Abstract
Aim
To describe the feasibility of image guided intensity modulated radiotherapy (IG-IMRT) using daily soft tissue matching in the treatment of bladder cancer.
Methods
Twenty-eight patients with muscle-invasive carcinoma of the bladder were recruited to a protocol of definitive radiation using IMRT with accelerated hypofractionation with simultaneous integrated boost (SIB). Isotropic margins of .5 and 1 cm were used to generate the high risk and intermediate risk planning target volumes respectively. Cone beam CT (CBCT) was acquired daily and a soft tissue match was performed. Cystoscopy was scheduled 6 weeks post treatment.
Results
The median age was 83 years (range 58-92). Twenty patients had stage II or III disease, and eight were stage IV. Gross disease received 66 Gy in 30 fractions in 11 patients (ten with concurrent chemotherapy) or 55 Gy in 20 fractions for those of poorer performance status or with palliative intent. All patients completed radiation treatment as planned. Three patients ceased chemotherapy early due to toxicity. Six patients (21 %) had acute Grade ≥ 2 genitourinary (GU) toxicity and six (21 %) had acute Grade ≥ 2 gastrointestinal (GI) toxicity. Five patients (18 %) developed Grade ≥2 late GU toxicity and no ≥2 late GI toxicity was observed.
Nineteen patients underwent cystoscopy following radiation, with complete response (CR) in 16 cases (86 %), including all patients treated with chemoradiotherapy. Eight patients relapsed, four of which were local relapses. Of the patients with local recurrence, one underwent salvage cystectomy. For patients treated with definitive intent, freedom from locoregional recurrence (FFLR) and overall survival (OS) was 90 %/100 % for chemoradiotherapy versus 86 %/69 % for radiotherapy alone.
Conclusion
IG- IMRT using daily soft tissue matching is a feasible in the treatment of bladder cancer, enabling the delivery of accelerated synchronous integrated boost with good early local control outcomes and low toxicity.
Similar content being viewed by others
Introduction
Muscle Invasive bladder cancer presents a unique set of treatment related challenges in what is typically an older patient group with significant medical co-morbidity. Radical surgery with cystectomy and pelvic lymph node dissection poses many challenges in this group of patients with high perioperative risks and potential ongoing morbidity in relation to sexual dysfunction and the physical and psychological impact of urinary diversion [1–3]. Bladder preservation, in which radiation is delivered with concurrent chemotherapy following maximal trans-urethral resection of bladder tumour (TURBT), is an alternative to surgical management, with similar 5 year overall survival rates of 48-65 % accounting for stage and co-morbidity [4–6]. However it remains underutilised, with patterns of care studies showing that aggressive radiation-based treatment is offered at a considerably lower rate compared with cystectomy [7, 8].
One of the barriers to greater utilisation of radiotherapy is perhaps the technical challenges with delivering this treatment. The distortable nature of the bladder, variable bladder filling, as well as motion of other pelvic organs all contribute to uncertainties with respect to target coverage [9–11]. The use of image guidance and adaptive therapy is potentially of great value in this setting by allowing the reduction of planning target volume (PTV) margins and improved target coverage [10, 12–14]. Another challenge lies in the radiobiologic characteristics of bladder cancer. There is a narrow therapeutic window with respect to irradiation of the bladder due to the risk of radiation toxicity to the bladder itself, as well as adjacent normal tissues [15, 16]. A radiation dose response has been established in the treatment of bladder cancer, but the wide margins required for standard conformal techniques are dose limiting [17, 18]. Furthermore, there is some evidence that urothelial carcinoma displays sensitivity to overall treatment time, with accelerated repopulation occurring at 5-6 weeks after commencing radiation [19].
IMRT is of considerable interest in this regard due to the superior conformality and normal tissue sparing demonstrated with its use in other pelvic malignancies, most notably prostate and cervical cancer [20, 21]. Its application in bladder cancer is less frequently described, but is appealing due to the potential to dose escalate gross disease using an integrated boost technique, and shorten overall treatment time. The concern with IMRT is of geographic miss; however with daily on treatment soft tissue alignment with CBCT it is possible to overcome this obstacle. In 2010, the Northern Sydney Cancer Centre developed a protocol of IG-IMRT with daily soft tissue matching for the treatment of patients with bladder cancer. Here, we report our experience with this technique in a cohort of 28 patients treated from 2010-2013.
