Abstract
Background
The World Health Organization (WHO) recommends exclusive breastfeeding (EBF) in infants for the first 6 months of life. This analysis aims to estimate the proportion of Indian infants exclusively breastfed for the first 6 months using the National Family Health Surveys (NFHS)-4 and 5, and further, determine factors associated with EBF practices.
Methods
EBF for this analysis was defined as when infants received only breast milk and no complementary feeds (solid food, water, animal milk, baby formula, juice, and fortified food) in the last 24 h prior to the survey. The proportion of infants exclusively breastfed was plotted from birth to 6 months as per the age of children at the time of the survey, and this was computed for individual states, union territories, and overall, for India. Univariate and multivariable logistic regression analyses were performed to examine factors influencing EBF in Indian infants.
Results
The proportion of Indian infants exclusively breastfed for 6 months was 31.3% (1280/4095; 95% CI 29.9, 32.7) and 43% (1657/3853; 95% CI 41.4, 44.6) as per the NFHS-4 and 5 surveys, respectively. In NFHS-5, infants of scheduled tribes (aOR 1.5; 95% CI 1.2, 1.9) and mothers who delivered at public health facilities (aOR 1.3; 95% CI 1.1, 1.5) showed an increased odds of being exclusively breastfed at 6 months of life compared to their counterparts. Further, infants of mothers aged < 20 years (aOR 0.5; 95% CI 0.4, 0.7), low birth weight infants (aOR 0.6; 95% CI 0.4, 0.8), and infants in whom breastfeeding was initiated one hour after birth (aOR 0.8; 95% CI 0.7, 0.9) showed a reduced odds of being exclusively breastfed at 6 months compared to their counterparts.
Conclusions
The overall EBF practice showed an increasing trend in the NFHS-5 compared to the NFHS-4 survey. However, a vast gap remains unaddressed in the Indian setting with > 50% of the population still not exclusively breastfeeding their infants for the WHO recommended duration of first 6 months. Behavioral studies dissecting the complex interplay of factors influencing EBF within the heterogenous Indian population can help plan interventions to promote and scale-up EBF in Indian infants.
Similar content being viewed by others
Background
The World Health Organization (WHO) and United Nations International Children’s Emergency Fund (UNICEF) recommend exclusive breastfeeding (EBF) of infants for the first 6 months of life, and further to initiate complementary foods by the same time while continuing breastfeeding up to 2 years of age [1, 2]. EBF as defined by WHO implies that the infant is only on breast milk with no other liquids or solids, not even water, however with the exception of oral rehydration solution (ORS), vitamin syrup or drops, minerals, and medicines [1, 2].
Data from low- and middle-income countries (LMIC) between 2000 and 2019 among children younger than 2 years of age showed that the overall EBF rate increased to 48.6% (41.9–55.2) in 2019 [3]. The analysis also highlighted that EBF increased across all regions of the world except in the middle-east and north African regions [3]. Another analysis of data from 78 LMICs showed that the number of child deaths attributed to sub-optimal breastfeeding was 804,000, implying 11.6% of the total under-5 deaths in 2011 [4]. A pooled analysis from three prospective longitudinal cohorts in Ghana, India, and Tanzania showed that EBF for the first 6 months reduced morbidity and mortality among infants in the first 6 months, with low EBF practice reducing the overall child survival in the first 2 years of life [5].
Meta-analyses have shown that breastfeeding can markedly reduce mortality and morbidity attributed to infectious diseases such as diarrhea and pneumonia, this being critical in developing countries with a background of high infectious diseases burden [6,7,8]. From the maternal health perspective, multiple studies including systematic reviews and meta-analyses have provided evidence on the impact of EBF on maternal health, revealing that breastfeeding for more than 12 months was protective against breast and ovarian cancers, and played a role in preventing diabetes mellitus in the long run [9, 10]. In a review to identify the impact of breastfeeding on short- and long-term infant and maternal health outcomes in high-income settings, it was found that early cessation of breastfeeding or no breastfeeding at all was associated with an increased risk of maternal postpartum depression [11]. EBF has over time demonstrated multiple, holistic benefits for both the mother and baby, and it is thereby pivotal to understand and scale-up strategies to promote EBF for up to 6 months, and further, to promote continued breastfeeding for the first 2 years of life, especially in the LMIC settings [4, 11, 12].
