Abstract
Purpose
Low back pain (LBP) is prevalent in military personnel. We aimed to systematically review the literature regarding risk factors for first-time LBP during military service among active duty military personnel.
Methods
We searched six electronic databases (inception-April 2020) for randomised controlled trials, cohort studies, and case–control studies published in English in peer-reviewed journals. Eligible studies were independently critically appraised by paired reviewers and a descriptive synthesis was conducted.
Results
We screened 1981 records, reviewed 118 full-text articles, and synthesised data from eight acceptable quality cohort studies. Studies assessed physical (n = 4), sociodemographic (n = 2), and/or occupational factors (n = 5) associated with LBP. Two studies reported prior LBP was associated with a greater than twofold increased risk of LBP compared to those without prior LBP. Other factors consistently associated with LBP included previous musculoskeletal injury (n = 2), less time spent on physical training (n = 2), female sex (n = 2), and lower rank (n = 2). Factors associated with LBP from single studies included marital status, lower education level, blast injury, job duties, and service type. We found inconsistent associations for performance on physical fitness tests, age, and occupation type. Psychological risk factors were not assessed in any included studies.
Conclusion
In active duty personnel, prior history of LBP, previous musculoskeletal injury, less time in physical training, female sex, and lower rank were consistent risk factors for LBP. This information is relevant for researchers, active duty military personnel, and other decision makers. Future studies should explore causal relationships for LBP in this population.
PROSPERO registration number: CRD42018084549.
Similar content being viewed by others
Introduction
Musculoskeletal (MSK) disorders, particularly low back pain (LBP), are highly prevalent and are one of the leading causes of disability in the general population [1, 2]. Similarly, the prevalence of LBP in military personnel is also high [3, 4]. An analysis of the United States (U.S.) Navy and Marine Corps Physical Evaluation Boards over a 1-year period demonstrated that MSK disorders were the most frequently diagnosed condition (43%), with back pain being the most frequently identified MSK disorder (29%) [5]. In the U.S. active duty military population, the overall incidence rate of LBP was 40.5 per 1000 person-years over an 8-year period [6]. However, the true burden of MSK disorders and LBP in this population may actually be higher, as there may be an underreporting of MSK injuries due to the fear of affecting future career opportunities [7]. Musculoskeletal disorders are a substantial financial burden [8], a common reason for medical evacuation during military duty, and reduce the probability of return to duty [9].
A variety of risk factors for LBP in the general population have been identified from previous systematic reviews [10, 11]. Specifically for workers, some occupational demands such as heavy lifting, awkward postures, and bending may be risk factors for LBP, although a causal relationship has not yet been determined [12,13,14]. While these reviews have looked at risk factors for LBP in various occupational settings, to our knowledge, no reviews have looked specifically at risk factors for LBP in the active duty military population. Given that the burden of LBP is high in this population and that their daily tasks are both physically and psychologically demanding, there is a need to better understand factors that may contribute to the development of LBP in this population. By understanding risk factors for LBP, prevention strategies may be developed and targeted to reduce the burden of LBP in active duty military personnel.
Therefore, the objective of this study was to critically appraise and synthesise the literature examining risk factors of incident LBP in active duty military personnel.
Methods
Study design
The systematic review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Additional file 1) [15]. The protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) [16] on January 16, 2018 and updated on August 28, 2020 (registration no. CRD42018084549).
Search strategy
The search strategy was developed in consultation with a health sciences librarian (KM) and reviewed by a second librarian using the Peer Review of Electronic Search Strategies (PRESS) Checklist [17]. The electronic databases PubMed, MEDLINE (EBSCO), Cumulative Index to Nursing and Allied Health Literature (EBSCO), Cochrane Database for Registered Trials, PsycINFO (OVID), and Embase (OVID) were systematically searched from database inception to March 2, 2018 and updated on April 15, 2020. The reference lists of all eligible articles were hand-searched to identify additional articles. Search terms consisted of subject headings specific to each database (e.g., MeSH in MEDLINE) and free text words relevant to military personnel, LBP, and risk factors (Additional file 2).
Eligibility criteria
Study population
Active military personnel were defined as individuals 16 years of age and older who were in active military duty at the time of the study. This population included members of the Armed Forces, Navy, and Air Force. Study populations of retired military personnel or those with a history of previous LBP during military service were excluded.
