Abstract
Background
The health workers in Jiaxing of China have established maternal health WeChat groups for maternal health education and management since 2019. Pregnant women in Jiaxing are invited to join the WeChat groups and a health worker as the group manager provides health education and individual counselling for women within the group. This study aimed to investigate the exclusive breastfeeding (EBF) status up to six months and its associated factors among the mothers of infants aged 7-12 months within the WeChat groups.
Methods
This was a cross-sectional survey on healthy mothers with infants aged 7-12 months from seven maternal health WeChat groups in October 2021 in Jiaxing, China. EBF was defined as breastfeeding infants exclusively up to six months. Data including breastfeeding practice from birth to six months, maternal sociodemographic and obstetric characteristics, hospitalization information, work related factors and reasons for non-EBF up to six months were collected using an online self-administered questionnaire. A multivariable logistic regression analysis was performed to identify the factors independently associated with EBF up to 6 months.
Results
A total of 822 mothers were included in this study. Among them, 586 mothers (71.3%) exclusively breastfed infants up to six months. Multivariable logistic regression analysis showed that older maternal age (adjusted odds ratio [AOR] 0.956; 95% confidence interval [CI] 0.917, 0.997) and perceived insufficient breast milk (AOR 0.104; 95% CI 0.072, 0.149) were associated with lower odds of EBF up to six months. The five of common reasons for non-EBF up to six months were no or insufficient breast milk (59.8%), return to work (23.9%), no flexible nursing breaks at work (18.2 %), infant crying or feeling tired or troubled with breastfeeding (9.7%), and nipple and breast problems (9.3%).
Conclusion
About 71.3% of infants were exclusively breastfed until six months of age in our WeChat groups. Perceived insufficient breast milk and work related factors are the main barriers to EBF up to six months in this setting. However, further comparative study is needed to confirm the effect of WeChat groups on breastfeeding.
Similar content being viewed by others
Background
World Health Organization (WHO) has set one of the global nutrition target as increasing the exclusive breastfeeding (EBF) rates up to 50% by 2025 [1]. In China, the EBF rates, as the measurement of exclusively breastfeeding infants under six months during the past 24 hours, were 20.7% in 2013 [2] and 29.5% in 2018 [3] as estimated by the nationally representative surveys. Hence, how to improve EBF rates has become one of the main challenges for public health care in China. There are many factors that can affect breastfeeding, including historical, socioeconomic, cultural, and individual factors; among them, health education and support provided by health professionals play an important role in breastfeeding outcomes [4,5,6,7,8,9].
WeChat, the most widely used mobile communication application in mainland China, supports one-on-one texting, group chats, multimedia sharing and more. To improve maternal health education and management, the health workers in Jiaxing, a relatively developed medium-sized city on the east coast of China, have established dedicated maternal health WeChat groups as part of traditional maternal health care since 2019. Jiaxing consists of five counties and two districts with a population of 5 400 868 and 37 366 births in 2020. Pregnant women in Jiaxing area are invited to join the WeChat groups on a voluntary basis when they attend the first antenatal clinics (about 4 months prenatal). Currently, each county and district in Jiaxing has established its own maternal health WeChat group, leading to a total of seven WeChat groups with women accounting for about 15% of the overall pregnant women in Jiaxing area. Each WeChat group has approximately 200-500 women covering the period from about 4 months prenatal to at least 12 months after birth, and a health worker as the group manager who provides weekly group education and individual counselling at any time on maternal health care including breastfeeding education and support. Also women within the group can share their breastfeeding experiences with each other through text and/or audio messages, as this is one of the WeChat group functions and encouraged by the group managers. The aim of this cross-sectional study was to investigate the prevalence of EBF from birth to six months among the mothers of infants aged 7-12 months within our seven maternal health WeChat groups. Additionally, the related factors potentially affecting EBF up to six months in this setting were also assessed.
Methods
Study design
This is a cross-sectional study which was conducted using an online self-administered questionnaire in October 2021 in Jiaxing, Zhejiang province, China. The inclusion criteria were healthy mothers with infants aged 7-12 months in our seven maternal health WeChat groups. The exclusion criteria were multiple gestations, premature delivery before 34 weeks, mastitis or prior breast surgery, major fetal congenital malformations, or any other problems that could affect breastfeeding. The study is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [10].
