Abstract
Background
Esophageal granular cell tumor (eGCT) is rare, and the recent literature suggests a link between eosinophilic esophagitis (EoE) and eGCT. The aim of our study was to determine if EoE or other disorders associated with eosinophilia are consistently associated with eGCT.
Methods
We retrospectively searched pathology databases of three academic institutions from 1999 to 2018 for eGCTs. The archived slides and medical records were reviewed.
Results
From 294,855 esophagogastroduodenoscopy procedures, 45 patients (17 males and 28 females) with eGCTs were identified. The patients (30–73 years in age, median 50) had eGCT 0.2–2.0 cm in size (average 0.71). Thirteen had a history of gastroesophageal reflux disease, 5 had Barrett esophagus/goblet cell metaplasia and 1 had EoE. Thirty-four eGCTs had intralesional eosinophils (14 with peak > 10 eosinophils/400x hpf); of these, 21 also had eosinophils in lamina propria (9 with peak > 10 eosinophils/hpf). eGCT with atypical features (including nuclear enlargement and prominent nucleoli) were more likely to have increased eosinophils in non-epithelial compartments than those without atypia. Pleomorphism and spindled cells were seen in 3 eGCT cases (mean peak intralesional eosinophils: 43 per hpf); 2 of these had goblet cell metaplasia. We found no association between EoE and eGCT, p = 0.5966, (95% C.I. 0.0276, 6.5389, Fisher’s exact test). Instead, most patients had gastroesophageal reflux disease or Barrett esophagus.
Conclusion
Eosinophilia, common in eGCT and adjacent stroma, likely drives atypical/reactive histologic features, but a pathogenic relationship between eosinophil rich inflammatory conditions and eGCT has not yet been established.
Similar content being viewed by others
Background
Granular cell tumor (GCT) was first described in the tongue by Abrikossoff in 1926. Other names for this entity are granular cell myoblastoma and Abrikossoff’s tumor [1, 2]. Although the lesion is most commonly seen in the skin, soft tissue and tongue, 8–11% of cases occur in the gastrointestinal tract [1,2,3,4,5]. In 1931, Abrikossoff first described GCT in the esophagus, which we now know is the most common site of involvement within the gastrointestinal tract, primarily the distal segment of the esophagus [3, 4].
In the esophagus, eosinophilic esophagitis (EoE) is a clinicopathologic disease that has been more consistently recognized, with increasing prevalence, since the initial publication of consensus recommendations in 2007 [6]. EoE is a chronic, immune/antigen-mediated disease with eosinophil-predominant inflammation that leads to esophageal dysfunction [7]. GCTs have been previously linked to sites of injury and inflammation, leading some to postulate that these lesions might be reactive in nature [8]. There have been several reported cases of concomitant esophageal granular cell tumor (eGCT) and EoE cases in both adults and pediatric patients [9,10,11]. More recently, two separate single center case series proposed an association between the two entities [12, 13]. In order to further study this possible link, we conducted a multi-center study including three separate academic center institutions from different regions of the United States.
Methods
Pathology databases from University of Washington Medical Center (UWMC), Duke University Medical Center (DUMC) and University of Michigan Medical Center (UMMC) were retrospectively searched for cases of eGCT from January 1999 to January 2018. Patient medical records were reviewed for demographic information, diagnoses, presenting clinical symptoms, endoscopic findings and follow-up. A total of 108,244 EGD procedures were performed at UWMC from January 1999 to January 2018, and 1704 patients had diagnosis of EoE by ICD9 and ICD10 codes from 2008 to 2018. Endoscopy procedure data were available from DUMC from January 2006 to January 2018, where 77,295 esophagogastroduodenoscopy (EGD) procedures were performed, and 1481 patients had diagnosis of EoE by ICD9 and ICD10 codes. At UMMC, there were 64,316 EGD procedures and 2692 cases of EoE by ICD9 and ICD10 codes from June 2012 to May 2020.