Risk factors
We searched for all risk factors including risk markers, predictors, and risk determinants. Risk markers are factors that are associated with an outcome of interest; predictors result from prediction model studies and may either be causal or non-causal; risk determinants are a cause of the outcome (causal modelling) [18]. We searched for risk factors in any domain, such as sociodemographic, physical, psychological, or occupational risk factors.
Outcomes
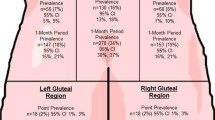
Low back pain was defined according to the European Guidelines for Prevention in Low Back Pain [19] as pain and discomfort, localised below the costal margin and above the inferior gluteal folds, with or without leg pain. Low back pain as a result of fracture/dislocation, infection, cancer, or other serious low back pathology were excluded. We included only individuals with incident LBP—defined as a new episode or first occurrence of LBP during military service. There was no minimum follow up period required for outcome assessment.
Study design
Randomised controlled trials, cohort studies, and case–control studies were included. We excluded cross-sectional studies, pilot studies, case reports or series, biomechanical studies, laboratory studies, qualitative studies, reviews (i.e., systematic reviews, meta-analyses, and narrative reviews), and guidelines.
Publication type
Articles published in English in peer-reviewed journals were included. The following publication types were excluded: protocols, letter, editorial, commentary, unpublished manuscript, dissertation, government report, book and/or book chapter, conference proceeding, meeting abstract, lecture, and consensus development statements.
Screening
All potentially relevant citations identified by the search strategy from the electronic databases were exported into EndNote X8 (Clarivate Analytics, Philadelphia, USA) for reference management and tracking of the screening process. A standardised Microsoft Excel (Microsoft Corporation, Redmond, USA) spreadsheet was used to enter results from the screening process. For the first level of screening, two reviewers (DT and MR) independently screened the titles and abstracts for all relevant and possibly relevant citations. In the second level of screening, the same reviewers independently reviewed full texts for all relevant and possibly relevant citations previously identified. Any disagreements during any phase of screening were resolved by discussion. If consensus could not be reached after discussion, a third reviewer (CC) was consulted to determine eligibility.
Critical appraisal of the literature
Eligible articles were independently appraised for risk of bias by two reviewers (DT and MR) using the Scottish Intercollegiate Guidelines Network (SIGN) criteria for cohort studies [20, 21]. No relevant randomised controlled trials or case–control studies were identified. The SIGN criteria for cohort studies prompted us to qualitatively assess items that could contribute to selection, information, and confounding bias. The SIGN criteria were used to assist reviewers in making an informed overall judgement of the internal validity of studies. In accordance with the SIGN criteria, articles were rated as either high, acceptable, or unacceptable quality. If confounding was not considered, but other relevant items were done sufficiently well, the studies were rated as “acceptable” and the studies were accepted as association studies. Articles rated as high or acceptable quality were then deemed low risk of bias, while those rated as unacceptable quality were deemed high risk of bias. Discussion was used to solve disagreements and reach consensus among the two reviewers. A third reviewer (CC) was consulted if disagreements persisted.
Data extraction, analysis, and synthesis
Data on study characteristics (e.g., author, year, study design, geographic region); participant characteristics (e.g., specific population, eligibility criteria), outcomes, risk factors assessed, and key findings from all eligible studies were extracted into a pre-piloted form by one reviewer (DT) and assessed for accuracy and completeness by another reviewer (CC). Data was extracted according to the CHARMS-PF (checklist for critical appraisal and data extraction for systematic reviews of prediction modelling studies—prognostic factors) where applicable [22]. We extracted measures of association between the risk factors and outcomes including odds ratios (OR), relative risks (RR), and hazard ratios (HR), and 95% confidence intervals (CI). If the confidence intervals were not reported, we computed them from the raw data if available. If a study included unadjusted and adjusted estimates, only adjusted estimates were extracted. Similar to previous reviews on risk factors for LBP [10, 11], risk factors were grouped into physical, sociodemographic, occupational, and psychological risk factors. They were also grouped by type of risk factor (e.g., marker, predictor, or determinant) [18].
A descriptive synthesis [23] was conducted due to the absence of adequate homogeneity across studies. We synthesised the associations between risk factors and LBP as (1) consistent association (association in the same direction demonstrated in ≥ 2 studies), (2) consistent non-association (no association demonstrated in ≥ 2 studies); (3) association/non-association (demonstrated in 1 study); and (4) inconsistent associations (≥ 2 studies demonstrating associations in different directions).