In LMICs, only 37% of infants are exclusively breastfed for the recommended first six months of life [13]. As per the UNICEF, based on Multiple Indicator Cluster Surveys (MICS), Demographic and Health surveys (DHS) and other nationally representative databases (2015–2021), only 48% of the infants aged between 0 and 5 months are exclusively breastfed worldwide with the highest EBF prevalence of 61% being documented in the South Asian region [14]. The sub-Saharan region showed an EBF prevalence of 55% including eastern and southern Africa, 38% in western and central Africa, and 32% in middle-eastern and northern Africa [14]. As per the last three rounds of National Family Health Survey (NFHS) reports, EBF in Indian infants under 6 months of age increased from 46% during 2005-06 to 55% during 2015-16, and further to 65% during 2019-21 [15,16,17]. However, a prospective longitudinal birth cohort with intensive bi-weekly surveillance conducted in urban Vellore in southern India found that the EBF was less than 2% at 6 months of age [18]. Another study which studied pooled data from three longitudinal birth cohorts in south India, between 2002 and 2009, deduced the prevalence of exclusive breastfeeding for the first 6 months as 11.4% [19]. Cohort studies have intensive and multiple rounds of follow-ups, covering the entire first 6 months of infant’s life, thereby giving more accurate estimates on infants exclusively breastfed as compared to cross-sectional surveys [16,17,18,19].
India accounts for about one fifth of the world’s annual births, and is potentially a large market for commercial milk formulas (CMF) [20]. The CMF industry and marketing play a crucial role in EBF practice as CMF is advertised and promoted as a solution to parenting challenges, influencing mothers to formula feed their young infants [21]. Further, CMF advertising and marketing assert that these specialized feeding formulas help alleviate common issues in the infant such as crying, unsettled behaviour, bloating due to gas, and short durations of night sleep [21, 22]. The industry targets vulnerable mothers who self-report insufficient milk, through product endorsements, and when endorsed through healthcare professionals make mothers in believing that CMF is the best option [23]. In urban areas, CMF is readily available and seen as an easy option for mothers struggling with breastfeeding due to a strict or sometimes absent maternity leave policy [23]. Additionally, a lack of family support adds to the challenge in establishing and maintaining breastfeeding, forcing the mother to adopt CMF [24]. However, CMF is not only at a disadvantage for the infant but expensive, especially for low-income families, adding to the financial burden of the family [25].
The NFHS in India is a country-wide, multi-round, cross-sectional survey, and involves data collected from different age groups in a sample of households [16, 17]. The survey covers children aged between 0 and 6 months and are assessed for EBF at the time of the survey [16, 17]. It is important to note that children aged less than 6 months who were on EBF at the time of survey, does not necessarily imply that the child would have been continued on EBF until six months of age, given that there were no further follow-ups to capture this. The lack of this follow-up consequently can lead to a higher estimate on children being exclusively breastfed using the NFHS surveys compared to individual cohort studies where full follow-ups are performed. To overcome this, it is important that an estimate be systematically made on the proportion of children exclusively breastfed as per the data available for each month during the first 6 months of life.
It is critical to understand the socio-demographic and cultural factors that influence exclusive breastfeeding practices for the first 6 months of life in various settings. A systematic review and meta-analysis that summarized evidence from developed countries found that maternal employment, insufficient or lack of breast milk, associated maternal/infant morbidities, lactational difficulties, cultural norms, and maternal body image issues were the barriers associated with low practice of EBF up to 6 months of life [26]. Lack of support from family or the absence of social support systems was also identified as one of the barriers for continuing EBF for 6 months. Further, cultural beliefs such as giving water along with feeds (believed to aid in digestion), influence the sub-optimal practice of EBF for 6 months [26]. Understanding the intricate web of factors associated with EBF practice in the Indian setting will help planning targeted approaches for promoting and scaling up EBF for the recommended first six months. This secondary data analysis aimed to estimate the proportion of Indian infants exclusively breastfed for the first 6 months of life using the NFHS-4 and 5 survey datasets. Further, factors associated with continuing EBF at four, and thereon up to 6 months of age were studied.
Methods
Study setting, design and population
The NFHS survey is a nationally representative cross-sectional survey conducted by the Ministry of Health and Family Welfare (MoHFW), Government of India (GoI), and is coordinated by the International Institute of Population Sciences (IIPS), Mumbai. The nationwide NFHS survey collects household level data, that includes the under-five children, women, and men. In the NFHS-4 survey, 601,509 households in 640 districts, 29 states and 7 union territories in India were surveyed, with a response rate of 98%, and similarly in the NFHS-5 survey, 636,699 households in 707 districts, 28 states and 8 union territories were surveyed, with a response rate of 98%. A two-stage stratified sampling with villages and Census Enumeration Blocks (CEBs) as the primary sampling units (PSU) in the rural and urban areas, respectively, was adopted during the first stage. Within each PSU, the households were selected using systematic random sampling in the second stage. In both the NFHS surveys, all married eligible women at the time of the survey were interviewed. Information was obtained on demographics, socio-economic characteristics, antenatal care, postpartum care, breastfeeding duration and practices [27, 28]. Individual-level data from the NFHS-4 & 5 surveys were used for this analysis. We obtained permission from Demographic and Health survey (DHS) team to access the NFHS-4 (2015-16) and NFHS-5 (2019–2021) datasets. A detailed description of the NFHS survey methodology and sample size has been provided in the NFHS reports [27, 28].
