM, n = 16), gray-level size zone matrix (GLSZM, n = 16), and neighborhood gray tone difference matrix (NGTDM, n = 5). For the GLCM feature, the bin width was set to 25 Hounsfield units. The radiomic features in PyRadiomics were based on the Image Biomarker Standardization Initiative, which established the validated definitions and benchmarks of the features, except for four features: shape_Maximum2DDiameterSlice, shape_Maximum2DDiameterColumn, shape_Maximum2DDiameterRow, and first-order_TotalEnergy [23].
Feature selection
The 107 radiomic features extracted from GTV were reduced using three independent feature selection methods. These three methods were applied to the training dataset in the whole dataset. This approach was used to determine the best feature selection methods in terms of prognostic performance. Then, the selection method that showed the best performance was used in the subgroup analysis.
Feature Selection 1 (FS1) selects only robust features using test–retest and multiple segmentation [9, 24]. The test–retest method uses a dataset created by Zhao et al. to evaluate the variability of tumor unidimensional, bidimensional, and volumetric measurements on same-day repeat CT scans [25]. This dataset can be downloaded from the publicly available online Reference Image Database to Evaluate Therapy Response (RIDER) test–retest dataset in the Cancer Imaging Archive (TCIA); this dataset consists of chest CT images of 32 patients that have been acquired twice at 15-min interval [26]. The test–retest method applies a radiomic analysis of tumors to two images of each patient and excludes features that significantly change over this short time as being less robust. The concordance correlation coefficient (CCC) served to evaluate the agreement between the values of two features, and feature selection was performed with CCC > 0.85 [24, 27, 28]. The multiple segmentation method uses a dataset created by van Baardwijk et al. to investigate whether auto-delineation reduces the interobserver variability compared to manual PET-CT–based GTV delineation [29]. This dataset can be downloaded from the publicly available online Quantitative Imaging Network multisite collection of lung CT data with nodule segmentations and RIDER data; this dataset consists of chest CT images of 20 patients that have been contoured by multiple physicians [26]. The multiple segmentation method uses a radiomic analysis of multiple ROIs of each patient and excludes features that vary significantly with small differences in contouring as being less robust. In addition, the intraclass correlation coefficient (ICC) served to evaluate the agreement between the values of multiple features, and feature selection was performed with ICC > 0.8 [24, 30]. In this study, we used 23 radiomic features selected in a previous study by Kadoya et al., who already performed test–retest and multiple segmentation using the abovementioned dataset and method [24].
Feature Selection 2 (FS2) excludes one of the correlated features from the analysis as redundant based on the correlation coefficients calculated by Pearson's correlation analysis for all features [21, 31]. An absolute value of the correlation coefficient of 0.8 or greater was the threshold to indicate strong correlation between two features [31, 32].
Feature Selection 3 (FS3) combines FS1 and FS2 [33, 34]. After robust features are selected using test–retest and multiple segmentation, non-redundant features are selected using Pearson's correlation analysis with a threshold of 0.8.
FS1, FS2, and FS3 are commonly used as feature selection methods for prognostic studies based on radiomics [9, 21, 33, 34]; therefore, we decided to adopt these feature selection methods in this study. MATLAB R2020a was used for all selection methods. Additional file 1: Supplementary B–D summarizes the robust and/or non-redundant features selected by FS1, FS2, and FS3, which were 23, 28, and 9, respectively.
Clinical predictors
As long as clinical predictors significantly affect prognosis [17, 21, 35], the most representative clinical predictors were added to the features used in this study. We used a total of eight clinical predictors, namely, gender, age, each TNM stage, clinical stage, histological subtype, and chemotherapy status [36,37,38].
Construction of the LASSO Cox regression model
Two different models were constructed: a model of radiomic features alone using the selected features in FS1, FS2, and FS3 (radiomic model) and a model combining radiomic and clinical features using the selected features plus clinical predictors (combined model). The LASSO Cox regression model was used to construct the model to predict survival prognosis. This regression model has often been used for radiomic analysis [18, 39].
Depending on λ, which is the weight of the constraint term on the likelihood function, the LASSO operation shrinks all regression coefficients toward zero and zeros the coefficients of irrelevant features. Learning models strongly depend on λ, such that large λ simplifies the model, whereas small λ reduces the role of weights and causes overfitting. We applied a fivefold cross-validation to prevent model simplification and overfitting and to select optimal λ for the data. In the fivefold cross-validation, to obtain model parameters, the dataset used for training was randomly divided into five parts, four of which were used as training data, and the remaining one was used as validation data. A model optimized for each λ for the training data was applied to the validation data, and the square error of residuals between the validation data and the model was computed. This treatment was repeated five times, and the five resulting square errors calculated for each λ were averaged to determine optimal λ for the smallest mean square error. Rad scores were calculated from linear combinations of features with nonzero coefficients at optimal λ. The rad score is represented by the sum of the nonzero coefficient features weighted by their respective coefficients (β), as shown in Eq. (1).