Results
Literature search
We screened 1981 titles and abstracts for eligibility (Fig. 1). Of these, 118 full-texts were screened. We critically appraised eight eligible cohort studies [24,25,26,27,28,29,30,31] and all were deemed of acceptable quality (i.e., low risk of bias). No additional studies were found with hand-searching of reference lists of eligible studies.
Risk of bias
The accepted studies had some methodological limitations (Table 1). For example, in most studies, it was unclear (and marked as “can’t say” according to the SIGN criteria) if the method of exposure assessment was reliable (6/8) [24,25,26,27, 30, 31] and there was no evidence that the method of outcome assessment was valid and/or reliable (6/8) [24, 25, 27, 29,30,31]. Additionally, it was unclear (“can’t say”) if the assessment of outcome was made blind to exposure status or if there was recognition that knowledge of exposure status could have influenced the assessment of outcome in all studies where these criteria were applicable (3/3) [27, 30, 31]. Potential confounders were not clearly identified in two studies [29, 31] that aimed to assess causal factors; therefore, we synthesised risk factors as risk markers rather than determinants.
Study characteristics
A summary of study characteristics is presented in Table 2. The majority of eligible studies were conducted in the U.S. (5/8) [24, 25, 27, 29, 30], and one each were conducted in Sweden [28], Finland [26], and Israel [31]. Two studies assessed Marines [24, 28], two assessed Army personnel [27, 29], and the remaining studies assessed the military as a whole [25, 26, 30, 31].
All studies were cohort studies (5/8 single-group cohorts [24, 26, 28, 29, 31]), which assessed risk factors for incident LBP in the active military population. Three studies were prospective cohort studies [26, 28, 29], while five were historical cohort studies conducted using pre-existing administrative and/or clinical data [24, 25, 27, 30, 31]. All studies examined non-causal associations between candidate risk factors and incident LBP, as there were either no clear a priori variables defined as potentially important for predicting incident LBP by the studies or the necessary confounding variables were not identified a priori and 1controlled for; therefore, only risk markers were identified. No studies identified included prediction or causal modelling; therefore, risk predictors and risk determinants could not be identified. Half of the studies examined risk factors in more than one category (e.g., physical, sociodemographic, and/or occupational) [24,25,26, 29]. Four studies examined physical risk factors (e.g., physical fitness, body characteristics) [26,27,28,29], three studies examined sociodemographic risk factors (e.g., age, sex, education) [24,25,26], and six studies examined occupational risk factors (e.g., occupational tasks, military service) [24,25,26, 29,30,31]. No studies assessed psychological risk factors for LBP.
Overview of risk factors
In the eight studies included in our review, 37 risk factors (all risk markers) were examined: 13 physical factors, 16 sociodemographic factors, and 8 occupational factors. Among prospective cohort studies, all used self-reported questionnaires to identify the risk factors [26, 28, 29]. The historical cohort studies used administrative data to identify the risk factors [24, 25, 27, 30, 31]. There were no consistent confounding variables that were adjusted for by all studies; however, age (5/8) [24,25,26,27, 30] and sex (4/8) [24, 25, 27, 28] were most commonly adjusted for. The outcomes and key findings for each risk factor studied is presented in Table 3.
Consistent associations between physical risk factors and LBP
A history of LBP demonstrated a consistent association with LBP during active duty military service [28, 29]. Monnier et al. concluded that back pain within six months prior was a risk factor for both LBP (HR 2.47, 95% CI 1.41–4.31) and LBP limiting work ability (HR 3.58, 95% CI 1.44–8.90) [28] and Roy and Lopez concluded that a history of LBP prior to military service was associated with LBP in the Brigade Support Battalion (OR 5.03, 95% CI 1.61–15.72), the Brigade Special Troops Battalion (OR 8.91, 95% CI 1.71–46.46), and the Infantry Battalion (OR 2.20, 95% CI 1.2–4.04) compared to those without a history of LBP [29]. Similarly, previous injury (e.g., lower extremity injury or sports injury) consistently demonstrated an association with LBP [26, 27]. Taanila et al. [26] concluded that having a sports injury during the prior month (HR 1.7, 95% CI 1.0–2.8) was a risk factor for LBP, while Seay et al. [27] concluded that lower extremity injury was a risk factor for LBP (HR 1.70, 95% CI 1.66–1.74) irrespective of sex (males—HR 1.76, 95% CI 1.72–1.80; females—HR 1.43, 95% CI 1.36–1.50). The amount of time spent on physical training also had an association with LBP, with one study demonstrating that those participating in fewer physical training sessions per week had a greater risk of LBP limiting work ability than those participating in more physical training sessions per week (HR 2.96, 95% CI 1.19–7.39) [28], while another study demonstrated that participation in more strength training was associated with a lower risk for LBP (OR 0.88, 95% CI 0.78–0.99) [29].
