Abstract
Background
A rare case of neuroendocrine cell tumor (NET) having both conventional and mucinous components was reported. Mucinous NET is rarely encountered in the pathological diagnosis of gastrointestinal (GI) tumors. Here we examined the mechanism for transformation of conventional NETs into mucinous NETs. Case presentation: Macroscopic examination revealed a tumor with ulceration in the ampulla of Vater that measured 1.7 cm in its largest diameter. Histologically, the tumor comprised two components: a tubular/ribbon-like feature and small nests floating in a mucinous lake. The tumor nests showed sheet, nest and ribbon-like structures of small cells having eosinophilic cytoplasm as well as small-sized nuclei with dense hyperchromatin. Immunohistochemical analysis showed tumor cells positive for pan-endocrine markers (synaptophysin, CD56, INSM1 and chromogranin). Based on the histological findings, the solid and mucinous components were diagnosed as conventional and mucinous NETs, respectively. Grading was NET G2 based on 12.8% and 13.2% Ki-67-positive cells in the solid and mucinous components, respectively. Immunohistochemically, the mucin phenotype of this tumor was gastric and intestinal. Only the mucinous NET component had cytoplasmic CD10 expression. Examination using a customized gene panel detected only a DPC4 mutation, which was limited to the mucinous component. Conclusions: Coexistence of conventional and mucinous NETs could provide important insight into evaluating the NET subtype histogenesis. Moreover, molecular alterations including cytoplasmic expression of CD10 and the DPC4 mutation can contribute to interpretation of tumor pathogenesis.
Similar content being viewed by others
Introduction
Gastrointestinal neuroendocrine cell tumors (GI-NETs) are a heterogeneous group of neoplasms arising from neuroendocrine cells, which represent a small fraction of the intestinal crypt [1]. GI-NETs are rare, but their incidence is increasing [2,3,4]. Gastric NETs (G-NETs) and duodenal NETs (D-NETs) are frequent upper GI-NETs in terms of tumor location [3,4,5]. D-NETs in particular have attracted increasing attention since duodenal tumors can be treated endoscopically [5, 6]. NETs rarely occur at the ampulla of Vater, and when they do occur at this site they have a different biological behavior [6, 7]. NETs are classified into three distinct subgroups: grade I, II, and III. Grade I (G1)-NETs have a low mitotic rate (< 2 mitoses/2 mm2) and Ki-67 index < 3% [8]. G2 NETs have an intermediate mitotic rate and Ki-67 index, whereas for G3 NETs the mitotic rate and Ki-67 index exceeds 20 mitoses/2 mm2 and > 20%, respectively. NECs (neuroendocrine cell carcinoma) have, by definition, a high mitotic rate (> 20 mitoses/2 mm2) and Ki-67 index > 20% and are classified as either large- or small-cell neuroendocrine carcinoma [8]. This classification is widely used to predict the malignant behavior of NETs [8].
Patients with NETs in the ampulla of Vater were recently shown to have worse overall survival (OS) than those having NETs in the duodenum [3, 4]. The reasons for this poor prognosis are unclear. Here we describe a rare case with histological features of mucinous NET, characterized by cells floating within a mucinous lake, mixed with NET G2.
Case presentation
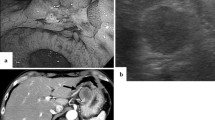
The patient was a Japanese woman in her 70 s who had no physical syndrome. She visited our hospital for liver dysfunction but had no jaundice. Computed tomography (CT) and endoscopic retrograde cholangiopancreatography (ERCP) revealed no finding at the time of her hospital visit. Biannual follow-up CTs were performed. Two years after the initial visit, CT and ERCP were performed again due to mild fever and left abdominal pain. The ERCP showed an ~ 20-mm mass in the ampulla of Vater with an ulcer and bleeding. A biopsy was performed.
A pancreaticoduodenectomy was performed after pathological findings of the endoscopic biopsy of the ampulla of Vater suggested the presence of a malignant tumor. Macroscopic examination revealed a tumor in the duodenal papilla measuring 1.7 cm in its largest diameter. Irregular nodules, bleeding and ulceration consistent with endoscopic findings were seen (Fig. 1-a).
