Abstract
Background
This study examined the perceived difficulty of getting help with substance use among sexual and gender minorities who have sex with men (SGMSM) who use methamphetamine during the early COVID-19 period.
Methods
SGMSM, aged 18+, who reported sex with a man and methamphetamine use in the past 6 months were recruited to complete an online survey using online advertisements. Ordinal regression models examined predictors of greater perceived difficulty of getting help. Explanatory variables included participant characteristics (i.e., age, HIV status, ethnicity, sexuality, gender, region, income) and variables assessing patterns of methamphetamine use (i.e., frequency, % time methamphetamine is used alone and during sex; perceived need for help) and patterns of healthcare access (i.e., regular provider, past substance use service utilization).
Results
Of 376 participants, most were gay-identified (76.6%), white (72.3%), cisgender (93.6%), and had annual incomes of less than $60,000 CAD (68.9%). Greater perceived difficulty of getting help was associated with having lower income, sometimes using methamphetamine prior to or during sex, and greater perceived need for help.
Conclusion
Based on these results, we urge greater investments in one-stop, low-barrier, culturally-appropriate care for SGMSM who use methamphetamine. This is especially important given that participants who perceive themselves as needing help to reduce or abstain from substance use perceive the greatest difficulty of getting such help.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
In Canada, less than 1% of the population used methamphetamine in the past year [1], with any lifetime use being approximately 4% [1]. Nonetheless, it is the third most commonly detected drug in illicit drug overdose deaths [2] – suggesting that people who use methamphetamine are in need of harm reduction and treatment services and supports. This is especially true for sexual and gender minority men who have sex with men (SGMSM), among whom the prevalence of methamphetamine is considerably higher. Estimates of methamphetamine use in the SGMSM population range from ten to twenty times greater than the general population [3]. For example, in a Vancouver-based sample of SGMSM recruited using respondent-driven sampling, an estimated 19.0% of participants used methamphetamine in the past 6 months, with 20.8% of those using at least weekly [4].
Two systematic reviews have evaluated the efficacy of methamphetamine treatment programs that aim to support SGMSM in changing methamphetamine use [5, 6]. These reviews highlight several potentially efficacious intervention strategies such as the use of cognitive behavioral, social support (e.g., support groups, social support strengthening), or other therapies [6]. However, the extent to which these interventions can benefit SGMSM is dependent on the person’s readiness to address their substance use, as well as the accessibility of effective supports and services and the ability of these supports and services to address interrelated health and social issues such as mental health problems and internalized homophobia that are strongly linked to substance use [5, 7, 8].
Not all SGMSM want to change their methamphetamine use [9, 10]. Literature examining methamphetamine use among SGMSM highlights its close association with “Party ‘n’ Play” (PnP) culture [11,12,13], which involves illicit drug use, especially methamphetamine, during sexual events. This can also include use of other drugs, such as amyl nitrate/butyrate (“poppers”), erectile drugs, gammahydroxybutyrate (GHB), and ketamine. The social connections that underlie the PnP scene, in addition to the biological drivers of methamphetamine dependence, can make it difficult for users to change their methamphetamine use [14, 15]; however, these social connections may also help individuals identify and access substance use supports and services [10, 16,17,18]. Matsuzaki et al. (2018) reports that people with greater social support have better perceived access to care and fewer barriers [19]. Likewise, membership in other social groups such as different income levels, age, ethnicity, region, education and gender can facilitate (or inhibit) the diffusion of health information (e.g., awareness of interventions) [20,21,22]. Seeing how perceived ability to access care is a common precondition to healthcare seeking and utilization [19, 23, 24], understanding these perceptions among SGMSM is critical to understanding interventions aimed to reduce harms among SGMSM who use methamphetamine.
In view of the importance of understanding the cascade of care for SGMSM who use methamphetamine, the purpose of this analysis was to explore factors associated with SGMSM’s perceived difficulty of getting help reducing or abstaining from substance use.
Methods
Context & Setting
In Canada, access to substance use services is patchwork, varying within and between provinces. This is true regarding both the cost and availability of substance use services. While general health services are covered by provincial health insurance programs, most substance use care falls under specialized programs. Few programs are available specifically tailored to SGMSM. Difficulty getting help was further compounded by the emergence of COVID-19 and associated lock downs in March 2021 – prior to which most of the data for this study were selected. Therefore, the context of COVID-19 must be considered in the interpretation of these findings.