Statistical analysis
A Kaplan–Meier survival analysis served to evaluate the association between the rad score and survival. The median rad score calculated by Eq. (1) provided the threshold for dividing training dataset into high- and low-risk groups, and Kaplan–Meier curves were created for each risk group. Then, the log-rank test tested for significant differences between high- and low-risk groups. The C-index was used to evaluate the prognostic performance. The test dataset was applied to the rad score Eq. (1) and evaluated using Kaplan–Meier survival analysis and the C-index as well as the training dataset.
Statistical analysis was performed using the R software 3.6.1 (http://www.R-project.org), where the R packages “survival”, “glmnet”, and “survminer” used the LASSO Cox regression model. Statistical significance was set at P < 0.05.
Subgroup analysis
The whole dataset containing 304 NSCLC patients was classified into histological subtypes and T stages to create the subgroup datasets. The histological subtypes SCC, ADC, LCC, and NOS contained 149, 135, 7, and 13 patients, respectively. However, the LCC and NOS subtypes were excluded from the analysis because they contained too few data to analyze. The T stages T0–T4 and TX contained 1, 93, 96, 49, 55, and 10 patients, respectively. Again, T0 and TX stages were excluded from the analysis group because of too few data. For further analysis by datasets with identical characteristics, the SCC and ADC subtypes were classified into T stages T1–T4. Altogether, a total of 14 groups were included in the subgroup analysis. The SCC and ADC subtypes that contained all T stages were denoted SCCall and ADCall, respectively, and those were further classified into T stages T1–T4 and denoted SCCT1, SCCT2, SCCT3, SCCT4, ADCT1, ADCT2, ADCT3, and ADCT4, respectively. Additional file 1: Supplementary E lists the patient characteristics for each subgroup.
As shown in Fig. 1, a fivefold cross-validation was used to validate the constructed model in subgroup analysis. Each subgroup dataset was divided into five parts using stratified sampling, while maintaining a constant ratio of deaths to surviving patients; then, four parts were set as the training dataset and one part as the test dataset. Fivefold cross-validation was used to ensure reliability of the model constructed with subgroup datasets with a small number of data. In addition, cross-validation may remove redundancy in the constructed model because, unlike the bootstrap method, it divides the dataset without allowing duplication. The C-indexes of both the radiomic and combined models in the analysis for All data were averaged for each feature selection method, and the method that produced the highest C-index was applied to the training dataset. Similar to the analysis for All data, the LASSO Cox regression model was used to construct radiomic models and combined models, and the test dataset was applied to each model. The Kaplan–Meier survival analysis and C-index were used to evaluate prognostic performance of the constructed model. The C-index used in the evaluation is the average of C-indexes of the five models constructed by the fivefold cross-validation. To compare the results of the whole dataset and the subgroup dataset under the same conditions, the same validation method as for the subgroup analysis was applied to All data.
To increase the reliability of this study, we applied the same subgroup analysis to a publicly available dataset (Lung 1, NSCLC-Radiomics) on TCIA [26]. Supplemental M indicates patient characteristics for this dataset. Other detailed information can be found in the paper by Aerts et al. [9]. Similar to the process applied to our dataset, after extracting 107 radiomic features from GTV of each patient in the Lung 1 dataset, Pearson's correlation analysis was applied to the training dataset as feature selection. We constructed radiomic models using only selected radiomic features. We also constructed combined models by adding clinical features to the radiomic model. However, because the Lung 1 dataset did not contain information on the chemotherapy status, a total of seven clinical features were included, excluding the chemotherapy status. The analysis was limited to three groups, including All data (n = 287), SCCall (n = 82), and ADCall (n = 27), owing to the number of data in each subgroup dataset. We applied exactly the same methods of learning and evaluation as described above.
Results
Table 2 shows the prognosis prediction performance when robust and/or non-redundant features are used in the analysis for All data. FS2 had the highest C-index of all selection methods in the training and test datasets for the radiomic model (0.64 and 0.61, respectively). Similarly, FS2 had the highest C-index of all selection methods in the training and test datasets for the combined model (0.65 and 0.63, respectively). Therefore, FS2 with Pearson's correlation analysis was applied for subgroup analysis.
