Abstract
Background
A significant proportion of children and adolescents experience back pain. However, a comprehensive systematic review on the effectiveness of rehabilitation interventions is lacking.
Objectives
To evaluate benefits and harms of rehabilitation interventions for non-specific low back pain (LBP) or thoracic spine pain in the pediatric population.
Methods
Seven bibliographic electronic databases were searched from inception to June 16, 2023. Moreover, reference lists of relevant studies and systematic reviews, three targeted websites, and the WHO International Clinical Trials Registry Platform were searched. Paired reviewers independently conducted screening, assessed risk of bias, and extracted data related to study characteristics, methodology, subjects, and results. Certainty of evidence was evaluated based on the GRADE approach.
Results
We screened 8461 citations and 307 full-text articles. Ten quantitative studies (i.e., 8 RCTs, 2 non-randomized clinical trials) and one qualitative study were included. With very low to moderate certainty evidence, in adolescents with LBP, spinal manipulation (1–2 sessions/week over 12 weeks, 1 RCT) plus exercise may be associated with a greater likelihood of experiencing clinically important pain reduction versus exercise alone; and group-based exercise over 8 weeks (2 RCTs and 1 non-randomized trial) may reduce pain intensity. The qualitative study found information provided via education/advice and compliance of treatment were related to effective treatment. No economic studies or studies examining thoracic spine pain were identified.
Conclusions
Spinal manipulation and group-based exercise may be beneficial in reducing LBP intensity in adolescents. Education should be provided as part of a care program. The overall evidence is sparse. Methodologically rigorous studies are needed.
Trial registration
CRD42019135009 (PROSPERO)
Similar content being viewed by others
Introduction
A significant proportion of children and adolescents experience back pain (i.e., thoracic spine pain and low back pain). A systematic review reported that the annual prevalence of low back pain (LBP) is 33.6% (95%CI 26.9%, 41%) in children and adolescents (≤ 18 years old) [1]. The lifetime prevalence of thoracic spine pain (TSP) varies from 9.5% to 72% in children and adolescents [2]. Most episodes of spinal pain (including neck and back pain) are brief in children and adolescents; however, 31% have a recurrence of spinal pain over one year and up to 25% have three or more episodes over one year, and approximately 13% reported episodes lasting five or more weeks [3, 4]. In a cross-sectional international study (650,851 participants), the prevalence of back pain in adolescents increases from early to late adolescents, and into young adulthood [5].
Two recent systematic reviews assessed the effectiveness of manual therapy to treat a number of conditions including back pain in children and adolescents, but a judgement of effectiveness was precluded due to limited and low-quality evidence (e.g., 4 studies including one case series and one cohort study without a control group in Prevost et al. [2019] review and only one study in Driehuis et al. [2019] review) [6, 7]. Another systematic review and meta-analysis evaluating the effectiveness of conservative interventions for LBP in children and adolescents reported that exercise interventions may be promising for improving pain intensity in children compared to no treatment. However, this review included studies with mixed neck, shoulder and back pain participants, and given their literature search is outdated (included studies until 2013), this evidence needs updating [8].
To inform healthcare professionals in a variety of clinical, rehabilitation or community settings for evidence-based care, we conducted an integrative systematic review of quantitative, qualitative, and economic evidence regarding the rehabilitative management of back pain (including TSP and LBP) in children and adolescents aged 19 years and younger.
Methods
We registered our protocol on the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42019135009) and published it in BMJ Open [9]. We reported our systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Additional file 1) [10], and the Synthesis Without Meta-analysis (SWiM) reporting guideline [10].
Eligibility criteria
Our review included studies that: 1) enrolled children and adolescents (aged 19 years or younger) with non-specific LBP or TSP; 2) investigated rehabilitation interventions (Table 1); 3) compared the intervention of interest with other conservative interventions, placebo or sham, wait list, standard care, and no intervention (including intervention of interest as an addition to active comparison interventions where the attributable effect of the comparison interventions can be isolated); and 4) reported patient-important outcomes related to functioning as described by the International Classification of Functioning, Disability and Health (ICF) framework [11] domains body functions and structures (to describe a child’s impairment such as pain), and activities and participation (to describe a child’s functional status and involvement in life situations), adverse events, cost measures or qualitative outcomes (Table 2). We used the Convention on the Rights of the Child and the WHO definitions of children (< 18 years of age) and adolescents (10–19 years of age) [12, 13].
The rehabilitation process is designed to assist individuals in regaining, improving, or maximizing functioning and quality of life after experiencing injuries, surgeries, diseases, or other health-related issues [14]. It encompasses a diverse range of interventions (single or in combination) and clinical disciplines, tailored to the specific needs of each individual. The ultimate goal of a rehabilitation process is to facilitate the highest level of independence and participation in daily life, school, work, and leisure activities, adapting to limitations when necessary and enhancing overall well-being. For instance, a person recovering from a low back injury might engage in a rehabilitation process that includes education on back care, targeted exercises, spinal manipulation, and psychological support to manage pain and promote re-engagement in daily activities, exemplifying a holistic approach to recovery.