Participant recruitment
Participants were recruited between February 14th, 2020 and June 1st, 2020 using advertisements on geosocial networking applications (i.e., Squirt and Scruff) and social media posts (i.e., Facebook, Twitter, Reddit) shared by our study team and community-based organizations in British Columbia (e.g., Community-based Research Centre) and Ontario (e.g., Gay Men’s Sexual Health Alliance). Eligibility was restricted to men, transmen, and non-binary individuals (i.e. women were ineligible), who (1) were aged 18 years or older, (2) had sex with a man in the past 6 months, (3) used methamphetamine in the past 6 months, and (4) lived in Canada. Immediately before completing the survey online, participants gave informed consent and were screened for eligibility using an online survey. Participants received a $10 honorarium, paid by e-transfer or cheque as compensation for their time, which was approximately 30–45 min. This study was approved by the Research Ethics Board at Research Ethics BC, the University of Victoria, Simon Fraser University, and the University of British Columbia (REB #BC 17–485).
Data collection
Survey development
The online survey was developed using a Community-Based Research approach that aims to address health inequities by engaging people with lived experience. This involved ongoing consultations with the SGMSM community throughout survey development including qualitative interviews with lived experiences with methamphetamine use to inform questionnaire items and structure and pilot testing.
Explanatory variables
Participants provided self-reported demographic information, information about their methamphetamine use, and their perceptions of healthcare access. Participant characteristics considered here included participant’s self-identified/reported age (in years), their ethnicity (which we collapsed into a binary variable representing white vs. non-white (self-reported) participants since most ethnicities were under-represented, creating small cell counts), gender (cisgender; transgender/non-binary), sexual orientation (grouped as gay vs. bisexual/other), self-reported HIV-status (I am HIV-positive; I think I am HIV-negative/I have never been tested for HIV), and province of residence (grouped due to some small cell counts as the Prairies [Alberta, Manitoba, and Saskatchewan], Eastern & Atlantic Canada [Ontario, Quebec, New Brunswick, Newfoundland & Labrador, Nova Scotia, Prince Edward Island]; Western Canada [British Columbia and Yukon Territory]).
Frequency of methamphetamine use was assessed over the previous 6 months (i.e., “Daily or almost daily”, “Weekly,” “Monthly,” “Once or twice,” “Never”). Participants who never used methamphetamine in the past 6 months were excluded from the study based on a priori inclusion criteria. Participants also reported the percent of the time they used methamphetamine prior to or during sex (what we operationalize as “sexualized methamphetamine use”) and the percent of time they used by themselves or alone (“Hardly any [0 - 19%];” “Only some [20 - 39%]”; “About half [40 - 59%];” “Most [60 - 79%];” “Nearly all [80 - 100%]”) over the previous 3 months.
Addressing issues related to healthcare access, participants indicated whether they had a primary healthcare provider, whether that provider knew they used methamphetamine, and whether they had accessed substance use services and supports in the past (“No,” “Yes, in the past 6 months;” “Yes, more than 6 months ago”). One item assessed whether participants felt they needed help with substance use (i.e., “In the past 6 months, to what extent did you feel you needed help in reducing your use of, or abstaining from (not using), substances?”). Responses were recorded on a 4-point ordinal scale ranging from “Completely” (1) to “Not at all” (4).
Outcome variable
The primary outcome of this analyses was a single question asking “At this time, overall, how easy is it for you to get help in reducing your use of, or abstaining from (not using) substances?” Responses were recorded on a 4-point ordinal scale ranging from “Completely” (getting help is completely easy) to “Not at all” (getting help is not at all easy).
Data analysis
Statistical analyses were conducted in R Studio [25]. As a first step, we cleaned the data and excluded participants with any missing responses on the variables of interest. Bivariable differences in included and excluded participants were identified using binary logistic regression. This was done because observations with missing variables would not be included in multivariable models and we felt the demographic, bivariable, and multivariable data should all be analyzed based on the same underlying data. Differences between included and excluded participants were calculated. Descriptive and bivariable statistics were calculated using the CreateTableOne() function in the TableOne package and the polr() function [26].
The Brant test was used to test the proportional odds assumption given the ordinal outcome [27]. This test revealed that the proportional odds assumption held for the relationship with all explanatory variables included in the final model. Nevertheless, the ordinal outcome variable was modeled in two ways as a sensitivity test [27]: First a multivariable ordinal logistic regression model (predicting greater perceived difficulty of getting help) and, second, a binary logistic regression model (predicting “getting help is not at all [easy] vs. completely [easy]). Only variables with a p-value less than 0.20 in bivariate testing – indicating a relationship with our outcome – were included in final models. A comparison model with all variables was initially considered, but had poor statistical characteristics. A p-value of 0.05 was considered statistically significant.