Table 3 shows the prognostic performance for each subgroup, and Additional file 1: Supplementary F–G show the prognostic performance of radiomic and combined models in each subgroup with fivefold cross-validation. In addition, Additional file 1: Supplementary I–J show Kaplan–Meier curves when divided into low- and high-risk groups based on the rad score in the radiomic and combined models for each subgroup. To avoid complications, the case when it was closest to the mean C-index of the test dataset among the fivefold cross-validation is shown. In the analysis of histological subtypes and T stages, both the radiomic and combined models produced higher C-indexes than did All data for all subgroups (except for the SCCall group). In particular, the C-index of the test dataset in the radiomic model improved the most for the T1 group (0.62 ± 0.03 for All data vs. 0.66 ± 0.04 for the T1 group), and that in the combined model improved the most for the T4 group (0.64 ± 0.04 for All data vs. 0.70 ± 0.06 for the T4 group). Kaplan–Meier curves representing the relationship between the rad score and survival time also showed that patients in ADCall and each T stage were significantly stratified between high and low rad score values compared to All data. The analysis of each T stage in the histological subtypes had different trends in the SCC and ADC groups. In the analysis of each T stage in the ADC group, both the radiomic and combined models produced higher C-indexes than the ADCall group for all groups. In particular, the C-index of the test dataset in the radiomic model increased the most for the ADCT3 group (0.64 ± 0.02 for the ADCall group vs. 0.81 ± 0.03 for the ADCT3 group), and that in the combined model increased the most for the ADCT1 group (0.69 ± 0.04 for the ADCall group vs. 0.83 ± 0.04 for the ADCT1 group). Conversely, in the analysis of each T stage in the SCC group, both the radiomic and combined models produced considerably lower C-indexes in the test dataset of the SCCT1, SCCT2, and SCCT3 groups than of the SCCall group. In addition, all T stage groups in SCC failed to stratify high and low rad score values in the Kaplan–Meier curves. In the analysis of all subgroups, the combined model showed a slightly or moderately higher C-index than did the radiomic model (Table 3).
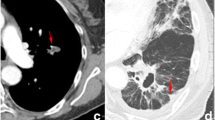
Figure 2 shows representative cases to illustrate the difference in heterogeneity between ADC and SCC. As an example, we show CT images of GTV in two cases selected from the low- and high-risk groups of the ADCT1 and SCCT1 test datasets that showed the closest values to the mean C-index among the fivefold cross-validation. The abovementioned image shows the largest ROI slice in GTV. For the low-risk groups, survival time for the two cases was 2606 and 1978 days in the SCCT1 group and 2623 and 1667 days in the ADCT1 group. For the high-risk group, survival time was 193 and 86 days in the SCCT1 group and 142 and 74 days in the ADCT1 group. We also show the value of the rad score in the combined model for each subgroup. In both the SCCT1 and ADCT1 groups, the rad score equation includes the texture feature regarding uniformity. The abovementioned images show that, in the ADCT1 group, homogeneity is constant in the low-risk groups, whereas homogeneity is sparse in the high-risk groups. The rad score value is also below the median (3.98) in the low-risk groups and above the median in the high-risk groups. Conversely, in the SCCT1 group, the rad score value is below the median (0.17), despite the heterogeneity observed in the images in the high-risk group, which indicates a discrepancy between the images and radiomic features.
Similar results were observed in the subgroup analysis using the Lung 1 dataset (Additional file 1: Supplementary N–P). Compared to All data, the test datasets of both the radiomic and combined models produced a higher C-index for the ADCall group and a lower C-index for the SCCall group (Additional file 1: Supplementary N). The Kaplan–Meier curves, which show the case that was closest to the mean C-index of the test dataset among the fivefold cross-validation, showed that the ADCall group was significantly stratified between high and low rad score values, whereas the SCCall group was not (Additional file 1: Supplementary O). In addition, all three subgroups showed higher prognostic performance in the combined model than in the radiomic model.
Discussion
Prognostic analysis of NSCLC patients using radiomics used mixed data with various subgroups [17,18,19]. In this study, we investigated the radiomics-based survival prediction for subgroup datasets with specific histological subtypes and T stages of NSCLC patients. The analysis of All data did not indicate high prognostic performance. However, the analysis of subgroups indicated better prognostic performance than did the analysis of All data. In particular, the analysis of each T stage in the ADC group produced a significant improvement in prognostic performance. This result suggests that the analysis of the NSCLC dataset by specific histological subtypes and T stages may significantly improve survival prediction.