Cases of eGCT were retrieved from the pathology archives of the three participating institutions and blindly reviewed by experienced GI pathologists practicing at each site. In addition to confirming the pathologic diagnosis, the pathologists also recorded typical histologic features including necrosis, spindling, nuclear pleomorphism, increased mitotic activity (≥2 mitosis/ 400x), increased nuclear size (at 100x), and large nucleoli (at 100x) for each case of eGCT [12, 14]. The lesional tissue, surrounding stroma and the overlying epithelium were evaluated for eosinophilia and the peak eosinophil count in each compartment was documented at 400x magnification (hpf). The statistical significance of observed versus expected rates of simultaneous eGCT and EoE was analyzed using Fischer’s exact test based on the null hypothesis of no association with a two-tailed p-value of < 0.05 considered statistically significant (calculated using STATA version 14, STATA Corp LP, TX).
Results
We pooled data from 294,855 EGD procedures at three academic medical centers and identified 45 patients with eGCT (Table 1).
Clinical findings
All 45 patients were adults; 17 were males and 28 were females (male to female ratio of 1:1.65). Ages ranged from 30 to 73 years, with a median of 50. The most common presenting symptoms were dysphagia, gastroesophageal reflux disease and abdominal pain. Other diseases that were reported clinically or by histology were gastroesophageal reflux disease (13 patients), Barrett esophagus/goblet cell metaplasia (5 patients) and EoE (1 patient). There were three patients with prior history of eGCT by biopsy or fine needle aspirate diagnosis who later underwent endoscopic resection. The majority of patients had their lesion removed by endoscopic mucosal resection. Patient follow-up ranged from 0 to 216 months, with an average of 45. No patient had evidence of metastatic eGCT.
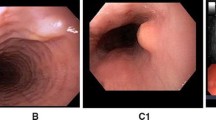
Endoscopic findings
The size of the eGCTs ranged from 0.2–2.0 cm, with an average of 0.71. The most common site was the distal segment of the esophagus and most patients presented with a single nodule. There were two patients with multiple nodules, one of whom had multifocal disease involving all segments of the esophagus.
Histologic findings
Specimens submitted for histopathologic evaluation were derived from either endoscopic biopsies (42%) or endoscopic mucosal resections with or without additional sampling of the esophagus (58%). Two patients had eGCT as an incidental finding during microscopic evaluation. One had eGCT in the proximal segment with a concomitant history of EoE with rings; the other underwent esophagogastrectomy for squamous cell carcinoma status post neoadjuvant therapy and was incidentally found to have eGCT in the distal segment.
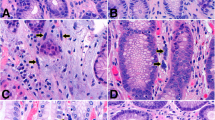
In the single case of EoE, the accompanying eGCT had minimal cytologic atypia and few intralesional eosinophils (Fig. 1A). Thirty-four eGCTs had intralesional eosinophils (14 cases with peak > 10 eosinophils/400x hpf); of these, 21 also had eosinophils in lamina propria (9 cases with peak > 10 eosinophils/hpf).
A, Incidental eGCT in an EoE patient with minimal atypia and lack of intralesional eosinophils (hematoxylin and eosin stain [H&E] at 100x). B, Atypical eGCT with significant intralesional eosinophilia (Geimsa histochemical stain at 200x). C, D, Biopsy from a Barrett esophagus and eGCT showing overlying epithelium with goblet cell metaplasia (H&E at 40x) and atypical GCT with areas of spindling, pleomorphism, increased nuclear size and prominent nucleoli (H&E at 200x)
Twenty-one cases of eGCT had atypical features; fourteen of these had ≤2 atypical features (increased nuclear size and presence of prominent nucleoli). In these cases, the mean peak intralesional eosinophil count was up to 10 eosinophils per 400x hpf. The remaining seven cases with atypia had additional atypical features (spindling and nuclear pleomorphism), and the peak intralesional eosinophils for these cases was up to 112 eosinophils per 400x hpf (Fig. 1B).