Methods
Patient selection
Approval for this study was obtained from the Northern Sydney Local Health District Human Research Ethics Committee. Potential candidates for the IG-IMRT protocol were identified at the genitourinary cancer multidisciplinary meeting attended by members of the departments of Urology, Pathology, Radiology, Medical Oncology and Radiation Oncology. Patients were eligible for treatment if they had biopsy proven muscle-invasive urothelial or squamous carcinoma of the bladder and were not for definitive cystectomy (either due to inoperable disease or patient preference). Exclusion criteria included previous pelvic radiation, poor performance status (ECOG ≥3) and extensive visceral metastases. Patients with low volume metastases were considered if their life expectancy was estimated to be >6 months.
In addition to diagnostic cystoscopy and biopsy, patients underwent staging with whole body bone scan and CT of the chest, abdomen and pelvis. Unless contraindicated, pelvic multiparametric MRI was performed to aid tumour delineation. In patients being considered for curative chemoradiation (CRT), maximal TURBT was performed ≤6 weeks prior to commencing radiation treatment. When possible, patients also had 3-4 gold markers inserted near the tumour bed under cystoscopic guidance. This procedure was performed by their Urologist under general anaesthesia.
Planning and treatment
After providing written consent for radiation treatment, patients underwent CT simulation. Two image sets were acquired for each patient: one with the patient’s bladder comfortably full, and the second with an empty bladder. Planning CT images were fused with the diagnostic contrast-enhanced CT and MRI to aid tumour volume delineation. As the bladder volume of the MRI commonly differed from the planning CT scan, the MRI was interpreted with the aid of a radiologist to define the anatomical area of the bladder at highest risk of gross residual disease (GTV), which was then contoured. The intermediate risk clinical target volume (IRCTV) was defined as the whole bladder and expanded by 10 mm to the intermediate risk PTV (IRPTV) and the GTV was expanded by 0.5 cm to create the high risk PTV (HRPTV). If treated, the uninvolved obturator, internal and external iliac nodes were contoured as a separate low risk CTV (LRCTV) and then expanded by a 1 cm margin to a low risk PTV (LRPTV).
Most patients were subsequently treated with an empty bladder, but the “full bladder” image set was used in patients when appropriate to separate the small bowel from the gross disease. This decision was made by the treating oncologist before the planning was performed. Radiation was planned and delivered using a 7-10 field sliding-window IMRT technique on a Varian Trilogy (Varian Medical Systems, Palo Alto, CA, USA). Patients were treated with and accelerated moderate hypofractionated schedule with either 20 or 30 fractions, incorporating a simultaneous integrated boost to the GTV if identified. The 30 fraction group included patients with localised disease who were regarded fit enough to receive combined chemo-irradiation. They received 66 Gy, 60 Gy and 54 Gy to the HRPTV, IRPTV and the pelvic nodes respectively. In patients treated with 20 fractions, the doses were 55 Gy, 50 Gy and 45 Gy without concurrent chemotherapy.
Platinum chemotherapy was administered concurrently in suitable candidates. Chemotherapy was cisplatin 35 mg/m2 once weekly unless contraindicated when weekly AUC2 carboplatin was used.
For patients planned with an empty bladder a hand-held ultrasound was performed daily prior to treatment to ensure the bladder was empty. A CBCT was obtained prior to treatment with the Varian Trilogy on board imaging system with a 2.5 mm slice thickness over a 16 cm length with a resolution of 384 × 384 pixels. Following this the treating radiation therapists performed a soft tissue match to the GTV. This was supervised by the treating Radiation Oncologist for the first five fractions, and thereafter as required based upon feedback from the radiation therapist. The first step was to identify if the bladder was outside the IRPTV, in which case these patients were asked to further empty their bladder. If present, fiducial markers were used to aid initial alignment in the superior/inferior direction, and then the GTV was matched. If no fiducials were present then the GTV was used to guide the entire match (see Fig. 1). This match was centred on the region of the bladder identified as the highest risk of gross disease (GTV), rather than identifying any abnormality on the CBCT itself. In patients treated with a full bladder a margin of 10 mm above and below the superior aspect of the bladder was defined on the planning scans. Patients were required to have a bladder volume within these limits on CBCT before proceeding with the match to the GTV.