This study applied three independent feature selection methods to All data to determine the best method in terms of prognostic performance. In the test dataset for both the radiomic and combined models, the highest prognostic performance is obtained when using FS2. Sun et al. [40] showed that Pearson's feature selection method (i.e., similar to FS2 in our method) in the Cox model produced the second highest C-index among the five selection methods. In addition, Leger et al. [41] also showed that the same Pearson's feature selection method in the Cox model produced the highest C-index among the 12 selection methods. These results are consistent with our result (i.e., FS2 had the highest C-index). Because the Cox model directly predicts the time to event with a simple regression equation, this model often produced overfitting [41]. Pearson's feature selection method is one of the filter-based methods, which can minimize overfitting by removing redundant feature interactions with high computational efficiency [42]. On the basis of these characteristics of the Cox model and Pearson's feature selection method, it can be explained that this selection method was the most useful method for prognosis prediction with the Cox model.
Previous studies, which validated the prediction performance by applying each subgroup dataset to the model trained with the whole dataset, have shown an improvement in prediction performance compared to applying the whole dataset [21, 43]. However, these studies have not constructed training models using subgroup datasets and performed only minimal subgroup analysis. Our study is the first study to construct both All data and subgroup models to perform prognostic analysis of NSCLC patients. The obtained results showed an improvement in prognostic performance in many subgroups (except for the SCCall, SCCT1, SCCT2, and SCCT3 groups) compared to All data. In particular, the best prognostic performance was achieved in the ADCT1 and ADCT3 groups (0.83 ± 0.04 and 0.81 ± 0.02, respectively). These are based on our hypothesis that high prognostic performance is produced by eliminating differences in trends of radiomic features among subgroups with different prognosis and heterogeneity. Therefore, the approach used in this study, in which the training model was constructed for each subgroup, may accurately reflect the characteristics of each group as a radiomic feature and may improve the performance of prognostic predictions.
Compared to that in All data, there was an improvement in prognostic performance in the ADC-related group, but there was a decrease in prognostic performance in some SCC-related groups. Two reasons may explain the degraded prognostic performance from the SCC-related groups. First, ADC occurs at a different site than does SCC. In general, ADC most commonly occurs at the peripheral of lung parenchyma. Conversely, SCC consists of mostly hilar-type lung cancers near the hilar area. In fact, the data used herein indicated that tumors occurred in the pulmonary hilar area in 22% of the SCC group, but in 8% of the ADC group. If a tumor is adjacent to the hilar area (i.e., contacts the main bronchus near the bronchial area), its boundaries may be difficult to determine when contouring. Second, there is a difference in the heterogeneity of ADC and SCC. Many studies have already reported that the heterogeneity difference between ADC and SCC is accurately represented as radiomic features [13, 14, 44]. However, this heterogeneity difference by histological subtype may have a significant impact on prognostic prediction. In other words, in the ADC-related group, the radiomic features may properly reflect tumor heterogeneity on the images, whereas in the SCC-related group, they do not, and may not have a clear difference in the heterogeneity separating the low- and high-risk groups.
Some studies have shown the potential clinical utility of the prognostic models based on radiomics analysis [9, 45]. This study aimed to achieve sufficient prognostic performance for clinical utility using an approach that focused on the prognostic analysis in subgroups with identical characteristics. Our results show relatively high prognostic performance in ADC-related subgroup datasets, which may bring us closer to potential clinical applications. However, there is a problem that must be addressed before future clinical applications are possible, i.e., the advent of therapies using immune checkpoint inhibitors and molecular targeted drugs. These therapies have considerably improved the prognosis of lung cancer patients [46]; thus, it is necessary to develop a prognostic model that accounts for these factors. Recently, high association with radiomics and potential for high prognosis prediction has been reported in a dataset of patients treated with these therapies [47,48,49]. A future challenge is to reveal whether the model can be adapted to data from patients who have been treated with the abovementioned treatments.
Finally, this study has several limitations. First, it considers the type of subgroups analyzed. Although excluded from this analysis owing to the considerable variation in the number of data between groups, the prognostic performance can be improved by unifying clinical stages that treatments and heterogeneity greatly varied between groups. Second, this study is based on a relatively small number of patients. Because the number of data for some subgroups is quite small, the results obtained herein require further validation using a study based on more data. Third, it considers the issue of contouring. Manual segmentation with a single oncologist was used in this study. Previous studies have reported that semi-automatic segmentation was useful owing to high reproducibility and reliability, although this method may have software dependence [50, 51].