Of the 5 cases with Barrett esophagus/goblet cell metaplasia (Fig. 1C), two had 4 atypical features in the accompanying eGCT with areas of spindling, pleomorphism, increased nuclear size and prominent nucleoli (Fig. 1D). No cases of eGCT had necrosis or increased mitosis. In addition, there was no association between eGCT with atypical features and the patient’s age.
Considering all EGD procedures performed at the three institutions with a diagnosis of EoE and eGCT, we found no association between EoE and eGCT, [p = 0.5966, (95% C.I. 0.0276, 6.5389, Fisher’s exact test)]. Considering the single case of eGCT associated with EoE from the UWMC cohort in isolation, there was still no association between EoE and eGCT [p = 0.3058, (95% C.I. 0.0688, 17.6042, Fisher’s exact test)].
Discussion
EoE is an antigen-driven allergic condition with both genetic and environmental contributions [15, 16]. Although EoE occurs in most racial and ethnic groups, there is a predominance in non-Hispanic whites [7]. EoE is more common in patients from rural regions and cold climate zones; it is inversely associated with Helicobacter pylori infection both in adult and pediatric studies [16]. In our study, we attempted to control for inherent differences in patient population and geographical region by collating data from multiple tertiary care centers located in different regions of the United States.
Recent studies have reported the co-occurence of eGCT and significant esophageal intraepithelial eosinophilia, most frequently in the pediatric population [9, 11, 12]. In our multicenter retrospective study of eGCT from 294,855 EGD procedures, 40% of cases had gastroesophageal reflux disease or Barrett esophagus, but only one case in our series of 45 adults had concomitant EoE and eGCT (2%). The apparent rate of concomitant EoE and eGCT in our adult cohort is considerably less than that observed in prior studies, both of which included pediatric patients. Riffle and colleagues identified 18 patients with eGCT from among > 30,000 esophageal cases in their study, 33% of whom (n = 6) also had EoE. Four of these patients were adults and two were adolescents [12]. Similarly, Nojkov and co-authors reported 16 cases of eGCT their series of 167,434 EGD procedures, 31% of which (n = 5) were associated with EoE. Four of these were identified in adults, while 1 was diagnosed in an adolescent [13]. Interesting, although the absence of pediatric patients in our multi-institutional cohort likely affected our observed rate of concomitant EoE and eGCT, this does not completely account for the differences between our study and the prior retrospective studies. A larger multicenter prospective study may be warranted to further investigate the reported association and to determine the underlying pathophysiology of EoE and eGCT.
In addition to the single case of EoE in our eGCT group, there were two cases with significant intraepithelial eosinophilic infiltrates. One was a resection specimen from a patient with squamous cell carcinoma status post neoadjuvant therapy with complete response. The other case had significant eosinophilic infiltrates in biopsies from the distal esophagus, suggesting a closer relationship to severe reflux esophagitis. Reflux disease or heart burn was the presenting symptom in 28% of our patients. The eGCTs found in these patients were in the distal segment of the esophagus (66%), ranging in size from 0.3 to 2.0 cm, in greatest dimension. These findings raise the possibility that the eGCT, by potentially impairing function of the gastroesophageal junction, may have contributed to the onset or severity of reflux esophagitis in these patients (a case report of an esophageal leiomyoma causing reflux esophagitis emphasizes this point [17]). It is tempting, with these observations in mind, to suggest the inclusion of mass lesions including eGCT in the differential diagnosis of new onset reflux esophagitis.
There are reports of concomitant presentation of eGCT and other neoplasms, both benign and malignant, including leiomyoma, squamous cell carcinoma and intramucosal adenocarcinoma in the setting of Barrett esophagus [18,19,20]. The latter illuminates one of the more interesting and novel findings of our study: the presence of eGCT in patients with an established diagnosis of Barrett esophagus or histologic evidence of goblet cell metaplasia. It is also of interest that cases of eGCT with background goblet cell metaplasia showed more atypical features, along with significantly increased intratumoral eosinophils.