GTV delineation and soft tissue match to GTV on CBCT. Figs. a and b demonstrate the following contours as delineated on MR fusion (a) and planning CT (b): GTV – blue; High Risk PTV (HRPTV) – red; Bladder - pink; Intermediate Risk PTV (IRPTV) – purple and Low Risk PTV (LRPTV) – light brown. Figs. c and d show these contours overlaid on the cone beam CT to facilitate soft tissue match
Assessment and follow up
Patients were assessed weekly during treatment and 3-6 monthly after treatment. Toxicity was graded by the treating physician at each assessment according to the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. Cystoscopy was performed 6-12 weeks post treatment and annually thereafter. CR was defined as no visible evidence of bladder tumour and a negative biopsy. The primary endpoint for the study was freedom from local failure (FFLR). Secondary endpoints were complete response rate on cystoscopy, acute and late toxicity and overall survival.
Statistics
Survival outcomes were calculated from the first day of radiation treatment to the first clinical, radiologic or cystoscopic evidence of recurrence in the bladder (FFLR), any recurrence (disease free survival, DFS) or death (OS). In the absence of any of these events, survival was censored at the last follow up. The rates of FFLR, DFS and OS and were calculated using the Kaplan-Meier method.
Results
Patient characteristics
Patient and tumour characteristics are outlined in Table 1. In total, twenty-eight patients were treated on this protocol between June 2010 and September 2013. The cohort included 22 males and six females, with a median age of 83 years (range 58-92). All but two patients had muscle-invasive transitional cell carcinoma; two others had squamous cell carcinoma. Stage T2, T3 and T4 disease was identified in 6, 14 and 8 patients respectively. Five patients had positive nodes, and four patients had distant metastatic disease. A maximal TURBT was possible in 64 % of cases and 32 % had hydronephrosis at presentation. A further 36 % had a history of previous superficial bladder cancer receiving intravesical BCG.
Treatment and toxicity
Radiation and chemotherapy treatment details are outlined in Table 2. In 23 patients, radiation treatment was given with curative intent with ten patients receiving concurrent chemotherapy (cisplatin n = 8; carboplatin n = 2) and 13 patients receiving radiation alone. In five patients, who had either extensive nodal involvement or metastatic disease at diagnosis, radiation treatment was considered palliative. These patients received a dose of 50-55 Gy in 20 fractions. A total of 22 patients received treatment to the regional lymph nodes, including all patients having concurrent chemotherapy. The GTV was identified and treated with an integrated boost in all but one patient. Fiducial markers were successfully placed in nine patients. There were a total of 680 fractions delivered to the 28 patients. Seventeen patients were treated with an empty bladder and eleven with a full bladder. Average treatment time, including set-up was 11 min, with patients scheduled in standard 15-min bookings.
All patients completed radiation treatment as prescribed. Reproducibility of bladder filling on the CBCT was very good with an empty bladder, with only five of 400 fractions requiring patients to be removed from the treatment couch. The full bladder protocol was less reproducible, with seven of the 11 patients requiring at least one re-set up to fill their bladders. In total, re-set up was required for 29 of 280 fractions in the full bladder group, 22 due to inadequate filling, five due to overfilling, one due to machine breakdown and one due to gas obscuring the GTV match. Of the 11 patients who commenced treatment with a full bladder plan, two were subsequently replanned with empty bladders, one at fraction 5 and one at fraction 10.
Three patients ceased concurrent chemotherapy early, two due to cisplatin-related emesis, and another due to Grade 2 thrombocytopenia. Four patients required admission to hospital during treatment. Two of these admissions were for supportive care and intravenous fluids due to treatment toxicity. A further two patients were admitted overnight for packed-cell transfusion to treat symptomatic anaemia resulting from haematuria which had been present at baseline. In both cases, the admissions took place in the first half of radiation treatment and the haematuria subsequently resolved.
Acute Grade 2 GU toxicity was reported by six patients (21 %). No patients experienced acute Grade 3 GU toxicity. Six patients reported Grade ≥2 GI toxicity, including two patients with grade 3 nausea. There were five patients (18 %) with Grade ≥2 late GU toxicity including one patient requiring bilateral ureteric stents (Grade 3). There was no late Grade 2 or 3 GI toxicity. These figures are summarised in Table 3.
