Abstract
Background
An understanding of maternal knowledge of the danger signs of obstetric and newborn complications is fundamental to attaining universal health coverage. In Northern Ghana, where maternal and newborn morbidity and mortality is high, little is known about the current knowledge level and associated determinants of these danger signs. This study assessed the effect of social behavior change communication (SBCC) package on knowledge of obstetric and newborn danger signs among mothers with children under 24 months of age.
Methods
This study used a non-randomized controlled community-based intervention design with pre and post-intervention household surveys in the intervention and comparison communities of the East Mamprusi District in Ghana. The study population were selected using a two-stage cluster sampling procedure.
Result
Only 521 (51.1%), 300 (29.4%) and 353 (34.6%) of the study participants knew at least three key danger signs during pregnancy, delivery and postpartum period respectively.
The intervention had a positive effect on maternal knowledge of danger signs. Compared to their counterparts in the comparison communities, women in the intervention communities were about 2.6 times (AOR = 2. 58 [CI: 1.87, 3.57]), 3.4 times (AOR = 3.39 [CI: 2.31, 4.96]) and 2.2 times (AOR = 2.19 [CI: 1.68, 2.84]) more likely to have higher knowledge of danger signs of childbirth, postpartum and neonate, respectively.
Having sought postnatal services at least once was significantly associated with the mentioning of at least three danger signs of postpartum (AOR = 3.90 [CI: 2.01, 7.58]) and childbirth (AOR = 1.75 [CI: 1.06, 2.85]).
Conclusion
There was a significant contribution of social and behavioral change communication as an intervention to maternal knowledge in obstetric danger signs after adjusting for confounding factors such as antenatal and post-natal care attendance. Therefore, provision of information, education and communication targeting women on danger signs of pregnancy and childbirth and associated factors would be an important step towards attaining universal health coverage.
Similar content being viewed by others
Background
On daily basis, an approximate number of 830 women die from preventable causes related to pregnancy and childbirth and almost all of these deaths occur in developing countries [1].
This notwithstanding, there is evidence that shows that low utilization of services, such as supervised deliveries and post-natal care continue to persist even where financial and geographic access is adequate [2], thereby making progress towards attainment of significant improvement in maternal and newborn health a big challenge to most developing countries including Ghana. Developing countries account for approximately 99% of the global maternal deaths in 2015, with sub-Saharan Africa alone accounting for roughly 66% [3].
Apart from poor quality of health services, socio-cultural factors in the form of practices, rituals, attitudes and beliefs (PRABs) have been identified as key contributors to the poor health seeking behaviors and has engaged the attention of Ghana’s Ministry of Health (MoH) over the past years [4–6]. In particular, a high maternal and neonatal death rates in East Mamprusi District of Northern Ghana were reported to be associated with household PRABs as well as non-recognition of danger signs and lack of timely decisions to access services, which all increase risks of obstetric complications [7]. Evidence suggests, however, that social norms and practices can be changed through the communication of culturally contextualized messages designed to support families in modifying high risk practices [8].
Adequate maternal knowledge of the danger signs associated with pregnancy, labour and the neonate is fundamental to utilization of maternal and newborn care (MNC) services [9–13]. Poor knowledge of newborn danger signs delays care seeking and ultimately greater risk of death. Evidence suggests that raising awareness for pregnant women to recognize these obstetric danger signs would improve early detection of problems and reduces the delay in deciding to seek obstetric care during labor, delivery and early postpartum period [14–17].
To address unhealthful social norms, attitudes and practices, lack of knowledge and poor demand for preventive health services among key population groups in the East Mamprusi District, a comprehensive community-based social and behavior change communication (SBCC) intervention trial was implemented by the Catholic Relief Services (CRS) and its collaborators to improve uptake of maternal and newborn health care services. This paper reports on the effect of the intervention on knowledge in obstetric danger signs among mothers who had given birth in the past 24 months prior to the study.
Methods
Survey design, population and sampling
The paper is based on data that were obtained as part of an intervention to evaluate the effectiveness of social and behaviour change communication (SBCC) through empowered community leaders to improve uptake of essential maternal and newborn care (MNC) services in the East Mamprusi district of Northern Ghana.
A “pretest-posttest non-equivalent groups design” was used. Two cross-sectional household surveys at baseline and end point were carried out in both the intervention and comparison areas district to measure change in key indicators. The baseline survey was carried out in February 2012 and the end line survey was conducted in July 2015.
The main outcome of this study was to increase the proportion of institutional deliveries. This outcome indicator was used to calculate a sample size of 1020 (510 per study arm). The sample was set to detect a 15% difference in the comparison (43%) and intervention areas (58%). Given the sampling method, a design effect of 2.0 was selected. Power (1-β) and statistical significance (α) were set at 90% and 0.05 respectively. A non-response of 10% was also considered in the sample size calculation.