Interestingly, neither Nojkov et al. nor Riffle et al. identified eGCT patients with Barrett esophagus/goblet cell metaplasia. Nonetheless, the latter report included observations similar to those in our study, including a high number of eGCTs (67%) with increased intratumoral eosinophilia and a disproportionately high number of eosinophils in eGCT with atypical features [12]. In our study, 76% of eGCT cases had increased intralesional eosinophils and 47% of the cases had eosinophils in the lamina propria of the overlying esophageal mucosa. Given the reproducibility of these findings, we postulate that eosinophilia within the eGCT and adjacent stroma may be driving the observed atypical/reactive histologic features. Although eGCT is commonly considered a benign entity; there are rare reports of cases that presented with lung and liver metastases. There is also a single report of eGCT secreting a tumor marker (carbohydrate antigen 19–9) [21,22,23,24]. Notably, we had no cases of metastatic eGCT in our patient cohort.
Our retrospective study of eGCT is the largest to date, drawing on patient populations from three tertiary care medical centers located in different geographic regions of the country. Even so, our investigation has limitations. Most significantly, our patient cohort consists of only adults and thus differs from the prior published studies. We had two eGCT that were diagnosed incidentally by histology because of procedures for other conditions. All other cases were initially diagnosed in standard esophageal biopsies, a sample type that is typically limited in usual practice, containing only the esophageal epithelium that is immediately superficial to the lesion. With the lack of submucosa in most biopsy specimens, our sample set likely underestimates the prevalence of eGCT in these populations. Also of note, nine patients in our cohort were diagnosed within the 2001–2007 year period, before consensus guidelines for EoE was established [6, 7]. If EoE was widely recognized as a disease entity earlier, more diagnostic and follow up material would have been available for histologic evaluation and we may have identified additional cases of eGCT in the setting of esophageal eosinophilia.
Conclusion
Most patients with eGCT in our cohort had gastroesophageal reflux disease (29%) or an established diagnosis of Barrett esophagus (11%). These patients have frequent follow up with higher rate of endoscopy; hence, the finding of eGCT may be coincidental. Importantly, we found no association between EoE and eGCT. We hypothesize that eosinophilia within the lamina propria of esophageal mucosa likely drives atypical/reactive histologic features within eGCT; however, a pathogenetic relationship between eosinophil mediated inflammatory conditions (including EoE) and eGCT is not yet established.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- GCT:
-
Granular cell tumor
- EoE:
-
Eosinophilic esophagitis
- eGCT:
-
Esophageal granular cell tumor
- UWMC:
-
University of Washington Medical Center
- DUMC:
-
Duke University Medical Center
- UMMC:
-
University of Michigan Medical Center
- EGD:
-
Esophagogastroduodenoscopy
References
Lack EE, Worsham GF, Callihan MD, et al. Granular cell tumor: a clinicopathologic study of 110 patients. J Surg Oncol. 1980;13:301–6.
Chen W, Zheng X, Jin L, Pan X, Ye M. Novel diagnosis and treatment of esophageal granular cell tumor: report of 14 cases and review of the literature. Ann Thorac Surg. 2014;97:296–302.
Johnston J, Helwig EB. Granular cell tumors of the gastrointestinal tract and perianal region: a study of 74 cases. Dig Dis Sci. 1981;26:807–16.
Goldblum JR, Rice TW, Zuccaro G, Richter JE. Granular cell tumors of the esophagus: a clinical and pathologic study of 13 cases. Ann Thorac Surg. 1996;62:860–5.
Parfitt JR, McLean CA, Joseph MG, Streutker CJ, Al-Haddad S, Driman DK. Granular cell tumors of the gastrointestinal tract: expression of nestin and clinicopathological evaluation of 11 patients. Histopathology. 2006;48:424–30.
Furuta GT, Liacouras CA, Collins MH, et al. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007;133:1342–63.
Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:3–20.
Roncati L, Manco G, Italia S, Barbolini G, Maiorana A, Rossi A. Granular cell tumor of the appendix: a new case and review of the literature. Springerplus. 2013;2:649–54.