Data collection
The questionnaire was designed by the researchers based on previous studies [3, 7] to address the survey objectives. It comprised a total of 28 items by using dichotomous, multiple-choice or open-ended questions, including breastfeeding practice from birth to six months, maternal sociodemographic characteristics, knowledge about the general breastfeeding recommendations by WHO (i.e. optimal infant breastfeeding should be initiated within the first hour of birth, EBF continue for six months and then appropriate complementary feeding should commence together with breastfeeding for at least two years) [11], obstetric information, breastfeeding support during hospitalization, and work related factors (Table 1). Regarding skin-to-skin contact and breastfeeding initiation after birth, the questionnaire asked participants if skin-to-skin contact started within 10 minutes (immediately) and breastfeeding started within the first hour after birth, respectively. To avoid recall bias, WHO recommends the indicator definition of EBF under six months is the percentage of infants 0-5 months of age who were fed exclusively with breast milk during the previous day [12]. Because this study only enrolled the mothers with infants aged 7-12 months, we investigated the breastfeeding practice from birth to six months. There were three options for the breastfeeding practice up to six months (i.e. EBF, mixed feeding or no breastfeeding). We explained in detail to the participants that EBF meant that they fed infants exclusively with breast milk without any additional food or drink, except for medicines, vitamins, and minerals from birth to six months. Participants who chose “mixed feeding” or “no breastfeeding” were grouped into non-EBF group and were asked to further report the reasons for non-EBF (open-ended and can be multiple).
The questionnaire was designed as simple as possible for participants to easily understand and make choices. Prior to the formal release, the questionnaire was pretested among 10 unselected mothers who did not included in the final survey to evaluate the appropriate wording and acceptability. Then the questionnaire was released online in the seven WeChat groups and all eligible mothers were invited to this survey. Each WeChat group manager who had been trained specifically for this survey was responsible for giving a full explanation to potential participants about the purpose of the survey, eligibility and exclusion criteria, questionnaire questions, and for answering any questions raised by the participants during the study via in-group text and/or audio messages. They also explained to the participants the voluntary and anonymity nature of the study including their right to not to participate in or to withdraw from the study at any time, but once they submitted the questionnaire meant they agreed to participate in the study. If agreed, participates were asked to complete and submit the questionnaire online on their mobile phones within two weeks.
Ethical considerations
This study was approved by the Local Research Ethics Committee of Jiaxing Maternity and Children Health Care Hospital (Approval No. 2021-F-61). It was a voluntary and anonymous online survey, participants were informed that completing and submitting the questionnaire meant they agreed to participate in the study. As such, the requirement for written informed consent was waived by the Ethics Committee.
Data analysis
The primary outcome was the self-reported EBF status from birth to six months. Continuous variables were presented as median (range), categorical variables were presented as number and percentage. Normal distribution for continuous variables was checked using the Shapiro-Wilk test and visual plot inspection. As the continuous variables were not normally distributed, univariate analysis was performed using Mann-Whitney U test, or the x 2 test and Fisher’s exact test to compare the differences between mothers with and without EBF. A multivariable logistic regression model was used to determine the different independent variables associated with EBF status up to six months by the adjusted odds ratio (AOR) and 95% confidence interval (CI). The independent variables that entered into the regression model were those of being significant in univariate analysis (P<0.10) or of possibly influencing EBF indicated by previous studies. Multicollinearity was assessed using the tolerance and variance inflation factor, with tolerance > 0.10 and variance inflation factor < 10.0 were considered acceptable. We did not perform a formal sample size calculation, but used a convenience sampling method. Data were analyzed using SPSS version 19.0 for Windows (IBM Corp., Armonk, NY, USA). A two-sided P < 0.05 was considered as statistically significant.
Results
Sample characteristics
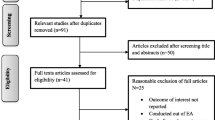
Based on the estimates of the group managers, there were about 1,140 eligible mothers in the seven WeChat groups at the survey time. A total of 857 mothers online completed and submitted the questionnaire (response rate was 75.2%). Thirty-five mothers were excluded due to multiple gestations (n=27), premature delivery before 34 weeks (n=5), postpartum severe hemorrhage (n=2) or infections (n=1), leaving 822 mothers included in this study. There were no significant differences in background characteristics between excluded and included mothers (data not shown). All submitted questionnaires were complete.