Given the comprehensive nature of the rehabilitation process, our systematic review remains open to the inclusion of studies that might focus on specific aspects of the rehabilitation process, including those that emphasize pain relief as a primary outcome. Recognizing pain as a significant barrier to participation and engagement in rehabilitation activities, studies dedicated to understanding and managing pain are considered valuable. Effective pain management is not only critical for the immediate relief of symptoms but also plays a crucial role in enabling individuals to actively participate in their rehabilitation journey and achieve long-term goals of independence and improved quality of life. Such an approach is aligned with the World Health Organization's person-centered perspective on rehabilitation, which emphasizes addressing the most pressing needs of individuals undergoing rehabilitation, including pain management [11].
We included randomized controlled trials (RCT), cohort studies, case–control studies, and mixed-methods studies (quantitative component) for effectiveness and safety of interventions; qualitative and mixed-methods studies (qualitative component) for users’ experiences, preferences, expectations, and valued outcomes of interventions; and trial- and model-based full economic evaluations for cost-effectiveness of interventions (Table 2).
Information sources
A health sciences librarian developed search strategies reviewed by a second health sciences librarian, using the Peer Review of Electronic Search Strategies (PRESS) checklist [15, 16]. The searches included a combination of subject headings specific to databases (e.g., MeSH in MEDLINE) and free text words to capture the key concepts of rehabilitative management of back pain in children and adolescents (Additional file 2).
We searched the following databases from inception to June 16, 2023: MEDLINE (Ovid), Embase (Ovid), PsycINFO (Ovid), CINAHL (EBSCOhost), the Index to Chiropractic Literature (Chiropractic Library Collaboration), the Cochrane Controlled Register of Trials (Ovid), and EconLit (EBSCOhost).
To mitigate the potential impact of publication bias, we further searched: 1) reference lists of included studies and relevant systematic reviews; 2) three websites (the Canadian Paediatric Society, the American Academy of Pediatrics, the European Paediatric Association); and 3) the WHO International Clinical Trials Registry Platform [17]. We included studies in any language.
Screening for eligibility
We conducted training exercises prior to initiating the screening process. Reviewers screened a random sample of 50 titles/abstracts and 25 full-text articles. Paired reviewers reached ≥ 90% agreement before starting screening [18].
Pairs of reviewers independently screened titles and abstracts retrieved from electronic databases, and subsequently the full text of each selected article to confirm inclusion. Paired reviewers discussed disagreements to reach consensus, involving a third reviewer, if necessary.
Furthermore, one reviewer screened reference lists of included studies and relevant systematic reviews, the three websites, and protocols retrieved from the WHO International Clinical Trials Registry Platform. A second reviewer reviewed the screening performed by the first reviewer. Disagreements were resolved through discussion.
Risk of bias in individual studies
We assessed the quality of studies using the Cochrane Risk of Bias (ROB) 1 tool [19] for RCTs; the risk of bias tool for nonrandomised studies for interventions (ROBINS-I) for cohort studies [20]; and the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for qualitative studies [21]. We categorized the validity or credibility of each study as either low risk of bias, unclear or high risk of bias. Paired reviewers independently assessed the eligible studies for quality. We contacted one author to request additional data for clarification [22]. Any disagreements between reviewers were resolved through discussion or with a third reviewer.
Data items and data extraction process
Paired reviewers independently extracted the data from all eligible studies and solved disagreements through discussion or a third reviewer. For the quantitative studies, we extracted data on the study and participant characteristics; intervention and comparator intervention characteristics using the Template for Intervention Description and Replication (TIDieR) checklist [23]; outcomes according to the ICF categories [24,25,26]; adverse events; key findings; and methodological quality. We used the PerSPecTIF question formulation framework to guide data extraction for the qualitative studies regarding the items: perspective, setting, phenomenon of interest, environment, timing, and findings (e.g., themes) [27].
Data synthesis
We used a sequential approach at the review level to synthesize and integrate the data [28]. This involved separate quantitative and qualitative findings synthesis followed by integration of the resultant quantitative and qualitative evidence.
Quantitative synthesis
We assessed clinical heterogeneity among studies. Differences in populations, interventions, comparators, or outcomes across studies resulted in clinical heterogeneity.
To quantify the effectiveness of interventions, effect estimates (e.g., mean differences [MD], odds ratio or relative risk) and precision of the estimate (95% confidence interval [CI]) were extracted or computed. This systematic review used two criteria to determine whether an intervention was effective: 1) precision of the estimate and 2) magnitude of the estimate. Generally, differences were considered statistically significant if the 95% CI excluded zero in the mean difference (MD) or one in a risk ratio. An effect estimate of at least 10% of the range of the scale (for mean differences or median scores) or at least 10% difference for dichotomous outcomes, was considered clinically important [29]. We described the effectiveness of interventions as either “improve/reduce” or “make little difference” to outcomes in comparison to placebo/sham, control or another intervention (Table 3). An intervention was considered to “improve/reduce” outcomes (depending on direction) versus the comparison if the effect estimate was clinically important, and its 95% CI was statistically significant. An intervention was considered “make little difference” to outcomes versus the comparison if the effect estimate was: 1) not clinically important; or 2) the 95% CI was not statistically significant. We assessed the safety of interventions by identifying and categorizing adverse events reported in studies.
We applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach to assess the certainty of evidence for each outcome (Table 4) [30]. Recognizing the unique challenges of rehabilitation research, we adapted our application of GRADE to emphasize a context-sensitive analysis across five key domains: risk of bias, imprecision, publication bias, inconsistency, and indirectness, as suggested by Cancelliere et al. (2023) [31]:
-
1.Risk of Bias: We assessed the risk of bias in individual studies, understanding that the internal validity of studies is crucial for confidence in our findings. High-quality (low risk of bias) studies were prioritized to ensure the credibility of our evidence synthesis.
-
2.Imprecision: We evaluated the precision of effect estimates, paying close attention to the width of confidence intervals, while also taking into account minimal clinically important differences.
-
3.Publication Bias: To mitigate the potential for publication bias, we systematically searched for and included studies from a broad range of sources, including reference lists of included studies and relevant systematic reviews, targeted websites, and the World Health Organization International Clinical Trials Registry Platform.
-
4.Inconsistency: Given the expected challenge of achieving clinical homogeneity in context-sensitive research like ours, we anticipated findings from only one study per PICO question. Therefore, we did not automatically downgrade the certainty of evidence for inconsistency if only one study was available. We recognized the inherent heterogeneity of rehabilitation interventions and their outcomes, prompting us to judiciously evaluate the homogeneity (or lack thereof) among populations, interventions, comparators, and outcomes across studies before deciding on meta-analyses or opting for a descriptive synthesis approach when more appropriate.
-
5.Indirectness: We addressed indirectness by using clear and focused eligibility criteria to enhance the applicability of our findings to the target patient population. We ensured the evidence directly addressed our research question by confirming the direct relevance of populations, interventions, comparators, and outcomes to our clinical focus.
Integration of quantitative and qualitative evidence
We integrated the evidence by juxtaposing findings in a matrix to generate hypotheses regarding the effectiveness and safety of rehabilitation interventions for LBP in children and adolescents [28].
Results
Study selection
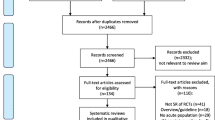
We screened 8461 citations and 307 full-text articles, and included 11 studies (Fig. 1). Of these 11 studies, the effectiveness of rehabilitation interventions were investigated in 10 quantitative studies including eight RCTs (518 participants) [22, 32,33,34,35,36,37,38,39] and two non-randomized clinical trials (40 participants) [40, 41] (Table 5), and one qualitative study investigated patients’ experience of physiotherapy (14 Participants) [42] (Table 6). We did not identify studies on cost-effectiveness of rehabilitation interventions. One RCT was reported in two full text articles [35, 36]. Two hundred ninety-five articles were excluded based on full text screening due to: 1) ineligible research question (8 articles); 2) ineligible population (238 articles); 3) ineligible intervention (2 articles); 4) ineligible outcome (3 articles); 5) ineligible study designs (36 articles); 6) duplicates (7 articles); and 7) cannot retrieve (1 article) (Additional file 3).
Study characteristics
Quantitative studies (Table 5)
The mean age of participants ranged from 12.3 to 18 years old. Among participants in the eight studies reporting sex, 50.4% (n= 261) were female [22, 32,33,34, 37, 38, 40, 41]. All studies included participants with nonspecific LBP, with no studies focusing on TSP. Participants received various rehabilitation interventions including exercise (4 studies) [34,35,36, 39, 40], spinal manipulation (2 studies) [22, 33], cognitive therapy (1 study) [38], whole-body vibration (1 study) [37], and multimodal care (2 studies) [32, 41]. The duration of rehabilitation interventions varied: 1) four weeks (1 study) [22]; 2) eight weeks (4 studies) [34,35,36, 38, 40]; and 3) 12 weeks (4 studies) [32, 33, 37, 39]; and 4) variable duration (1 study) [41]. These 10 studies investigated rehabilitation interventions: 1) as an addition to active comparison interventions where the attributable effect of the comparison interventions can be isolated (4 studies) [32, 33, 37, 39]; 2) compared to no treatment (3 studies) [34,35,36, 38]; 3) compared to sham (1 study) [22]; and 4) compared to other active interventions (2 studies) [40, 41], respectively. Outcomes included LBP intensity (9 studies) [22, 32,33,34,35,36,37,38,39,40], function (5 studies) [22, 32, 33, 38, 41], quality of life (2 studies) [32, 33], improvement (2 studies) [22, 33], satisfaction (1 study) [33], wellbeing (1 study) [34], feelings about school and life (1 study) [34], absence from school or physical activity (1 study) [35], and health resource utilization (1 study) [22]. The 10 studies were clinically heterogeneous, therefore, a meta-analysis was not conducted [43].
Qualitative study (Table 6)
The qualitative study used grounded theory methodology to explore the experience of adolescents (aged 12–18 years) with LBP who received individually tailored physical therapy and home exercise [42].
Risk of bias assessment
Among eight RCTs, one was rated as overall unclear risk of bias [33] and seven were rated as high risk of bias [22, 32, 34,35,36,37,38,39] (Table 7, Risk of Bias Assessment of Included Studies). The two non-randomized clinical trials were rated as overall serious risk of bias (Table 8, Risk of Bias Assessment of Included Studies) [40, 41]. One qualitative study was rated as overall low risk of bias (Table 9) [42].
Synthesis of quantitative studies
Spinal manipulation
Two RCTs evaluated the effectiveness of spinal manipulation in adolescents with LBP [22, 33]. (Table 10).