Study Population and Sampling
The primary respondents comprised women of reproductive age who delivered within the last 2 years. Two sub districts which were geographically far apart but of similar socio-economic, demographic and health care characteristics were selected as intervention and comparison areas. A two-stage cluster sampling method was applied in each sub district to select the communities using probability proportional to size (PPS). Thirty clusters (i.e. communities) were selected randomly in the first stage from each study arm. In the second stage, eligible index households were selected in each cluster using systematic random sampling. Households with at least one woman who had delivered in the past 24 months were eligible for selection.
In each cluster, a complete list of all households was compiled serially and systematic random sampling used in selecting study participants. In the first step, the total number of households in a cluster was divided by the expected sample size of 17 to give the sampling interval. The first household was randomly selected by picking any number from 1 to the calculated sampling interval. Subsequent selections were made by adding the sampling interval to the selected number in order to locate the next household to visit. If the selected household did not have a target respondent, then the next household was selected using the systematic sampling procedure. This was done until the sample size was obtained.
Description of interventions
A community-based non-randomized cluster intervention was implemented involving two arms; one intervention study area and one comparison study area. The Comparison Group received only standard maternal health services. The Intervention Group received an innovative intervention in addition to the standard maternal health services.
The innovative intervention in this study was based on evidence which suggests, that social norms and practices can be changed through the social and behaviour change communication (SBCC) which focuses on the community as the unit of change. On the basis of this, key community leaders (KCLs) including chiefs, queen mothers, religious leaders and traditional healers were mobilized to constitute what we termed ‘Council of Champions’ (CoCs) who assisted in delivering messages designed to support families in modifying high risk practices and delivered through interpersonal interactions involving reasoning and negotiation between frontline healthcare workers and target populations at the household and community level. The CoCs comprised 5-7 most influential community members who were trained and regularly supervised by the project.
These KCLs are also the custodians of the norms and values of their people and exert significant influence on various household decision makers whose actions influence the health of women and children within their communities [18, 19].
The intervention whose details have been published [20] was implemented from 2012 through 2015. The main project intervention package was a social and behavior change communication (SBCC) strategy which sought to bring about significant and sustainable improvements in maternal and newborn outcomes.
Delivery of health and nutrition messages through behaviour change communication (BCC), training, outreach and counselling were the key activities undertaken by the project. In the intervention communities, community leaders and volunteers were trained to identify and offer preventive and promotive care and counseling to pregnant and postpartum women. Health facility strengthening was done in all facilities to improve quality of care. Community health workers (CHWs) were trained and supported to promote early and regular ANC attendance.
Variables and measurement
This study measured maternal knowledge in obstetric danger signs. Mothers were asked about risks associated with frequent pregnancies, signs and symptoms during pregnancy, delivery, newborn and postpartum danger signs which demanded seeking immediate care from the health facility or health workers.
A categorical variable was created to indicate the mother’s knowledge of such danger signs. A score of 1 was assigned if a mother could mention any of a listed number of danger signs. Knowledge of women about danger signs were measured by the total number of correct spontaneous answers to 8 items on knowledge of pregnancy danger signs, 7 items on knowledge of childbirth danger signs, 9 items on knowledge of postpartum danger signs and 10 items on newborn danger signs. Multiple responses were possible and spontaneous knowledge in this study refers to the respondent’s mentioning a sign without being given clues. The mothers were categorized into two based on the total scores obtained: Mothers who could mention 0–2 and those who could mention three or more danger signs. The category ‘knows up to 2 danger signs’ was used as the reference category.
Assessment of Adequacy of Antenatal Care Service Utilization
The overall adequacy of prenatal care was measured using the Adequacy of Prenatal Care Utilization Index (APNCU) [21], modified according to the recommendation by the World Health Organization (WHO) for developing countries. The WHO recommends that for normal pregnancies, antenatal care (ANC) should consist of at least four visits during the course of the pregnancy, the first of which should occur within the first trimester. This measure involves both timing and number of prenatal care visits. Consequently, ANC was considered adequate if the women started ANC within the first trimester and made at least four visits. A woman who initiated ANC later than the first trimester but made at least four visits was thus classified as having inadequate ANC.
Assessment of essential newborn care practices
In determining good essential newborn practices, composite indices were created: (i) Safe cord care (defined as use of a clean cutting instrument to cut the umbilical cord plus clean thread to tie the cord plus no substance applied to the cord); (ii) Optimal thermal care (defined as baby wrapped within 10 min of birth plus baby being dried/wiped immediately after birth); and (iii) Good neonatal feeding practices (defined as initiating breastfeeding within the first 1 h after birth, plus no prelacteal given and colostrum fed to the child). These composite variables were then dichotomized to Yes (all practices present) or No (one or more practices missing).