The median age of participants was 29.6 (range 17-47) years. All participants were of Han ethnic and received a junior high school education or above (i.e. all had completed at least the nine-year compulsory education). The majority of surveyed mothers were married (98.1%), employed full-time or part-time (86.5 %) with a monthly family income of more than 5 000 RMB (91.1%), and aware of all three WHO recommendations about breastfeeding (86.1%). All mothers gave birth at seven public hospitals located in Jiaxing, of which five had Baby-Friendly Hospital Initiative (BFHI) certificates. With respect to obstetric and hospitalization information, 89.9% of mothers reported term (> 37 weeks), 67.3% reported primiparous, 65.3% reported vaginal delivery, 92.5% reported room-in, 88.6% reported skin-to-skin contact with their infants within 10 minutes after birth, 67.2% reported breastfeeding initiation within the first hour of birth and 88.9% reported EBF during hospitalization. In addition, of the full-time employed mothers (n=480), the majority (87.5%) reported that they returned to work after a paid maternity leave of 128 days for vaginal delivery and 143 days for cesarean delivery, but 72.7% reported that there was no independent breastfeeding room at their workplaces.
EBF status up to six months and associated factors
Overall, 586 mothers reported that they exclusively breastfed their infants until six months of age, with a rate of EBF up to six months of 71.3% (95% CI 68.2, 74.4%). Univariate analysis showed that higher odds of EBF up to six months were found among the mothers with the following characteristics: younger (P=0.001), lower body mass index (BMI) (P=0.015), unemployed (P=0.003), vaginal delivery (P=0.014), breastfeeding initiation within the first hour post birth (P=0.017), and no perception of insufficient breast milk (P<0.001) (Table 2). After adjustment for other variables, multivariable regression analysis indicated that only older maternal age (AOR 0.956; 95% CI 0.917, 0.997) and perceived insufficient breast milk (AOR 0.104; 95% CI 0.072, 0.149) were associated with lower odds of EBF up to six months compared to the counterparts (Table 3).
Reasons for non-EBF up to six months
In 236 non-EBF mothers, the top five reasons given for non-EBF up to six months were no or insufficient breast milk (n=141, 59.8%), inability to breastfeed their infants as needed after return to work (n=56, 23.9%), no flexible nursing breaks at work (n=43, 18.2 %), infant crying or feeling tired or troubled with breastfeeding (n=23, 9.7%), and nipple and breast problems (n=22, 9.3%), respectively. Other reasons included the concern that breast milk alone was not sufficient for infant’s nutritional needs (n=17, 7.2%), infant’s weight below the standard (n=16, 6.8%), no breastfeeding room or refrigerator for expressing or storing breast milk at workplace (n=16, 6.8%), perceived inconveniences or discomfort of breastfeeding in public (n=10, 4.2%), maternal illness (n=6, 2.5%), and pain or discomfort (n=4, 1.7%).
Discussion
The current study reveals that the EBF rate, as the measurement of exclusively breastfed infants from birth to six months, is 71.3% among the mothers of infants aged 7-12 months within our maternal health WeChat groups. However, considering that the participants were only from the WeChat groups, further comparative study is needed to confirm the role of WeChat groups in promoting breastfeeding.
Health workers have played an important role in breastfeeding initiation and continuation [4,5,6,7,8,9]. In the traditional model of maternal health care, women are required to attend antenatal and postnatal clinics or classes regularly, and health workers are needed to follow up the mothers by telephone calls or home visits after their hospital discharge. This could decrease the compliance of women and increase the workload of health workers, which in turn diminishes the effectiveness of maternal health care. Because WeChat is now universally used by almost all women of childbearing age in our area, we adopt the establishment of maternal health WeChat groups as part of routine maternal health care. To facilitate management, we have established seven WeChat groups according to the administrative regions, namely, one WeChat group is responsible for the perinatal women of a county or district. In this way, health workers can provide regular breastfeeding education for all women and individual counseling for those who are experiencing feeding problems. The higher awareness rate (86.1%) of all three breastfeeding WHO recommendations in this study also reflects the effectiveness of this model of health education. In addition, the mothers within the group can also share their breastfeeding experiences with each other, thereby enhancing their breastfeeding confidence.
We acknowledge that other factors could also contribute to this higher rate of EBF up to six months in this study. In particular, most mothers gave birth at the BFHI certificate hospitals which adopted the “Ten Steps to Successful Breastfeeding” launched by WHO [13]. Therefore, it is not surprising that a higher proportion of mothers, even for those with cesarean delivery, reported that they had skin-to-skin contact immediately after birth, rooming-in with their infants, breastfeeding initiation within the first hour and EBF during hospitalization in our study. These interventions have all been shown to be strong contributors to establishment and continuation of breastfeeding [7, 14,15,16,17].