Conclusions
This study investigated the radiomics-based survival prediction for subgroup datasets with specific histological subtypes and T stages of NSCLC patients. Our results showed that the models based on ADC-related groups and each T stage group had a higher C-index than had the models based on All data. Therefore, the prognostic analysis of specific subgroups can be expected to significantly improve the performance of prognostics.
Availability of data and materials
There is no availability of these data, which were used under license for the current study and so are not publicly available.
Abbreviations
- NSCLC:
-
Non-small-cell lung cancer
- TNM:
-
Tumor-node-metastasis
- CT:
-
Computed tomography
- SCC:
-
Squamous cell carcinoma
- ADC:
-
Adenocarcinoma
- LCC:
-
Large cell carcinoma
- NOS:
-
Not otherwise specified
- AUC:
-
Area under the curve
- T:
-
Tumor
- N:
-
Lymph node
- M:
-
Metastasis
- GTV:
-
Gross tumor volume
- LASSO:
-
Least absolute shrinkage and selection operator
- C-index:
-
Concordance-index
- ROI:
-
Region of interest
- GLCM:
-
Gray-level co-occurrence matrix
- GLDM:
-
Gray-level dependence matrix
- GLRLM:
-
Gray-level run length matrix
- GLSZM:
-
Gray-level size zone matrix
- NGTDM:
-
Neighborhood gray tone difference matrix
- FS:
-
Feature selection
- TCIA:
-
The Cancer Imaging Archive
- RIDER:
-
Reference Image Database to Evaluate Therapy Response
- CCC:
-
Concordance correlation coefficient
- ICC:
-
Intraclass correlation coefficient
- ML:
-
Machine learning
References
Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc. 2008;83(5):584–94.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359-386.
Liang W, Zhang L, Jiang G, Wang Q, Liu L, Liu D, Wang Z, Zhu Z, Deng Q, Xiong X, et al. Development and validation of a nomogram for predicting survival in patients with resected non-small-cell lung cancer. J Clin Oncol. 2015;33(8):861–9.
Rami-Porta R, Asamura H, Goldstraw P. Predicting the prognosis of lung cancer: the evolution of tumor, node and metastasis in the molecular age-challenges and opportunities. Transl Lung Cancer Res. 2015;4(4):415–23.
Lambin P, Zindler J, Vanneste BG, De Voorde LV, Eekers D, Compter I, Panth KM, Peerlings J, Larue RT, Deist TM, et al. Decision support systems for personalized and participative radiation oncology. Adv Drug Deliv Rev. 2017;109:131–53.
Lambin P, van Stiphout RG, Starmans MH, Rios-Velazquez E, Nalbantov G, Aerts HJ, Roelofs E, van Elmpt W, Boutros PC, Granone P, et al. Predicting outcomes in radiation oncology–multifactorial decision support systems. Nat Rev Clin Oncol. 2013;10(1):27–40.
Morin O, Vallieres M, Jochems A, Woodruff HC, Valdes G, Braunstein SE, Wildberger JE, Villanueva-Meyer JE, Kearney V, Yom SS, et al. A deep look into the future of quantitative imaging in oncology: a statement of working principles and proposal for change. Int J Radiat Oncol Biol Phys. 2018;102(4):1074–82.
Aerts HJ, Velazquez ER, Leijenaar RT, Parmar C, Grossmann P, Carvalho S, Bussink J, Monshouwer R, Haibe-Kains B, Rietveld D, et al. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun. 2014;5:4006.
Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data. Radiology. 2016;278(2):563–77.
Huynh E, Coroller TP, Narayan V, Agrawal V, Hou Y, Romano J, Franco I, Mak RH, Aerts HJ. CT-based radiomic analysis of stereotactic body radiation therapy patients with lung cancer. Radiother Oncol. 2016;120(2):258–66.
Wu W, Parmar C, Grossmann P, Quackenbush J, Lambin P, Bussink J, Mak R, Aerts HJ. Exploratory study to identify radiomics classifiers for lung cancer histology. Front Oncol. 2016;6:71.
Liu J, Cui J, Liu F, Yuan Y, Guo F, Zhang G. Multi-subtype classification model for non-small cell lung cancer based on radiomics: SLS model. Med Phys. 2019;46(7):3091–100.