Assessment of negative maternal and newborn care health (MNCH) rituals and beliefs
Potential negative maternal and newborn care health (MNCH) rituals and beliefs were assessed using the Likert-type of questions which elicited responses from respondents on their position regarding different rituals and birthing practices. Respondents were specifically asked how much they agree or disagree with the following statements:
-
i.
A woman who is pregnant for the first time should only seek ANC services after she has announced her pregnancy to the community (Prisibu).
-
ii.
Charcoal, oil, cow dung, a concoction or cosmetic pomades should be applied to help heal the cord of newborns.
-
iii.
Before a woman in labor can go to the facility to deliver, the gods or ancestors should be consulted.
-
iv.
A woman who delivers her baby at home is more of a “real woman” than a woman who delivers in a health facility.
-
v.
After the birth of a baby, the mother should not go to the health facility until the naming ceremony has been performed.
Data Collection
The data were collected using predesigned and pretested semi-structured questionnaire. Targeted eligible women were interviewed in the local language in their homes. Data collected included socio-economic conditions of household, nutritional status, maternal and newborn care practices, and health services utilization.
In order to ensure reliability and validity of data collected, all field assistants with a minimum qualification of Senior High School were given training for 3 days. The content of the training included objectives and methodology, standard measurement procedures, data recording, recruitment, administration of questionnaires and supervision.
Data Analysis
The analysis of data took into account the complex design of multi-stage cluster surveys. All quantitative data were coded for statistical analysis using SPSS Complex Samples module for windows 18.0 (SPSS Inc, Chicago). This was done in order to make statistically valid population inferences and computed standard errors from sample data. Design weights were added to each region’s sample data (that is, total population divided by number of respondents) to perform weighted analysis.
The unit of analysis employed in this study is reproductive women with a child less than 24 months who were asked information on danger signs. A woman was considered knowledgeable when she could mention at least three recognizable danger signs for each of the critical periods of pregnancy, delivery, neonatal and postpartum.
The impact of the intervention was assessed using difference-in-difference (DID) analysis and measures of association (odds ratio). DID analyses allow for the determination of whether the intervention households did better than comparison households while taking into account any initial differences between the groups at baseline. By doing so it controls for any changes that took place in the project area that are not related to project interventions or that are only indirectly related to them through spillover effects.
Bivariate and multiple logistic regression analyses were performed to explore the knowledge levels and factors determining maternal knowledge on obstetric and newborn danger signs. The association between dependent variables and independent variables was determined using multiple logistic regressions modeling, which included all potential socioeconomic, and demographic confounders that were significant at p values < 0.05 in the bivariate analysis. The associations between knowledge on key danger signs of obstetric complication during the four periods (pregnancy, childbirth, neonatal and postpartum) and each independent variable were presented as adjusted odds ratios (AOR) with 95% confidence intervals (CI). A CI was considered statistically significant when the interval between the upper and lower values did not include one.
Ethics approval and consent to participate
Approval for the conduct of this study was given by the Institutional Review Board (IRB) of the School of Medicine and Health Sciences, University for Development Studies (Reference no. SMHSER0001). Study participants were free to refuse or withdraw from the study at any time without any penalty. The study’s purpose and objectives were explained to each participant prior to interview. Informed consent was sought from all study participants before the commencement of any interviews or study activity. Additionally, participants who were literates signed the consent form but those who could not read made a thump-print after obtaining verbal explanation from the interviewer.
No biological sample was obtained as a part of the data collection. Data were kept strictly confidential and no personal identifiers were put on the questionnaires.
Results
Comparison of socio-demographic characteristics at baseline
At base-line, a total of 1003 respondents were interviewed; 510 from the Intervention Area (that is, Sakogu Sub-district) and 493 from the Comparison Area (Langbinsi Sub-district). There were significant differences between the two areas with respect to the age distribution of the children and ethnicity of the mothers. A greater proportion of women in the intervention than in the comparison communities were at least 6 km away from a health facility.
Both intervention and nonintervention groups were comparable in terms of age of mothers, educational level and parity. There were also significant differences in maternal knowledge in obstetric danger signs at baseline (Table 1).
Maternal Knowledge on danger signs and symptoms during pregnancy and delivery
Vaginal bleeding, severe abdominal pain and decreased foetal movement were frequently mentioned as the danger signs of pregnancy. Only 51.1% of respondents could mention at least three of the danger signs and symptoms during pregnancy that would prompt the mother to seek immediate care.
Similarly, the most commonly mentioned danger sign of childbirth was excessive vaginal bleeding by 485 (47.5%). Fast/difficult breathing and prolonged labour as danger signs were mentioned by a relatively smaller percentage of the respondents. The proportion of women who were able to mention three or more danger signs during delivery in the whole sample was 29.4% (Table 2).