Results
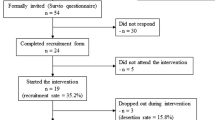
A total of 803 of those consented and were eligible to participate. Figure 1 shows the recruitment timeline, and illustrates that most participants were recruited following the institution of COVID-19 lockdown protocols in early March 2020. Due to high drop-off rates among participants, 376 observations were included in our analytic sample (15.2% dropped off before completing the demographics section [section 1], 33.5% before completing the substance use patterns section [section 2], and 44.5% before completing the healthcare access section [section 3]). Any participant with missing data was excluded from the study. Included and excluded participants did not differ based on age (p = 0.761), ethnicity (p = 0.990), gender (p = 0.822), sexual orientation (p = 0.154), income (p = 0.222), province of residence (p = 0.579), their frequency of methamphetamine use in past 6 months (daily, weekly, monthly, once or twice) (p = 0.059), whether they had ever received treatment/counselling/harm reduction services (p = 0.618), and whether they used methamphetamine before or during sex (0.916). Participants who were excluded were more likely to use methamphetamine ‘alone nearly all of the time’ vs. with others (24.1% vs. 14.1%; p = 0.024).
Table 1 provides a demographic description of the analytic sample. Most participants were white (72.3%), gay (76.6%), cisgender (93.6%), and had annual incomes of less than $60,000 CAD (68.9%). Approximately one-third (33.2%) of participants reported using methamphetamine daily or almost daily and one-third (32.4%) reported using methamphetamine only once or twice in the past 6 months. The remainder reported using methamphetamine weekly (16.8%) or monthly (17.6%). Speaking to the often-sexualized nature of methamphetamine use, three-quarters of participants (76.6%) reported that for at least half of the time they were using methamphetamine, it was prior to or during sex. Half of the sample reported this sexualized context nearly all (80–100%) of the time (See Fig. 2). Greater frequency of methamphetamine use was also associated with a greater proportion of methamphetamine use within a sexual context (p < 0.0001).
In regards to the social nature of methamphetamine use, 39.6% reported that they hardly ever used methamphetamine alone (See Fig. 3). A total of 14.1% reported using methamphetamine alone nearly all of the time and 15.4% reported using alone about half the time. A total of 33.6% of those who reported daily or almost daily use of methamphetamine reported using alone nearly all of the time; however, greater frequency of use was also associated with using alone more frequently (p < 0.0001).
Regarding mode of use in the past 6 months, 40.4% reported snorting methamphetamine and 23.3% reported injecting methamphetamine. Among participants who reported injecting methamphetamine, 21.7% used shared syringes, 27.9% used shared water, 20.9% used shared filters, and 19.4% used shared containers or spoons.
In terms of disclosure of methamphetamine use to a health care provider, 34.0% of the sample had a primary healthcare provider that was aware of their methamphetamine use, 43.4% had a primary healthcare provider who did not know about their use, and 22.6% did not have a primary healthcare provider at all. Among all participants, 6.1% felt they “completely” needed help reducing or abstaining from using substance, 17.6% felt like they needed help “a lot”, 41.8% felt like they needed “a little” help, and 34.6% felt they did “not at all” need help.
Table 2 shows bivariable comparisons for our analysis examining factors associated with perceived difficulty of getting help to reduce or abstain from substances. Greater frequency of methamphetamine use (p = 0.049), more frequent sexualized methamphetamine use (p = 0.003), and greater perceived need for help (p < 0.001) were associated with increased perceived difficulty of getting help. Lower income (p = 0.12) and not having a primary health care provider (p = 0.106) were marginally associated with increased perceived difficulty of getting help – but this association was not statistically significant. Contrary to our expectations, region of residence, past utilization of substance use services, and using methamphetamine alone were not associated with perceived difficulty of getting help to reduce or abstain from using substances.
Table 3 shows multivariable results of our analysis examining factors associated with perceived difficulty of getting help to reduce or abstain from substances. These results showed that greater perceived difficulty of getting help was associated with having lower income, more frequent sexualized methamphetamine use, and greater perceived need for help. Participants perceived it was easier to get help if they had a regular healthcare provider who knew about their methamphetamine use compared with those who had no healthcare provider. Individuals with a healthcare provider who did not know about their methamphetamine use were not statistically more or less likely to perceive greater difficulty of getting help. At the multivariable level, frequency of methamphetamine use in the past 6 months was not significant, though the direction of effects remained.
Discussion
Primary findings
The present study sought to identify whether participant characteristics and patterns of methamphetamine use were associated with perceived difficulty getting help to reduce or abstain from using substances. Most data were collected after lockdowns were instituted across Canada to Control for COVID-19 transmission. Results showed that greater perceived difficulty in getting help to reduce or abstain from using substances during this time was more common among SGMSM with lower incomes, SGMSM who used methamphetamine within the context of sex, SGMSM with greater self-perceived need for help, and SGMSM without a primary care provider. Other demographic factors and previous utilization of substance use services and supports were not statistically associated with perceived difficulty of getting help to reduce or abstain from using substances.