Outcomes
Patients were analysed according to the intent of treatment (definitive versus palliative). Within the definitive group, subset analyses were performed for patients treated with chemoradiation and those who received radiation alone. Results are summarised in Table 4.
Definitive cohort
Nineteen of the 23 definitive patients underwent cystoscopy and biopsy following treatment, including nine of the ten patients who received CRT and ten of 13 patients in the RT alone group. Of the four patients who did not have cystoscopy, one was lost to follow up overseas and three patients treated with RT alone declined the procedure. The cystoscopic complete response rate was 86 %, (100 % in the CRT group and 81 % in the radiotherapy alone group). At 2 years the local control was 90 % in the CRT group and 86 % in the definitive RT alone group and OS was 100 % and 69 % respectively.
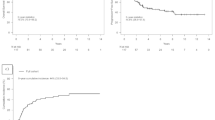
In patients treated definitively, freedom from local failure was 78 % at 2 years (Fig. 2). There were four local failures, with one patient proceeding to salvage cystectomy. Of the remaining three patients, two declined intervention and remain alive with disease; one patient has died as a result of obstructive renal failure. A further two patients in the group have had documented distant relapse. The DFS and overall survival rates were 73 % and 80 % at 2 years respectively. Kaplan Meier curves for overall survival are shown in Fig. 3.
Palliative cohort
Three of the five patients treated with palliative intent died during the follow up period, two due to bladder cancer and one from an unrelated illness. One patient experienced local progression, translating to a 1 year FFLR of 80 %, and a median of 6 months. Median survival was 10 months (1 year OS 30 %).
Discussion
In our series, IG-IMRT with a synchronous integrated boost was well tolerated, with excellent early results. Although longer follow up is required, the high complete response rate and 2 year loco-regional control support the feasibility and promise of this technique.
The heterogeneous nature of our cohort in terms of tumour stage and treatment is acknowledged. However, allowing for this, our results compare favourably to larger bladder preservation studies employing 3D conformal techniques and minimal image guidance. In the landmark BC2001 study of chemoradiation with mitomycin and 5-fluorouracil versus radiation alone, James et al. reported a 2-year locoregional DFS of 67 % in the chemoradiotherapy group, and 54 % in the radiotherapy alone group [5]. In two sequential phase II trials of definitive chemoradiation with weekly low dose cisplatin conducted by the Trans Tasman Radiation Oncology Group (TROG) Gogna et al. reported a CR rate of 70 % and local control of 45 % at 5 years [22]. This compares to our cohort who had a 90 % 2 year local control following chemoradiotherapy and 86 % for radiotherapy alone.
Although there is limited literature on the use of IMRT for bladder cancer, two studies that are available report similar outcomes. Turgeon et al. reported a CR rate of 83 % and a 2 year OS of 69 % in a series of 24 patients treated with hypofractionated IMRT and concurrent chemotherapy [23]. In a separate prospective study Hsieh et al. described a 2-year locoregional recurrence free survival of 87.5 % in 19 patients with bladder cancer who were treated with either IMRT or tomotherapy. The overall survival in their cohort was low (26.3 % at 2 years) reflecting the fact that one third of the cohort had stage IV disease [24]. Of note neither of these studies used daily soft tissue matching, and PTV margins were generous at 1.5 to 2.5 cm. The addition of daily soft tissue matching in our protocol allowed a margin reduction to 0.5 cm for high-risk areas and 1 cm around the bladder. With the use of IMRT and small margins, relative dose escalation was possible while achieving low toxicity (see Table 3).
Palliative cases notwithstanding, our cohort as a whole represents a high-risk population. The majority of the cases were stage III/IV, and overall the patients were elderly (median age 83 years). One third of patients had hydronephrosis, incomplete TURBT or a history of superficial carcinoma progressing despite BCG, all of which are known poor prognostic indicators [25–28]. In this context, our 2 year FFLR and OS for the definitive cohort (78 % and 80 % respectively) are very encouraging. Therefore although we have demonstrated excellent outcomes for a highly selected group of patients who received combined chemoradiation, high dose radiation need not be reserved for these patients alone.
