Abstract
Background
The presence of depression related to an increased risk of all-cause and cardiovascular disease (CVD) mortality has been reported. However, studies conducted on certain specific depressive symptoms are scarce. Our purpose was to assess the effect of both depressive symptoms scores and certain specific depressive symptoms on all-cause and CVD mortality.
Methods
In the present cohort study, all participants, aged 18 years or older, were enrolled in the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2014. Depressive symptoms score was assessed using the validated 9-item Patient Health Questionnaire Depression Scale (PHQ-9), which ranges from 0 to 27, with a PHQ-9 score ≥ 10 diagnosed as depression. The outcome events were all-cause and CVD mortality, which were followed up from 2005 to 2014. The associations of both depressive symptoms score and certain specific depressive symptoms with all-cause and CVD mortality were examined by weighted multivariable proportional hazards models.
Results
A total of 26,028 participants aged ≥ 18 years were included in the statistical analysis, including 12,813 (49.2%) males and 13,215 (50.8%) females, with a mean (SD) age of 47.34 (18.86) years. During the 9.32 (3.20) years of mean (SD) follow-up, 3261 deaths were recorded, of which 826 were cardiovascular deaths. All-cause mortality was 16.87/1000 person-years in subjects with depression. In terms of CVD mortality, these figures were 4.53/1000 person-years. In the full model (model 3), elevated depressive symptoms scores were independently associated with an increased risk of all-cause mortality (Highest depression symptom score group: adjusted hazard ratio, 1.63; 95% CI 1.44–1.85) and CVD mortality (Highest depression symptom score group: adjusted hazard ratio, 1.73; 95% CI 1.34–2.24). All 9 specific depressive symptoms that make up the PHQ-9 were related to an increased risk of all-cause mortality. However, only 3 symptoms, including trouble sleeping or sleeping too much, poor appetite or overeating, and suicidal ideation, were no significantly associated with an increased risk of CVD mortality.
Conclusions
The elevated depressive symptoms scores were strongly associated with an increased risk of all-cause and CVD mortality in US adults. Furthermore, all 9 specific depressive symptoms were associated with high all-cause mortality. However, trouble sleeping or sleeping too much, poor appetite or overeating, and suicidal ideation might not increase the risk of CVD mortality.
Similar content being viewed by others
Introduction
Depression is one of the most common mental disorders in the world, and depressive symptoms are also common in the population [1]. Like much of the world, the prevalence of Americans is increasing. The incidence of depression has become an increasingly important public-health priority [2]. Studies have shown that the lifetime and 12-month prevalence are 20.6% and about 10.4%, respectively, and the prevalence of women (26.1%) is higher than that of men (14.7%) [3]. Notably, depressive symptoms have been associated with death from all causes, such as all-cause mortality, cardiovascular disease (CVD) mortality, and cancer mortality [3,4,5,6]. The higher the severity of depressive symptoms, the greater the risk of death [7]. Therefore, to reduce mortality, understanding the association between depressive symptoms and mortality is important.
Currently, depressive symptoms are mainly assessed by some rating scales, such as the Center for Epidemiological Studies Depression Scale (CES-D) [8] and the Geriatric Depression Scale [9]. These scales identify depression disorder with established and validated cut-off points, and although these scales cannot diagnose major depressive disorders, they have been widely applied in research and daily practice. Most previous studies [5, 7, 10,11,12] examining the association between depressive symptoms and risk of death have only analyzed the presence or absence of depression or the total score on the scales. Although analyzing specific depression symptoms is also essential [13], there is a lack of evidence to support an association between specific depressive symptoms and mortality. Sheida Zolfaghari et al. found that sleep disorders (one form of depressive symptom) were associated with an increased risk of death, and that these effects differed by gender [14]. Quanhe Yang et al. reported that poor appetite or overeating was independently associated with both all-cause and cardiovascular mortality [11]. However, there are very few such studies, and the relationship between each specific depressive symptom and mortality is unclear. Due to the heterogeneity of depressive symptoms and important differences between depressed individuals, therefore, studies on specific depressive symptoms associated with mortality could provide new ideas for individualized treatment of patients with depression disorder.
Until now, the impact of both depressive symptoms scores and specific depressive symptoms on all-cause and CVD mortality has remained unknown, which prompted us to conduct this study. We assumed that depressive symptoms scores and certain specific depressive symptoms would be associated with an increased risk of all-cause and CVD mortality.
Methods
Study population
This study is a cohort study with data from the publicly available National Health and Nutrition Examination Survey (NHANES) database. Conducted every 2 years, the health survey program uses a complex, multicenter, stratified sampling design with data collected from a nationally representative sample of U.S. civilians to monitor the health and nutritional status of adults and children across the United States [15]. Details of the survey design and the method are available on the NHANES website (https://www.cdc.gov/nchs/nhanes/index.htm).
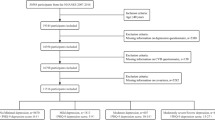
This study initially included participants aged ≥ 18 years from five survey cycles in the period 2005–2014. 4211 participants with incomplete information on depressive symptoms were excluded, and 26,028 participants were included in the final analysis. What is more, all participants included in the final analysis were effectively followed up. The project was approved by the Research Ethics Review Board of the National Center for Health Statistics (Protocol #2005-06 and #2011-17) and was in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines (https://www.cdc.gov/nchs/nhanes/irba98.htm). Informed consent has been obtained from all participants for the NHANES data. Due to the free availability of the NHANES database, the present study does not require additional ethical review and approval.