Implications
Each of our findings has important implications for addressing barriers to treatment among SGMSM. First, the finding that SGMSM who perceived a greater need for treatment also perceived a greater difficulty of getting help to reduce or abstain from using substances is highly concerning. It suggests that there are significant barriers among those who are most interested in changing their substance use. Those who have greater perceived need for help may have greater awareness of other barriers that may prevent them from accessing care, such as cost, stigma, and not being ready to stop using [28]. This may be compounded by internal dialogues of shame, guilt or embarrassment [29]. Conversely, those who don’t feel the need to adapt their drug use may not be seeking out support services and thus are unaware of whether or not they are hard to access. There is much room for improvement within the status quo public health and medical systems to better serve those seeking care. This is consistent with the significant amount of literature that highlights barriers to care for people who use drugs [30,31,32,33,34]. This challenge is all the more difficult given lack of consistent treatment guidelines and efficacious treatments for people who use methamphetamine, much less for populations with unique needs such as SGMSM. We recommend the development of consistent treatment guidelines, efficacious treatments, and public health messaging that supports engagement with marginalized populations, such as SGMSM.
Second, our finding that SGMSM who are lower income perceive greater difficulty in getting the help with their substance use echoes research findings examining low-incomes as a barrier to care [35,36,37,38]. Analyzing data from the Canadian Community Health Survey, Slaunwhite (2015) showed that individuals from low-income (<$29,999) households are significantly more likely to report all types of barriers to care [36]. These barriers to care among people living with low-income arise from the general living conditions of having a low-income, the poor quality of interactions with providers, and the complexity of the health system [35]. McCall et al. (2019) developed recommendations based on community-driven work to help address barriers to care for those who use drugs and are socially disadvantaged. These recommendations advocate for culturally sensitive care including engagement of those with lived experiences in care delivery, recognition amongst care providers of the layers of social inequalities individuals face and the importance of fostering an environment of trust, safety and respect (31). Implementing these recommendations alongside increased funding to support interdisciplinary, integrated services can help to reduce these barriers and streamline care (27). Other literature supports the creation of one-stop, low-barrier, integrated care that is culturally sensitive and trauma informed [39,40,41,42,43]. The need for these services is particularly important given the bifurcation of services tailored for SGMSM and other people who use drugs (i.e., SGMSM services may not be culturally safe to people who use methamphetamine and other services tailored for people who use methamphetamine may not be culturally safe to SGMSM [44]).
Third, our finding regarding sexualized methamphetamine use shows that SGMSM who participate in PnP culture face barriers to substance use supports access. Given that sexualized drug use is an important setting for social connectedness and sexual expression, participants may fear loss of social connection with their friends or loss of their sexual subculture and identity if they reduce or quit using methamphetamine [45]. It is important to note that sex is an important way for SGMSM to form social connections and friendships, and that PnP is a setting where this can occur, given the effects that drugs such as methamphetamine have on feelings of pleasure and connectedness [46]. Of course, these benefits do not necessarily negate harms may arise from PnP use. Indeed, we observed that greater frequency of use was associated with more frequent sexualized methamphetamine use. These deterrents in accessing care may be heightened by the stigmatization that exists between SGMSM services towards people who inject drugs (PWID) and vice versa [44]. This territorial stigmatization has been identified as a barrier to accessing healthcare. As a result, SGMSM who use methamphetamine may feel excluded from both services exacerbating inequalities in accessing support. It is essential that services that prioritize support for certain groups (e.g., for PWID or SGMSM) support and engage with each other to increase ease of access. This has implications for how support services are designed and located. Inclusive services that acknowledge the important role that sex plays in social connectedness for the SGMSM community may provide opportunities to address socially produced barriers to care.
Given the prevalence of injection drug use and sharing equipment in this sample harm reduction strategies should focus on providing harm reduction supplies and services for drug use and sexual activity in tandem, such as new needles, snorting kits, gloves, condoms, lubricant, HIV pre-exposure prophylaxis, and Hepatitis C screening. Organizations who provide these supplies and services may also be well placed to provide referrals to support services for reducing drug use. Initiatives that combine harm reduction strategies for both drug use and sexual health have been implemented successfully globally including in the United Kingdom, Germany, and Australia [47, 48]. Modelled after these programs, Canadian organizations such as MAX Ottawa’s campaign Spill the Tea, AIDS Community Care Montreal (ACCM)‘s Kontak program, and The Gay Men’s Sexual Health Alliance of Ontario (GMSH)‘s Party n Play Your Way are a few examples of organizations that are working to utilize peer driven engagement harm reduction strategies that can meet these service gaps.
