Abstract
Background
Viral encephalitis is a devastating condition for which delayed treatment is associated with increased morbidity and mortality. Clinical audits indicate substantial scope for improved detection and treatment. Improvement strategies should ideally be tailored according to identified needs and barriers to change. The aim of the study is to evaluate the effectiveness and cost-effectiveness of a tailored intervention to improve the secondary care management of suspected encephalitis.
Methods/Design
The study is a two-arm cluster randomised controlled trial with allocation by postgraduate deanery. Participants were identified from 24 hospitals nested within 12 postgraduate deaneries in the United Kingdom (UK). We developed a multifaceted intervention package including core and flexible components with embedded behaviour change techniques selected on the basis of identified needs and barriers to change. The primary outcome will be a composite of the proportion of patients with suspected encephalitis receiving timely and appropriate diagnostic lumbar puncture within 12 h of hospital admission and aciclovir treatment within 6 h. We will gather outcome data pre-intervention and up to 12 months post-intervention from patient records. Statistical analysis at the cluster level will be blind to allocation. An economic evaluation will estimate intervention cost-effectiveness from the health service perspective.
Trial registration
Controlled Trials: ISRCTN06886935.
Similar content being viewed by others
Background
There is evidence that the current clinical management of serious acute neurological infections is suboptimal [1-3]. Encephalitis, inflammation of the brain tissue, is most commonly caused by herpes simplex virus in the United Kingdom (UK) [4,5]. When herpes simplex virus encephalitis is treated promptly with aciclovir, there is a significant improvement in patient outcomes [6,7]. Encephalitis affects between five and eight people per 100,000 per year [8]. Sequelae after hospital discharge can include significant morbidities such as epilepsy, memory loss, and speech and behavioural disorders [9,10], which also impair patients return to work [10].
Whilst herpes simplex virus encephalitis is relatively rare [5], clinical presentations including features consistent with suspected encephalitis occur relatively frequently but in different ways to other brain injuries. Encephalitis typically presents with one or more of headache, fever, new-onset seizures, altered consciousness, and behavioural disturbances [11]. This variable and non-specific presentation often results in delayed diagnosis, especially in children who may only present with fever and irritability [12]. Furthermore, delays in using the main diagnostic technique, lumbar puncture, may further delay treatment [13-16].
Clinical guidelines have been developed in response to these problems [1-3,5,17]. However, simple dissemination of clinical guidelines is often unlikely to bring about significant changes in clinical practice [18-20]. Furthermore, interventions to implement clinical guidelines should ideally be based upon a diagnosis of barriers to change, preferably focusing on those most amenable to change [21].
Aims
We developed a multifaceted intervention package including core and flexible components with embedded behaviour change techniques selected on the basis of identified needs and barriers to change (Backman, submitted). We will evaluate the effectiveness and cost-effectiveness of a tailored intervention to improve the secondary care management of suspected encephalitis.
Methods
Study design
Participating sites will be randomly allocated to intervention or control (no intervention) arms in a cluster randomised controlled trial.
Participants
Hospitals
This trial takes place in the context of ENCEPH UK—Understanding and Improving the Outcome of Encephalitis, an ongoing research programme assessing the epidemiology and clinical outcomes of encephalitis. In order to reduce the likelihood of any unintended co-intervention effects we sought hospitals not directly participating in other ENCEPH UK studies. Sites had to have facilities to perform lumbar punctures and neuroimaging and willing to be randomised to intervention or control arms. We aimed to recruit a range of types of hospital, providing secondary, tertiary, (specialist) and paediatric care, to broadly represent national provision and improve the generalizability of subsequent findings.
We were aware that trainee doctors, one key target intervention group, work and rotate between different hospitals within postgraduate deaneries. If we randomised hospitals to intervention and control arms within the same deanery, there would be a risk of contamination. We therefore used deaneries as the unit of randomisation to minimise contamination.