Evaluation of depressive symptoms
The depressive symptoms of the study subjects were assessed according to the 9-item Patient Health Questionnaire Depression Scale (PHQ-9) [16, 17]. The PHQ-9 is an internationally validated screening and diagnostic tool for depressive symptoms that assesses the frequency and severity of various depressive symptoms over the past two weeks [18]. PHQ-9 is composed of 9 items: (1) have little interest in doing things; (2) feeling down, depressed, or hopeless; (3) trouble sleeping or sleeping too much; (4) feeling tired or having little energy; (5) poor appetite or overeating; (6) feeling bad about yourself; (7) trouble concentrating on things; (8) moving or speaking slowly or too fast; and (9) thought you would be better off dead. Each question was scored as 0 (not at all); 1 (several days); 2 (more than half the days); and 3 (nearly every day) [16]. The total score was calculated by summing the scores for each item and ranged from 0 to 27, with depressive symptom severity increasing with the score. Based on the diagnostic criteria for depression in the NHANES, participants with scores ≥ 10 were considered to suffer from depression [19].
Assessment of outcome status
The primary outcome indicators for this study consisted of all-cause mortality and CVD mortality. The survival status of participants was tracked through death files, which were collected by the NHANES-linked National Death Index (NDI) (https://www.cdc.gov/nchs/data-linkage/mortality-public.htm#). The files provide details of follow-up visits from the date of the interview to December 31, 2015. The specific causes of death are classified according to the International Classification of Diseases guidelines, 10th revision (ICD-10). All-cause mortality was ascribed to death from any cause. CVD mortality was determined as death due to cardiovascular disease (ICD-10 codes: I00-I09, I11, I13, and I20-I51) or cerebrovascular disease (ICD-10 codes: I60-I69).
Ascertainment of covariates
Demographic information was acquired through interviews and questionnaires: age, sex, race (Mexican, Non-Hispanic white, Non-Hispanic black, and other), and education level (Less than high school, High school, and above high school). A physical examination was conducted by professional medical examiners to obtain relevant index data: waist, systolic blood pressure (SBP), and diastolic blood pressure (DBP). Personal history included self-reported smoking status and drinking status (Never, Former, or Current). Medical Conditions consist of Congestive heart failure, Coronary heart disease, Hypertension, Hyperlipidemia, Diabetes, Chronic kidney disease (CKD), and Stroke. Hypertension was defined as meeting one of the following criteria: (1) SBP ≥ 140 mmHg or DBP ≥ 90 mmHg measured at baseline; (2) taking antihypertensive medication; (3) a self-reported history of hypertension [20]. Diabetes was characterized by fasting blood glucose ≥ 7.0 mmol/L or hemoglobin ≥ 6.5%, a self-reported history of diabetes, or being on anti-diabetic medication [21]. Hyperlipidemia was described as one of the following conditions: (1) triglycerides ≥ 150 mg/dL; (2) total cholesterol ≥ 200 mg/dL; (3) low-density lipoprotein-cholesterol ≥ 130 mg/dL; (4) high-density lipoprotein-cholesterol < 40 mg/dL (male) or < 50 mg/dL (female); and (5) use of cholesterol-lowering drugs [22]. An estimated glomerular filtration rate (eGFR) of < 60 mL/min/1.73 m2 was classified as CKD [23]. The eGFR was measured with the Scr formula recommended by the Chronic Kidney Disease Epidemiology Collaborative Group in 2009 [24]. The details of all data could be found at https://www.cdc.gov/nchs/nhanes/.
Statistical analyses
The data were weighted with the Taylor linearization method according to the design of NHANES multi-stage probability sampling. Continuous variables were expressed as mean (standard deviation, SD), and categorical variables were displayed as frequency (percentage). Baseline characteristics of continuous and categorical variables were compared between groups by the T-test and the Chi-square test, respectively. The detailed missing data was described in Supplementary Table 1.
The follow-up period ranged from the survey date at baseline (2005–2014) to the time of death, end of follow-up, or loss of follow-up, depending on each participant. All-cause and CVD mortality rates for each 1000 person-years were computed based on depressive symptoms. Cox proportional hazard regression models were performed to explore the association of both depressive symptoms scores and specific depressive symptoms with all-cause and CVD mortality, and the results were expressed as hazard ratios (HRs) and 95% confidence intervals (CIs). There were three models: Model 1 adjusted for sex, age, and race; Model 2 adjusted for age, sex, race, education level, smoking status, drinking status, waist, and SBP; and Model 3 made additional adjustments for congestive heart failure, coronary heart disease, hypertension, hyperlipidemia, diabetes, chronic kidney disease, and stroke based on Model 2. In addition, nine specific depressive symptoms were simultaneously added to Model 3 for analysis.