Spinal manipulation and exercise versus same exercise
One RCT compared spinal manipulation (1–2 sessions/week over 12 weeks) plus exercise (12 weeks) to the same exercise [33].
For pain, immediately following a 12-week treatment, participants in the spinal manipulation group were more likely to experience a clinically important reduction (RR 2.15 [1.16, 3.98] for 75% pain reduction, moderate certainty evidence; and RR 2.68 [1.01, 7.12] for 100% pain reduction, low certainty evidence). Similar results were observed immediately and at 3 and 9 months following the 12-week treatment, with the largest effect size at 3 months and smallest at 9 months following the treatment. For details, see Table 10 and Additional file 4.
Twelve-week spinal manipulation made little difference to function (RMDQ, MD 0.54 [-0.25, 1.34]), quality of life (PedsQL, MD 1.33 [-1.64, 4.31]), patient-reported improvement (a 9-point scale, MD -0.29 [-0.66, 0.09]) or satisfaction (a 7-point scale, MD -0.36 [-0.65, -0.07]) immediately following the treatment (moderate certainty evidence). Similar results were observed at 3 months or 9 months following the treatment (moderate certainty evidence). For details, see Table 10 and Additional file 4.
Due to very low certainty evidence, it is uncertain whether participants in spinal manipulation plus exercise group and exercise alone group had similar chance of experiencing adverse events (RR 1.00 [0.16, 6.30]).
Spinal manipulation and exercise versus sham manipulation and same exercise
One RCT compared spinal manipulation (2 sessions in total over one week) and exercise (4 weeks) to sham spinal manipulation and the same exercise [22].
For pain, two sessions of spinal manipulation made little difference to LBP intensity (measured by scale 0–10 on numerical rating scale [NRS]) immediately following the treatment (MD -0.58 [-1.49, 0.33]) and at 5 months following the treatment (MD -0.26 [-0.82, 0.31]) (low to moderate certainty evidence).
Low certainty evidence suggests that spinal manipulation made little difference to function (PSFS) immediately following the treatment (MD 2.8 [-0.91, 5.51]) and at the 5 months following the treatment (MD 1.08 [-2.2, 4.36], PFPS), and improvement (Global Rating of Change) (MD 0.66 [-0.95, 2.27]) immediately following the treatment.
Due to very low certainty evidence, it is uncertain whether participants in both the spinal manipulation and sham groups were equally likely to use health resources (RR 0.59 [0.25, 1.39], by evaluation of seeking additional treatment for LBP during follow-up period) or have a recurrence of symptoms (RR 0.77 [0.45, 1.30], significant enough to impair participation during follow-up period).
Due to very low certainty evidence, it is uncertain whether participants in the spinal manipulation group and sham group had an equal chance of experiencing adverse events [22].
Group-based exercise
Four RCTs evaluated the effectiveness of group-based exercise in adolescents with LBP [34,35,36, 39, 40]. (Table 10, Additional file 4).
Group-based exercise, monthly personal tailored exercise and home-based exercise versus monthly personal tailored exercise and home-based exercise
One RCT compared group-based exercise (one session/week over 12 weeks) combined with monthly personal tailored exercise and home-based exercise to the same monthly exercise and home-based exercise [39]. It is uncertain whether the addition of weekly group exercise made little difference to LBP intensity (MD -1.2 [-2.65, 0.25], scale range 0–10 on a Visual Analogue Scale [VAS]; very low certainty evidence) immediately following the 12-week treatment.
Group-based exercise versus no treatment
Two RCTs compared group-based progressive exercise provided at school for eight weeks to no treatment34-36.
For pain, low certainty evidence suggests that group-based exercise reduced pain immediately following the treatment (MD -2.3 [-3.1 to -1.5]; scale range 0 to 10 on NRS; 1 RCT) [35, 36]. However, at 4 weeks following the treatment, it is uncertain whether group-based exercise reduced pain (MD -1.50 [-2.68, -0.32]; scale range 0 to 10 on VAS), or whether participants in group-based exercise group were less likely to have LBP (RR 0.74 [0.57, 0.94]; 1 RCT) [34]. Low certainty evidence from the same study suggests that group-based exercise participants were less likely to have LBP at 4 months following the treatment (RR 0.52 [0.34, 0.78]; 1 RCT) [34].
For absence from school, group-based exercise made little difference to absence from school during the past seven days (MD 0 [-0.1, 0.1]; low certainty evidence, 1 RCT) immediately following the treatment [35, 36]. For absence from physical activity, due to very low certainty evidence (1 RCT), it is uncertain whether group-based exercise made little difference to absence from physical activity during the past seven days (MD 0.6 day [-1, 0.2]) immediately following the treatment [35, 36].
For well-being, group-based exercise made little difference at 4 weeks following the treatment (MD 0 [-1.69, 1.69], scale range 5–30 on the Mental Health Inventory-5 (MHI-5), 30 = psychosocial well-being; 1 RCT, low certainty evidence) [34]. Similar results were observed for well-being, and feelings about school and life at 4 weeks and 4 months following the 8-week group exercise. For details, see Table 10 and Additional file 4.