Finally, we found that SGMSM without a regular primary healthcare provider (relative to those who had a doctor who knew about their methamphetamine use) were more likely to perceive getting help to reduce or abstain from using substances as difficult. Meanwhile, there was no difference between those who had a primary healthcare provider that did not know about their methamphetamine use and those who did not have a primary healthcare provider. Ensuring all people are attached to primary care providers may help ensure they receive referrals to substance use and mental health treatments [49]. Among patients that do have primary care providers, screening, brief interventions, and referrals to treatment can help open dialogues about substance use or patient education on treatment options and how to access the services and supports they want [49]. It is also important to note that patient-provider trust is crucial to ensuring that open dialogue is possible and for SGMSM to feel comfortable disclosing their methamphetamine use [50]. This can be done through proactive inquiry concerning sexual identity, gender identity, sexual behaviour, and routine monitoring of patient experiences, such as proactively asking for consent to discuss patient’s sexual and substance use history. Full-spectrum (e.g., harm reduction and treatment) and integrated care is also needed to support primary-care interventions [6, 51]. This includes services that go beyond traditional harm reduction models – such as supervised consumption sites – which may not be consistent with sexualized drug use. Indeed, given the central importance of social and sexual connection for SGMSM who use methamphetamine, services must allow for these sorts of community oriented interactions to occur without rigid, asexual, and beurocratic barriers to harm reduction. For example, pairing consumption sites with access to sexual health supplies and support services may help to foster a more inclusive and accessible care environment. Identifying and engaging patients who need access to primary care provider could also support substance use care for these individuals.
Strengths and limitations
The present study is limited by its use of an online convenience sample and poor survey completion rates resulting in a modest sample size, however it is still within range of past online survey response and completion rates achieved with SGMSM and illicit drug use populations. Furthermore, our survey was designed prior to the start of COVID-19, however most responses were collected after the COVID-19 pandemic had already caused lockdowns and physical distancing. Further, our survey reached more SGMSM who used methamphetamine than what could be achieved through national surveillance programs, including Canada’s national behavioural surveillance study of SGMSM – The Sex Now Study – and the Canadian Community Health Survey. We also highlight that our recruitment strategy was further strengthened by consultations with the SGMSM community on appropriate and effective recruitment methods. While the survey used in this study has not yet undergone comprehensive psychometric validation, it has strong face and ecological validity. We note that some concepts (e.g., region of residence) could have been measured in ways that would have provided alternative results. For example, measuring rurality and urbanity may produce different results than measuring province/region of residence. As the survey development was informed by community-based methods including consultations with the SGMSM community the questions and structure reflect the sensitivities and attributes of the SGMSM and methamphetamine use context. Due to the self-reported nature of the study, potential response biases may exist, for example as the survey explored topics of drug use and sexual behavior participants may have provided socially desirable responses (e.g., reported less stigmatized use forms of methamphetamine use [52]). That said, given the novelty of this work within this population, our data point to future directions in research that could lead to more rigorous evaluation of the topics explored here. We hope that this work provides a foundational motive to generate higher quality data examining substance use services and support for SGMSM. We also note that the included and excluded participants differed (though not statistically) on important factors, including frequency of methamphetamine use. Efforts are needed to improve response and loss information bias, as the loss of these individuals could be an important factor in shaping statistical significance in bivariable and multivariable models.
Conclusion
Our findings indicate that perceived difficulty of getting help abstaining or quitting from substances is elevated for those who are ready to make these changes, particularly so among those with low incomes, those connected to the PnP community, and those without a primary care provider. These findings highlight connection to care, income and social supports, and referral and linkage services as critical components of the treatment cascade for SGMSM who use methamphetamine. Better integrating health, social, and substance use support services may reduce some of the perceived difficulties of getting help for substance use among SGMSM.
Availability of data and materials
Data and materials for this study available upon request.
Abbreviations
- GHB:
-
gammahydroxybutyrate (GHB)
- SGMSM:
-
Sexual and Gender Minority Men Who Have Sex With Men
- PnP:
-
Party and Play
References
Canadian Tobacco Alcohol and Drugs (CTADS). 2017 supplementary tables [Internet]. Ottawa: Health Canada; 2018. Available from: https://www.canada.ca/en/health-canada/services/canadian-tobacco-alcohol-drugs-survey/2017-summary/2017-detailed-tables.html
British Columbia Coroners Service. Ministry of Public Safety and Solicitor General. In: Illicit drug overdose deaths in BC, January 1, 2008 – May 31, 2018. Burnaby: British Columbia coroners service; 2018.
Cheng B, Sang JM, Cui Z, Bacani N, Armstrong HL, Zhu J, et al. Factors associated with cessation or reduction of methamphetamine use among gay, bisexual, and other men who have sex with men (gbMSM) in Vancouver Canada. Subst Use Misuse. 2020;55(10):1692–701. https://doi.org/10.1080/10826084.2020.1756854.