Non-associations between physical risk factors and LBP
Based on a single study by Taanila et al., the following factors were not found to be associated with LBP: body mass index, waist circumference, self-assessed health, chronic disease, regular medications, orthopedic surgery, chronic impairment due to prior MSK injury, and self-assessed physical fitness [26].
Inconsistent associations between physical risk factors and LBP
There was conflicting evidence on whether poor performance on various physical fitness tests were associated with LBP. For example, Monnier et al. demonstrated that performing less pull ups was associated with incident LBP (HR 1.87, 95% CI 1.17–3.01) [28], but Taanila et al. found no association [26]. Similarly, Taanila et al. found an association between poor performance on certain combinations of physical fitness tests (e.g., poor results in the combination of push-up and Cooper test (12-min running test) (HR 2.1, 95% CI 1.1–4.2); poor results in the combination of back lift and Cooper test (HR 2.4, 95% CI 1.1–5.4); poor results in the combination of sit-up and push-up test (HR 2.2, 95% CI 1.1–4.5); and poor results in the combination of push-up and back lift test (HR 2.8, 95% CI 1.4–5.9)) but not individual physical fitness tests (e.g., push-up or Cooper test alone) [26]. There was also conflicting evidence on the association between height and LBP, with one study reporting an association between shorter height and LBP (HR 1.98, 95% CI 1.19–3.29) and LBP limiting work ability (HR 4.48, 95% CI 2.01–9.97) [28], while another study found no association [26].
Consistent associations between sociodemographic risk factors and LBP
Being female was the only sociodemographic risk factor that consistently demonstrated an association with LBP [24, 25]. MacGregor et al. concluded that females (OR 1.94, 95% CI 1.61–2.34) were more likely to report LBP compared to males [24], and Knox et al. concluded that being female (IRR 1.45, 95% CI 1.39–1.52) was associated with LBP [25].
Associations between sociodemographic risk factors and LBP
An association with LBP was reported for ‘single’ marital status being less likely to experience LBP (IRR 0.87, 95% CI 0.84–0.91) compared to individuals reporting ‘married’ as their marital status [25]. Additionally, lower education level (HR 1.6, 95% CI 1.1–2.3) was associated with LBP [26]. As these were only reported in single studies, these sociodemographic risk factors may be further studied.
Non-associations between sociodemographic risk factors and LBP
Based on a single study by Taanila et al., the following factors were not found to be associated with LBP: father’s occupation, urbanisation level of place of residence, smoking habits, use of alcohol, frequency of drunkenness before military service, agreeing that soldiers need good physical fitness, amount of time spent on sweating exercises, participation in individual aerobic sports, belonging to a sports club, participation in competitive sports, and last degree in school sports [26]. Additionally, Knox et al. reported that race was not associated with LBP [25].
Inconsistent associations between sociodemographic risk factors and LBP
There was conflicting evidence on the association between age and LBP, with Knox et al. reporting that younger age (less than 20 years) was associated with LBP (IRR 1.24, 95% CI 1.15–1.36) [25], while Ernat et al. reported that among infantrymen, the incidence of LBP increased with age (from IRR 0.61, 95% CI 0.59–0.63 in those under the age of 20 to IRR 0.91, 95% CI 0.86–0.97 in those over the age of 40) [30]. Two studies reported no association between age and LBP [24, 26].
Consistent associations between occupational risk factors and LBP
Among occupational risk factors, lower rank consistently demonstrated an association with LBP, with one study demonstrating that junior rank was associated with a higher risk for incident LBP compared to those with senior rank (IRR 1.60, 95% CI 1.52–1.70) [25], while another study demonstrated that mid-level ranks (compared to junior ranks) were associated with a lower risk for LBP (OR 0.73, 95% CI 0.64–0.83) [24].