NFHS- 4 and 5 datasets
We accessed the ‘children recode file’ from the DHS program website [29]. We included infants aged between 0 and 6 months to study the proportion distribution of exclusive breastfeeding practices during the first 6 months across the NFHS-4 and 5 surveys. For estimating the EBF practices at each month of age, infants were categorized into age groups: 0–30 days (1 month), 31–60 days (2 months), 61–90 days (3 months), 91–120 days (4 months), 121–150 days (5 months) and 151–180 days (6 months).
Exposure and outcome variables
The exposure variables used in this analysis were broadly divided into three categories: household, maternal and infant characteristics. The household characteristics included religion [Hindu, Muslim, and others (Christian, Sikh, Buddhist/neo-Buddhist, Jain, Jewish, Parsi/Zoroastrian, no religion)]; caste categorized as scheduled caste (SC), scheduled tribe (ST), other backward class (OBC) and others (do not belong to SC/ST/OBC); place of residence (urban/rural); and wealth index (calculated from a standard set of assets held by the household and classified as quintiles, with a quintile of 1–5 representing lowest, lower, middle, higher and highest classes, respectively) [27, 28].
The maternal characteristics included mother’s age in years; number of antenatal visits during the pregnancy for last birth (the ideal number of antenatal visits being at least 4); maternal education [no education, primary (1 to 5 years of schooling), secondary (6 to 12 years of schooling) and higher (> 12 years of schooling)]; type of delivery classified as normal vaginal and caesarean delivery; and place of delivery (home delivery, delivery at a government or private facility). Infant characteristics included gender (male or female); birth order; and birth weight (< 2000 g, 2000 to 2499 g and ≥ 2500 g).
In line with the WHO recommendation of exclusive breastfeeding that the infant should receive only breastmilk for 6 months of life with exception of oral rehydration solution, drops and syrups of vitamins, minerals and medicines, ‘exclusive breastfeeding’ for our analysis was defined as infants who were on only breast milk and not given any other complementary feeds (solid food, water, animal milk, baby formula, juice and fortified food) in the last 24 h prior to the survey [1]. We studied the factors associated with EBF among those who continued EBF for more than 4 months (> 120 days) and more than 5 months (> 150 days), respectively. For this, we compared children aged more than 120 days and still on EBF with those not on EBF by the time they reached 120 days of age. Similarly, we compared children aged more than 150 days and still on EBF with those not on EBF by the time they reached 150 days of age.
Statistical analysis
Analysis was performed using descriptive statistics, univariate, and multivariable logistic regression. The proportion of infants exclusively breastfed was plotted according to age in months. The proportion of infants exclusively breastfed at 6 months of age (151–180 days) was calculated for the individual states as well as union territories, and for India overall. Further, descriptive statistics were performed to compute the proportion of infants exclusively breastfed for > 120 days and > 150 days of age, respectively by household, maternal and infant characteristics. Univariate and multivariable binary logistic regression were performed to examine the factors influencing EBF for > 120 and > 150 days of age. Univariate logistic regression was performed between the binary outcome variable i.e. exclusive breastfeeding (yes, no) and the independent study variables. Further, variables with p-value < 0.25 on univariate analysis were included in multivariable analysis. The multivariable logistic regression included religion, caste, rural or urban setting, wealth index, maternal age, maternal education, number of antenatal visits, mode of delivery, place of delivery, gender of the infant, birth weight and time of breastfeeding initiation following birth. Crude Odds Ratios (cOR) and adjusted Odds Ratio (aOR) with their 95% confidence interval (CI) are reported here. A p-value < 0.05 was considered statistically significant. All the descriptive statistics and analysis are presented here after adjusting for sampling weight, clustering, and strata. STATA version 14.1 (StataCorp LLC, College Station, TX, USA) was used for analysis and adjustment for sampling weight, clustering and strata was done using svyset command.
Results
Of the 259,627 children aged under 5 years in the NHFS-4 survey, 23,918 infants aged between 0 and 6 months at the time of survey were included in the final analysis (weighted N = 22,433). Similarly, for the NHFS-5 survey, of the 232,920 under-five children, 23,678 infants aged between 0 and 6 months were included in the final analysis (weighted N = 23,156) (Fig. 1).
Exclusive breastfeeding practices among Indian infants aged between 0 and 6 months
At 2 months of age, the proportion of infants exclusively breastfed was 66.7% (2268/3401; 95% CI 65.1, 68.3) during the NFHS-4 survey that increased to 70.4% (2770/3938; 95% CI 68.9, 71.8) during the NFHS-5 survey. At 4 months of age, the EBF proportion was 61.5% (2443/3972, 95% CI 60, 63) during the NFHS-5 survey which was higher when compared to the NFHS-4 survey at 50.2% (1958/3904; 95% CI 48.6, 51.7). At 6 months of age, the proportion of infants exclusively breastfed was again higher during the NFHS-5 survey with 43% (1657/3853; 95% CI 41.4, 44.6) infants being exclusively breastfed when compared to 31.3% (1280/4095; 95% CI 29.9, 32.7) during the NFHS-4 survey (Fig. 2 and Supplementary Table 1).