In line with previous studies [4, 5, 18,19,20], we found that there were significant differences in maternal age, BMI, employment status, mode of delivery, breastfeeding initiation, and perception of insufficient breast milk between mothers with and without EBF based on the univariate analyses. However, multivariable regression analysis showed that only maternal age and perception of insufficient breast milk were statistically associated with EBF up to six months, especially that perceived insufficient breast milk significantly decreased the odds of EBF from birth to six months. Regarding the relationship between maternal age and EBF, data in the literatures are conflicting. Some studies observed that older mothers were associated with lower EBF compared to younger ones [3, 5]; in contrast, other studies showed that older mothers were more likely to practice EBF than younger ones [19, 21]. In this study, maternal age was found to be negatively but marginally associated with EBF, indicating a limited effect.
The lack of associations of employment status and breastfeeding initiation with EBF up to six months may be due to the fact that the majority of surveyed mothers were employed and had breastfeeding initiation within the first hour. As for mode of delivery, previous studies suggested that women with cesarean delivery were less likely to EBF than those with vaginal delivery [3, 14]. Delayed onset of lactation, disrupted mother-infant interaction, inhibited infant suckling and poor pain relief may mediate the effects of caesarean delivery on breastfeeding [22]. In the current study, although caesarean delivery was less common in EBF mothers than in non-EBF mothers, it was not statistically associated with EBF up to six months after adjustment for other confounding variables. This result is consistent with the study by Ruan et al [5], and suggests that if the mothers receive adequate breastfeeding support during hospitalization, caesarean delivery is not necessarily a barrier to EBF. This may be especially important considering that a relatively higher caesarean delivery rate in China [23]. In addition, we did not found the differences in mothers’ educational level, monthly family incomes, skin-to-skin contact, and room-in between mothers with and without EBF, those have been identified as the factors related to EBF in previous studies [2, 3, 8, 17]. Again, sample characteristics and hospital practices may explain the discrepancies between this study and other studies.
With regard to the reasons for non-EBF up to six months, no or insufficient breast milk is the foremost one reported by the non-EBF mothers. This is consistent with the results of multivariable regression analysis and of other studies [3, 5, 6]. However, in fact, only few mothers have physiological insufficient milk supply and most mothers can produce enough breastmilk to meet their infant’s demand [24]. As such, this result may imply the inadequate education and guidance provided by health workers on this issue. The next main reasons are those work related factors, including inability to breastfeed their infants as needed after return to work and lack of flexible breaks at work. Notably, although fewer mothers (6.8%) stated no breastfeeding room or refrigerator at workplaces as the reason for non-EBF, 72.7% of the employed mothers reported there was no breastfeeding room at their workplaces. Other reasons are various, including infant crying or mother feeling tired or troubled with breastfeeding, nipple and breast problems, the concern about breast milk alone being not sufficient for infant’s needs, and perceived inconveniences or discomfort of breastfeeding in public. Fortunately, most reasons listed above can be amended through education and interventions. For example, health workers can guide mothers how to tell the difference between physiological and perceived insufficient breast milk, prepare mothers for tiredness and fatigue, improve mothers’ ability to soothe their infants, and eliminate their concern about insufficient breast milk nutrition. Returning to work before six months is still the common reason of early weaning breastfeeding for working mothers [5, 7, 9]. Thus, breastfeeding-friendly work policies and environments are needed for improving EBF among those mothers. For example, a relatively long maternity leave can extend breastfeeding duration for working mothers [7, 18, 25]. Hence, government may consider a longer paid maternity leave, guarantee frequent and flexible breaks at work, and encourage the provision of an independent breastfeeding room with a refrigerator at the workplaces. In Jiaxing, women can now have a paid maternity leave of 128 days for vaginal delivery and 143 days for cesarean delivery.