Associations between occupational risk factors and LBP
Several risk factors demonstrating an association with LBP were studied in single studies. These included having a blast injury (OR 2.29, 95% CI 1.64–3.19) [24], job duties (e.g., lifting > 30 pounds (OR 1.30, 95% CI 1.06–1.60) or wearing body armour (OR 1.14–1.30, 95% CI 1.07–1.53)) [29], and service type (e.g., Army (IRR 2.74, 95% CI 2.60–2.89) and Air Force (IRR 1.98, 95% CI 1.84–2.14) compared to Marines) [25]. In a study of U.S. military service members, no association with LBP was found for location of deployment and time deployed [24].
Inconsistent associations between occupational risk factors and LBP
There were no military occupations that were consistently found to be associated with developing LBP, as positive associations were found for many different occupations [24, 26, 30]. MacGregor et al. concluded that being in the service/supply occupation (compared to administrative/other occupations) (OR 1.33, 95% CI 1.12–1.59) and being in the electrical/mechanical/craftsworker occupation (compared to administrative/other occupations) (OR 1.31, 95% CI 1.12–1.53) were risk factors for LBP [24]. Taanila et al. concluded that being part of the engineer company (HR 2.0, 95% CI 1.2–3.3) was associated with LBP compared to those working in the anti-tank company [26]. Ernat et al. concluded that infantrymen had a lower risk of LBP compared to non-infantry soldiers (IRR 0.69, 95% CI 0.68–0.70) [30]. There was also no consistent evidence for the association of driving and incident LBP [25, 31]. Knox et al. concluded that being a military vehicle operator was associated with an increased risk of LBP compared to those of other occupations (IRR 1.15, 95% CI 1.13–1.17) [25], while Zack et al. concluded that professional truck drivers were less likely to experience LBP compared to those working in administrative units (RR 0.49, 95% CI 0.40–0.60) [31].
Discussion
The objective of our systematic review was to synthesise the literature on risk factors of incident LBP in active duty military personnel. We identified eight relevant cohort studies. None of the studies were designed to assess a causal relationship between candidate factors and incident LBP; therefore, all studies identified risk markers. In active duty military personnel, we found consistent associations between LBP and physical factors (e.g., prior LBP, prior musculoskeletal injury, less time spent on physical training), sociodemographic factors (e.g., female sex), and occupational factors (e.g., lower rank). The magnitude of the associations between prior LBP and incident LBP ranged from 2.20 (95% CI 1.2–4.04) to 8.91 (95% CI 1.71–46.46) [28, 29]. We also found associations between LBP and other sociodemographic and occupational factors (e.g., married marital status, lower education level, blast injuries, job duties including lifting > 30 pounds or wearing body armour, Army or Air Force service type); non-associations between LBP and physical (e.g., body mass index, waist circumference, self-assessed health) and sociodemographic factors (e.g., race, smoking habits, urbanisation of place of residence); and inconsistent associations between LBP and other physical (e.g., poor performance on physical fitness tests), sociodemographic (e.g., younger age), and occupational (e.g., occupation types such as service/supply, electrical/mechanical/craftsworker, engineer, infantry, or military vehicle operators) factors. Psychological risk factors were not assessed in any of the included studies.
To our knowledge, no other reviews investigated risk factors for incident LBP in the military population; thus, it is unknown if our results are comparable. However, the risk factors identified in our review are comparable to risk factors identified in the literature for incident LBP in other occupational settings. Having previous episodes of LBP has been consistently shown to significantly increase the risk of new episodes of LBP in both community and occupational settings [2, 10, 11]. A systematic review and meta-analysis on incidence and risk factors for first-time LBP by Taylor et al. [10] indicated that physical risk factors for incident LBP (pain free at baseline) included increased weight or body mass index, poor health behaviours, a low assessment of physical fitness (e.g. measured on endurance or strength tests), and having occupational demands that include lifting or carrying more than 25 pounds. In an umbrella review of systematic reviews on risk factors for LBP [11], lifting over 25 kg, higher frequency of lifting, and prolonged standing or walking were also identified as risk factors for LBP.