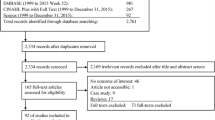
We assessed all 266 acute trusts in England, Wales and Scotland for eligibility (Figure 1 and Additional file 1 detail a full CONSORT checklist). After excluding 47 participating in other ENCEPH UK studies and 10 specialist hospitals not usually providing routine care for suspected encephalitis patients, e.g. orthopaedic hospitals, we invited 209 hospitals to participate via senior medical members of staff.
Patients
We will identify records of patients with features suggestive of suspected encephalitis using three sets of criteria adapted from previous studies [1,22].
Method 1
Mandatory
-
Acute or sub-acute (<4 weeks) alteration in consciousness, cognition, personality or behaviour persisting for more than 24 h. Personality/behaviour change includes: agitation, psychosis, somnolence, insomnia, catatonia, mood liability, altered sleep pattern and (in children) new-onset enuresis or irritability.
Plus any two of:
-
Fever (≥38°C) or prodromal illness—acute or sub-acute
-
New-onset seizures
-
Focal neurological signs of acute or sub-acute onset, including focal weakness, oromotor dysfunction, movement disorders (chorea, athetosis, dystonia, hemiballismus, stereotypies, orolingual dyskinesia and tics) including Parkinsonism (bradykinesia, tremor, rigidity and postural instability) and amnesia
-
Pleocytosis: cerebrospinal fluid white cell count of more than four cells per microlitre
-
Neuroimaging compatible with encephalitis
-
Electroencephalogram (EEG) compatible with encephalitis
Method 2
There was an initial clinical suspicion of encephalitis.
Method 3
There was a clinical suspicion of encephalitis, and the patient died before investigations were completed.
Intervention package
Using theoretically informed semi-structured interviews based upon the Theoretical Domains Framework [23,24], we explored barriers and enablers to diagnosing and managing patients with suspected encephalitis, specifically performing lumbar punctures and initiating antiviral therapy within 6 h (Backman, submitted). We mapped identified barriers and enablers to the patient pathway. We matched behaviour change techniques targeting clinicians to the most salient barriers and enablers and embedded them within an intervention package [25].
The intervention package comprised ‘core’ interventions and, to allow for local flexibility, ‘optional’ interventions (Table 1). We defined ‘core’ interventions as those which we anticipated all hospitals being able to use. These included educational and action planning meetings, feedback of pre-intervention audit data and provision of lumbar puncture kits within refillable boxes. We defined ‘optional’ interventions which hospitals could use depending upon local resources and skills. These included decision support via phone apps and algorithms, an online quiz, prompts and posters, personalised invitation letters to attend educational meetings and a quality improvement cycle pack. Table 1 gives full details of the package following the Template for Intervention Description and Replication (TIDieR) reporting guidance [26].
We presented the package to a 1-day meeting of senior doctors and nurses from intervention hospitals. We emphasised their roles in directly delivering the various intervention components locally and recommended that they each convene an action planning meeting on return to their hospitals.
Outcomes
The primary outcome is a composite measure of the proportion of patients with suspected encephalitis whose care meets both of the following criteria: aciclovir given within 6 h from admission to hospital and a lumbar puncture performed within 12 h of hospital arrival unless clinically contraindicated.
Secondary outcomes comprise:
-
The proportion of all adults started on intravenous aciclovir within an appropriate dosage range for a neurological presentation who met the definition of suspected encephalitis
-
The proportion of all children started on intravenous aciclovir within an appropriate dosage range for a neurological presentation who met the definition of suspected encephalitis
-
The proportion of patients with suspected encephalitis who had a lumbar puncture performed within 12 h unless there was a clinical contraindication
-
The proportion of patients with suspected encephalitis who had a lumbar puncture at any point during the index presentation
-
The proportion of patients with suspected encephalitis who had either magnetic resonance imaging (MRI) or computer tomography (CT) scan within 24 h of admission
-
The proportion of patients with suspected encephalitis having had a lumbar puncture, who had the following cerebrospinal fluid (CSF) investigations performed: ratio of glucose within the cerebrospinal fluid and the serum calculated and having herpes simplex virus polymerase chain reaction (PCR) performed
We will also compare outcomes between adults and children.