Knowledge on danger signs during postpartum and neonatal periods
When the participants were asked to mention danger signs during postpartum, the most common spontaneously mentioned danger signs were severe abdominal pain and vaginal bleeding. The knowledge levels on the rest of the danger signs among the respondents were very low (Table 3).
Fever and poor suckling or feeding were the new born danger signs that were frequently mentioned and will prompt mothers to take their newborns to a health facility. The knowledge levels on other danger signs among the respondents were very low. Out of the ten newborn danger signs, only 37.5% of respondents could mention at least three danger signs.
The effect of Social Behaviour Change Communication (SBCC) on maternal knowledge in obstetric danger signs
The difference-in-difference (DID) analysis comparing the changes over time for eligible intervention households and the comparison households indicates a significant improvement in respect of maternal knowledge in least 3 danger signs (Table 4).
There was a significant relative improvement in the proportion of women who could identify at least three danger signs during pregnancy, delivery and postpartum that needed the urgent attention of a health professional. However, the intervention had a negative impact on maternal knowledge in newborn danger signs.
Using binary logistic regression, there was significant improvement in maternal knowledge in least 3 danger signs (P < 0.001) in the Intervention Group as compared to Comparison Group. Though there were significant differences in maternal knowledge in obstetric danger signs at baseline, these were not a significant determinants of maternal knowledge at follow-up (Table 5).
Factors associated with knowledge of women on danger signs of pregnancy and childbirth
In a multivariate logistic regression analysis, the intervention, maternal age, uptake of postnatal services, and negative maternal and newborn care health (MNCH) rituals and beliefs were independently associated with the mentioning of at least three obstetric danger signs (Table 6).
The intervention had a positive effect on maternal knowledge of danger signs. Compared to their counterparts in the comparison communities, women in the intervention communities were about 2.6 times (AOR = 2. 58 [CI: 1.87, 3.57]), 3.4 times (AOR = 3.39 [CI: 2.31, 4.96]) and 2.2 times (AOR = 2.19 [CI: 1.68, 2.84]) more likely to have higher knowledge of danger signs of childbirth, postpartum and neonate, respectively.
The other strong predictor of knowledge about the danger signs of postpartum and childbirth was patronage of postnatal services in the first week after delivery. Having sought postnatal services at least once was significantly associated with the mentioning of at least three danger signs of child birth (AOR = 1.75 [CI: 1.06, 2.85]), postpartum (AOR = 3.90 [CI: 2.01, 7.58]) and newborn danger signs (AOR = 1.54 [CI: 1.02, 2.32]). Women who sought postnatal services in the first week after delivery were 3.9 times more likely to be knowledgeable in the dangers during the postpartum period, compared to women who did not.
Maternal age at interview showed an independent association only with knowledge of women in the danger signs of pregnancy. Mothers aged at least 35 years were 1.5 times (AOR = 1. 52 [CI: 1.03, 2.23]) more likely to be knowledgeable about the danger signs of pregnancy as compared to those who were less than 25 years.
Women who received adequate ANC services were about 1.5 times (AOR = 1.50 [CI: 1.05, 2.16]) and 1.6 times (AOR = 1.58 [CI: 1.19, 2.10]) more likely to have higher knowledge of danger signs of postpartum and neonate as compared to their counterparts who did not get adequate ANC.
Women who reported no unhealthful social norms, beliefs, attitudes and practices were 1.8 times (AOR = 1. 81 [CI: 1.40, 2.35]; 1.7 times (AOR = 1. 72 [CI: 1.26, 2.32]; 1.4 times (AOR = 1. 39 [CI: 1.02, 1.89]; and 30.0% (AOR = 0. 70 [CI: 0.53, 0.92]) more likely to recognize danger signs during pregnancy, delivery, postpartum and newborn respectively.
Having at least one wrong maternal and newborn care health (MNCH) belief was negatively associated with the mother’s ability to recognize danger signs during pregnancy, delivery and postpartum. Some of the negative rituals and birthing practices were:
-
i.
A woman who is pregnant for the first time should only seek ANC services after she has announced her pregnancy to the community (Locally known as “Prisibu”).
-
ii.
Before a woman in labour can go to the facility to deliver, the gods or ancestors should be consulted.
-
iii.
A woman who delivers her baby at home is more of a “real woman” than a woman who delivers in a health facility.
-
iv.
After the birth of a baby, the mother should not go to the health facility until the naming ceremony has been performed.
Other independent variables including parity, marital status, occupation, place of delivery and religion were not associated with awareness of a danger sign during pregnancy, delivery and after delivery in the bivariate logistic regression analysis, and were therefore not included in the multivariate logistic regression analysis.