Furthermore, participants were divided into 5 groups (Q1: 0–0, Q2: 0–1, Q3: 1–2, Q4: 2–4, Q5: 5–27) based on quintiles of total depressive symptoms scores. The correlations between depressive symptoms scores and mortality were examined using Cox proportional risk regression models (models 1–3), with the Q1 group as the reference group. Meanwhile, restricted cubic spline (RCS) plots were performed to show the dose–response relationship between total depressive symptoms scores and all-cause and CVD mortality. Kaplan–Meier curves and log-rank tests were conducted to describe the association between depressive symptom scores and the corresponding survival rates. Stratification by baseline characteristics (age, sex, and race, education level, smoking status, drinking status, waist, congestive heart failure, coronary heart disease, hypertension, hyperlipidemia, diabetes, chronic kidney disease, and stroke) was performed to explore whether the association between depressive symptoms scores (Q1-Q5) and the risk of all-cause and CVD mortality differs in different subgroups. The P-value for interaction was applied to reflect whether interactions occurred, and the P-value for trend was applied to examine the trend of linear change.
Sensitivity analyses were performed: participants with missing values (n = 4476) were excluded, and the Cox proportional risk regression analysis was repeated for participants with complete data (n = 21,552). All tests were performed using two-sided tests a statistical significance level of 0.05. Statistical analyses were performed through R 4.2.1 software.
Results
The baseline characteristics of the study population are shown in Table 1. A total of 26,028 participants aged ≥ 18 years were included in the statistical analysis, including 12,813 (49.2%) males and 13,215 (50.8%) females, with a mean (SD) age of 47.34 (18.86) years. At baseline, 2291 (8.8%) participants were diagnosed with depression disorder (total score of PHQ-9 ≥ 10). Compared with the non-depressed population, the depressed population were more likely to be female (64.3% vs. 49.5%; P-value < 0.001), have less than high school education (38.5% vs. 25.3%; P-value < 0.001), be smokers (37.8% vs 19.6%; P-value < 0.001), be former drinkers (24.7% vs 18.1%; P-value < 0.001), have combination of Congestive heart failure (6.7% vs 2.8%; P-value < 0.001), Coronary heart disease (6.4% vs 3.7%; P-value < 0.001), Hypertension (49.6% vs 38.8%; P-value < 0.001), Hyperlipidemia (73.9% vs 67.7%; P-value < 0.001), Diabetes (25.6% vs 16.4%; P-value < 0.001), Chronic kidney disease (21.5% vs 17.6%; P-value < 0.001), and Stroke (7.9% vs 3.5%; P-value < 0.001), and have higher levels of DBP (mean [SD], 70.23 [12.49] vs 69.26 [12.12]; P-value < 0.001) and waist (mean [SD], 101.77 [18.34] vs 97.97 [16.19]; P-value < 0.001). There were no significant differences in age, race, and SBP between the two groups. In addition, the baseline characteristics of participants with complete data information (n = 21,552) are shown in Supplementary Table 2, and similar baseline differences were found.
Between the follow-up periods of 2005 and 2014, 3261 deaths were recorded, of which 826 were CVD deaths. All-cause mortality was 16.87/1000 person-years in subjects with depression and 13.13/1000 person-years in subjects without depression. In terms of CVD mortality, these figures were 4.53/1000 person-years and 3.30/1000 person-years, respectively. Table 2 displays the relationships between depression with all-cause and CVD mortality in models 1, 2, and 3. After full adjustment for potential confounders (Model 3), the presence of depression increased the risk of all-cause mortality by 51% (HR, 1.51; 95% CI 1.30–1.76; P-value < 0.001) and the risk of CVD mortality by 76% (HR, 1.76; 95% CI 1.36–2.26; P-value < 0.001). Participants with missing values were excluded, and consistent results were gained when the remaining complete data were re-analyzed (Supplementary Table 3). Participants were divided into five groups according to the quintiles of the total PHQ-9 score, as shown in Table 2. Participants in the Q5 group had a significantly higher incidence of all-cause mortality (HR, 1.63; 95% CI 1.44–1.85; P-value < 0.001) compared to the reference group (Q1). Similar results were obtained for CVD mortality using the same statistical treatment (HR, 1.73; 95% CI 1.34–2.24; P-value < 0.001). RCS plots demonstrated that there were linear relationships between total depressive symptom scores with all-cause (P-value for nonlinear = 0.074) and CVD mortality (P-value for nonlinear = 0.182). All-cause and CVD mortality tended to increase in the same direction as the total depressive symptom score, as shown in Fig. 1A and B. Consistent results were obtained in Kaplan–Meier survival curves. With the extension of the follow-up period, the survival rate of each depressive symptom score group tended to decrease, either in the all-cause mortality group (Fig. 2A) or the CVD mortality group (Fig. 2B). In addition, the survival rate of the low-score group was always higher than that of the high-score group at the same time period.
The correlations of specific depressive symptoms with all-cause mortality and CVD mortality were explored in Table 3. All nine items in the PHQ-9 were independently associated with all-cause mortality after full adjustment for confounders: Uninterested in things (adjusted HR, 1.21; 95% CI 1.14–1.28; P-value < 0.001), Feeling down (adjusted HR, 1.19; 95% CI 1.12–1.26; P-value < 0.001), Sleep problems (adjusted HR, 1.07; 95% CI 1.02–1.12; P-value < 0.001), Tiredness (adjusted HR, 1.18; 95% CI 1.12–1.24; P-value < 0.01), Change of appetite (adjusted HR, 1.15; 95% CI 1.09–1.22; P-value < 0.001), Feeling bad about yourself (adjusted HR, 1.14; 95% CI 1.08–1.22; P-value < 0.001), Difficulty in concentration (adjusted HR, 1.15; 95% CI 1.08–1.23; P-value < 0.001), Change in speed of action (adjusted HR, 1.18; 95% CI 1.09–1.29; P-value < 0.001), Suicidal ideation (adjusted HR, 1.26; 95% CI 1.10–1.44; P-value < 0.001). Similarly, six items were significantly associated with CVD mortality, and the details are shown in Table 3.