Limitations
This study has some limitations. First, due to the nature of cross-sectional design, we cannot establish causal relationships between EBF and associated factors. Second, this study only enrolled the mothers within our maternal health WeChat groups, so the sample would be underrepresented. It is possible that women who joined in the WeChat groups had stronger intention to breastfeed exclusively than those outside groups. Further study, such as prospective cohort study, is therefore needed to explore the effect of WeChat groups on breastfeeding and women’s perceptions of WeChat groups by comparing women within WeChat groups with those outside. Such a study should also use the WHO definition of EBF in order to be comparable with other studies. Third, the response rate was estimated to be about 75.3%. It is possible that mothers who did not practice EBF were less willing to respond than those who did, which may lead to overestimation of the EBF rate. Fourth, because the mothers completed the questionnaire six months after their delivery, the recall bias could not be avoided. Also the self-report nature of the study may cause reporting bias. Finally, the questionnaire was designed to be relatively simple in order to increase the participation rate. There were some important factors that failed to be measured, such as mothers’ intention and attitude to breastfeeding, the time when mothers introduce complementary foods and stop breastfeeding, supports of husbands and families, etc. These variables have previously been reported as the factors affecting EBF [7, 25] and may provide more information for future breastfeeding education and interventions.
Conclusions
In summary, this preliminary study shows that 71.3% of mothers within our maternal health WeChat groups exclusively breastfed their infants up to six months, but further comparative study is needed to confirm the effect of WeChat groups on breastfeeding. On the other hand, the perceived insufficient breast milk and work related factors are still the main barriers to EBF up to six months in our study setting. Therefore, future health care should provide more adequate breastfeeding education, especially concerning insufficient breast milk, and promote the provision of a breastfeeding-friendly work environment for working mothers.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- EBF:
-
Exclusively breastfeeding
- OR:
-
Odds ratio
- WHO:
-
World Health Organization
References
World Health Organization. Global nutrition targets 2025: policy brief series. 2014. Available from: https://www.who.int/publications/i/item/WHO-NMH-NHD-14.2. Accessed 22 Oct 2021.
Duan Y, Yang Z, Lai J, Yu D, Chang S, Pang X, et al. Exclusive breastfeeding rate and complementary feeding indicators in China: A national representative survey in 2013. Nutrients. 2018;10:249. https://doi.org/10.3390/nu10020249.
Shi H, Yang Y, Yin X, Li J, Fang J, Wang X. Determinants of exclusive breastfeeding for the first six months in China: A cross-sectional study. Int Breastfeed J. 2021;16:40. https://doi.org/10.1186/s13006-021-00388-y.
Wang W, Lau Y, Chow A, Chan KS. Breast-feeding intention, initiation and duration among Hong Kong Chinese women: a prospective longitudinal study. Midwifery. 2014;30:678–87. https://doi.org/10.1016/j.midw.2013.07.015.
Ruan Y, Zhang Q, Li J, Wan R, Bai J, Wang W, et al. Factors associated with exclusive breast-feeding: A cross-sectional survey in Kaiyuan, Yunnan, Southwest China. PLoS One. 2019;14:e0223251. https://doi.org/10.1371/journal.pone.0223251.
Li J, Zhao C, Wang Y, Wang YP, Chen CY, Huang Y, et al. Factors associated with exclusive breastfeeding practice among mothers in nine community health centres in Nanning city, China: a cross-sectional study. Int Breastfeed J. 2021;16:71. https://doi.org/10.1186/s13006-021-00416-x.
Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, et al. Lancet Breastfeeding Series Group. Why invest, and what it will take to improve breastfeeding practices? Lancet. 2016;387:491–504. https://doi.org/10.1016/S0140-6736(15)01044-2.
Zhang Z, Zhu Y, Zhang L, Wan H. What factors influence exclusive breastfeeding based on the theory of planned behaviour. Midwifery. 2018;62:177–82. https://doi.org/10.1016/j.midw.2018.04.006.
Jama NA, Wilford A, Masango Z, Haskins L, Coutsoudis A, Spies L, et al. Enablers and barriers to success among mothers planning to exclusively breastfeed for six months: a qualitative prospective cohort study in KwaZulu-Natal, South Africa. Int Breastfeed J. 2017;12:43. https://doi.org/10.1186/s13006-017-0135-8.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–9. https://doi.org/10.1016/j.ijsu.2014.07.014.
World Health Organization. Infant and young child feeding. World Health Organization. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding. Accessed 22 Oct 2021.
World Health Organization. Indicators for assessing infant and young child feeding practices: definitions and measurement methods. Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF), 2021. Available from: https://creativecommons.org/licenses/by-nc-sa/3.0/igo. Accessed 28 Sept 2022.