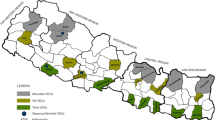
Exclusive breastfeeding practices at 6 months among different states and union territories of India as per the NFHS-4 and NFHS-5 surveys
As per the NFHS-5 survey, EBF practices in Chhattisgarh (71%), Haryana (69.5%), and Jharkhand (61.7%) were higher when compared to the overall proportion of 43% for India, while the practice was lower in Meghalaya (23%), Manipur (24.5%), West Bengal (25.4%) and Uttarakhand (25.5%). In the NHFS-4 survey, EBF practices in Tripura (58.5%), Chhattisgarh (47.2%) and Himachal Pradesh (43.4%) were higher compared to the overall EBF practice of 31.3% for India, with the same being lower for Meghalaya (15.1%), Sikkim (17.5%), Karnataka (22.9%), and Uttar Pradesh (23.4%) (Fig. 3 and Supplementary Table 2).
Exclusive breastfeeding practices among Indian infants at 6 months in relation to baseline characteristics
The baseline characteristics of exclusively breastfed infants for </> 120 days and </> 150 days are depicted in Table 1. EBF practices were higher among Hindu mothers with 20.7% exclusively breastfeeding their infants as per the NFHS-5 survey which increased from 14.6% during the NFHS-4 survey. The NFHS-5 survey showed that EBF practices among mothers with ≥ 4 antenatal visits during pregnancy was higher (21.8%) when compared to those with < 4 antenatal visits (18.9%) or no visits (14.9%). Further, the EBF practices as per the NFHS-5 survey among mothers who delivered at a public healthcare (government) facility was higher (22.2%) compared to those who delivered at a private healthcare facility (16.7%) or at home (14.5%). The EBF practices during the NFHS-5 survey were similar for both male (19.6%) and female (20%) infants whereas in the NFHS-4 survey it was higher among male (15.4%) when compared to female (12.6%) infants. EBF practices at 6 months were higher among mothers who breastfed immediately after birth (25.1%) when compared to those who breastfed within (22.6%) and after one hour of birth (18.1%) as per the NFHS-5 survey. EBF practices at 6 months were higher among children immediately breastfed after birth in NFHS-5 survey (50.3%) compared to NFHS-4 survey (25.1%) (Table 1).
Factors affecting exclusive breastfeeding practices at 6 months among Indian infants as per NFHS-4 and 5 surveys
In the NFHS-5 survey, infants belonging to schedule caste (aOR 1.2; 95% CI 1, 1.5), schedule tribe (aOR 1.5; 95% CI 1.2, 1.9), or other backward classes (aOR 1.3; 95% CI 1.1, 1.5) were at an increased odds of being exclusively breastfed for 6 months compared to those belonging to other categories. In the NFHS-5 survey, infants belonging to Muslim (aOR 0.8; 95% CI 0.6, 0.9) or Christian religion (aOR 0.5; 95% CI 0.4, 0.6) had a decreased odds of being exclusively breastfed for 6 months compared to those from Hindu religion. Infants of mothers aged < 20 years (aOR 0.5; 95% CI 0.4, 0.7) were at a decreased odds of being exclusively breastfed at 6 months compared to mothers aged between 25 and 31 years. Also, the NFHS-5 survey showed that infants whose mothers delivered at a public (government) healthcare facility (aOR 1.3; 95% CI 1.1, 1.5) were more likely to exclusively breastfeed their infants for 6 months compared those mothers who delivered at a private healthcare facility. Low birth weight infants (< 2000 g) (aOR 0.6; 95% CI 0.4, 0.8) and infants with birth order ≥ 3 (aOR 0.7; 95% CI 0.6, 0.8) were at a decreased odds of being exclusively breastfed for 6 months compared to their counterparts. Further, infants of mothers who breastfed after one hour of birth (aOR 0.8; 95% CI 0.7, 0.9) were at decreased odds of continuing EBF for upto 6 months when compared to those who were breastfed immediately after birth. In the NFHS-4 survey, infants from rural areas (aOR 1.3; 95% CI 1.1, 1.6), showed an increased odds of being exclusively breastfed for 6 months compared to those from urban areas whereas no such difference was noted in the NFHS-5 survey (Table 2).