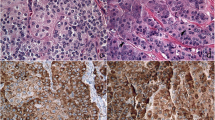
Histologically, the tumor had two components including a solid nest and mucinous lake formation (Fig. 1-b). The solid nest was characterized as sheets and nests with a ribbon like-structure of small cells having eosinophilic cytoplasm and small-sized nuclei with dense hyperchromatin and little mucus (Fig. 1-c, d). Such nests did not show trabecular or well-differentiated tubular features and also lacked goblet and Paneth-like cells. In addition, mucous cells scattered within the nests was found in the present case. The mucinous lake formation resembled mucinous carcinoma (Fig. 1-e) and had nests of tumor cells surrounded by extracellular mucin; the cell nests floated within an extra-cellular mucin lake (Fig. 1-f) that histologically resembled those of the solid component (Fig. 1-e and -f). However, pleomorphic nuclear features and well- to moderately-differentiated tubular formations that are typically found in duodenal adenocarcinoma were not seen in the current case. On the basis of the findings, the nests of the two components were suggestive of NET. We thus considered that the tubular/ribbon-like nests and the nests within the mucinous lake were NETs, specifically, conventional and mucinous NETs, respectively. Next, we examined immunohistochemical endocrine makers including synaptophysin, INSM1, CD56 and chromogranin to determine the NET’ characteristic. Immunohistochemical analysis was positive for several pan-endocrine markers (synaptophysin, INSM1, CD56 and chromogranin) (Fig. 2-a-h; Table 1). Although INSM1, CD56 and chromogranin positivity was scattered (Fig. 2c–h), expression of synaptophysin was diffuse positive (Fig. 1a and -b). The sample was negative for the functional markers including somatostatin, insulin, glucagon, gastrin, and serotonin. Fourteen lymph nodes were identified and showed no tumor involvement. The final diagnosis of the two tumor components was neuroendocrine cell tumor, NET, grade 2, of the duodenal papilla, based on auto-analyzer measurements at hot spot regions that showed a 12.8% and 13.2% Ki-67 index in the solid nest and mucinous components, respectively. Hot spots in the solid nest and mucinous components had mitotic counts of 3 and 5, respectively (Fig. 2-i and j). We also examined immunohistochemical expression of mucin markers (MUC2, MUC5AC and MUC6) and CD10. Both components had diffuse positive MUC2 expression (Fig. 2-k and -l) and focal MUC5AC expression (Fig. 2-m and -n). No MUC6 staining was detected in either component (Fig. 2-o and -p). The mucin phenotype was determined to be mixed gastric and intestinal (GI phenotype). The mucinous component was positive for cytoplasmic CD10 expression, but the conventional component was negative (Fig. 2-q and -r). Separate examination of gene mutations in both components using a customized gene panel containing 28 genes (APC, BRAF, TP53, CDKN2A, MET, ATM, MLH-1, PMS2, HRAS, AXIN2, BAX, DCC, MSH2, POLE, RNF43, PTEN, EPCAM, MSH6, BUB1B, RHOA, KRAS, NRAS, SMAD4, CDK4, PIK3CA, STK11, TGFBR2, and EGFR) detected only a DPC4 mutation that was limited to the mucinous component (R361H (cGc > cAc).
Immunohistochemical findings of the tumor sample. Diffuse positive staining of synaptophysin in the (a) conventional and (b) mucinous NET component. Scattered positive staining of INSM1 in the (c) conventional and (d) mucinous NET component. Scattered positive staining of CD56 in the (e) conventional and (f) mucinous NET component. Scattered positive staining of chromogranin in the (g) conventional and (h) mucinous NET component. Ki-67 positive ratio in (i) conventional and (j) mucinous NET is 3.4%. Diffuse positive MUC2 staining in (k) conventional and (l) mucinous NET. Focal positive staining of MUC5AC in (m) conventional and (n) mucinous NET. Negative staining of MUC6 in (o) conventional and (p) mucinous NET. Negative CD10 expression in (q) conventional NET and (r) positive CD10 cytoplasmic staining in mucinous NET
Discussion
Goblet cell carcinoid (GCC) and conventional adenocarcinoma with endocrine cell differentiation are important factors for the differential diagnosis of disease in this patient and can be distinguished based on histological, immunohistochemical and molecular findings [9, 10]. GCC is a histologically amphicrine neoplasm containing goblet-like mucinous cells with varying numbers of endocrine cells and Paneth-like cells that typically have a tubular or clustered (or trabecular) arrangement [9]. However, the current case did not have such characteristic cytological findings with neither goblet-like nor Paneth-like cells found. Moreover, this case did not have the typical architecture of the GCC tumor cell nests and instead had medium- to large-sized nests rather than small, trabecular nests that are frequently found in GCC [9]. Based on these histological findings, GCC can likely be excluded from the histological diagnosis [9]. Second, conventional adenocarcinoma with endocrine cell differentiation is histologically characterized by pleomorphic nuclear features, and well- to moderately-differentiated tubular formations, but these features, which are typically found in duodenal adenocarcinoma, were not seen in the current case [11, 12]. In particular, nuclear pleomorphism is an important finding for differential diagnosis between duodenal adenocarcinoma and duodenal NET [11, 12]. However, the current case lacked nuclear pleomorphism and a high mitotic count that is generally seen for duodenal adenocarcinoma. In addition, synaptophysin in both tumor components of the current case, which supports the diagnosis of NET since in adenocarcinoma with endocrine cell differentiation endocrine cells are scattered within cancer nests. The diagnosis for the current case is further supported by the finding that only a DPC4 mutation was detected. In contrast, the specific mutational spectrum of duodenal adenocarcinoma frequently includes mutations in TP53 and KRAS, which are rare in NETs [13]. These findings suggest that conventional NET can transform into mucinous NET that may arise from mucous cells scattered within the nests. Indeed, a case of ductal carcinoma of the breast was reported to have endocrine differentiation resulting in mucinous NEC [14]. However, the present case differs in the coexistence of conventional and mucinous NETs. To our knowledge, this is the first case of conventional NET that progressed into mucinous NET in the ampulla of Vater.