Group-based exercise versus advice and individual training
One non-randomized clinical trial compared 8-week group-based muscle control exercise to advice and individual training [40]. Due to very low certainty evidence, it is uncertain whether group-based exercise reduced days with pain during the four weeks period immediately after the 8-week treatment (between-group mean difference not reported). Due to very low certainty evidence, it is uncertain whether group-based exercise made little difference to maximum and median pain intensity during the four weeks after the 8-week treatment (between-group mean difference not reported).
Whole-body vibration
Whole-body vibration and trunk stabilization exercise versus trunk stabilization exercise
One RCT evaluated whole-body vibration when added to trunk stabilization exercise in adolescents with LBP, it is uncertain whether its addition made little difference to LBP intensity when compared to trunk muscle stabilization exercise alone (MD -0.66 [-1.27, -0.05], scale range 0–10 on NRS; very low certainty evidence) immediately following a 12-week treatment among adolescents [37]. (Table 10, Additional file 4).
Cognitive functional therapy
Cognitive functional therapy versus no treatment
One RCT compared cognitive functional therapy to no treatment in adolescents with LBP [38]. Due to very low certainty evidence, it is uncertain whether 8 weeks of cognitive functional therapy 1) reduced LBP intensity following a 15-min ergometer trial immediately post-intervention (MD -2.4 [-4.1, -0.63], scale range 0 to 10 on NRS); and 2) improved function immediately following the treatment (MD 4.1 [0.9, 7.3], scale range 0–30 on PFPS, 30 = no function limitation) and four weeks after the 8-week treatment (MD 4.0 [0.8, 7.2], PFPS). (Table 10, Additional file 4).
Multimodal care
One RCT and one non-randomized controlled trial evaluated the effectiveness of multimodal care in adolescents with LBP [32, 41]. (Table 10, Additional file 4).
Multimodal care, home exercise and education versus home exercise and education
One RCT compared multimodal care (including supervised exercise; manual therapy and mechanical diagnostic therapy as needed) plus home exercise and education to the same home exercise and education [32].
Due to very low certainty, it is uncertain whether the addition of multimodal care made little difference to LBP intensity (MD -0.5 [-3.9, 2.9], scale range 0–10 on VAS) and quality of life measured by Child Health Questionnaire-Child Form (no standard deviation or 95%CI reported) when compared to home exercise and education alone immediately following a 12-week treatment.
For function, multimodal care did not improve function when compared to home exercise and education alone (MD -0.8 (-2.31, 0.7), scale range 0–24 on RMDQ) immediately following a 12-week treatment (low certainty evidence).
Physiotherapist-led multimodal care (exercise, manual therapy, modalities for pain) versus physician-led care
One non-randomized clinical trial compared physiotherapist-led care (exercise, manual therapy, modalities for pain) to physician-led care (including physiotherapy). The mean days of care provided was 62 days. It is uncertain whether multimodal care made little difference to function (MD 6 [-13.22, 25.22], scale range 0–100 on Micheli Functional Scale; very low certainty evidence) [41].
Summary of quantitative findings
There is low to moderate certainty evidence that spinal manipulation (1–2 sessions/week over 12 weeks) and exercise may be associated with a greater likelihood of experiencing clinically important pain reduction versus exercise alone immediately following the intervention and in the short-term in adolescents with LBP [33]. There is very low to low certainty evidence that group-based exercise programs (over 8 weeks) may reduce pain immediately post-intervention and in the short-term in adolescents with LBP [34,35,36, 40]. Due to very low certainty evidence, the clinical benefit of cognitive functional therapy in improving pain and function is uncertain [38]. The three interventions included an education component and reasonable compliance of the interventions was achieved.
There is low certainty evidence that multimodal care (including supervised exercise; manual therapy and mechanical diagnostic therapy as needed) may not bring additional benefit in improving function when added to home exercise and education [32]. It is uncertain whether the addition of whole-body vibration made little difference to pain intensity when compared to trunk muscle stabilization exercise alone (very low certainty evidence) [37].
Findings of qualitative study
The qualitative study explored the experiences of adolescents with LBP treated by individually tailored physical therapy and home exercise [42]. A core category, mobilizing own resources, emerged from the analysis, describing how adolescents with LBP succeed in managing their main concern, gaining body confidence, in daily life. The core category was divided into four categories labelled: 1) coaching from the physiotherapist, 2) seeking for information, 3) compliance with physiotherapy, and 4) gaining energy from pain-free moments (Table 6). Information-seeking is related to information available to participants that enhance their understanding and leads to change. Compliance with treatment refers to tailored exercises with the physiotherapist restoring control to participants on physical as well as psychological levels, which prompted them to return for the next appointment.
Integration of quantitative and qualitative evidence
We used a joint display table to illustrate the connection between quantitative and qualitative results (Table 11). The interventions evaluated in four quantitative studies fulfilled subcategories 2 and 3 (i.e., seeking for information, compliance with treatment) (Table 11) [33, 34, 38, 40]. These interventions improved pain intensity and/or function (very low to moderate certainty evidence). Interventions evaluated in other six quantitative studies did not fulfill at least one of the two subcategories [22, 32, 35,36,37, 39, 41, 42]. All these interventions except one (group-based exercise) [35, 36] did not bring benefit or additional benefit if combined with other interventions.