Card KG, Armstrong HL, Carter A, Cui Z, Wang L, Zhu J, et al. A latent class analysis of substance use and culture among gay, bisexual, and other men who have sex with men. Cult Health Sex. 2018;20(12):1424–39. https://doi.org/10.1080/13691058.2018.1439186.
Rajasingham R, Mimiaga MJ, White JM, Pinkston MM, Baden RP, Mitty JA. A systematic review of behavioral and treatment outcome studies among HIV-infected men who have sex with men who abuse crystal methamphetamine. AIDS Patient Care STDs. 2012;26(1):36–52. https://doi.org/10.1089/apc.2011.0153.
Knight R. Investments in implementation science are needed to address the harms associated with the sexualized use of substances among gay, bisexual and other men who have sex with men. J Int AIDS Soc. 2018;21 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5987811/.
Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12(1):18. https://doi.org/10.1186/1475-9276-12-18.
Abiola T, Udofia O, Sheikh TL, Sanni K. Assessing change readiness and treatment eagerness among psychoactive substance users in northern Nigeria. J Subst Abus Treat. 2015;58:72–7. https://doi.org/10.1016/j.jsat.2015.06.012.
Fawcett DM. Lust, men, and meth: a gay Man’s guide to sex and recovery. La Vergne, Tennessee: Lightning Source Inc; 2015.
Westhaver R. “A Kind of Sorting Out”: Crystal Methamphetamine, Gay Men, and Health Promotion. Sci Technol Hum Values. Sage Publications, Inc. 2011;36:160–89.
Maxwell S, Shahmanesh M, Gafos M. Chemsex behaviours among men who have sex with men: a systematic review of the literature. Int J Drug Policy. 2019;63:74–89. https://doi.org/10.1016/j.drugpo.2018.11.014.
Tomkins A, George R, Kliner M. Sexualised drug taking among men who have sex with men: a systematic review: Perspect Public Health [Internet]. London: SAGE Publications Sage UK; 2018. Available from: https://journals.sagepub.com/doi/10.1177/1757913918778872?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed
Edmundson C, Heinsbroek E, Glass R, Hope V, Mohammed H, White M, et al. Sexualised drug use in the United Kingdom (UK): a review of the literature. Int J Drug Policy. 2018;55:131–48. https://doi.org/10.1016/j.drugpo.2018.02.002.
Harawa NT, Williams JK, Ramamurthi HC, Manago C, Avina S, Jones M. Sexual behavior, sexual identity, and substance abuse among low-income bisexual and non-gay-identifying African American men who have sex with men. Arch Sex Behav. 2008;37(5):748–62. https://doi.org/10.1007/s10508-008-9361-x.
Nakamura N, Semple SJ, Strathdee SA, Patterson TL. Methamphetamine initiation among HIV-positive gay and bisexual men. AIDS Care. 2009;21(9):1176–84. https://doi.org/10.1080/09540120902729999.
Kennedy DP, Osilla KC, Hunter SB, Golinelli D, Maksabedian E, Tucker JS. A pilot test of a motivational interviewing social network intervention to reduce substance use among housing first residents. J Subst Abus Treat. 2018;86:36–44. https://doi.org/10.1016/j.jsat.2017.12.005.
Day E, Copello A, Seddon JL, Christie M, Bamber D, Powell C, et al. Pilot study of a social network intervention for heroin users in opiate substitution treatment: study protocol for a randomized controlled trial. Trials. 2013;14(1):264. https://doi.org/10.1186/1745-6215-14-264.
Des Jarlais DC, Sloboda Z, Friedman SR, Tempalski B, McKnight C, Braine N. Diffusion of the D.A.R.E and Syringe Exchange Programs. Am J Public Health. 2006;96:1354–8.
Matsuzaki M, Vu QM, Gwadz M, Delaney JAC, Kuo I, Trejo MEP, et al. Perceived access and barriers to care among illicit drug users and hazardous drinkers: findings from the seek, test, treat, and retain data harmonization initiative (STTR). BMC Public Health. 2018;18(1):366. https://doi.org/10.1186/s12889-018-5291-2.
Weiss D, Rydland HT, Øversveen E, Jensen MR, Solhaug S, Krokstad S. Innovative technologies and social inequalities in health: A scoping review of the literature. PLoS ONE. 2018;13 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5882163/.
Card KG, Fournier AB, Sorge JT, Morgan J, Grace D, Ham D, et al. Substance use patterns and awareness of biomedical HIV prevention strategies among sexual and gender minority men in Canada. AIDS Care. 2020;32(12):1–9. https://doi.org/10.1080/09540121.2020.1719026.