Discussion
The present analysis that was performed to understand exclusive breastfeeding practices among Indian mothers using the nationally representative NFHS-4 and 5 surveys. The proportion of Indian infants exclusively breastfed for 6 months showed an increase from 31.3% during the NFHS-4 (2015-16) survey to 43% in the NFHS-5 (2019–2021) survey as per the definitions used in this analysis. The mothers from the scheduled tribe community, delivering at public health facilities, and having had ≥ 4 antenatal visits during pregnancy showed an increased odds of exclusively breastfeeding their infants for upto 6 months. Younger mothers (< 24 years), low birth weight infants (< 2000 g), higher birth order (≥ 3), and initiation of breastfeeding more than one hour following birth were associated with a reduced odds of being exclusively breastfed for upto 6 months of life. Place of residence (rural or urban), wealth index and infant gender played no role in influencing exclusive breastfeeding for 6 months.
Comparison of exclusive breastfeeding practices in Indian infants with other settings
Our analysis showed that 31.3% and 43% of Indian infants from the NFHS-4 and 5 surveys, respectively, were exclusively breastfed for up to 6 months of age (151–180 days) which is low when compared to the reported national prevalence for India of 54.9% and 63.7%, respectively (as per the NFHS-4 and 5) survey reports [16, 17]. The reasons for this lower prevalence estimates in our analysis can be explained by the fact that for estimating EBF practices at 6 months of age, we included only age-appropriate children, that is children aged between 151 and 180 days at the time of the survey.
Our analysis estimates are lower than estimates from other cross-sectional studies conducted across India that have reported EBF percentages for up to 6 months as ~ 50% [30, 31]. Our analysis showed that EBF was 61.5% and 43% at four and 6 months of age, respectively (NFHS-5 survey). This finding is similar to the study from the neighboring country of Sri Lanka where EBF at 4 months was higher (62%) when compared to 6 months (16%) [32]. It is to be reiterated that NFHS surveys are based on maternal recall. In a study by Andarge et al. which assessed recall period accuracies found that one week recall period gave a more accurate estimate of exclusive breastfeeding practice than a 24-hour recall among infants younger than 6 months of age. This study by Andarge et al. found that the EBF was estimated at 71% from a single 24-hour recall, an overestimate when compared to 47% EBF computed from repeated weekly surveillance [33]. Given that the NFHS surveys for breastfeeding are based on a 24-hour recall, EBF at six months of age in our analysis was estimated at 43% which is very high compared to EBF of 2% from a longitudinal birth cohort study with bi-weekly surveillance [18].
Factors affecting exclusive breastfeeding practices at six months of age in Indian infants
The present analysis showed that the differences in EBF practices based on the infant’s gender at 6 months of age was statistically significant in the NFHS-4 data but did not hold true for the NFHS-5 data. This result is consistent with an urban cohort study conducted in Vellore, southern India [18, 19]. This is a notable and encouraging finding that gender disparities that existed in the past may have narrowed now in the Indian setting. EBF practice among scheduled tribes is known to be high, and this is substantiated by the present analysis [34]. The majority of scheduled tribes belong to low socioeconomic background, and the reason for the high rate of exclusive breastfeeding in this population could be attributed to the reduced financial access to breastfeeding substitutes or formula foods [34]. It is interesting to note that EBF practices as per the NFHS-5 survey were significantly higher among mothers who delivered at public healthcare facilities when compared to those who delivered at private healthcare facilities or at home. This clearly indicates an improved and expanded access to maternal/breastfeeding counselling and care at public health facilities that are providing early education and motivation to mothers, perhaps becoming pivotal in sustaining continued EBF for up to 6 months of age [35, 36]. Also, there is a possibility that mothers who deliver at public health facilities cannot afford breastmilk substitutes compared to those delivering at private health facilities. The NFHS-5 data further has highlighted that a higher number of antenatal visits during pregnancy (≥ 4) implied a greater chance of the mothers going on to exclusively breastfeed their infants for up to 6 months suggesting that healthcare workers (anganwadi workers/peripheral health nurses/doctors) during antenatal visits and follow-ups are playing a key role in educating and encouraging the mothers-to-be about the benefits of EBF along with support through other maternal healthcare programs and postnatal care facilities provided by the government [36,37,38].
Young mothers (< 24 years) seemed to less likely breastfeed their infants exclusively up to 6 months. This can perhaps be attributed to the lack of awareness about the benefits and misconceptions regarding EBF [39,40,41]. The same was seen with infants born with lower birth weight perhaps explained by the fact that these are high-risk infants requiring nursery care and support, delaying the initiation and continuation of EBF, and possibly put on formula feeds during and after nursery care [39,40,41]. According to the NFHS-5 data, the higher the birth order, lower was the EBF practice for up to 6 months. This can possibly be explained by the fact that an increased family size demands the mother getting back to household chores early or work to avoid loss of wages, and thereby being unable to exclusively breastfeed her infant for the recommended 6 months due to greater and conflicting demands.