The stratified Cox proportional risk regression analyses were performed to investigate whether the associations between the severity of depressive symptoms score and mortality were influenced by confounding factors, and the results are summarized in Table 4. There were significant interactions between age (P-value for interaction = 0.004) and drinking status (P-value for interaction = 0.01) on the association between depressive symptoms score and all-cause mortality. In different age subgroups, the positive association between depressive symptoms score and all-cause mortality was stronger in individuals ≤ 65 years (adjusted HR, 1.59; 95% CI 1.26–1.99) compared to those > 65 years (adjusted HR, 1.42; 95% CI 1.22–1.65). In subgroups with different statuses, the positive association between depressive symptoms score and all-cause mortality was more prominent in former drinkers (adjusted HR, 1.72; 95% CI 1.42–2.07) compared with never drinkers (adjusted HR, 1.63; 95% CI 1.15–2.32) and current drinkers (adjusted HR, 1.57; 95% CI 1.32–1.88). There was no significant interaction between depressive symptom score and CVD mortality in any subgroup (all P-values for interaction > 0.05).
Discussion
We found both a linear and positive association between depressive symptom score with all-cause and CVD mortality from the NHANES database of 26,028 USA adults. Participants with depression had an increased risk of all-cause mortality and CVD mortality by 51% and 76%, respectively, compared with participants without depression. In addition, the presence of all nine depressive symptoms (uninterested in things, feeling down, sleep problems, tiredness, change of appetite, feeling bad about yourself, difficulty in concentration, change in speed of action, and suicidal ideation) in the PHQ-9 was independently associated with all-cause mortality, and the presence of six symptoms (except sleep problems, change of appetite, and suicidal ideation) was independently correlated with CVD mortality. Furthermore, there were significant interactions between age and drinking status on depression symptom score and all-cause mortality.
The association between major depression and mortality has been investigated in different populations from different countries [11, 25,26,27,28,29,30]. The Helsinki Birth Cohort Study followed 1995 participants in Finland for a mean duration of 14.1 years. Depression was diagnosed according to the Beck Depression Inventory, and increased mortality was observed as a result of depression (melancholic depressive disorder: adjusted HR, 1.49; 95% CI 1.02–2.20; non-melancholic depressive disorder: adjusted HR, 1.12; 95% CI 0.83–1.52) [31]. Another study of 24,542 participants aged 45–69 years in Central and Eastern Europe reported that an increase in depressive symptoms (“depressive symptoms” assessed by the Center for Epidemiologic Studies Depression Scale) was significantly and positively associated with CVD and all-cause mortality at a median follow-up of 7 years [32]. Meanwhile, a prospective study of 1999 community residents conducted in China with up to 12 years of follow-up discovered that time-dependent depression increased the risk of all-cause (adjusted HR: 1.48; 95% CI 1.26–1.73) and CVD death (adjusted HR: 1.40; 95% CI 1.08–1.82) by 48% and 40%, respectively [28]. Our results are in general agreement with previous studies. However, systematic reviews and meta-analyses have pointed out that this association may have been overestimated due to the large proportion of previous low-quality studies (such as small sample size, short follow-up time, and large cohort heterogeneity) [29, 33]. Considering that our study population was a nationally representative group of adults with a large sample size, the results of this study are highly credible.
Most previous studies classified populations as healthy or depressed by the sum of scale symptoms, ignoring the heterogeneity of depressive symptoms and important differences between individuals with depression [13, 34]. That is one of the main reasons for the slow progress and poor results in the field of clinical antidepressant development [35]. Until now, depression has been shown to be associated with all-cause mortality and cardiovascular mortality, but the association between a single depressive symptom and mortality has been unclear. This study found that all nine items of the PHQ-9 were independently associated with all-cause mortality, of which six were independent risk factors for CVD mortality. This finding provides new ideas for individualized treatment of patients with depression. Restricted activity was associated with chronic conditions, such as cerebrovascular accidents, cardiovascular diseases, and so on. This restricted activity associated with chronic disease appears to be significantly related to suicidal ideation [36]. What’s more, suicidal ideation also contributed largely to heart disease deaths [37]. Trouble sleeping or sleeping too much could increase incident CVD morbidity and mortality, especially among the elderly [38]. Poor appetite leads to poor nutritional status, which causes high mortality among hospitalized older patients [39]. Obesity from overeating reduces working capacity, decreases life quality, leads to high CVD morbidity [40], and causes early death [41, 42]. In addition, among older Chinese people, 2 individual symptoms (disturbed sleep and loneliness) were significantly associated with cardiovascular disease incidence [43]. Having little interest in doing things and Feeling tired or having little energy has been shown to be associated with all-cause mortality and cardiovascular mortality [44]. Importantly, although depressive symptoms tend to fluctuate over time, time-dependent depressive symptoms still increase the risk of all-cause mortality and cardiovascular mortality in the elderly [28]. However, our study found three specific depressive symptoms, including suicidal ideation, sleep problems, and changes in appetite, had no concern with CVD mortality, which might be where our results are inconsistent with previous studies. Three specific symptoms in our study were from PHQ-9 and were used to assess whether there was depression. Inconsistencies in symptom assessment methods might have contributed to the variable study results. Moreover, although the overall sample size of this study is large, the research specific to a certain depressive symptom weakens the sample size.