The acute toxicity observed in our cohort was modest compared to rates reported in other high dose trials. James et al. reported CTCAE grade 3-4 acute side effects in 27.5 % and 36 % in the radiotherapy alone and chemoradiotherapy groups respectively [5]. In the TROG chemoradiation trials, 35 % of patients experienced grade 2 GI effects, and more than 40 % reported grade 2 GU toxicity [22]. These trials used conformal radiation techniques, and we note that the low GI toxicity experienced by our patients is in keeping with the normal tissue sparing properties of pelvic IMRT [23, 24]. More specifically, clinical and planning studies have demonstrated the superiority of IMRT compared with conformal therapy with respect to small bowel volumes receiving doses of 20-50Gy [29, 30]. This is of particular relevance to patients in whom the clinical target extends beyond the bladder to include the regional nodes, as was the case in the majority of our patients. Although pelvic nodal relapse following bladder radiotherapy is reportedly uncommon, the large margins employed for the radiation delivered in previous trials may have resulted in the majority of the regional nodes receiving therapeutic radiation doses. In our cohort, nodal irradiation was justified on the basis of the comparatively small margins (1 cm) used in our technique and evidence from surgical series demonstrating improved outcome with nodal dissection [31].
Our patients received a simultaneous integrated boost to the GTV, identified using clinical, cystoscopic and radiologic information. We found multiparametric MRI to be a substantial aid in GTV delineation. The main limitation with MRI fusion was the requirement for a comfortably full bladder at the time of MRI to aid diagnostic reporting, with most patients having their final volumes on an empty bladder scan. We are currently investigating elastic deformation to account for the anisotropic margins required for changes in bladder size, which will enable better fusion of the MRI and planning CT. MRI is not only promising with respect to bladder tumour staging and characterisation, but also as a potential predictor of pathologic response to therapy [32, 33].
An alternative means to identify the GTV is fiducial markers, which were successfully placed around the tumour bed in nine of our patients. Elsewhere, the use of fiducial markers has been reported with few complications and excellent visibility on CBCT [34–36]. However, in our experience, the implementation of a fiducial marker program for bladder radiation proved to be a challenging process and did not always aid in tumour delineation. As such it was ceased part way through the study. Custom-designed equipment as described by Garcia et al. may address some of the technical difficulties that inhibited marker placement in many of our patients [34].
Various adaptive strategies have been described by several groups including ‘PTV of the day’ selection, isocentre shifts and corrections for translational and rotational motion [12, 14, 37, 38]. Our daily image-guidance with CBCT and soft tissue match is unique with no previously published IMRT series utilising this approach. It is clear from the extensive experience in other pelvic malignancies that as the quality of on-board CBCT imaging has improved, so has the workflow and ease of matching. In our patients, on average treatment was completed well within the allocated time, and therefore did not impact adversely on departmental resources or workflow. The treating Radiation Oncologist supervised the matching during the first week of treatment and only attended subsequent to this if problems were identified by the radiation therapy team, including the seven occasions when reset up was required and two patients who ultimately needed replanning.
In a paper comparing matching techniques in patients treated on an adaptive planning bladder study, Foroudi et al. found 1 cm CTV to PTV margins were found to be feasible when using soft tissue match. The resulting coverage with this margin was adequate in 89 % of cases, whereas margins of 2 cm or greater were required to achieve the same coverage using bony alignment or skin tattoos [39]. Our study further supports this finding, with only 5/400 fractions treated with an empty bladder requiring the patient to be taken off the table. We believe this high rate of daily bladder filling reproducibility is a result of patient education with respect to bladder emptying and subsequent reinforcement by daily feedback from the treating therapists based on ultrasound and CBCT images. This is in contrast to the large variations in bladder filling reported from the recent TROG study: 16 % of patients in that study had, on at least one occasion, a pre-treatment bladder CTV extending beyond all of the three possible adaptive plans [37].
A limitation of our study was no CBCTs were performed after treatment to assess intrafraction motion which may be important, especially with the high dose gradients of IMRT which could be more pronounced on days of hydration for cisplatin chemotherapy [37]. The risk is the bladder may move outside the IRPTV for part of the beam-on time. Our excellent local control, despite this risk, supports the concept that not all regions of the bladder require the same dose. This was shown in the BC2001 study. In this study there was similar 2-year local control with partial bladder irradiation (64 %) and full bladder irradiation (61 %) [40]. Intrafraction motion will also be reduced in the future with the introduction of volumetric arc therapy (VMAT) [41].