Association between improved maternal knowledge in obstetric danger signs and uptake of maternal and newborn health services
As shown in Table 7, improved knowledge of obstetric danger signs was associated with uptake of ANC services and adoption of essential newborn care practices but not patronage of health facilities for delivery. Association between maternal knowledge in danger signs and maternal and newborn practices/behaviours Table 8 shows the association between maternal knowledge in danger signs and maternal and newborn practices/behaviours..
Discussion
In Northern Ghana, where maternal and newborn morbidity and mortality is high, little is known about the current knowledge level on obstetric, newborn danger signs and associated determinants among women of reproductive age. This study has provided evidence that may be useful in planning and monitoring the impact of behavior change communication programme efforts by Maternal and Child Health programmes that seek to increase knowledge of danger signs among women and to prevent delays in seeking MNCH services/care.x
Maternal Knowledge on risks and danger signs associated with pregnancy, delivery and newborn and postpartum
An understanding of maternal knowledge of the danger signs of obstetric and newborn complications is fundamental to attaining universal health coverage. In this study a woman was considered knowledgeable if she could mention at least three recognized danger signs for each of the critical periods of pregnancy, delivery, postpartum and neonate.
Consistent with other studies, a significant proportion of mothers were not knowledgeable about the danger signs of pregnancy, childbirth, postpartum and the newborn in the district.
Several studies have also revealed that mothers from some developing countries including Sri Lanka, Kenya, Uganda and Nepal had unsatisfactory levels of knowledge in the recognition of newborn danger signs [22–26]. A community based cross-sectional study conducted in Tanzania showed that about half of the study subjects knew at least one obstetric danger sign [27], and in Kenya, only 27.9% of women attending ANC were not informed about danger signs in pregnancy [16]. This finding is also consistent with studies conducted in Ethiopia in which 30.9% of respondents mentioned at least two danger signs of pregnancy [28, 29]. This indicates a significant number of pregnant women who do not have the knowledge are likely to delay in deciding to seek care.
Excessive vaginal bleeding was the most common and spontaneously mentioned danger sign of pregnancy, childbirth and during the postpartum period, whilst severe abdominal pain and decreased foetal movement were also frequently added as danger signs of pregnancy. Severe abdominal pain was also mentioned as a danger sign during postpartum, with fever and poor suckling or feeding more frequently mentioned as new born danger signs.
Higher awareness of vaginal bleeding as a danger sign has been reported in Karachi, Pakistan [30]. Some studies have indicated that vaginal bleeding after delivery is most commonly recognized as a danger sign perhaps because it is the most visible sign and the most common cause of maternal death immediately after delivery [11, 31].
Recognizing danger signs by pregnant women could improve early detection of problems and reduce the delay in deciding to seek obstetric care [14–16]. Thus, the importance of creating awareness on danger signs among pregnant women and family members to take appropriate steps to ensure a safe birth and to seek timely skilled care in emergencies cannot be over-emphasized.
The strong predictors of knowledge of women about danger signs of labor and childbirth were adequate ANC, postnatal services and having at least one wrong maternal and newborn care health (MNCH) belief. Maternal age was an independent predictor only with knowledge of women about the danger signs of pregnancy. Increased knowledge levels among older women may be related to their own experiences with pregnancy. This implies that young women in their first pregnancy may need more consideration when providing counseling and health education.
The evidence from this study suggests that exposure to adequate ANC services was critical and more likely to increase mothers’ awareness and knowledge regarding danger signs. This finding is in consonance with earlier studies which have shown that health education during antenatal care improves mothers’ knowledge about obstetric danger signs [32, 33].
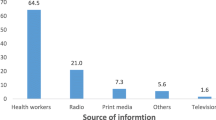
However, the study revealed that only a small proportion of women really received adequate ANC services. The health and local community authorities would have to put measures in place to promote uptake of ANC services early in pregnancy. In addition to the antenatal and postnatal care counseling, other channels of spreading key messages including community-based radio broadcasts should be considered. Furthermore, it is important for educational messages to target women’s groups, husbands, mothers in-law, and other family members, who play an important role in the decision making process [34, 35].
The postnatal period begins immediately after the birth of the baby and extends up to 6 weeks (42 days) after birth [36]. The immediate postpartum period is a dangerous time for both the mother and newborn [36–38] and between 50 and 71% of maternal deaths happen during postpartum period, particularly in the first few hours [39]. Recognizing danger signs and symptoms during this period is therefore critical for the health of mother and newborn. In this study, patronizing postnatal services at least once during the first week after delivery was the most important predictive factor for increased awareness of danger signs in the postpartum period. This finding is corroborated in at least one study [40]. This can be explained by the fact that women would have become aware of obstetric danger signs through education received at postnatal care centres as this issue is often among the topics for discussion. In spite of this, only 31.4% of mothers in the study sample utilized postnatal care service at least twice in the first week of delivery.