Discussion
There is evidence of clinical benefit from spinal manipulation (low to moderate certainty) and group-based exercise (very low to low certainty). Multimodal care did not appear to be beneficial (very low to low certainty), and the benefit of both cognitive therapy and whole-body vibration were uncertain (very low certainty). Qualitative findings suggest that seeking/receiving information and compliance with treatment are important factors to mobilize own resources to manage in daily life.
Only two studies evaluated adverse events [22, 33]. Due to very low certainty evidence, it is uncertain whether participants receiving spinal manipulation and participants without spinal manipulation had similar likelihood of adverse events.
We identified neither studies on TSP, mixed methods studies, nor economic studies in children and adolescents.
Strengths and limitations
This systematic review has strengths. First, this review included comprehensive and peer-reviewed literature search strategies and examined all non-surgical rehabilitation interventions without language restrictions. Second, this review used a definition of rehabilitation as proposed by Cochrane Rehabilitation, which allowed us to capture what can be considered components of broader rehabilitation interventions that are provided within the rehabilitation process.
Due to limited number of relevant studies and clinical heterogeneity, a meta-analysis could not be conducted. Second, it was challenging to apply GRADE to the included studies to examine rehabilitation interventions due to clinical heterogeneity and blinding issues caused by the nature of rehabilitation interventions. Therefore, we adapted the GRADE approach and tailored it to rehabilitation studies.
Comparison to other systematic reviews and guideline
There are three systematic reviews identified in evaluating rehabilitation interventions for the management of LBP in pediatric population published between 2014 and 2019 [6,7,8]. Our review agreed with the systematic review by Michaleff et al. (2014) [8] suggesting that a supervised exercise program was better than no treatment. We augmented this conclusion by adding one non-randomized clinical trial [40]. However, we do not agree that a supervised exercise program reduces absences from physical activity due to a non-clinical important change [35, 36]. The systematic review by Driehuis et al. (2019) [6] suggested spinal manipulation did not bring adverse events; however, our review found the certainty of evidence is very low. Further studies are needed before making a conclusion about adverse events associated with spinal manipulation. Driehuis et al. did not identify studies on the effectiveness of spinal manipulation for LBP. Last, both Prevost et al. (2019) [7] and our review found that spinal manipulation reduced LBP intensity. Our review further clarified that spinal manipulation (1–2 sessions/week over 12 weeks) combined with exercise is probably associated with a greater likelihood of experiencing clinically important pain reduction immediately following the intervention and over the short-term versus exercise alone [33]. In addition to all the three reviews, we identified studies on the effectiveness of cognitive functional therapy, whole-body vibration and multimodal care.
Implications
The findings in our review have important implications for clinical practice. First, as evident in the included qualitative study, the patient-doctor relationship should be highlighted, providing a foundation for a positive interaction that may facilitate increased compliance with treatment towards the goal of recovery (i.e., subcategories 2 and 3: coaching from care providers, compliance with treatment) [42]. Second, information provided via education/advice should be considered as part of care program [44]. Third, spinal manipulation and group-based exercise may be considered through shared decision-making to reduce pain intensity in adolescents with LBP based on low to moderate certainty evidence [33,34,35,36].
Compared to previous reviews, evidence is expanding. However, future studies with rigorous methodological quality are still needed. Two previous systematic reviews only identified four studies (including one case series and one cohort study without a control group) [7] and one study [6], respectively. Our review identified 10 quantitative studies (i.e., 8 RCTs, 2 non-randomized clinical trials) and one qualitative study. Of those, nine quantitative studies had high risk of bias. Specifically, blinding of participants, treatment providers and outcome assessors (e.g., participants for self-reported outcomes) are the main challenge in the included RCTs. This challenge is due to the nature of rehabilitation interventions. To minimize potential biases caused by these issues, future RCTs can be restricted to participants who are naïve to the studies interventions [31]. Alternatively, future RCTs can consider measuring treatment credibility/expectancy and blinding, and consider these in the analysis and interpretation of potential biases and the implications on intervention effect estimates [31]. Furthermore, apart from RCTs, future studies can consider various study designs (e.g., quasi-experimental design, qualitative, mixed methods, and implementation studies) depending on the research question [31]. These study designs can complement the evidence obtained from RCTs, therefore contributing to a more holistic perspective on the evaluation of benefits and harms, specifically for a context-sensitive condition (e.g., LBP). For example, qualitative studies can explore patients’ lived experiences and assist better understanding of evidence from RCTs regarding treatment effects, compliance etc.
Conclusion
Spinal manipulation and group-based exercise may be beneficial in reducing LBP intensity in adolescents based on evidence ranging from very low to moderate certainty. Education should be provided as part of a care program. Studies with rigorous methodological quality are needed.
Availability of data and materials
All data generated/analysed in this systematic review are included in this published systematic review and its supplementary information files.