The Infant Milk Substitutes, Feeding Bottles and Infant Foods (Regulation of Production, Supply and Distribution) act, 1992 as amended in 2003 (IMS act) aligns with the objectives of the International Code of Marketing of Breastmilk Substitutes [42]. The IMS act has played a crucial role in India in controlling the promotion and advertisement of CMFs. The act prohibits pregnant women or mothers being contacted directly for the purpose of promoting infant milk substitutes or infant foods [43]. Additionally, it provides recommendations for healthcare workers on how measures could be taken to prevent being influenced by baby food manufacturing companies [43]. Notably, India is one of the few countries in Asia to implement the guideline fully and has ensured that breastfeeding is strictly not undermined by the marketing of breastmilk substitutes [44]. In addition to protecting breastfeeding practices from being influenced or impacted by commercial promotion of CMFs, the IMS Act also regulates the marketing practices of baby food manufacturers [43]. Also, the implementation of the IMS Act by the Breastfeeding Promotion Network of India (BPNI) in 49 districts has helped improving EBF rates [45]. During the last 10 years (2010–2020), breastfeeding in India has increased by 5% as a result of the IMS Act, Maternity Benefits Act (adopted in 2017 to extend paid maternity leave for upto 26 weeks), and the government’s ‘Mother’s Absolute Affection’ campaign that promotes breastfeeding through counselling [46].
Strengths, limitations and recommendations
This analysis that used the extensive, nationally representative NFHS-4 and 5 survey datasets covering all states and union territories of India, allowed the comparison of changes over time in EBF practices, and further to deduce factors influencing EBF, and this is the major strength of the study. In this study only eligible children who belonged to appropriate age groups were considered for analyzing the prevalence of exclusive breast feeding. However, a few limitations must be considered when interpreting the results of this analysis. In cross sectional surveys like these, estimates of EBF are based on maternal recall and this recall bias could potentially overestimate the prevalence of EBF practices reported. Despite these inherent limitations, there is overwhelming evidence that the NFHS surveys have provided valuable information on key population and health issues and have been instrumental in building India’s decision-making capacity and policies on health [17]. It is to be noted that NFHS data are collected by intensively trained staff, and the NFHS-4 and 5 surveys have a high response rate [17].
Qualitative studies to understand the driving factors among populations that have shown high exclusive breastfeeding rates such as among mothers from scheduled tribes and those who delivered at public healthcare facilities will help throw light to scale up the same amongst mothers of low birthweight babies in other Indian settings and backgrounds. Interventions and support targeted towards young mothers, mothers with low birth weight babies, and strongly encouraging mothers to initiate breastfeeding immediately after birth are some of the premises to be worked upon to enhance exclusive breastfeeding rates for up to 6 months in the Indian setting.
Conclusion
Our analysis found that exclusive breastfeeding practices in the Indian setting was higher in the NFHS-5 survey when compared to NFHS-4 survey from birth to 6 months. The practices of EBF at 6 months was seen to be better among mothers from scheduled tribes, those who delivered at public healthcare facilities and those with adequate number of antenatal visits during pregnancy. EBF for 6 months was low among young mothers, those with low-birth-weight infants, higher birth order, and mothers who initiated breastfeeding after one hour of birth. An enhanced focus on promoting EBF practices by targeting special groups identified from this analysis through the existing maternal and child national health programmes such as Janani shishu suraksha Karyakram (JSSK), home-based newborn care (HBNC), and home-based care of young child (HBYC) must be meticulously harnessed to improve exclusive breastfeeding rates for up to 6 months. Added to this, qualitative studies to understand the intricate and complex driving factors associated with exclusive breastfeeding practices in the Indian setting could be pivotal in scaling up the same across all settings in India.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study. The NFHS-4 and 5 datasets are available on the DHS platform: https://dhsprogram.com/data/.
Abbreviations
- aOR:
-
Adjusted Odds Ratio
- cOR:
-
Crude Odds Ratio
- CI:
-
Confidence Interval
- CMF:
-
Commercial Milk Formula
- DHS:
-
Demographic and Health surveys
- EBF:
-
Exclusive Breastfeeding
- GOI:
-
Government of India
- IIPS:
-
International Institute of Population Sciences
- LMIC:
-
Low–and Middle–income countries
- MICS:
-
Multiple Indicator Cluster Surveys
- NFHS:
-
National Family Health Survey
- PHC:
-
Primary Health Centre
- WHO:
-
World Health Organization
References
Exclusive breastfeeding for six months best for babies everywhere. https://www.who.int/news/item/15-01-2011-exclusive-breastfeeding-for-six-months-best-for-babies-everywhere. Accessed 21 Mar 2023.
Complementary feeding. https://www.who.int/health-topics/complementary-feeding. Accessed 21 Mar 2023.