Data collection
We recognise that suspected cases would go through one or more of several types of hospital department but mainly paediatrics, neurology, infectious diseases, medical assessment unit, accident and emergency and microbiology. Staff in participating hospitals will identify suspected cases retrospectively by performing two mandatory searches, of discharge codes for encephalitis in the preceding 12 months and of all patients undergoing a lumbar puncture within the same time period. Hospitals can also find eligible patients via records of intravenous aciclovir prescriptions or of orders for cranial CT scan or MRI within the last 12 months. We are using these combined approaches to maximise likelihood of case identification and reduce differences in ascertainment between hospitals. We included both adult and paediatric cases.
Pre-intervention, we collected data to pilot outcome measures and provide data for the feedback intervention. We aimed for 30 adult and paediatric cases per hospital to allow for possible under-recruitment in some of the smaller hospitals; however, we later sought some additional cases from higher recruiting hospitals to better inform exploratory analyses of the baseline data and to compensate for lower recruiting sites. We plan to ask for a further 30 cases per hospital in the final trial data collection, thus the total patient sample size will be a maximum of 720. We anticipate a degree of imbalance between hospitals to achieve the total required sample size, limited by the upper limit of 40 cases per hospital.
Data are collected using structured case review forms. No patient identifiable information is sent to the central trial team. We trained data collectors, mainly nurses and trainee doctors, via face-to-face meetings and/or written briefing materials. We emphasised the need for a systematic approach to case identification to reduce the likelihood of selection bias. The trial research fellow (RB) is monitoring fidelity to the intervention via regular telephone and email contact with relevant hospitals. She is also collecting qualitative data from staff interviews and observational field notes in a sub-sample of four intervention hospitals data as part of a process evaluation.
Sample size
Using pilot data from 315 patients across 26 hospitals in four deaneries, we estimated the standard deviations of the deanery and hospital random effects to be 0.244 and 1.108, respectively, and the current proportion of adherence to the primary outcome to be 5%. Table 2 shows the power of the likelihood ratio test for a significant difference between intervention and control arms as a function of m, the number of eligible patients recruited per hospital, and p, the proportion meeting the primary outcome criteria under the intervention. Using these estimates and based upon a total of 24 hospitals, recruiting 20 patients per hospital should achieve a power of at least 0.8 when the compliance proportion under the intervention is 0.20.
Randomisation
As explained above, we used deaneries as the unit of randomisation to minimise contamination between hospitals within the same deanery. We defined two blocks of deaneries, a block of six including hospitals (outside of the trial) where research teams were already actively involved in other ENCEPH UK studies and a block of six where there were no such ongoing studies (Figure 1). An independent statistician randomised equal numbers of clusters within each block to the intervention and routine arms, blinded to hospital identity.
Statistical analysis
We will analyse the results in R (http://www.r-project.org) using a generalised linear mixed model [28] with binomial errors, logistic link, fixed effects for blocks and treatments, random effects for deanery and for hospital. If the intervention is effective, it will raise awareness of suspected encephalitis and lead to increased documentation in the clinical records of encephalitis as a differential diagnosis. In our baseline (pre-intervention analysis), we found that cases mainly included on this basis (method two) tended to be less likely to comply with the primary outcome criteria. One explanation is that these may represent clinical presentations at lower risk of having encephalitis and may therefore tend to be investigated and treated less thoroughly compared with more strongly suspected cases. It is therefore likely that the intervention will result in differential case mixes between the intervention and control arms, in this scenario diluting any real intervention effect. In our analysis of the outcome data, we will adjust for any relationship between the method of inclusion and compliance with the primary outcomes and analysis will be undertaken by a statistician blind to hospital assignment.