Zhu X, Dong D, Chen Z, Fang M, Zhang L, Song J, Yu D, Zang Y, Liu Z, Shi J, et al. Radiomic signature as a diagnostic factor for histologic subtype classification of non-small cell lung cancer. Eur Radiol. 2018;28(7):2772–8.
Abel S, Hasan S, White R, Schumacher L, Finley G, Colonias A, Wegner RE. Stereotactic ablative radiotherapy (SABR) in early stage non-small cell lung cancer: comparing survival outcomes in adenocarcinoma and squamous cell carcinoma. Lung Cancer (Amsterdam, Netherlands). 2019;128:127–33.
Fukui T, Taniguchi T, Kawaguchi K, Fukumoto K, Nakamura S, Sakao Y, Yokoi K. Comparisons of the clinicopathological features and survival outcomes between lung cancer patients with adenocarcinoma and squamous cell carcinoma. Gen Thorac Cardiovasc Surg. 2015;63(9):507–13.
Yang L, Yang J, Zhou X, Huang L, Zhao W, Wang T, Zhuang J, Tian J. Development of a radiomics nomogram based on the 2D and 3D CT features to predict the survival of non-small cell lung cancer patients. Eur Radiol. 2019;29(5):2196–206.
Soufi M, Arimura H, Nagami N. Identification of optimal mother wavelets in survival prediction of lung cancer patients using wavelet decomposition-based radiomic features. Med Phys. 2018;45(11):5116–28.
Bortolotto C, Lancia A, Stelitano C, Montesano M, Merizzoli E, Agustoni F, Stella G, Preda L, Filippi AR. Radiomics features as predictive and prognostic biomarkers in NSCLC. Expert Rev Anticancer Ther. 2021;21(3):257–66.
Chaddad A, Desrosiers C, Toews M, Abdulkarim B. Predicting survival time of lung cancer patients using radiomic analysis. Oncotarget. 2017;8(61):104393–407.
Yang J, Wu Q, Xu L, Wang Z, Su K, Liu R, Yen EA, Liu S, Qin J, Rong Y, et al. Integrating tumor and nodal radiomics to predict lymph node metastasis in gastric cancer. Radiother Oncol. 2020;150:89–96.
van Griethuysen JJM, Fedorov A, Parmar C, Hosny A, Aucoin N, Narayan V, Beets-Tan RGH, Fillion-Robin JC, Pieper S, Aerts H. Computational radiomics system to decode the radiographic phenotype. Cancer Res. 2017;77(21):e104–7.
Zwanenburg A, Vallières M, Abdalah MA, Aerts H, Andrearczyk V, Apte A, Ashrafinia S, Bakas S, Beukinga RJ, Boellaard R, et al. The image biomarker standardization initiative: standardized quantitative radiomics for high-throughput image-based phenotyping. Radiology. 2020;295(2):328–38.
Kadoya N, Tanaka S, Kajikawa T, Tanabe S, Abe K, Nakajima Y, Yamamoto T, Takahashi N, Takeda K, Dobashi S, et al. Homology-based radiomic features for prediction of the prognosis of lung cancer based on CT-based radiomics. Med Phys. 2020;47(5):2197–205.
Zhao B, James LP, Moskowitz CS, Guo P, Ginsberg MS, Lefkowitz RA, Qin Y, Riely GJ, Kris MG, Schwartz LH. Evaluating variability in tumor measurements from same-day repeat CT scans of patients with non-small cell lung cancer. Radiology. 2009;252(1):263–72.
Clark K, Vendt B, Smith K, Freymann J, Kirby J, Koppel P, Moore S, Phillips S, Maffitt D, Pringle M, et al. The Cancer Imaging Archive (TCIA): maintaining and operating a public information repository. J Digit Imaging. 2013;26(6):1045–57.
Zhao B, Tan Y, Tsai WY, Qi J, Xie C, Lu L, Schwartz LH. Reproducibility of radiomics for deciphering tumor phenotype with imaging. Sci Rep. 2016;6:23428.
Tanaka S, Kadoya N, Kajikawa T, Matsuda S, Dobashi S, Takeda K, Jingu K. Investigation of thoracic four-dimensional CT-based dimension reduction technique for extracting the robust radiomic features. Phys Med. 2019;58:141–8.
van Baardwijk A, Bosmans G, Boersma L, Buijsen J, Wanders S, Hochstenbag M, van Suylen RJ, Dekker A, Dehing-Oberije C, Houben R, et al. PET-CT-based auto-contouring in non-small-cell lung cancer correlates with pathology and reduces interobserver variability in the delineation of the primary tumor and involved nodal volumes. Int J Radiat Oncol Biol Phys. 2007;68(3):771–8.