Neves PAR, Vaz JS, Maia FS, Baker P, Gatica-Domínguez G, Piwoz E, et al. Rates and time trends in the consumption of breastmilk, formula, and animal milk by children younger than 2 years from 2000 to 2019: analysis of 113 countries. Lancet Child Adolesc Health. 2021;5:619–30.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51.
NEOVITA Study Group. Timing of initiation, patterns of breastfeeding, and infant survival: prospective analysis of pooled data from three randomised trials. Lancet Glob Health. 2016;4:e266-275.
Effect of breastfeeding on. Infant and child mortality due to infectious Diseases in less developed countries: a pooled analysis. WHO Collaborative Study Team on the role of breastfeeding on the Prevention of Infant Mortality. Lancet Lond Engl. 2000;355:451–5.
Lamberti LM, Fischer Walker CL, Noiman A, Victora C, Black RE. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Public Health. 2011;11:15.
Lamberti LM, Zakarija-Grković I, Fischer Walker CL, Theodoratou E, Nair H, Campbell H, et al. Breastfeeding for reducing the risk of Pneumonia morbidity and mortality in children under two: a systematic literature review and meta-analysis. BMC Public Health. 2013;13(Suppl 3):18.
Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, Rollins N, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr Oslo Nor 1992. 2015;104:96–113.
Gunderson EP. Breast-feeding and Diabetes: long-term impact on mothers and their infants. Curr Diab Rep. 2008;8:279–86.
Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid ReportTechnology Assess. 2007;(153):1–186.
Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev. 2012;2012:CD003517.
Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet Lond Engl. 2016;387:475–90.
Breastfeeding, UNICEF DATA. https://data.unicef.org/topic/nutrition/breastfeeding/. Accessed 21 Mar 2023.
IIPS. National Family Health Survey – 3 India Report. 2015. http://rchiips.org/nfhs/NFHS-3%20Data/VOL-1/India_volume_I_corrected_17oct08.pdf. Accessed 21 Mar 2023.
IIPS. National Family Health Survey – 4 India Report. 2015. http://rchiips.org/nfhs/NFHS-4Reports/India.pdf. Accessed 21 Mar 2023.
IIPS. National Family Health Survey-5 India Report. 2019. https://dhsprogram.com/pubs/pdf/FR375/FR375.pdf Accessed 21 Mar 2023.
Reddy NS, Sindhu KN, Ramanujam K, Bose A, Kang G, Mohan VR. Exclusive breastfeeding practices in an urban settlement of Vellore, southern India: findings from the MAL-ED birth cohort. Int Breastfeed J. 2019;14:29.
Velusamy V, Premkumar PS, Kang G. Exclusive breastfeeding practices among mothers in urban slum settlements: pooled analysis from three prospective birth cohort studies in South India. Int Breastfeed J. 2017;12:35.
Rana K. Breastfeeding and the role of the commercial milk formula industry. Lancet Lond Engl. 2023;402:446.
Rollins N, Piwoz E, Baker P, Kingston G, Mabaso KM, McCoy D, et al. Marketing of commercial milk formula: a system to capture parents, communities, science, and policy. Lancet Lond Engl. 2023;401:486–502.
Baker P, Smith JP, Garde A, Grummer-Strawn LM, Wood B, Sen G, et al. The political economy of infant and young child feeding: confronting corporate power, overcoming structural barriers, and accelerating progress. Lancet Lond Engl. 2023;401:503–24.
Pérez-Escamilla R, Tomori C, Hernández-Cordero S, Baker P, Barros AJD, Bégin F, et al. Breastfeeding: crucially important, but increasingly challenged in a market-driven world. Lancet Lond Engl. 2023;401:472–85.
Gavine A, Shinwell SC, Buchanan P, Farre A, Wade A, Lynn F, et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev. 2022;10:CD001141.
Barennes H, Slesak G, Goyet S, Aaron P, Srour LM. Enforcing the international code of marketing of breast-milk substitutes for better promotion of exclusive breastfeeding: can lessons be learned? J Hum Lact. 2016;32:20–7.
Balogun OO, Dagvadorj A, Anigo KM, Ota E, Sasaki S. Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review. Matern Child Nutr. 2015;11:433–51.
IIPS. National Health Survey-4 India Interviewer’s Manual. 2019. http://rchiips.org/NFHS/NFHS4/manual/NFHS-4%20Interviewer%20Manual.pdf. Accessed 21 Mar 2023.
IIPS. National Health Survey-5 India Interviewer’s Manual. 2019. http://rchiips.org/NFHS/NFHS5/manuals/NFHS-5%20Interviewer%20Manual_Eng.pdf. Accessed 21 Mar 2023.
The DHS Program - Data. https://dhsprogram.com/data/. Accessed 21 Mar 2023.
Nishimura H, Krupp K, Gowda S, Srinivas V, Arun A, Madhivanan P. Determinants of exclusive breastfeeding in rural South India. Int Breastfeed J. 2018;13:40.