In contrast to findings from other LBP reviews, no studies included in our review examined psychological or psychosocial risk factors for incident LBP among active duty military personnel. Psychosocial factors have also been found to increase the risk of developing LBP [2, 10, 11]. These include mental distress (e.g., feeling stressed, nervous, tense), depression, psychosomatic factors, sleep problems, job dissatisfaction and dissatisfaction with life, participation in monotonous work, and interpersonal stress at work [10, 11]. Many of these psychosocial risk factors were identified within occupational settings including workers in clerical support and office, agricultural and forestry, crafts and trades, machine operators, farming, manufacturing, and healthcare; however, these were not identified in our review. A potential reason for the lack of studies examining psychosocial risk factors for incident LBP among this population relates to the stigma-related barriers to help-seeking for mental health problems among military members (e.g., shame/embarrassment, negative social judgement, confidentiality concerns, employment-related discrimination) [32].
Strengths and limitations
There is the possibility of publication bias in our review because we only included articles that were published in peer-reviewed journals and in English. Therefore, other potentially eligible articles may have been missed and non-English studies may be captured in a subsequent review. A major strength of our review was the comprehensive search strategy. We included six databases using a robust and peer-reviewed search strategy.
Implications
Our study identifying only risk markers of incident LBP has research implications. For example, the markers that had a consistent association with LBP can be studied further to assess if they are predictors or determinants of LBP. Subsequently, strategies or interventions targeting identified modifiable risk predictors or determinants may then be developed and tested to see if they prevent LBP in the active duty military. The association between psychological or psychosocial factors and incident LBP in the active duty military should also be further studied, as they have been identified to be significant risk factors for LBP in both the general population and in various occupational settings [10, 11]. Given that we only identified risk markers and studies of “acceptable” methodological quality, future research of high methodological quality may change our conclusions.
Conclusion
Physical and occupational risk factors for incident LBP in active duty military were most commonly studied, with less focus on sociodemographic factors and none on psychological or psychosocial factors. A prior history of LBP, less physical training, previous injury, female sex, and lower rank consistently demonstrated an association with LBP. There was conflicting evidence of association for performance on physical fitness tests, body height, age, and various occupations, including driving. Our conclusions may change in light of future studies of higher methodological quality; future studies should explore the role of psychological/psychosocial risk factors in the development of LBP among active duty military personnel, and whether identified risk markers predict or cause incident LBP. Our results are relevant for researchers, active duty military personnel, and other decision makers who may be involved in developing strategies to reduce the risk of LBP in the active duty military population.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MSK:
-
Musculoskeletal
- LBP:
-
Low back pain
- U.S.:
-
United States
- OR:
-
Odds ratio
- RR:
-
Relative risk
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- IRR:
-
Incidence rate ratio
References
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–602.
Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–67.
Cohen SP, Gallagher RM, Davis SA, Griffith SR, Carragee EJ. Spine-area pain in military personnel: a review of epidemiology, etiology, diagnosis, and treatment. Spine J. 2012;12(9):833–42.
Clark LL, Hu Z. Diagnoses of low back pain, active component, U.S. Armed Forces, 2010–2014. MSMR. 2015;22(12):8–11.
Litow CD, Krahl PL. Public health potential of a disability tracking system: analysis of U.S. Navy and Marine Corps physical evaluation boards 2005–2006. Mil Med. 2007;172(12):1270–4.
Knox J, Orchowski J, Scher DL, Owens BD, Burks R, Belmont PJ. The incidence of low back pain in active duty United States military service members. Spine (Phila Pa 1976). 2011;36(18):1492–500.
Smith L, Westrick R, Sauers S, Cooper A, Scofield D, Claro P, et al. Underreporting of musculoskeletal injuries in the US Army: findings from an Infantry Brigade Combat Team Survey Study. Sports Health. 2016;8(6):507–13.
Dijksma I, Bekkers M, Spek B, Lucas C, Stuiver M. Epidemiology and financial burden of musculoskeletal injuries as the leading health problem in the military. Mil Med. 2020;185(3–4):e480–6.
Cohen SP, Brown C, Kurihara C, Plunkett A, Nguyen C, Strassels SA. Diagnoses and factors associated with medical evacuation and return to duty for service members participating in Operation Iraqi Freedom or Operation Enduring Freedom: a prospective cohort study. Lancet. 2010;375(9711):301–9.