Cost-effectiveness analysis
The economic evaluation will take the perspective of the UK National Health Service (NHS). We will use trial records and observations to estimate the costs of intervention delivery. Data on health care resource utilisation will be gathered from case record reviews. Unit costs will be obtained from publicly available routine data [29,30]. Costs and health benefits occurring over 12 months will be discounted at 3.5% per annum. Therefore, results will include, in addition to incremental costs and benefits, an estimate of total cost per patient for each arm. In order to estimate quality-adjusted life years (QALYs), utility values will be estimated from the results of administering the EQ-5D, primary economic outcome, and the SF-6D utility scores derived from the SF-36, following Brazier’s methodology [31].
We will analyse cost data using regression methods for handling censored cost data and accounting for clustered nature of the data [32]. We will analyse costs and benefits jointly using a bivariate probability distribution. Sample uncertainty in estimated cost difference and incremental cost-effectiveness ratios between arm groups will be described using bootstrapped confidence intervals [33] as well as with cost-effectiveness acceptability curves. Parameter uncertainty and robustness of findings will be accounted for through univariate sensitivity analysis and probabilistic sensitivity analysis.
Estimates of costs and health outcome (utilities) will be used to populate a model of suspected encephalitis patient management in both intervention and control conditions. The model will cover the remaining patient lifetime within which the (probability of) cost-effectiveness of the alternative will be analysed [34]. Data analysis will be performed using Stata [35].
Ethical review
The study was reviewed by Preston North West Research Ethics Committee (13/NW/0279) (Additional file 2).
Trial status
The trial is ongoing with pre-intervention data collection completed; we are yet to undertake post-intervention outcome data collection and analysis.
References
Michael BD, Sidhu M, Stoeter D, Roberts M, Beeching NJ, Bonington A, et al. North West Neurological Infections Network. Acute central nervous system infections in adults—a retrospective cohort study in the NHS North West region. QJM. 2010;103(10):749–58.
Bell DJ, Suckling R, Rothburn MM, Blanchard T, Stoeter D, Michael BD, et al. Management of suspected herpes simplex encephalitis in adults in a U.K. teaching hospital. Clin Med. 2009;9(3):231–5.
Kelly C, Sohal A, Michael BD, Riordan A, Solomon T, Kneen R. Suboptimal management of central nervous system infections in children: a multi-centre retrospective study. BMC Pediatr. 2012;12:145.
Michael BD, Solomon T. Seizures and encephalitis: clinical features, management, and potential pathophysiologic mechanisms. Epilepsia. 2012;53:63–71.
Solomon T, Michael BD, Smith PE, Sanderson F, Davies NWS, Hart I, et al. National Encephalitis Guidelines Developement and Stakeholders Group. Management of suspected viral encephalitis in adults—Association of British Neurologists and British Infection Association National Guidelines. J Infect. 2012;64:347–73.
Hughes PS, Jackson AC. Delays in initiation of acyclovir therapy in herpes simplex encephalitis. Can J Neurol Sci. 2012;39:644–8.
Raschilas F, Wolff M, Delatour F, Chaffaut C, De Broucker T, Chevret S, et al. Outcome of and prognostic factors for herpes simplex encephalitis in adult patients: results of a multicenter study. Clin Infect Dis. 2002;35(3):254–60.
Granerod J, Cousens S, Davies NWS, Crowcroft NS, Thomas SL. New estimates of incidence of encephalitis in England. Emerg Infect Dis. 2013;19(9):1455–62.
McGrath N, Anderson NE, Croxson MC, Powell KF. Herpes simplex encephalitis treated with aciclovir: diagnosis and long term outcome. J Neurol Neurosurg Psychiatry. 1997;63:321–6.
Mailles A, De Broucker T, Costanzo P, Martinez-Almoyna L, Vaillant V, Stahl J-P. Long-term outcome of patients presenting with acute infectious encephalitis of various causes in France. Clin Infect Dis. 2012;54(10):1455–64.
Solomon T, Hart IJ, Beeching NJ. Viral encephalitis: a clinician’s guide. Pract Neurol. 2007;7:288–305.
Kneen R, Jakka S, Mithyantha R, Riordan A, Solomon T. The management of infants and children treated with aciclovir for suspected viral encephalitis. Arch Dis Child. 2010;95:100–6.