In the present study, subgroup analysis revealed an interaction between age and drinking status on the association between depressive symptoms scores and all-cause mortality. Compared to seniors, young and middle-aged people generally suffer from higher levels of stress due to various factors such as employment, marriage, and support for children and parents [45, 46]. Stress triggers increased inflammatory activity, leading to the onset and progression of depression [47]. In addition, elderly patients with depression usually have a combination of other chronic diseases and take more medications, some of which have the effect of inhibiting the inflammatory response. As a result, people with depression aged < 65 years have a higher risk of all-cause mortality compared to those aged ≥ 65 years. Drinking is related to an increased risk of premature death and physical and mental health problems in China [48]. The risk of symptoms of depression and anxiety is higher in abstainers and heavy drinkers [49]. Compared to moderate drinkers, the former and heavy drinkers continued to show increased risks of 51 and 45% for all-cause mortality in older adults, respectively [50]. Tom et al. revealed there were significant interactions between male drinkers and female ex-drinkers on the association between depressive symptoms and 11-year all-cause mortality [10]. This explained in part that there was high mortality in the former drinker with depression.
The association between depressive symptoms and increased risk of death is complex, with unhealthy lifestyle habits and pathophysiological changes being the focus of attention among many possible mechanisms. The depressed population often has poor lifestyle habits, such as smoking, excessive energy intake, overconsumption of alcohol, and a lack of exercise, among others [17, 51,52,53,54]. These unhealthy lifestyles have been recognized as risk factors for many chronic diseases such as CVD, metabolic diseases, and cancer, which further increase the risk of death [11, 55,56,57]. Similar results have been reported in several other studies [53, 58,59,60]. To sum up the above, quitting smoking, moderate alcohol consumption, and appropriate exercise may reduce the risk of death in individuals with depression. In terms of pathophysiology, depression increases the risk of death mainly through dysregulated inflammatory responses, oxidative stress damage, and hypothalamic–pituitary–adrenal (HPA) axis disorders. Higher levels of pro-inflammatory mediators, such as interleukin 6 (IL-6), C-reactive protein (CRP), and tumor necrosis factor⁃α (TNF-α), are usually detected in the blood of depressed patients compared to the healthy population [61]. Not only does inflammation play a key role in the development and progression of CVD (e.g., hypertension [62, 63], coronary atherosclerotic heart disease [64, 65], and heart failure [66]), but it is also closely related to other diseases such as diabetes, cancer, and the metabolic syndrome [14, 67,68,69]. In addition, inflammation-related factors activate cortisol secretion at three levels: the hypothalamus, pituitary, and adrenal cortex [70]. The HPA axis is hyperactive in depressed patients, resulting in a loss of circadian rhythm of cortisol secretion and a weakened ability to inhibit inflammatory control pathways, further producing more inflammatory responses and creating “positive feedback” [71].
Strengths and limitations
The merits of this study include the national representativeness of the data, the large sample size, and the prospective design, which make the conclusions more convincing. In addition, we analyzed the associations of a single specific depressive symptom with outcomes (all-cause and CVD mortality), which is crucial. There are still some limitations to our study. Firstly, there were unadjusted residual confounding factors, such as marital status, depression-related medication use, etc. Secondly, causality could not be deduced since the study was an observational study. Thirdly, this study was conducted in the United States, and further validation is needed to see if the results could be generalized to other populations.
Conclusions
The elevated depressive symptoms scores were strongly associated with an increased risk of all-cause and CVD mortality in USA adults. All nine items of the PHQ-9 were independently associated with all-cause mortality, of which six were independent risk factors for CVD mortality (trouble sleeping or sleeping too much, poor appetite or overeating, and suicidal ideation might not increase the risk of CVD mortality). These findings might be of significant value for the individualized treatment of patients with specific depressive symptoms.
Data availability
The data of the present study can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.
References
Liu Q, Cai H, Yang LH, Xiang YB, Yang G, Li H, Gao YT, Zheng W, Susser E, Shu XO. Depressive symptoms and their association with social determinants and chronic diseases in middle-aged and elderly Chinese people. Sci Rep. 2018;8(1):3841.
Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, Vos T, Whiteford HA. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11): e1001547.
Lee SY, Lee JP, Lee J, Park JY, Kim EY. Association between depressive symptoms and the risk of all-cause and cardiovascular mortality among US adults. Prog Neuropsychopharmacol Biol Psychiatry. 2023;125: 110755.
Prigge R, Wild SH, Jackson CA. Depression, diabetes, comorbid depression and diabetes and risk of all-cause and cause-specific mortality: a prospective cohort study. Diabetologia. 2022;65(9):1450–60.
Wei J, Lu Y, Li K, Goodman M, Xu H. The associations of late-life depression with all-cause and cardiovascular mortality: the NHANES 2005–2014. J Affect Disord. 2022;300:189–94.
Pinquart M, Duberstein PR. Depression and cancer mortality: a meta-analysis. Psychol Med. 2010;40(11):1797–810.