Bohnert ASB, Bradshaw CP, Latkin CA. A social network perspective on heroin and cocaine use among adults: evidence of bidirectional influences. Addict Abingdon Engl. 2009;104(7):1210–8. https://doi.org/10.1111/j.1360-0443.2009.02615.x.
Kadden RM, Litt MD. The role of self-efficacy in the treatment of substance use disorders. Addict Behav. 2011;36(12):1120–6. https://doi.org/10.1016/j.addbeh.2011.07.032.
Rapp RC, Xu J, Carr CA, Lane DT, Wang J, Carlson R. Treatment barriers identified by substance abusers assessed at a centralized intake unit. J Subst Abus Treat. 2006;30(3):227–35. https://doi.org/10.1016/j.jsat.2006.01.002.
R Core Team. R: A language and environment for statistical computing. 2017. Available from: http://www.R-project.org/
Introduction to tableone [Internet]. [cited 2020 Dec 21]. Available from: https://cran.r-project.org/web/packages/tableone/vignettes/introduction.html
Brant R. Assessing Proportionality in the Proportional Odds Model for Ordinal Logistic Regression. Biometrics. [Wiley Int Biom Soc]. 1990;46:1171–8.
Ali MM, Teich JL, Mutter R. Reasons for not seeking substance use disorder treatment: variations by health insurance coverage. J Behav Health Serv Res. 2017;44(1):63–74. https://doi.org/10.1007/s11414-016-9538-3.
Cumming C, Troeung L, Young JT, Kelty E, Preen DB. Barriers to accessing methamphetamine treatment: a systematic review and meta-analysis. Drug Alcohol Depend. 2016;168:263–73. https://doi.org/10.1016/j.drugalcdep.2016.10.001.
Fante-Coleman T, Jackson-Best F. Barriers and facilitators to accessing mental healthcare in Canada for black youth: a scoping review. Adolesc Res Rev. 2020;5(2):115–36. https://doi.org/10.1007/s40894-020-00133-2.
Ross LE, Vigod S, Wishart J, Waese M, Spence JD, Oliver J, et al. Barriers and facilitators to primary care for people with mental health and/or substance use issues: a qualitative study. BMC Fam Pract. 2015;16(1):135. https://doi.org/10.1186/s12875-015-0353-3.
Russell C, Neufeld M, Sabioni P, Varatharajan T, Ali F, Miles S, et al. Assessing service and treatment needs and barriers of youth who use illicit and non-medical prescription drugs in Northern Ontario, Canada. PLoS ONE Public Libr Sci. 2019;14:e0225548.
Grella C, Ostile E, Scott C, Dennis M, Carnavale J. A scoping review of barriers and facilitators to implementation of medications for treatment of opioid use disorder within the criminal justice system. Int J Drug Policy. 2020;81:102768. https://doi.org/10.1016/j.drugpo.2020.102768.
Priester MA, Browne T, Iachini A, Clone S, DeHart D, Seay KD. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: an integrative literature review. J Subst Abus Treat. 2016;61:47–59. https://doi.org/10.1016/j.jsat.2015.09.006.
Loignon C, Hudon C, Goulet É, Boyer S, De Laat M, Fournier N, et al. Perceived barriers to healthcare for persons living in poverty in Quebec, Canada: the EQUIhealThY project. Int J Equity Health. 2015;14 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4300157/.
Slaunwhite AK. The role of gender and income in predicting barriers to mental health Care in Canada. Commun Ment Health J. 2015;51(5):621–7. https://doi.org/10.1007/s10597-014-9814-8.
Esser-Stuart J, Lyons M. Barriers and influences in seeking health care among lower income minority women. Soc Work Health Care Routledge. 2002;35(3):85–99. https://doi.org/10.1300/J010v35n03_06.
George S, Daniels K, Fioratou E. A qualitative study into the perceived barriers of accessing healthcare among a vulnerable population involved with a community Centre in Romania. Int J Equity Health. 2018;17(1):41. https://doi.org/10.1186/s12939-018-0753-9.
McCall J, Pauly B. Sowing a seed of safety: providing culturally safe Care in Acute Care Settings for people who use drugs. J Ment Health Addict Nurs. 2019;3(1):e1–7. https://doi.org/10.22374/jmhan.v3i1.33.
Treatment (US) C for SA. Trauma-Informed Care: A Sociocultural Perspective. Trauma-Inf Care Behav Health Serv Subst Abuse Mental Health Serv Adm (US). 2014; Available from: https://www.ncbi.nlm.nih.gov/books/NBK207195/.