Kneen R, Solomon T, Appleton R. The role of lumbar puncture in suspected CNS infection—a disappearing skill? Arch Dis Child. 2002;87(3):181–3.
Hasbun R, Abrahams J, Jekel J, Quagliarello V. Computed tomography of the head before lumbar puncture in adults with suspected meningitis. N Engl J Med. 2001;345(24):1727–33.
Heyderman RS, Lambert HP, O’Sullivan I, Stuart JM, Taylor BL, Wall RA. Early management of suspected bacterial meningitis and meningococcal septicaemia in adults. J Infect. 2003;46:75–7.
Kneen R, Solomon T, Appleton R. The role of lumbar puncture in children with suspected central nervous system infection. BMC Pediatr. 2002;2:8.
Kneen R, Michael BD, Menson E, Mehta B, Easton A, Hemingway C, et al. Management of suspected viral encephalitis in children—Association of British Neurologists and British Paediatric Allergy Immunology and Infection Group National guidelines. J Infect. 2012;64:449–77.
Thomas RH, Smith PE. Encephalitis guidelines: a recipe for success? Clin Med. 2009;9(3):210–1.
Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PAC. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–65.
Gagliardi AR, Brouwers MC, Palda VA, Lemieux-Charles L, Grimshaw JM. How can we improve guideline use? A conceptual framework of implementability. Implement Sci. 2011;6:26.
Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. The Cochrane Database of Systematic Reviews. 2010;3, CD005470. Doi:10.1002/14651858.CD005470.pub2.
Granerod J, Ambrose H, Davies N, Clewley J, Walsh A, Morgan D, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010;10(12):835–44.
Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol. 2008;57(4):660–80.
Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37.
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
Michael B, Geleta D. Development of ClickClinica: a novel smartphone application to generate real-time global disease surveillance and clinical practice data. BMC Med Inform Decis Mak. 2013;13:70.
Breslow NE, Clayton DG. Approximate inference in generalized linear mixed models. J Am Stat Assoc. 1993;88:9–25.
Health Do: Reference costs guidance 2013–14. In. Edited by Health Do; 2014.
Curtis L: PSSRU Unit Costs of Health & Social Care 2013. In. University of Kent (United Kingdom); 2013.
Brazier J, Roberts J, Deveril M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21:271–92.
Grieve R, Cairns J, Thompson SG. Improving costing methods in multicentre economic evaluation: the use of multiple imputation for unit costs. Health Econ. 2010;19(8):939–54.
Chaudhary M, Stearns S. Estimating confidence intervals for cost effectiveness ratios: an example from a randomized trial. Stat Med. 1996;15:1447–58.
Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ. 2001;10:779–87.
StataCorp. Stata statistical software. 9th ed. College Station, TX: StataCorp LP; 2005.
Acknowledgements
This paper summarises the independent research funded by the National Institute for Health Research under its Programme Grants for Applied Research scheme (“Understanding and Improving the Outcomes of Viral Encephalitis”; RP-PG-0108-10048). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Funding
UK National Institute for Health Research (NIHR) Programme for Applied Research: “Understanding and Improving the Outcomes of Viral Encephalitis”; RP-PG-0108-10048.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Robbie Foy is Deputy Editor-in-Chief of Implementation Science. All decisions about this manuscript were made by another editor.
Authors’ contributions
RB wrote the first draft of the protocol and all authors participated in further drafting. PD planned and performed all statistical work and AML planned the health economics. TS and RF conceived the original idea for this study. All authors read and approved the final manuscript.
Additional files
Additional file 1:
CONSORT 2010 checklist of information to include when reporting a cluster randomised trial.
Additional file 2:
Confirmation of ethical approval.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Backman, R., Foy, R., Diggle, P.J. et al. The evaluation of a tailored intervention to improve the management of suspected viral encephalitis: protocol for a cluster randomised controlled trial. Implementation Sci 10, 14 (2015). https://doi.org/10.1186/s13012-014-0201-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13012-014-0201-1