Xia W, Jiang H, Di H, Feng J, Meng X, Xu M, Gan Y, Liu T, Lu Z. Association between self-reported depression and risk of all-cause mortality and cause-specific mortality. J Affect Disord. 2022;299:353–8.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77–84.
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37–49.
Greenfield TK, Rehm J, Rogers JD. Effects of depression and social integration on the relationship between alcohol consumption and all-cause mortality. Addiction (Abingdon, England). 2002;97(1):29–38.
Meng R, Yu C, Liu N, He M, Lv J, Guo Y, Bian Z, Yang L, Chen Y, Zhang X, et al. Association of depression with all-cause and cardiovascular disease mortality among adults in China. JAMA Netw Open. 2020;3(2): e1921043.
Gilman SE, Sucha E, Kingsbury M, Horton NJ, Murphy JM, Colman I. Depression and mortality in a longitudinal study: 1952–2011. Can Med Assoc J. 2017;189(42):1304–10.
Fried EI, Nesse RM. Depression sum-scores don’t add up: why analyzing specific depression symptoms is essential. BMC Med. 2015;13:72.
Zolfaghari S, Keil A, Pelletier A, Postuma RB. Sleep disorders and mortality: a prospective study in the Canadian longitudinal study on aging. Sleep Med. 2024;114:128–36.
Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, Curtin LR. National health and nutrition examination survey: analytic guidelines, 1999–2010, Vital and health statistics series 2. Data Eval Methods Res. 2013;161:1–24.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Patel JS, Oh Y, Rand KL, Wu W, Cyders MA, Kroenke K, Stewart JC. Measurement invariance of the patient health questionnaire-9 (PHQ-9) depression screener in US adults across sex, race/ethnicity, and education level: NHANES 2005–2016. Depress Anxiety. 2019;36(9):813–23.
Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, Aguglia A, Belvederi Murri M, Brakoulias V, Amore M, et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): a systematic review. J Affect Disord. 2021;279:473–83.
Negeri ZF, Levis B, Sun Y, He C, Krishnan A, Wu Y, Bhandari PM, Neupane D, Brehaut E, Benedetti A, et al. Accuracy of the Patient Health Questionnaire-9 for screening to detect major depression: updated systematic review and individual participant data meta-analysis. BMJ (Clinical research ed). 2021;375: n2183.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20.
Classification and Diagnosis of Diabetes. Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S14-s31.
National Cholesterol Education Program (US). Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106(25):3143–421.
Levey AS, Coresh J, Bolton K, Culleton B, Harvey KS, Ikizler TA, Johnson CA, Kausz A, Kimmel PL, Kusek J, Levin A. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1-266.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Felipe LRR, Barbosa KSS, Virtuoso Junior JS. Depressive symptoms and mortality in older people in Latin America: systematic review and meta-analysisSíntomas de depresión y mortalidad en personas mayores en América Latina: revisión sistemática con metanálisis. Pan Am J Public Health. 2022;46: e205.
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–50.
Corrêa VP, Confortin SC, d’Orsi E, de Sá-Junior AR, de Oliveira C, Schneider IJC. Depressive symptoms as an independent risk factor for mortality. Rev Brasil Psiquiatr. 2021;43(3):247–53.
Li H, Van Halm-Lutterodt N, Zheng D, Liu Y, Guo J, Feng W, Li X, Wang A, Liu X, Tao L, et al. Time-dependent depressive symptoms and risk of cardiovascular and all-cause mortality among the Chinese elderly: the Beijing Longitudinal Study of Aging. J Cardiol. 2018;72(4):356–62.
Machado MO, Veronese N, Sanches M, Stubbs B, Koyanagi A, Thompson T, Tzoulaki I, Solmi M, Vancampfort D, Schuch FB, et al. The association of depression and all-cause and cause-specific mortality: an umbrella review of systematic reviews and meta-analyses. BMC Med. 2018;16(1):112.
Moise N, Khodneva Y, Jannat-Khah DP, Richman J, Davidson KW, Kronish IM, Shaffer J, Safford MM. Observational study of the differential impact of time-varying depressive symptoms on all-cause and cause-specific mortality by health status in community-dwelling adults: the REGARDS study. BMJ Open. 2018;8(1): e017385.
Eriksson MD, Eriksson JG, Korhonen P, Koponen H, Salonen MK, Mikkola TM, Kajantie E, Wasenius NS, von Bonsdorff M, Kautiainen H, et al. Depressive symptoms and mortality-findings from Helsinki birth cohort study. Acta Psychiatr Scand. 2023;147(2):175–85.
Kozela M, Bobak M, Besala A, Micek A, Kubinova R, Malyutina S, Denisova D, Richards M, Pikhart H, Peasey A, et al. The association of depressive symptoms with cardiovascular and all-cause mortality in Central and Eastern Europe: prospective results of the HAPIEE study. Eur J Prev Cardiol. 2016;23(17):1839–47.
Wei J, Hou R, Zhang X, Xu H, Xie L, Chandrasekar EK, Ying M, Goodman M. The association of late-life depression with all-cause and cardiovascular mortality among community-dwelling older adults: systematic review and meta-analysis. Br J Psychiatry. 2019;215(2):449–55.