Taylor JB, Goode AP, George SZ, Cook CE. Incidence and risk factors for first-time incident low back pain: a systematic review and meta-analysis. Spine J. 2014;14(10):2299–319.
Parreira P, Maher CG, Steffens D, Hancock MJ, Ferreira ML. Risk factors for low back pain and sciatica: an umbrella review. Spine J. 2018;18(9):1715–21.
Hanvold TN, Kines P, Nykanen M, Thomee S, Holte KA, Vuori J, et al. Occupational safety and health among young workers in the Nordic countries: a systematic literature review. Saf Health Work. 2019;10(1):3–20.
Kwon BK, Roffey DM, Bishop PB, Dagenais S, Wai EK. Systematic review: occupational physical activity and low back pain. Occup Med Lond. 2011;61(8):541–8.
Coenen P, Gouttebarge V, van der Burght AS, van Dieën JH, Frings-Dresen MH, van der Beek AJ, et al. The effect of lifting during work on low back pain: a health impact assessment based on a meta-analysis. Occup Environ Med. 2014;71(12):871–7.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
National Institute for Health Research (NIHR). International prospective register of systematic reviews (PROSPERO). Available from https://www.crd.york.ac.uk/prospero/.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
Kent P, Cancelliere C, Boyle E, Cassidy JD, Kongsted A. A conceptual framework for prognostic research. BMC Med Res Methodol. 2020;20(1):172.
Burton AK, Balague F, Cardon G, Eriksen HR, Henrotin Y, Lahad A, et al. Chapter 2: European guidelines for prevention in low back pain: November 2004. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deformity Soc Eur Sect Cervical Spine Res Soc. 2006;15(Suppl 2):S136–68.
Scottish Intercollegiate Guidelines Network. (2001–2019). Scottish intercollegiate guidelines network. Available from https://www.sign.ac.uk/checklists-and-notes.html.
Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ Clin Res Ed. 2001;323(7308):334–6.
Riley RD, Moons KGM, Snell KIE, Ensor J, Hooft L, Altman DG, et al. A guide to systematic review and meta-analysis of prognostic factor studies. BMJ Clin Res Ed. 2019;364:k4597.
Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ Clin Res Ed. 2020;368:l6890.
MacGregor AJ, Dougherty AL, Mayo JA, Rauh MJ, Galarneau MR. Occupational correlates of low back pain among U.S. Marines following combat deployment. Mil Med. 2012;177(7):845–9.
Knox JB, Orchowski JR, Scher DL, Owens BD, Burks R, Belmont PJ Jr. Occupational driving as a risk factor for low back pain in active-duty military service members. Spine J. 2014;14(4):592–7.
Taanila HP, Suni JH, Pihlajamäki HK, Mattila VM, Ohrankämmen O, Vuorinen P, et al. Predictors of low back pain in physically active conscripts with special emphasis on muscular fitness. Spine J. 2012;12(9):737–48.
Seay JF, Shing T, Wilburn K, Westrick R, Kardouni JR. Lower-extremity injury increases risk of first-time low back pain in the US army. Med Sci Sports Exerc. 2018;50(5):987–94.
Monnier A, Larsson H, Nero H, Djupsjöbacka M, Äng BO. A longitudinal observational study of back pain incidence, risk factors and occupational physical activity in Swedish marine trainees. BMJ Open. 2019;9(5):e025150.
Roy TC, Lopez HP. A comparison of deployed occupational tasks performed by different types of military battalions and resulting low back pain. Mil Med. 2013;178(8):e937–43.
Ernat J, Knox J, Orchowski J, Owens B. Incidence and risk factors for acute low back pain in active duty infantry. Mil Med. 2012;177(11):1348–51.
Zack O, Levin R, Krakov A, Finestone AS, Moshe S. The relationship between low back pain and professional driving in young military recruits. BMC Musculoskelet Disord. 2018;19(1):110.
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45(1):11–27.
Acknowledgements
Not applicable.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors (DT, MR, KM, CC) assisted in designing and planning the study, developing the research questions, and systematic review methodology. DT and CC drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA 2009 Checklist.
Additional file 2.
Sample search strategy in MEDLINE (EBSCO).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
To, D., Rezai, M., Murnaghan, K. et al. Risk factors for low back pain in active military personnel: a systematic review. Chiropr Man Therap 29, 52 (2021). https://doi.org/10.1186/s12998-021-00409-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12998-021-00409-x