Conclusion
IG-IMRT with daily soft tissue matching is a promising approach in the treatment of muscle invasive bladder cancer, enabling the delivery of an accelerated simultaneous integrated boost IMRT with low rates of toxicity. Early local control and disease free survival are encouraging, especially in light of our high-risk population. Longer follow-up is required to assess the efficacy of this technique.
Abbreviations
- CBCT:
-
Cone beam CT
- CR:
-
Complete response
- CRT:
-
Chemoradiation
- CTV:
-
Clinical target volume
- DFS:
-
Disease free survival
- FFLR:
-
Freedom from locoregional recurrence
- GI:
-
Gastrointestinal
- GTV:
-
Gross tumour volume
- GU:
-
Genitourinary
- HRPTV:
-
High risk planning target volume
- IG-IMRT:
-
Image-guided intensity modulated radiotherapy
- IRCTV:
-
Intermediate risk clinical target volume
- IRPTV:
-
Intermediate risk planning target volume
- LRPTV:
-
Low risk planning target volume
- SIB:
-
Simultaneous integrated boost
- TURBT:
-
Transurethral resection of bladder tumour
References
Benner C, Greenberg M, Shepard N, Meng MV, Rabow MW. The natural history of symptoms and distress in patients and families following cystectomy for treatment of muscle invasive bladder cancer. J Urol. 2014;191(4):937–42.
Caffo O, Fellin G, Graffer U, Luciani L. Assessment of quality of life after cystectomy or conservative therapy for patients with infiltrating bladder carcinoma. A survey by a self-administered questionnaire. Cancer. 1996;78(5):1089–97.
Henningsohn L. Quality of life after therapy for muscle-invasive bladder cancer. Curr Opin Urol. 2006;16(5):356–60.
Choudhury A, Swindell R, Logue JP, Elliott PA, Livsey JE, Wise M, et al. Phase II study of conformal hypofractionated radiotherapy with concurrent gemcitabine in muscle-invasive bladder cancer. J Clin Oncol. 2011;29(6):733–8.
James ND, Hussain SA, Hall E, Jenkins P, Tremlett J, Rawlings C, et al. Radiotherapy with or without chemotherapy in muscle-invasive bladder cancer. N Engl J Med. 2012;366(16):1477–88.
Tunio MA, Hashmi A, Qayyum A, Mohsin R, Zaeem A. Whole-pelvis or bladder-only chemoradiation for lymph node-negative invasive bladder cancer: single-institution experience. Int J Radiat Oncol Biol Phys. 2012;82(3):e457–62.
Gray PJ, Fedewa SA, Shipley WU, Efstathiou JA, Lin CC, Zietman AL, et al. Use of potentially curative therapies for muscle-invasive bladder cancer in the United States: results from the National Cancer Data Base. Eur Urol. 2013;63(5):823–9.
Kozak KR, Hamidi M, Manning M, Moody JS. Bladder preservation for localized muscle-invasive bladder cancer: the survival impact of local utilization rates of definitive radiotherapy. Int J Radiat Oncol Biol Phys. 2012;83(2):e197–204.
Lotz HT, Pos FJ, Hulshof MC, van Herk M, Lebesque JV, Duppen JC, et al. Tumor motion and deformation during external radiotherapy of bladder cancer. Int J Radiat Oncol Biol Phys. 2006;64(5):1551–8.
Redpath AT, Muren LP. CT-guided intensity-modulated radiotherapy for bladder cancer: isocentre shifts, margins and their impact on target dose. Radiother Oncol. 2006;81(3):276–83.
Fokdal L, Honoré H, Høyer M, Meldgaard P, Fode K, von der Maase H. Impact of changes in bladder and rectal filling volume on organ motion and dose distribution of the bladder in radiotherapy for urinary bladder cancer. Int J Radiat Oncol Biol Phys. 2004;59(2):436–44.
Burridge N, Amer A, Marchant T, Sykes J, Stratford J, Henry A, et al. Online adaptive radiotherapy of the bladder: small bowel irradiated-volume reduction. Int J Radiat Oncol Biol Phys. 2006;66(3):892–7.