NET grading as G1, G2 and G3 describes the aggressive or malignant nature of a tumor [8]. The tumor in the present case was G2 based on its 3.8% Ki-67 positive rate and its mitotic count. Previous studies indicated that the prognosis of ampulla of Vater NET is poorer than that of duodenal NET [4, 15]. However, the prognosis of G2 NET in general is currently unclear since there were few studies describing NET grading including G2 before the proposal of the World Health Organization that was published in 2010 [13].
In immunohistochemical analysis of gastric mucin markers and CD10, the tumor had a GI phenotype suggestive of differentiation toward a gastric and intestinal phenotype [16]. The staining pattern is supported by the previous finding that a GI phenotype is common in rectal NET [16]. Here cytoplasmic expression of CD10 was detected only in mucinous NET. Cytoplasmic expression of CD10 correlates with tumor aggressiveness and increased metastatic potential, especially in colorectal cancer [17, 18]. The clinicopathological significance of cytoplasmic CD10 expression in NETs should be elucidated in the future.
We detected no mutations in the tumor in an examination using a customized panel of 28 genes that are closely associated with GI tumor carcinogenesis. This finding suggests that mutations that drive GI cancer may be less relevant to NET G2. Meanwhile, TP53 and DPC4 mutations that contribute to GI tumorigenesis [19] rarely occur in well-differentiated endocrine tumors [20]. Here we found no TP53 mutation, but a DPC4 mutation was detected in the mucinous NET component indicating that DPC4 could promote tumorigenesis in some NETs [21].
In summary, this tumor has both conventional NET G2 and a mucinous component termed mucinous NET. This NET variant is a rare tumor in duodenal NET, especially in the ampulla of Vater, and the prognosis may be assumed to be poor. Additional cases are needed to fully characterize the pathogenesis of this variant. Finally, only the mucinous component had cytoplasmic CD10 expression and DPC4 mutation that both may be associated with progression from conventional to mucinous NET.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Chetty R. An overview of practical issues in the diagnosis of gastroenteropancreatic neuroendocrine pathology. Arch Pathol Lab Med. 2008;132:1285–9. https://doi.org/10.5858/2008-132-1285-AOOPII.
O’Toole D, Delle Fave G, Jensen RT. Gastric and duodenal neuroendocrine tumours. Best Pract Res Clin Gastroenterol. 2012;26:719–35. https://doi.org/10.1016/j.bpg.2013.01.002.
Malladi UD, Chimata SK, Bhashyakarla RK, Lingampally SR, Venkannagari VR, Mohammed ZA, et al. Duodenal neuroendocrine tumor-tertiary care center experience: A case report. World J Transl Med. 2023;11:1–8. https://doi.org/10.5528/wjtm.v11.i1.1.
Bornstein-Quevedo L, Gamboa-Domínguez A. Carcinoid tumors of the duodenum and ampulla of vater: a clinicomorphologic, immunohistochemical, and cell kinetic comparison. Hum Pathol. 2001;32:1252–6. https://doi.org/10.1053/hupa.2001.28955.
Mandair D, Kamieniarz L, Pizanias M, Weickert MO, Narayan A, O’Mahony LF, et al. Diagnostic features and management options for duodenal neuroendocrine neoplasms: a retrospective, multi-centre study. Sci Rep. 2022;12:15762. https://doi.org/10.1038/s41598-022-19738-9.
Hartel M, Wente MN, Sido B, Friess H. Büchler MW. 2005;20:676–81. https://doi.org/10.1111/j.1440-1746.2005.03744.x.
Chen J, Chen Q, Deng Y, Jiang Y, Huang Z, Zhou J, et al. Development and Validation of Prognostic Nomograms for Periampullary Neuroendocrine Neoplasms: A SEER Database Analysis. Curr Oncol. 2022;30:344–57. https://doi.org/10.3390/curroncol30010028.