Level of education was not an important determinant of the mother’s ability to mention at least three danger signs during pregnancy and childbirth in this study population and this may be due to the very large numbers of non-educated women in our sample. However, a number of studies have shown strong association of mother’s educational attainment with their knowledge of danger signs [41–44].
Effect of behavior communication intervention on maternal knowledge of obstetric danger signs
The findings of the present study demonstrated that effective behavior communication intervention significantly improved in danger sign recognition.
The results of the study support findings of earlier studies in which BCC effectively improved obstetric danger sign recognition [45] though maternal knowledge of newborn care rather decreased in the intervention arm, compared to changes in the comparison arm in our sample.
Furthermore, such knowledge acquired positively associated with uptake of antenatal care services and adoption of essential newborn care practices. Improved knowledge of obstetric danger signs is expected to enhance utilization of maternal health services. This is because recognition of obstetric danger signs is a key factor in seeking preventive care or health promotion during pregnancy and childbirth.
Increased obstetric knowledge is reported to have enhanced greater use of facility delivery care [46]. Therefore, provision of information, education and communication targeting women on danger signs of pregnancy and childbirth would be an important step towards attaining universal health coverage.
Though increased obstetric knowledge was associated with adequate utilization of ANC services in the present study, it did not improve health facility delivery. This may be attributed to the absence of midwife in the intervention area. The midwife left the intervention area as a result of internal tribal conflict in the area during the project period.
This notwithstanding, some studies have shown that increased knowledge is not necessarily linked with behavior change [47].
Conclusion
There was a significant contribution of social and behavioral change communication as an intervention to maternal knowledge in obstetric danger signs after adjusting for confounding factors such as antenatal and post-natal care attendance.
This study further showed that the proportion of mothers who could mention at least three danger signs associated with frequent pregnancies, delivery, postpartum and newborn was low. The implication of this low knowledge levels is that delays in deciding to seek emergency care would still persist. Therefore, measures including provision of information, education and communication should be put in place by the health and local community authorities to promote uptake of ANC services early in pregnancy. In addition to the antenatal and postnatal care counseling, other channels of spreading key messages including community-based radio broadcasts should target women’s groups, husbands, mothers in-law, and other family members, who play an important role in the decision making process. It is suggested that further studies on the quality of counseling on danger signs and utilization of health services be carried out in order to design appropriate training modalities for health workers.
Limitations of the study
A number of factors may confound our findings. First of all, though there were significant differences in baseline characteristics between the study arms, these were accounted for using a difference-indifferences analysis. Secondly, responses were based on self-report and so measurement bias cannot also be ruled out. Finally, recall bias was more likely since women were asked for events which have already happened within the past 2 years prior to this study in spite of the fact that the youngest child and for that matter recent births were being referred to in the interviews.
Abbreviations
- ANC:
-
Antenatal care
- AOR:
-
adjusted odds ratios
- APNCU:
-
Adequacy of Prenatal Care Utilization
- MNC:
-
Maternal and newborn care
- MNCH:
-
Maternal and newborn care health
- PPS:
-
Probability Proportionate to Population Size
- PSU:
-
Primary sampling unit
- SBCC:
-
Social and behaviour change communication
References
Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016;387(10017):462–74.
Kyomuhendo GB. Low use of rural Maternity service in Uganda: Impact of women’s Status, traditional beliefs and limited resource. Reprod Health Matters. 2003;11(21):16–26.
WHO, UNICEF, UNFPA, World Bank Group, United Nations Population Division. Trends in maternal mortality: 1990 to 2015. Geneva: World Health Organization; 2015.
Ghana Statistical Service (GSS), Ghana Health Service (GHS), ICF Macro. Ghana Demographic and Health Survey (GDHS) 2008. Accra: GSS, GHS, and ICF Macro; 2009.
MOH. The Health Sector Medium-term development plan, 2010 (HSMTDP, 2010-2013. Accra: Ghana Ministry of Health; 2010.
MOH. National Health Policy: Creating Wealth through Health. Accra: Ministry of Health; 2007.
Wuni A. Determinants of use of MCH services among women of reproductive age in West and East Mamprusi. Northern Health Monitor. 2009;2(6):43–53.
Darmstadt GL, Tarigopula UK. Behavior Change Communication as an Intervention to Improve Family Health Outcomes. J Family Welfare. 2010;56:1–7.
Choi Y, El Arifeen S, Mannan I, Rahman SM, Bari S, et al. Can mothers recognize neonatal illness correctly? comparison of maternal report and assessment by community health workers in rural Bangladesh. Trop Med Int Health. 2010;15(6):743–53.