Foroudi F, Pham D, Bressel M, Hardcastle N, Gill S, Kron T. Comparison of margins, integral dose and interfraction target coverage with image-guided radiotherapy compared with non-image-guided radiotherapy for bladder cancer. Clin Oncol (R Coll Radiol). 2014;26(8):497–505.
Pos FJ, Hulshof M, Lebesque J, Lotz H, van Tienhoven G, Moonen L, et al. Adaptive radiotherapy for invasive bladder cancer: a feasibility study. Int J Radiat Oncol Biol Phys. 2006;64(3):862–8.
Viswanathan AN, Yorke ED, Marks LB, Eifel PJ, Shipley WU. Radiation dose-volume effects of the urinary bladder. Int J Radiat Oncol Biol Phys. 2010;76(3 Suppl):S116–22.
Kavanagh BD, Pan CC, Dawson LA, Das SK, Li XA, Ten Haken RK, et al. Radiation dose-volume effects in the stomach and small bowel. Int J Radiat Oncol Biol Phys. 2010;76(3 Suppl):S101–7.
Cowan RA, McBain CA, Ryder WD, Wylie JP, Logue JP, Turner SL, et al. Radiotherapy for muscle-invasive carcinoma of the bladder: results of a randomized trial comparing conventional whole bladder with dose-escalated partial bladder radiotherapy. Int J Radiat Oncol Biol Phys. 2004;59(1):197–207.
Majewski W, Maciejewski B, Majewski S, Suwinski R, Miszczyk L, Tarnawski R. Clinical radiobiology of stage T2-T3 bladder cancer. Int J Radiat Oncol Biol Phys. 2004;60(1):60–70.
Maciejewski B, Majewski S. Dose fractionation and tumour repopulation in radiotherapy for bladder cancer. Radiother Oncol. 1991;21(3):163–70.
Mundt AJ, Lujan AE, Rotmensch J, Waggoner SE, Yamada SD, Fleming G, et al. Intensity-modulated whole pelvic radiotherapy in women with gynecologic malignancies. Int J Radiat Oncol Biol Phys. 2002;52(5):1330–7.
Zelefsky MJ, Levin EJ, Hunt M, Yamada Y, Shippy AM, Jackson A, et al. Incidence of late rectal and urinary toxicities after three-dimensional conformal radiotherapy and intensity-modulated radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2008;70(4):1124–9.
Gogna NK, Matthews JH, Turner SL, Mameghan H, Duchesne GM, Spry N, et al. Efficacy and tolerability of concurrent weekly low dose cisplatin during radiation treatment of localised muscle invasive bladder transitional cell carcinoma: a report of two sequential Phase II studies from the Trans Tasman Radiation Oncology Group. Radiother Oncol. 2006;81(1):9–17.
Turgeon GA, Souhami L, Cury FL, Faria SL, Duclos M, Sturgeon J, et al. Hypofractionated intensity modulated radiation therapy in combined modality treatment for bladder preservation in elderly patients with invasive bladder cancer. Int J Radiat Oncol Biol Phys. 2014;88(2):326–31.
Hsieh CH, Chung SD, Chan PH, Lai SK, Chang HC, Hsiao CH, et al. Intensity modulated radiotherapy for elderly bladder cancer patients. Radiat Oncol. 2011;6:75.
Schrier BP, Hollander MP, van Rhijn BW, Kiemeney LA, Witjes JA. Prognosis of muscle-invasive bladder cancer: difference between primary and progressive tumours and implications for therapy. Eur Urol. 2004;45(3):292–6.
Scrimger RA, Murtha AD, Parliament MB, Venner PM, Hanson J, Houle G, et al. Muscle-invasive transitional cell carcinoma of the urinary bladder: a population-based study of patterns of care and prognostic factors. Int J Radiat Oncol Biol Phys. 2001;51(1):23–30.
Wu CE, Lin YC, Hong JH, Chuang CK, Pang ST, Liaw CC. Prognostic value of complete response in patients with muscle-invasive bladder cancer undergoing concurrent chemoradiotherapy. Anticancer Res. 2013;33(6):2605–10.