Mori M, Passoni P, Incerti E, Bettinardi V, Broggi S, Reni M, Whybra P, Spezi E, Vanoli EG, Gianolli L, et al. Training and validation of a robust PET radiomic-based index to predict distant-relapse-free-survival after radio-chemotherapy for locally advanced pancreatic cancer. Radiother Oncol. 2020;153:258–64.
Li H, Zhang R, Wang S, Fang M, Zhu Y, Hu Z, Dong D, Shi J, Tian J. CT-based radiomic signature as a prognostic factor in stage IV ALK-positive non-small-cell lung cancer treated with TKI crizotinib: A Proof-of-Concept Study. Front Oncol. 2020;10:57.
Erdim C, Yardimci AH, Bektas CT, Kocak B, Koca SB, Demir H, Kilickesmez O. Prediction of benign and malignant solid renal masses: machine learning-based CT texture analysis. Acad Radiol. 2020;27(10):1422–9.
Lin P, Yang PF, Chen S, Shao YY, Xu L, Wu Y, Teng W, Zhou XZ, Li BH, Luo C, et al. A Delta-radiomics model for preoperative evaluation of Neoadjuvant chemotherapy response in high-grade osteosarcoma. Cancer Imaging. 2020;20(1):7.
Baessler B, Nestler T, Pinto Dos Santos D, Paffenholz P, Zeuch V, Pfister D, Maintz D, Heidenreich A. Radiomics allows for detection of benign and malignant histopathology in patients with metastatic testicular germ cell tumors prior to post-chemotherapy retroperitoneal lymph node dissection. Eur Radiol. 2020;30(4):2334–45.
Kakino R, Nakamura M, Mitsuyoshi T, Shintani T, Kokubo M, Negoro Y, Fushiki M, Ogura M, Itasaka S, Yamauchi C, et al. Application and limitation of radiomics approach to prognostic prediction for lung stereotactic body radiotherapy using breath-hold CT images with random survival forest: A multi-institutional study. Med Phys. 2020;47(9):4634–43.
Wang L, Dong T, Xin B, Xu C, Guo M, Zhang H, Feng D, Wang X, Yu J. Integrative nomogram of CT imaging, clinical, and hematological features for survival prediction of patients with locally advanced non-small cell lung cancer. Eur Radiol. 2019;29(6):2958–67.
van Timmeren JE, van Elmpt W, Leijenaar RTH, Reymen B, Monshouwer R, Bussink J, Paelinck L, Bogaert E, De Wagter C, Elhaseen E, et al. Longitudinal radiomics of cone-beam CT images from non-small cell lung cancer patients: evaluation of the added prognostic value for overall survival and locoregional recurrence. Radiother Oncol. 2019;136:78–85.
Oikonomou A, Khalvati F, Tyrrell PN, Haider MA, Tarique U, Jimenez-Juan L, Tjong MC, Poon I, Eilaghi A, Ehrlich L, et al. Radiomics analysis at PET/CT contributes to prognosis of recurrence and survival in lung cancer treated with stereotactic body radiotherapy. Sci Rep. 2018;8(1):4003.
Lao J, Chen Y, Li ZC, Li Q, Zhang J, Liu J, Zhai G. A deep learning-based radiomics model for prediction of survival in glioblastoma multiforme. Sci Rep. 2017;7(1):10353.
Sun W, Jiang M, Dang J, Chang P, Yin FF. Effect of machine learning methods on predicting NSCLC overall survival time based on Radiomics analysis. Radiat Oncol. 2018;13(1):197.
Leger S, Zwanenburg A, Pilz K, Lohaus F, Linge A, Zöphel K, Kotzerke J, Schreiber A, Tinhofer I, Budach V, et al. A comparative study of machine learning methods for time-to-event survival data for radiomics risk modelling. Sci Rep. 2017;7(1):13206.
Saeys Y, Inza I, Larrañaga P. A review of feature selection techniques in bioinformatics. Bioinformatics (Oxford, England). 2007;23(19):2507–17.
Zhou X, Yi Y, Liu Z, Zhou Z, Lai B, Sun K, Li L, Huang L, Feng Y, Cao W, et al. Radiomics-based preoperative prediction of lymph node status following neoadjuvant therapy in locally advanced rectal cancer. Front Oncol. 2020;10:604.