Veeranki SP, Nishimura H, Krupp K, Gowda S, Arun A, Madhivanan P. Suboptimal breastfeeding practices among women in rural and low-resource settings: a study of women in rural Mysore, India. Ann Glob Health. 2017;83:577–83.
Agampodi SB, Agampodi TC, Piyaseeli UKD. Breastfeeding practices in a public health field practice area in Sri Lanka: a survival analysis. Int Breastfeed J. 2007;2: 13.
Andarge SD, Fenta EH, Gebreyesus SH, Belachew RY. One-week recall period gives a more accurate estimate of exclusive breastfeeding practice than 24-h recall among infants younger than six months of age. Int Breastfeed J. 2021;16:65.
Sarkar D, Dalai CK, Sarkar K, Das SS, Banerjee S. Breastfeeding practices and infant feeding pattern of a tribal population region of Eastern India. J Fam Med Prim Care. 2020;9:4570–5.
Aguayo VM, Gupta G, Singh G, Kumar R. Early initiation of breast feeding on the rise in India. BMJ Glob Health. 2016;1:e000043.
Ministry of Women and Child Development. Pradhan Mantri Matru Vandana Yojana (PMMVY). Government of India. https://pmmvy.wcd.gov.in/. Accessed 21 Mar 2023.
Ministry of Health and Family Welfare. Janani Suraksha Yojana (JSY). Government of India. ; 2023. https://nhm.gov.in/index1.php?lang=1&level=3&lid=309&sublinkid=841. Accessed 21 Mar 2023.
Ministry of Health and Family Welfare. Janani-Shishu Suraksha Karyakram(JSSK). Government of India; 2023. https://nhm.gov.in/index1.php?lang=1&level=3&sublinkid=842&lid=308. Accessed 21 Mar 2023.
Harding KL, Aguayo VM, Webb P. Birthweight and feeding practices are associated with child growth outcomes in South Asia. Matern Child Nutr. 2018;14: e12650.
Sinha B, Sommerfelt H, Ashorn P, Mazumder S, Taneja S, Bahl R, et al. Effect of community-initiated kangaroo mother care on breastfeeding performance in low birthweight infants: a randomized clinical trial. Matern Child Nutr. 2022;18:e13419.
Vesel L, Bellad RM, Manji K, Saidi F, Velasquez E, Sudfeld CR, et al. Feeding practices and growth patterns of moderately low birthweight infants in resource-limited settings: results from a multisite, longitudinal observational study. BMJ Open. 2023;13:e067316.
Arun G, YP G. Status of infant and young child feeding in 49 Districts (98 Blocks) of India 2003. Breastfeeding Promotion Network of India; 2004. https://www.bpni.org/report/statusofiycf.pdf. Accessed 21 Mar 2023.
Government of India. The infant milk substitutes, feeding bottles and infant foods (Regulation of production, supply and distribution) act,1992. https://www.indiacode.nic.in/bitstream/123456789/1958/1/199241.pdf. Accessed 21 Mar 2023.
World Health Organization. Country implementation of the international code of marketing of breast-milk substitutes: status report. 2011. https://apps.who.int/iris/bitstream/handle/10665/85621/9789241505987_eng.pdf. Accessed 21 Mar 2023.
National Policy & Programme - BPNI. Breastfeed. Promot. Netw. India - BPNI. https://www.bpni.org/national-policy-programme-4/. Accessed 21 Mar 2023.
Bhatt N. Breastfeeding in India is disrupted as mothers and babies are separated in the pandemic. BMJ. 2020;370:m3316.
Acknowledgements
We acknowledge the contributions of all the survey participants and staff of the NFHS- 4 and 5 surveys without whose commitment and enthusiasm, this precious dataset would have not been made possible, making this important analysis impossible. We would like to sincerely thank DHS for providing us access to the NFHS-4 and 5 datasets.
Funding
This analysis was supported by a funding from Grand Challenges India – ‘Knowledge integration (ki) data challenge for Maternal and Child health’ jointly funded by Department of Biotechnology (DBT), Ministry of Science and Technology, Government of India, and Bill & Melinda Gates Foundation (BMGF) (BT/kiData0393/06/18).
Author information
Authors and Affiliations
Contributions
KNS and SSR conceived the idea, provided critical inputs for analysis, reviewed, and finalised the manuscript. AD and SSR performed the statistical analysis. SSR, JJ, and AD wrote the first draft. All authors read and approved the final draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Reddy N, S., Dharmaraj, A., Jacob, J. et al. Exclusive breastfeeding practices and its determinants in Indian infants: findings from the National Family Health Surveys-4 and 5. Int Breastfeed J 18, 69 (2023). https://doi.org/10.1186/s13006-023-00602-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13006-023-00602-z