Abbreviations
- 95%CI:
-
95% Confidence interval
- JBI critical appraisal checklist:
-
The Joanna Briggs Institute Critical Appraisal Checklist
- LBP:
-
Low back pain
- MD:
-
Mean difference
- MHI-5:
-
Mental Health Inventory-5
- NRS:
-
Numerical rating scale
- PedsQL:
-
Pediatric Quality of Life Inventory
- PRESS:
-
The Peer Review of Electronic Search Strategies
- PRISMA:
-
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO:
-
The International Prospective Register of Systematic Reviews
- PSFS:
-
Patient Specific Functional Scale
- RCT:
-
Randomized controlled trial
- RMDQ:
-
Roland Morris Disability Questionnaire
- ROB 1 tool:
-
The Cochrane Risk of Bias 1 tool
- ROBINS-I:
-
The risk of bias tool for nonrandomised studies for interventions
- RR:
-
Relative risk
- SWiM:
-
The Synthesis Without Meta-analysis
- TIDieR:
-
The Template for Intervention Description and Replication checklist
- TSP:
-
Thoracic spine pain
- VAS:
-
Visual analog scale
References
Calvo-Munoz I, Gomez-Conesa A, Sanchez-Meca J. Prevalence of low back pain in children and adolescents: a meta-analysis. BMC Pediatr. 2013;13:14.
Jeffries LJ, Milanese SF, Grimmer-Somers KA. Epidemiology of adolescent spinal pain: a systematic overview of the research literature. Spine (Phila Pa 1976). 2007;32(23):2630–7.
Dissing KB, Hestbaek L, Hartvigsen J, Williams C, Kamper S, Boyle E, et al. Spinal pain in Danish school children - how often and how long? The CHAMPS Study-DK. BMC Musculoskelet Disord. 2017;18(1):67.
Santos VS, Leite MN, Camargo BIA, Saragiotto BT, Kamper SJ, Yamato TP. Three in Every 10 School-aged Children in Brazil Report Back Pain in Any Given Year: 12-Month Prospective Cohort Study of Prevalence, Incidence, and Prognosis. J Orthop Sports Phys Ther. 2022;52(8):554–62.
Roy R, Galán S, Sánchez-Rodríguez E, Racine M, Solé E, Jensen MP, et al. Cross-National Trends of Chronic Back Pain in Adolescents: Results From the HBSC Study, 2001–2014. J Pain. 2022;23(1):123–30.
Driehuis F, Hoogeboom TJ, Nijhuis-van der Sanden MWG, de Bie RA, Staal JB. Spinal manual therapy in infants, children and adolescents: A systematic review and meta-analysis on treatment indication, technique and outcomes. PLoS One. 2019;14(6):e0218940.
Parnell Prevost C, Gleberzon B, Carleo B, Anderson K, Cark M, Pohlman KA. Manual therapy for the pediatric population: a systematic review. BMC Complement Altern Med. 2019;19(1):60.
Michaleff ZA, Kamper SJ, Maher CG, Evans R, Broderick C, Henschke N. Low back pain in children and adolescents: a systematic review and meta-analysis evaluating the effectiveness of conservative interventions. Eur Spine J. 2014;23(10):2046–58.
Cancelliere C, Wong JJ, Yu H, Mior S, Brunton G, Shearer HM, et al. Rehabilitative management of back pain in children: protocol for a mixed studies systematic review. BMJ Open. 2020;10(10):e038534.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
World Health Organization. International Classification of Functioning, Disability and Health: Children and Youth Version: ICF-CY. Geneva: World Health Organization; 2007. Available online: http://apps.who.int/iris/bitstream/10665/43737/1/9789241547321_eng.pdf. Accessed 2 May 2024.
The World Health Organization. [Available from: https://www.who.int/health-topics/adolescent-health#tab=tab_1.
Unicef. Convention on the Rights of the Child, 20 November 1989. Annu Rev Popul Law. 1989;16:95:485–501.
Negrini S, Selb M, Kiekens C, Todhunter-Brown A, Arienti C, Stucki G, et al. Rehabilitation Definition for Research Purposes: A Global Stakeholders’ Initiative by Cochrane Rehabilitation. Am J Phys Med Rehabil. 2022;101(7):e100–7.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6.
Sampson M, McGowan J, Cogo E, Grimshaw J, Moher D, Lefebvre C. An evidence-based practice guideline for the peer review of electronic search strategies. J Clin Epidemiol. 2009;62(9):944–52.
Godin K, Stapleton J, Kirkpatrick SI, Hanning RM, Leatherdale ST. Applying systematic review search methods to the grey literature: a case study examining guidelines for school-based breakfast programs in Canada. Syst Rev. 2015;4:138.
Belur J, Tompson L, Thornton A, Simon M. Interrater reliability in systematic review methodology: exploring variation in coder decision-making. Sociol Methods Res. 2021;50(2):837–65.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. 2015;13(3):179–87.
Selhorst M, Selhorst B. Lumbar manipulation and exercise for the treatment of acute low back pain in adolescents: a randomized controlled trial. J Man Manip Ther. 2015;23(4):226–33.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
Cieza A, Brockow T, Ewert T, Amman E, Kollerits B, Chatterji S, et al. Linking health-status measurements to the International Classification of Functioning. Disability and Health J Rehabil Med. 2002;34(5):205–10.
Cieza A, Fayed N, Bickenbach J, Prodinger B. Refinements of the ICF Linking Rules to strengthen their potential for establishing comparability of health information. Disabil Rehabil. 2019;41(5):574–83.
Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustun B, Stucki G. ICF linking rules: an update based on lessons learned. J Rehabil Med. 2005;37(4):212–8.