Fried EI. Problematic assumptions have slowed down depression research: why symptoms, not syndromes are the way forward. Front Psychol. 2015;6:309.
Fried EI, Nesse RM. Depression is not a consistent syndrome: an investigation of unique symptom patterns in the STAR*D study. J Affect Disord. 2015;172:96–102.
Jang SY, Choi B, Ju EY, Kim YM, Kang SB, Park S, Yang SH, Joo MH, Kim IH. Association between restriction of activity related to chronic diseases and suicidal ideation in older adults in Korea. Geriatr Gerontol Int. 2014;14(4):983–8.
Batterham PJ, Calear AL, Mackinnon AJ, Christensen H. The association between suicidal ideation and increased mortality from natural causes. J Affect Disord. 2013;150(3):855–60.
Newman AB, Spiekerman CF, Enright P, Lefkowitz D, Manolio T, Reynolds CF, Robbins J, The Cardiovascular Health Study Research Group. Daytime sleepiness predicts mortality and cardiovascular disease in older adults. J Am Geriatr Soc. 2000;48(2):115–23.
Cox NJ, Er Lim S, Howson F, Moyses H, Ibrahim K, Sayer AA, Roberts HC, Robinson SM. Poor appetite is associated with six month mortality in hospitalised older men and women. J Nutr Health Aging. 2020;24(10):1107–10.
Manuel DG, Perez R, Sanmartin C, Taljaard M, Hennessy D, Wilson K, Tanuseputro P, Manson H, Bennett C, Tuna M, et al. Measuring burden of unhealthy behaviours using a multivariable predictive approach: life expectancy lost in Canada attributable to smoking, alcohol, physical inactivity, and diet. PLoS Med. 2016;13(8): e1002082.
Hall KD, Sacks G, Chandramohan D, Chow CC, Wang YC, Gortmaker SL, Swinburn BA. Quantification of the effect of energy imbalance on bodyweight. Lancet (London, England). 2011;378(9793):826–37.
Engin A. Eat and death: chronic over-eating. Adv Exp Med Biol. 2017;960:53–80.
Li H, Zheng D, Li Z, Wu Z, Feng W, Cao X, Wang J, Gao Q, Li X, Wang W, et al. Association of depressive symptoms with incident cardiovascular diseases in middle-aged and older Chinese adults. JAMA Netw Open. 2019;2(12): e1916591.
Zhang Z, Jackson SL, Gillespie C, Merritt R, Yang Q. Depressive symptoms and mortality among US adults. JAMA Netw Open. 2023;6(10): e2337011.
Stone AA, Schneider S, Broderick JE. Psychological stress declines rapidly from age 50 in the United States: yet another well-being paradox. J Psychosom Res. 2017;103:22–8.
Aldwin CM, Sutton KJ, Chiara G, Spiro A 3rd. Age differences in stress, coping, and appraisal: findings from the normative aging study. J Gerontol B Psychol Sci Soc Sci. 1996;51(4):P179-188.
Yang L, Zhao Y, Wang Y, Liu L, Zhang X, Li B, Cui R. The effects of psychological stress on depression. Curr Neuropharmacol. 2015;13(4):494–504.
Im PK, Millwood IY, Chen Y, Guo Y, Du H, Kartsonaki C, Bian Z, Tan Y, Su J, Li Y, et al. Problem drinking, wellbeing and mortality risk in Chinese men: findings from the China Kadoorie Biobank. Addiction (Abingdon, England). 2020;115(5):850–62.
Rodgers B, Korten AE, Jorm AF, Jacomb PA, Christensen H, Henderson AS. Non-linear relationships in associations of depression and anxiety with alcohol use. Psychol Med. 2000;30(2):421–32.
Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos BS, Moos RH. Late-life alcohol consumption and 20-year mortality. Alcohol Clin Exp Res. 2010;34(11):1961–71.
Ljungberg T, Bondza E, Lethin C. Evidence of the importance of dietary habits regarding depressive symptoms and depression. Int J Environ Res Public Health. 2020;17(5):1616.
Hoveling LA, Liefbroer AC, Schweren LJS, Bültmann U, Smidt N. Socioeconomic differences in major depressive disorder onset among adults are partially explained by lifestyle factors: a longitudinal analysis of the Lifelines Cohort Study. J Affect Disord. 2022;314:309–17.
Werneck AO, Vancampfort D, Stubbs B, Silva DR, Cucato GG, Christofaro DGD, Santos RD, Ritti-Dias RM, Bittencourt MS. Prospective associations between multiple lifestyle behaviors and depressive symptoms. J Affect Disord. 2022;301:233–9.
Marijnissen RM, Naudé PJ, Comijs HC, Schoevers RA, Oude Voshaar RC. Waist circumference and neutrophil gelatinase-associated lipocalin in late-life depression. Brain Behav Immun. 2014;37:231–9.
Soh Y, Tiemeier H, Kawachi I, Berkman LF, Kubzansky LD. Eight-year depressive symptom trajectories and incident stroke: a 10-year follow-up of the HRS (health and retirement study). Stroke. 2022;53(8):2569–76.
Burns RJ, Briner E, Schmitz N. Trajectories of depressive symptoms and incident diabetes: a prospective study. Ann Behav Med. 2022;56(3):311–6.
McFarland DC, Doherty M, Atkinson TM, O’Hanlon R, Breitbart W, Nelson CJ, Miller AH. Cancer-related inflammation and depressive symptoms: systematic review and meta-analysis. Cancer. 2022;128(13):2504–19.