Laird AM, Libutti SK. Management of Other Gastric and Duodenal Neuroendocrine Tumors. Surg Oncol Clin N Am. 2020;29:253–66. https://doi.org/10.1016/j.soc.2019.11.009.
Albores-Saavedra J, Henson DE, Batich K. Pathologic classification and clinical behavior of the spectrum of goblet cell carcinoid tumors of the appendix. Am J Surg Pathol. 2009;33:1259–60. https://doi.org/10.1097/PAS.0b013e3181a1b59e. author reply 1260–1.
Chen Y, Liang Y, Cao L, Dong X, Sun D. Neuroendocrine differentiation: a risk fellow in colorectal cancer. World J Surg Oncol. 2023;21:89. https://doi.org/10.1186/s12957-023-02952-8.
Cloyd JM, George E, Visser BC. Duodenal adenocarcinoma: Advances in diagnosis and surgical management. World J Gastrointest Surg. 2016;8:212–21. https://doi.org/10.4240/wjgs.v8.i3.212.
Bosman FT, Carneiro F, Hruban R, Theise N. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon: International Agency for Research on Cancer (IARC); 2010.
Yuan W, Zhang Z, Dai B, Wei Q, Liu J, Liu Y, et al. Whole-exome sequencing of duodenal adenocarcinoma identifies recurrent Wnt/β-catenin signaling pathway mutations. Cancer. 2016;122:1689–96. https://doi.org/10.1002/cncr.29974.
Limaiem F, Bouraoui S. Mucinous breast carcinoma with neuroendocrine differentiation: Case report. Clin Case Rep. 2022;10:e6665. https://doi.org/10.1002/ccr3.6665.
Makhlouf HR, Burke AP, Sobin LH. Carcinoid tumors of the ampulla of Vater: a comparison with duodenal carcinoid tumors. Cancer. 1999;85:1241–9. https://doi.org/10.1002/(sici)1097-0142(19990315)85:6%3c1241::aid-cncr5%3e3.0.co;2-4.
Hirata Y, Mizoshita T, Mizushima T, Shimura T, Mori Y, Kubota E, et al. Gastric-and-intestinal mixed endocrine cell phenotypic expression of carcinoid tumors in the rectum. Oncol Rep. 2009;21:107–12.
Deschamps L, Handra-Luca A, O’Toole D, Sauvanet A, Ruszniewski P, Belghiti J, et al. CD10 expression in pancreatic endocrine tumors: correlation with prognostic factors and survival. Hum Pathol. 2006;37:802–8. https://doi.org/10.1016/j.humpath.2006.02.024.
Kuniyasu H, Luo Y, Fujii K, Sasahira T, Moriwaka Y, Tatsumoto N, et al. CD10 enhances metastasis of colorectal cancer by abrogating the anti-tumoural effect of methionine-enkephalin in the liver. Gut. 2010;59:348–56. https://doi.org/10.1136/gut.2009.178376.
Network CGA. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487(7407):330–7. https://doi.org/10.1038/nature11252.
Ishida S, Akita M, Fujikura K, Komatsu M, Sawada R, Matsumoto H, et al. Neuroendocrine carcinoma and mixed neuroendocrine窶地on-neuroendocrine neoplasm of the stomach: a clinicopathological and exome sequencing study. Hum Pathol. 2021;110:1–10. https://doi.org/10.1016/j.humpath.2020.12.008. (Epub 2021 Jan 21).
Bartsch D, Hahn SA, Danichevski KD, Ramaswamy A, Bastian D, Galehdari H, et al. Mutations of the DPC4/Smad4 gene in neuroendocrine pancreatic tumors. Oncogene. 1999;18:2367–71. https://doi.org/10.1038/sj.onc.1202585.
Acknowledgements
The authors thank Ms. E. Sugawara and Ms. C. Ishikawa for technical assistance, and members of the Southern Tohoku General Hospital Diagnostic Pathology Center for their support.
Funding
The authors have no funding sources to disclose.
Author information
Authors and Affiliations
Contributions
T.S. wrote the main manuscript text and N.U. prepared Figures 1–2 and Table. N.S., M.H. and T.A. provided clinical support during manuscript preparation. M.S. and N.Y. supported the clinicopathological findings. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient for publication of the details of their medical case and any ACCOMPANYING IMAGES.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sugai, T., Uesugi, N., Suzuki, M. et al. A rare case of neuroendocrine cell tumor mixed with a mucinous component in the ampulla of Vater. Diagn Pathol 19, 64 (2024). https://doi.org/10.1186/s13000-024-01488-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13000-024-01488-z