Ranjbar N, Erb M, Mohammad O, Moreno FA. Trauma-informed care and cultural humility in the mental health Care of People from Minoritized Communities. FOCUS Am Psychiatr Publ. 2020;18(1):8–15. https://doi.org/10.1176/appi.focus.20190027.
Felsenstein DR. Enhancing lesbian, gay, bisexual, and transgender cultural competence in a Midwestern primary care clinic setting. J Nurses Prof Dev. 2018;34(3):142–50. https://doi.org/10.1097/NND.0000000000000450.
Kuzma EK, Pardee M, Darling-Fisher CS. Lesbian, gay, bisexual, and transgender health: creating safe spaces and caring for patients with cultural humility. J Am Assoc Nurse Pract. 2019;31(3):167–74. https://doi.org/10.1097/JXX.0000000000000131.
Collins AB, Parashar S, Closson K, Turje RB, Strike C, McNeil R. Navigating identity, territorial stigma, and HIV care services in Vancouver, Canada: a qualitative study. Health Place. 2016;40:169–77. https://doi.org/10.1016/j.healthplace.2016.06.005.
Smith V, Tasker F. Gay men’s chemsex survival stories. Sex Health. 2018;15(2):116–22. https://doi.org/10.1071/SH17122.
Bryant J, Hopwood M, Dowsett GW, Aggleton P, Holt M, Lea T, et al. The rush to risk when interrogating the relationship between methamphetamine use and sexual practice among gay and bisexual men. Int J Drug Policy. 2018;55:242–8. https://doi.org/10.1016/j.drugpo.2017.12.010.
Stardust Z, Kolstee J, Joksic S, Gray J, Hannan S, Stardust Z, et al. A community-led, harm-reduction approach to chemsex: case study from Australia’s largest gay city. Sex Health CSIRO Publ. 2018;15(2):179–81. https://doi.org/10.1071/SH17145.
Party and play in Canada: What is its impact on gay men’s health? [Internet]. [cited 2021 Jun 1]. Available from: https://www.catie.ca/en/pif/spring-2019/party-and-play-canada-what-its-impact-gay-men-s-health
Ellenberg L. SBIRT with LGBT Patients: Identifying and Addressing Unhealthy Substance Use in Primary Care Settings LGBTQIA+ Health Education Center. Natl LGBTQIA Health Educ Cent. 2015; Available from: https://www.lgbthealtheducation.org/courses/sbirt-with-lgbt-patients-identifying-and-addressing-unhealthy-substance-use-in-primary-care-settings/.
Stults CB, Grov C, Anastos K, Kelvin EA, Patel VV. Characteristics associated with trust in and disclosure of sexual behavior to primary care providers among gay, bisexual, and other men who have sex with men in the United States. LGBT Health. 2020;7(4):208–13. https://doi.org/10.1089/lgbt.2019.0214.
Fisher CB, Fried AL, Macapagal K, Mustanski B. Patient-provider communication barriers and facilitators to HIV and STI preventive Services for Adolescent MSM. AIDS Behav. 2018;22(10):3417–28. https://doi.org/10.1007/s10461-018-2081-x.
Catania JA, Gibson DR, Chitwood DD, Coates TJ. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychol Bull US Am Psychol Assoc. 1990;108(3):339–62. https://doi.org/10.1037/0033-2909.108.3.339.
Acknowledgements
The authors would like to thank the participants and our community partners, including staff at the Community-based Research Centre (CBRC) and the Gay Men’s Sexual Health Alliance (GMSHA).
Funding
This study was funded by the Canadian HIV Trials Network. Dr. Kiffer Card is currently funded bythe Michael Smith Foundation for Health Research Trainee and Scholar Awards, the Canadian Institutes of Health Research Systems Impact Fellowship and the Canadian HIV Trials Network Postdoctoral Fellowship. Dr. Nathan Lachowsky is currently funded by the Michael Smith Foundation for Health Research Scholar Award.
Author information
Authors and Affiliations
Contributions
KGC, KF, GB, MH, and NJL designed this study. KGC conducted analyses and drafted initial manuscript. All authors provided review and edits across multiple rounds of reviews. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Board at Research Ethics BC, the University of Victoria, Simon Fraser University, and the University of British Columbia (REB #BC 17–485). All participants provided informed consent prior to participation.
Consent for publication
All authors provide their consent for publication.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Card, K., McGuire, M., Bond-Gorr, J. et al. Perceived difficulty of getting help to reduce or abstain from substances among sexual and gender minority men who have sex with men (SGMSM) and use methamphetamine during the early period of the COVID-19 pandemic. Subst Abuse Treat Prev Policy 16, 88 (2021). https://doi.org/10.1186/s13011-021-00425-3
Accepted:
Published:
DOI: https://doi.org/10.1186/s13011-021-00425-3