World Health Organization. National implementation of the baby-friendly hospital initiative 2017. ISBN 978-92-4-151238-1. Available from: https://apps.who.int/iris/bitstream/handle/10665/255197/9789241512381-eng.pdf;sequence=1. Accessed 20 Oct 2021.
Hakala M, Kaakinen P, Kääriäinen M, Bloigu R, Hannula L, Elo S. Maternity ward staff perceptions of exclusive breastfeeding in Finnish maternity hospitals: A cross-sectional study. Eur J Midwifery. 2021;5:16. https://doi.org/10.18332/ejm/134846.
Hawkins SS, Stern AD, Baum CF, Gillman MW. Evaluating the impact of the baby-friendly hospital initiative on breast-feeding rates: A multi-state analysis. Public Health Nutr. 2015;18:189–97. https://doi.org/10.1017/S1368980014000238.
Cinquetti M, Colombari AM, Battisti E, Marchetti P, Piacentini G. The influence of type of delivery, skin-to-skin contact and maternal nationality on breastfeeding rates at hospital discharge in a baby-friendly hospital in Italy. Pediatr Med Chir. 2019;41:17–21. https://doi.org/10.4081/pmc.2019.207.
Jaafar SH, Ho JJ, Lee KS. Rooming-in for new mother and infant versus separate care for increasing the duration of breastfeeding. Cochrane Database Syst Rev. 2016;(8):CD006641. https://doi.org/10.1002/14651858.CD006641.
Mirkovic KR, Perrine CG, Scanlon KS, Grummer-Strawn LM. Maternity leave duration and full-time/part-time work status are associated with US mothers' ability to meet breastfeeding intentions. J Hum Lact. 2014;30:416–9. https://doi.org/10.1177/0890334414543522.
Moshi FV, Akyoo EE, Seif SA. Prevalence and predictor of exclusive breastfeeding among mothers of 0 to 6 months infants from pastoralists and hunters' community in Tanzania; A community based cross-sectional study. East Afr Health Res J. 2021;5:82–90. https://doi.org/10.24248/eahrj.v5i1.655.
Castillo H, Santos IS, Matijasevich A. Maternal pre-pregnancy BMI, gestational weight gain and breastfeeding. Eur J Clin Nutr. 2016;70:431–6. https://doi.org/10.1038/ejcn.2015.232.
Yang X, Ip WY, Gao LL. Maternal intention to exclusively breast feed among mainland Chinese mothers: A cross-sectional study. Midwifery. 2018;57:39–46. https://doi.org/10.1016/j.midw.2017.11.001.
Prior E, Santhakumaran S, Gale C, Philipps LH, Modi N, Hyde MJ. Breastfeeding after cesarean delivery: A systematic review and meta-analysis of world literature. Am J Clin Nutr. 2012;95:1113–35. https://doi.org/10.3945/ajcn.111.030254.
Li HT, Luo S, Trasande L, Hellerstein S, Kang C, Li JX, et al. Geographic variations and temporal trends in cesarean delivery rates in China, 2008-2014. JAMA. 2017;317:69–76. https://doi.org/10.1001/jama.2016.18663.
Hector D, King L, Webb K, Heywood P. Factors affecting breastfeeding practices: applying a conceptual framework. N S W Public Health Bull. 2005;16:52–5. https://doi.org/10.1071/nb05013.
Gebrekidan K, Hall H, Plummer V, Fooladi E. Exclusive breastfeeding continuation and associated factors among employed women in North Ethiopia: A cross-sectional study. PLoS One. 2021;16:e0252445. https://doi.org/10.1371/journal.pone.0252445.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
C.Y.F. and X.J.T. formulated the concept and design of the survey. C.Y.F., L.P.P., H.Y.J. and J.F.Y. carried out the survey. C.Y. F. and L.Z.W. collected and analysed the data and completed the first draft. All authors contributed to revising the draft and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Local Research Ethics Committee of Jiaxing Maternity and Children Health Care Hospital (Approval No. 2021-F-61). As it was an online survey and participants were informed about the voluntary nature of the survey, the requirement for written informed consent was waived by the Ethics Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fu, CY., Tang, XJ., Pan, LP. et al. Exclusive breastfeeding rate and related factors among mothers within maternal health WeChat groups in Jiaxing, Zhejiang province, China: a cross-sectional survey. Int Breastfeed J 17, 80 (2022). https://doi.org/10.1186/s13006-022-00521-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13006-022-00521-5