Hill Z, Kendall C, Arthur P, Kirkwood B, Adjei E. Recognizing childhood illnesses and their traditional explanations: exploring options for care-seeking interventions in the context of the IMCI strategy in rural Ghana. Trop Med Int Health. 2003;8(7):668–76.
Wilcox MA, Chang AMZ, Johnson IR. The effects of parity on birthweight using successive pregnancies. Acta Obstet Gynecol Scand. 1996;75:459–63.
Niswander K, Jackson EC. Physical characteristics of the gravida and their association with birth weight and perinatal death. Am J Obstet Gynecol. 1974;119:306–13.
Blair EM, Liu Y, de Klerk NH, Lawrence DM. fetal growth for the Caucasian singleton and assessment of appropriateness of fetal growth: an analysis of a total population perinatal database. BMC Pediatr. 2005;5:13.
Prentice AM, Cole TJ, Foord FA, Lamb WH, Whitehead RG. Increased birthweight after prenatal dietary supplementation of rural African women. Am J Clin Nutr. 1987;46:912–25.
Lechtig A, Habicht JP, Delgado H, Klein RE, Yarbrough C, Martorell R. Effect of food supplementation during pregnancy on birthweight. Pediatrics. 1975;56:508–20.
Ceesay SM, Prentice AM, Cole TJ, Foord F, Weaver LT, Poskitt EM, et al. Effects on birth weight and perinatal mortality of maternal dietary supplements in rural Gambia: 5 year randomised controlled trial. BMJ. 1997;315:786–90.
UNICEF. The state of the world's children. In Available: www.unicef.org/publications/files/UNICEF_SOWC_2016.pdf.
ICF International. Survey organization manual for demographic and health surveys vol. 2015. Calverton: ICF International; 2012.
Rustein SO, Johnson K. The DHS Wealth Index. In: DHS Comparative Reports No 6. Calverton: Micro International; 2004.
Tuli K, Wilcox S. Evaluation of Encouraging Positive Practices for Improving Child Survival, East Mamprusi, Ghana, West Africa. Washington, DC: Catholic Relief Services; 2015.
UN ACC/SCN. Second report on the world nutrition situation In Global and regional results, vol. I. Geneva: Administrative Committee on Coordination–Subcommittee on Nutrition; 1992. p. 1–112.
Sharan M. Determinants of safe motherhood and newborn care behaviors in Rural India [Ph.D. thesis]. Johns Hopkins University; 2004.
Senarath U, Fernando D, Vimpani G, Rodrigo I. Factors associated with maternal knowledge of newborn care among hospital-delivered mothers in Sri Lanka. Trans R Soc Trop Med Hyg. 2007;101(8):823–30.
Obimbo E, Musoke RN, Were F. Knowledge, attitudes and practices of mothers and knowledge of health workers regarding care of the newborn umbilical cord. East Afr Med J. 1999;76(8):425–9.
Tuladhar S. The Determinants of Good Newborn Care Practices in the Rural Areas of Nepal. [MSc. thesis], University of Canterbury; 2010.
Sandberg J, Odberg Pettersson K, Asp G, Kabakyenga J, Agardh A. Inadequate knowledge of neonatal danger signs among recently delivered women in Southwestern Rural Uganda: a community survey. PLoS One. 2014;9(5):e97253.
Merialdi M, Carroli G, Villar J, Abalos E, Gulmezoglu AM, Kulier R, et al. Nutritional interventions during pregnancy for the prevention or treatment of impaired fetal growth: an overview of randomized controlled trials. J Nutr. 2003;133(5 Suppl 2):1626S–31S.
de Onis M, Villar J, Gulmezoglu M. Nutritional interventions to prevent intrauterine growth retardation: evidence from randomized controlled trials. Eur J Clin Nutr. 1998;52 Suppl 1:S83–93.
Sumbele IUN, Bopda OSM, Kimbi HK, Ning TR, Nkuo-Akenji T. Nutritional status of children in a malaria meso endemic area: cross sectional study on prevalence, intensity, predictors, influence on malaria parasitaemia and anaemia severity. BMC Public Health. 2015;15:1099.
Pedersen CB, Sun Y, Vestergaard M, Olsen J, Basso O. Assessing fetal growth impairments based on family data as a tool for identifying high-risk babies. An example with neonatal mortality. BMC Pregnancy Childbirth. 2007;7:28.
Oaxaca R. Male-female wage differentials in Urban labor markets. Int Econ Rev. 1973;14:693–709.
Pembe AB, Urassa DP, Carlstedt A, Lindmark G, Nystrom L, Darj E. Rural Tanzanian women’s awareness of danger signs of obstetric complications. BMC Pregnancy Childbirth. 2009;9:12.