Rantanen AT, Korkeila JJA, Löyttyniemi ES, Saxén UKM, Korhonen PE. Awareness of hypertension and depressive symptoms: a cross-sectional study in a primary care population. Scand J Prim Health Care. 2018;36(3):323–8.
van den Berg KS, Wiersema C, Hegeman JM, van den Brink RHS, Rhebergen D, Marijnissen RM, Oude Voshaar RC. Clinical characteristics of late-life depression predicting mortality. Aging Ment Health. 2021;25(3):476–83.
Hjorthøj C, Østergaard ML, Benros ME, Toftdahl NG, Erlangsen A, Andersen JT, Nordentoft M. Association between alcohol and substance use disorders and all-cause and cause-specific mortality in schizophrenia, bipolar disorder, and unipolar depression: a nationwide, prospective, register-based study. Lancet Psychiatry. 2015;2(9):801–8.
Beurel E, Toups M, Nemeroff CB. The bidirectional relationship of depression and inflammation: double trouble. Neuron. 2020;107(2):234–56.
Xiao L, Harrison DG. Inflammation in hypertension. Can J Cardiol. 2020;36(5):635–47.
Bergantin LB. Depression rises the risk of hypertension incidence: discussing the link through the Ca2+/cAMP signalling. Curr Hypertens Rev. 2020;16(1):73–8.
Kong P, Cui ZY, Huang XF, Zhang DD, Guo RJ, Han M. Inflammation and atherosclerosis: signaling pathways and therapeutic intervention. Signal Transduct Target Ther. 2022;7(1):131.
Chrysohoou C, Kollia N, Tousoulis D. The link between depression and atherosclerosis through the pathways of inflammation and endothelium dysfunction. Maturitas. 2018;109:1–5.
Li Z, Zhao H, Wang J. Metabolism and chronic inflammation: the links between chronic heart failure and comorbidities. Front Cardiovasc Med. 2021;8: 650278.
Schachter J, Martel J, Lin CS, Chang CJ, Wu TR, Lu CC, Ko YF, Lai HC, Ojcius DM, Young JD. Effects of obesity on depression: a role for inflammation and the gut microbiota. Brain Behav Immun. 2018;69:1–8.
Dregan A, Rayner L, Davis KAS, Bakolis I, Arias de Torre J, Das-Munshi J, Hatch SL, Stewart R, Hotopf M. Associations between depression, arterial stiffness, and metabolic syndrome among adults in the UK Biobank population study: a mediation analysis. JAMA Psychiatry. 2020;77(6):598–606.
Polityńska B, Pokorska O, Wojtukiewicz AM, Sawicka M, Myśliwiec M, Honn KV, Tucker SC, Wojtukiewicz MZ. Is depression the missing link between inflammatory mediators and cancer? Pharmacol Ther. 2022;240: 108293.
Silverman MN, Sternberg EM. Glucocorticoid regulation of inflammation and its functional correlates: from HPA axis to glucocorticoid receptor dysfunction. Ann NY Acad Sci. 2012;1261:55–63.
Rothenberg DO, Zhang L. Mechanisms underlying the anti-depressive effects of regular tea consumption. Nutrients. 2019;11(6):1361.
Acknowledgements
Thanks to Zhang Jing (Shanghai Tongren Hospital) for his work on the NHANES database. His outstanding work, nhanesR package and webpage, makes it easier for us to explore NHANES database.
Funding
This work was supported by Shanghai University of Medical and Health Sciences Research Fund Project (Grant number: SSF-23–25-002), the Shanghai Jinshan District Health Commission Project Fund (Grant number: JSKJ-KTQN-2022–11 and JSKJ-KTMS-2020–09), and the Shanghai Jinshan District Medical and Health Science and Technology Innovation Fund Project (Grant number: 2022-WS-61).
Author information
Authors and Affiliations
Contributions
Tao Liu: Investigation, Methodology, Formal analysis, Conceptualization, Writing-Original Draft and Funding; Lili Wang: Methodology, Software, Validation; Lifang Sun, Zhijian Zhu, Bing Wang, and Zhigang Lu: Conceptualization, Investigation and Resources; Yesheng Pan: Conceptualization, Supervision, Project administration and Funding.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The project was approved by the Research Ethics Review Board of the National Center for Health Statistics (Protocol #2005–06 and #2011–17) and was in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines (https://www.cdc.gov/nchs/nhanes/irba98.htm). Informed consent has been obtained from all participants for the NHANES data. Due to the free availability of the NHANES database, the present study does not require additional ethical review and approval.
Competing interests
All patients have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12991_2024_509_MOESM2_ESM.docx
Additional file 2. Baseline characteristics according to depressive symptoms status in subpopulations of 21,552 participants.
12991_2024_509_MOESM3_ESM.docx
Additional file 3. Association of depressive symptoms status with incidence of all-cause mortality and cardiovascular mortality in subpopulations of 21,552 participants.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, T., Wang, L., Zhu, Z. et al. Association of both depressive symptoms scores and specific depressive symptoms with all-cause and cardiovascular disease mortality. Ann Gen Psychiatry 23, 25 (2024). https://doi.org/10.1186/s12991-024-00509-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12991-024-00509-x