Booth A, Noyes J, Flemming K, Moore G, Tuncalp O, Shakibazadeh E. Formulating questions to explore complex interventions within qualitative evidence synthesis. BMJ Glob Health. 2019;4(Suppl 1):e001107.
Harden A, Thomas J, Cargo M, Harris J, Pantoja T, Flemming K, et al. Cochrane Qualitative and Implementation Methods Group guidance series-paper 5: Methods for integrating qualitative and implementation evidence within intervention effectiveness reviews. J Clin Epidemiol. 2018;97:70–8.
Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW. Spinal manipulative therapy for acute low-back pain. Cochrane Database Syst Rev. 2012;2012(9):Cd008880.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Cancelliere C, Yu H, Southerst D, Connell G, Verville L, Bussières A, et al. Improving Rehabilitation Research to Optimize Care and Outcomes for People with Chronic Primary Low Back Pain: Methodological and Reporting Recommendations from a WHO Systematic Review Series. J Occup Rehabil. 2023;33(4):673–86.
Ahlqwist A, Hagman M, Kjellby-Wendt G, Beckung E. Physical therapy treatment of back complaints on children and adolescents. Spine (Phila Pa 1976). 2008;33(20):E721-7.
Evans R, Haas M, Schulz C, Leininger B, Hanson L, Bronfort G. Spinal manipulation and exercise for low back pain in adolescents: a randomized trial. Pain. 2018;159(7):1297–307.
Fanucchi GL, Stewart A, Jordaan R, Becker P. Exercise reduces the intensity and prevalence of low back pain in 12–13 year old children: a randomised trial. Aust J Physiother. 2009;55(2):97–104.
Jones M, Stratton G, Reilly T, Unnithan V. The efficacy of exercise as an intervention to treat recurrent nonspecific low back pain in adolescents. Pediatr Exerc Sci. 2007;19(3):349–59.
Jones MA, Stratton G, Reilly T, Unnithan VB. Recurrent non-specific low-back pain in adolescents: the role of exercise. Ergonomics. 2007;50(10):1680–8.
Jung KS, Jung JH, In TS, Cho HY. The Effectiveness of Trunk Stabilization Exercise Combined with Vibration for Adolescent Patients with Nonspecific Low Back Pain. Int J Environ Res Public Health. 2020;17(19):7024.
Ng L, Cañeiro JP, Campbell A, Smith A, Burnett A, O’Sullivan P. Cognitive functional approach to manage low back pain in male adolescent rowers: a randomised controlled trial. Br J Sports Med. 2015;49(17):1125–31.
Vitman N, Hellerstein D, Zeev A, Gilo Y, Nakdimon O, Peretz A, et al. A Comparison between Different Types and Frequency of Physiotherapy Treatment for Children and Adolescents with Postural Problems and Low Back Pain. Phys Occup Ther Pediatr. 2022;42(2):215–26.
Harringe ML, Nordgren JS, Arvidsson I, Werner S. Low back pain in young female gymnasts and the effect of specific segmental muscle control exercises of the lumbar spine: a prospective controlled intervention study. Knee Surg Sports Traumatol Arthrosc. 2007;15(10):1264–71.
Selhorst M, Rodenberg R, Padgett N, Fischer A, Ravindran R, MacDonald J. An Alternative Model of Care for the Treatment of Adolescent Athletes with Extension-Based Low Back Pain: A Pilot Study. Int J Sports Phys Ther. 2021;16(1):227–35.
Ahlqwist A, Sällfors C. Experiences of low back pain in adolescents in relation to physiotherapy intervention. Int J Qual Stud Health Well-being. 2012;7(1):15471.
Deeks JJ HJ, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors) 2023 [Available from: www.training.cochrane.org/handbook.
Haynes RB, Devereaux PJ, Guyatt GH. Physicians’ and patients’ choices in evidence based practice. BMJ. 2002;324(7350):1350.
Acknowledgements
We thank Ann Taylor-Vaisey, research associate from Ontario Tech University for developing search strategies and Kent Murnaghan, research librarian from the Canadian Memorial Chiropractic College for peer reviewing the literature search strategies and updating the literature search.
Funding
This work was supported by the Canadian Chiropractic Association (CCA).
Author information
Authors and Affiliations
Contributions
HY conceptualized and designed the study, conducted screening and data extraction, critically appraised studies, synthesized evidence, and drafted the initial manuscript. CC conceptualized and designed the study, conducted screening and data extraction, critically appraised studies, and synthesized evidence. DS conducted screening, critically appraised studies, and synthesized evidence. JJW conceptualized and designed the study, conducted screening, and critically appraised studies. LV conducted screening, critically appraised studies, and synthesized evidence. GC conducted screening and critically appraised studies. LE conducted screening, critically appraised studies, and synthesized evidence. SM critically appraised studies. LH critically appraised studies. MS critically appraised studies. GB conducted screening. HMS conducted screening and critically appraised studies. EP conducted screening and critically appraised studies. DT conducted screening and critically appraised studies. DG conducted screening. KP critically appraised studies. CCE conducted screening. All authors critically reviewed, revised and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest relevant to this article to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, H., Southerst, D., Wong, J.J. et al. Rehabilitation of back pain in the pediatric population: a mixed studies systematic review. Chiropr Man Therap 32, 14 (2024). https://doi.org/10.1186/s12998-024-00538-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12998-024-00538-z