Kabakyenga JK, Östergren PO, Turyakira E, Pettersson K. Knowledge of obstetric danger signs and birth preparedness practices among women in rural Uganda. Reprod Health. 2011;8:33.
Shah PS. Parity and low birth weight and preterm birth: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89:862–75.
Melve KK, Skjaerven R, Oyen N. Families with a perinatal death: is there an association between the loss and the birthweight of surviving siblings? Paediatr Perinat Epidemiol. 2002;16:23–32.
Olofin I, McDonald CM, Ezzati M, et al. Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: a pooled analysis of ten prospective studies. PLoS One. 2013;8:e64636.
Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369:60–70.
Gillespie S. Improving adolescent and maternal nutrition: An overview of benefit and options. In: UNICEF Staff Working Papers, Nutrition Series, 97-002. New York: UNICEF; 1997.
Beard J. Functional consequences of nutritional anemia in adults. In: Ramakrishnan U, editor. Nutritional anemias. Boca Raton: CRC Pres; 2001. p. 111–28.
O’Donnell OA, Wagstaff A, Van Doorslaer E, Lindelow M, editors. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and their Implementation. Washington DC: World Bank Publications; 2008.
Hailu D, Berhe H. Knowledge about obstetric danger signs and associated factors among mothers in Tsegedie District, Tigray Region, Ethiopia 2013: community based cross-sectional study. PLoS One. 2014;9(2):e83459.
Dile M, Taddesse D, Gedefaw M, Asmama T. Knowledge of obstetric danger signs and its associated factors in Debaytilatgin District, Ethiopia: a community based cross sectional study. Gynecol Obstet (Sunnyvale). 2015;5:315.
Hoque M, Hoque ME. Knowledge of danger signs for major obstetric complications among pregnant KwaZulu-Natal women: implications for health education. Asia Pac J Public Health. 2011;23(6):946–56.
Amenu G, Mulaw Z, Seyoum T, Bayu H: Knowledge about Danger Signs of Obstetric Complications and Associated Factors among Postnatal Mothers of Mechekel District Health Centers, East Gojjam Zone, Northwest Ethiopia, 2014. Scientifica 2016, Article ID 3495416, 7 pages, doi:10.1155/2016/3495416.
Jennings L, Yebadokpo AS, Affo J, Agbogbe M. Antenatal counseling in maternal and newborn care: use of job aids to improve health worker performance and maternal understanding in Benin. BMC Pregnancy Childbirth. 2010;10:75.
Ensor T, Paula Quigley P, Green C, Badru AR, Kaluba D, Siziy S. Knowledgeable antenatal care as a pathway to skilled delivery: modelling the interactions between use of services and knowledge in Zambia. Health Policy Plan. 2014;29:580–8.
Khadduri R, Marsh DR, Rasmussen B, Bari A, Nazir R, Darmstadt GL. Household knowledge and practices of newborn and maternal health in Haripur district, Pakistan. J Perinatol. 2008;28:182–7.
Acknowledgements
The authors are grateful to the East Mamprusi District Health Directorate, supervisors, data collectors and study participants for their assistance and cooperation during the study.
We wish to gratefully acknowledge the Catholic Relief Services (CRS), Ghana for providing technical support.
Funding
No funding was received for this work.
Availability of data and materials
The dataset used in this analysis is available and can be made available upon request in writing to the corresponding author.
Authors’ contribution
MS, PA and RK conceived the study and its design. MS did the analysis and interpretation of data and was deeply involved in drafting the manuscript. AM and RK assisted in data retrieval and analysis. PA and MA were involved in manuscript writing, and critically commented on the draft manuscript for important intellectual content. All authors gave final approval of the version to be published.
Authors’ information
MS, PA and RK are Senior Lecturers at the School of Allied Health Sciences, University for Development Studies, Ghana. MA is Health Programme Manager at Catholic Relief Services, Ghana and AM is a field Officer at Catholic Relief Services, Ghana.
Competing interest
“The authors declare that they have no competing interests.”
Consent for publication
Not applicable
Ethics approval and consent to participate
Approval for the conduct of this study was given by the Institutional Review Board (IRB) of the School of Medicine and Health Sciences, University for Development Studies (Reference no. SMHSER0001). Verbal informed consent was also sought from all study participants before the commencement of any interviews or study activity. Study participants were free to refuse or withdraw from the study at any time without any penalty. The study’s purpose and objectives were explained to each participant prior to interview. No biological sample was obtained as a part of the data collection. Data were kept strictly confidential and no personal identifiers were put on the questionnaires.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Saaka, M., Aryee, P., kuganab-lem, R. et al. The effect of social behavior change communication package on maternal knowledge in obstetric danger signs among mothers in East Mamprusi District of Ghana. Global Health 13, 19 (2017). https://doi.org/10.1186/s12992-017-0243-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12992-017-0243-7