Buratti S, Savides TJ, Newbury RO, Dohil R. Granular cell tumor of the esophagus: report of a pediatric case and literature review. J Pediatr Gastroenterol Nutr. 2004;38:97–101.
Lucendo AJ, De Rezende L, Martín-Plaza J, Larrauri J. Esophageal granular cell tumor and eosinophilic esophagitis: two interesting entities identified in the same patient. Case Rep Gastroenterol. 2008;2:33–9.
Mohammad S, Naiditch JA, Jaffar R, Rothstein D, Bass LM. Granular cell tumor of the esophagus in an adolescent girl. J Pediatr Gastroenterol Nutr. 2012;54:715.
Riffle ME, Polydorides AD, Niakan J, Chehade M. Eosinophilic esophagitis and esophageal granular cell tumor: an unexpected association. Am J Surg Pathol. 2017;41:616–21.
Nojkov B, Amin M, Ghaith G, Cappell MS. A statistically significant association between esophageal granular cell tumors and eosinophilic esophagitis: a 16-year analysis at two large hospitals of 167,434 EGDs. Dig Dis Sci. 2017;62:3517–24.
Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG. Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol. 1998;22:779–97.
Kottyan LC, Parameswaran S, Weirauch MT, Rotenberg ME, Martin LJ. The genetic etiology of eosinophilic esophagitis. J Allergy Clin Immunol. 2020;145:9–15.
Jensen ET, Dellon ES. Enviromental factors and eosinophilic esophagitis. J Allergy Clin Immunol. 2018;142:32–40.
Howden PE, Dewar EP. Oesophageal leiomyoma-a rare cause of reflux esophagitis. J R Nav Med Serv. 1996;82:27–8.
D’Errico A, Corti B, Fiorentino M, Simone MD, Mattioli S, Grigioni WF. Endoscopic finding of granular cell tumor associated with leiomyomas in the oesophagus. Dig Liver Dis. 2004;36:292–5.
Szumilo J, Dabrowski A, Skomra D, Chibowski D. Coexistence of esophageal granular cell tumor and squamous cell carcinoma: a case report. Dis Esophagus. 2002;15:88–92.
Alkhoury F, Martin JT, Fiedler P, Jaffe PE. Esophageal granular cell tumor colliding with intramucosal adenocarcinoma: a case report. Cases J. 2009;2:8093.
Machado I, Cruz J, Arana E, et al. Lung metastases from esophageal granular cell tumor: an undoubted criterion for malignancy. J Thorac Oncol. 2017;12:1320–2.
Yoshizawa A, Ota H, Sakaguchi N, et al. Malignant granular cell tumor of the esophagus. Virchows Arch. 2004;444:304–6.
Christopher PR, Kingsley PA, Bedi HS, Kwatra KS, Rathore S, Das KC. Large mid-esophageal granular cell tumor: benign versus malignant. Rare Tumors. 2015;7:5772.
Yanoma T, Fukuchi M, Sakurai S, Shoji H, Naitoh H, Kuwano H. Granular cell tumor of the esophagus with elevated preperative serum carbohydrate antigen 19-9: a case report. Int Surg. 2015;100:365–9.
Acknowledgements
Not applicable.
Disclosures
An earlier version of this work was presented in the case study poster sessions at the College of American Pathologists 2018 Annual Meeting (CAP18).
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
DR: Primary corresponding author drafted the manuscript; CC: Collated data from University of Washington Medical Center; DC: Principal investigator from Duke University Medical Center; MS: Collated pathology and patient data from Duke University Medical Center; MW Principal investigator from University of Michigan Medical Center; EM: Collated data from University of Michigan Medical Center; YT: Statistics; LC: Collated endoscopy procedure data from Duke University Medical Center; PES: Principal investigator from University of Washington Medical Center. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional IRB approved study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Reddi, D., Chandler, C., Cardona, D. et al. Esophageal granular cell tumor and eosinophils: a multicenter experience. Diagn Pathol 16, 49 (2021). https://doi.org/10.1186/s13000-021-01113-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13000-021-01113-3