Rödel C, Grabenbauer GG, Kühn R, Papadopoulos T, Dunst J, Meyer M, et al. Combined-modality treatment and selective organ preservation in invasive bladder cancer: long-term results. J Clin Onc. 2002;20(14):3061–71.
Søndergaard J, Høyer M, Petersen JB, Wright P, Grau C, Muren LP. The normal tissue sparing obtained with simultaneous treatment of pelvic lymph nodes and bladder using intensity-modulated radiotherapy. Acta Oncol. 2009;48(2):238–44.
van Rooijen DC, van de Kamer JB, Hulshof MC, Koning CC, Bel A. Improving bladder cancer treatment with radiotherapy using separate intensity modulated radiotherapy plans for boost and elective fields. J Med Imaging Radiat Oncol. 2010;54(3):256–63.
Elzayat EA, Al-Zahrani AA. Pelvic lymphadenectomy in the treatment of invasive bladder cancer: literature review. Adv Urol. 2011;2011:701481.
Rajesh A, Sokhi HK, Fung R, Mulcahy KA, Bankart MJ. Bladder cancer: evaluation of staging accuracy using dynamic MRI. Clin Radiol. 2011;66(12):1140–5.
Yoshida S, Koga F, Kobayashi S, Ishii C, Tanaka H, Komai Y, et al. Role of diffusion-weighted magnetic resonance imaging in predicting sensitivity to chemoradiotherapy in muscle-invasive bladder cancer. Int J Radiat Oncol Biol Phys. 2012;83(1):e21–7.
Garcia MM, Gottschalk AR, Brajtbord J, Konety BR, Meng MV, Roach M, et al. Endoscopic gold fiducial marker placement into the bladder wall to optimize radiotherapy targeting for bladder-preserving management of muscle-invasive bladder cancer: feasibility and initial outcomes. PLoS One. 2014;9(3):e89754.
Mangar S, Thompson A, Miles E, Huddart R, Horwich A, Khoo V. A feasibility study of using gold seeds as fiducial markers for bladder localization during radical radiotherapy. Br J Radiol. 2007;80(952):279–83.
Nishioka K, Shimizu S, Shinohara N, Ito YM, Abe T, Maruyama S, et al. Prospective phase II study of image-guided local boost using a real-time tumor-tracking radiotherapy (RTRT) system for locally advanced bladder cancer. Jpn J Clin Oncol. 2014;44(1):28–35.
Foroudi F, Pham D, Rolfo A, Bressel M, Tang CI, Tan A, et al. The outcome of a multi-centre feasibility study of online adaptive radiotherapy for muscle-invasive bladder cancer TROG 10.01 BOLART. Radiother Oncol. 2014;111(2):316–20.
Redpath AT, Wright P, Muren LP. The contribution of on-line correction for rotational organ motion in image-guided radiotherapy of the bladder and prostate. Acta Oncol. 2008;47(7):1367–72.
Foroudi F, Pham D, Bressel M, Wong J, Rolfo A, Roxby P, et al. Bladder cancer radiotherapy margins: a comparison of daily alignment using skin, bone or soft tissue. Clin Oncol (R Coll Radiol). 2012;24(10):673–81.
Huddart RA, Hall E, Hussain SA, Jenkins P, Rawlings C, Tremlett J, et al. Randomized noninferiority trial od reduced high-dose volume versus standard volume radiation therapy for muscle-invasive bladder cancer: results of the BC2001 trial. Int J Radiat Oncol Biol Phys. 2013;87(2):261–9.
Foroudi F, Wilson L, Bressel M, Haworth A, Hornby C, Pham D, et al. A dosimetric comparison of 3D conformal vs intensity modulated vs volumetric arc radiation therapy for muscle invasive bladder cancer. Radiat Oncol. 2012;7:111–4.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DW participated in the care of patients treated on the protocol and drafted the manuscript. HC obtained and analysed key radiotherapy parameters including daily target coverage and plan dosimetry. PM performed the statistical analysis. LG maintains the patient database and coordinated patient follow-up. AK and TE designed the treatment protocol, conceived the study and helped to draft the manuscript. All authors have read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Whalley, D., Caine, H., McCloud, P. et al. Promising results with image guided intensity modulated radiotherapy for muscle invasive bladder cancer. Radiat Oncol 10, 205 (2015). https://doi.org/10.1186/s13014-015-0499-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-015-0499-0