Ouyang ML, Xia HW, Xu MM, Lin J, Wang LL, Zheng XW, Tang K. Prediction of occult lymph node metastasis using SUV, volumetric parameters and intratumoral heterogeneity of the primary tumor in T1–2N0M0 lung cancer patients staged by PET/CT. Ann Nucl Med. 2019;33(9):671–80.
Wang X, Duan H, Li X, Ye X, Huang G, Nie S. A prognostic analysis method for non-small cell lung cancer based on the computed tomography radiomics. Phys Med Biol. 2020;65(4):045006.
Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, Yokoi T, Chiappori A, Lee KH, de Wit M, et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med. 2017;377(20):1919–29.
Sun R, Limkin EJ, Vakalopoulou M, Dercle L, Champiat S, Han SR, Verlingue L, Brandao D, Lancia A, Ammari S, et al. A radiomics approach to assess tumour-infiltrating CD8 cells and response to anti-PD-1 or anti-PD-L1 immunotherapy: an imaging biomarker, retrospective multicohort study. Lancet Oncol. 2018;19(9):1180–91.
Liu C, Gong J, Yu H, Liu Q, Wang S, Wang J. A CT-based radiomics approach to predict nivolumab response in advanced non-small-cell lung cancer. Front Oncol. 2021;11:544339.
Zhao S, Hou D, Zheng X, Song W, Liu X, Wang S, Zhou L, Tao X, Lv L, Sun Q, et al. MRI radiomic signature predicts intracranial progression-free survival in patients with brain metastases of ALK-positive non-small cell lung cancer. Transl Lung Cancer Res. 2021;10(1):368–80.
Rios Velazquez E, Aerts HJ, Gu Y, Goldgof DB, De Ruysscher D, Dekker A, Korn R, Gillies RJ, Lambin P. A semiautomatic CT-based ensemble segmentation of lung tumors: comparison with oncologists’ delineations and with the surgical specimen. Radiother Oncol. 2012;105(2):167–73.
Velazquez ER, Parmar C, Jermoumi M, Mak RH, van Baardwijk A, Fennessy FM, Lewis JH, De Ruysscher D, Kikinis R, Lambin P, et al. Volumetric CT-based segmentation of NSCLC using 3D-Slicer. Sci Rep. 2013;3:3529.
Funding
This study was supported in part by the Japan Society for the Promotion of Science Grant-in-Aid for Scientific Research (C) (19K08116).
Author information
Authors and Affiliations
Contributions
YS, ST, HO, and MU collected the lung cancer data. YS, NK, and ST contributed to the conception and design of the study. YS, ST, and ST wrote the program. YS and MU performed the analysis. YS mainly drafted the manuscript. NK, YT, TK, DS, TK, and JK reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study applied for an application to ethics committee of Tohoku University Graduate School of Medicine and have already obtained consent to this (2019–1-132).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary A.
List of radiomic features used in this study. Supplementary B: List of robust radiomic features. (FS1). Supplementary C: List of non-redundant radiomic features. (FS2). Supplementary D: List of robust and non-redundant radiomic features. (FS3). Supplementary E: Patient characteristics for each subgroup. Supplementary F: Prognostic performance of the radiomic model in each subgroup with five-fold cross-validation. Supplementary G: Prognostic performance of the combined model in each subgroup with five-fold cross-validation. Supplementary H: Feature selection using the LASSO Cox model in the radiomic and combined models for each subgroup. Supplementary I: Kaplan–Meier curves for low- and high-risk groups based on the rad score in the radiomic models for each subgroup. Supplementary J: Kaplan–Meier curves for low- and high-risk groups based on the rad score in the combined models for each subgroup. Supplementary K: For each analysis group, the features and their coefficients selected by the LASSO Cox regression model in the radiomic models. Supplementary L: For each analysis group, the features and their coefficients selected by the LASSO Cox regression model in the combined models. Supplementary M: Patient characteristics for the Lung 1 dataset. Supplementary N: Prognostic performance of the radiomic and combined models in each subgroup with five-fold cross-validation (Lung 1 dataset). Supplementary O: Kaplan–Meier curves for low- and high-risk groups based on the rad score in the radiomic and combined models for each subgroup (Lung 1 dataset). Supplementary P: For each analysis group, the features and their coefficients selected in the LASSO Cox regression model in the radiomic and combined models (Lung 1 dataset).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sugai, Y., Kadoya, N., Tanaka, S. et al. Impact of feature selection methods and subgroup factors on prognostic analysis with CT-based radiomics in non-small cell lung cancer patients. Radiat Oncol 16, 80 (2021). https://doi.org/10.1186/s13014-021-01810-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-021-01810-9