Abstract
Background
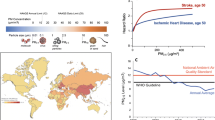
Exposure to air pollution has been associated with adverse effects on human health, and ultimately increased morbidity and mortality. This is predominantly due to hazardous effects on the cardiovascular system. Exposure to particulate matter (PM) is considered to be responsible for the most severe effects.
Main body
Here we summarize current knowledge from existing epidemiological, clinical and animal studies on the influence of PM exposure on high-density lipoprotein (HDL) functionality and the potential initiation and progression of atherosclerosis. We highlight experimental studies that bring support to the causality and point to possible mechanistic links. Recent studies indicate that the functional properties of HDL are more important than the levels per se. Fine (PM2.5–0.1) and ultrafine (UFP) PM are composed of chemicals as well as biological elements that are redox-active and may trigger pro-inflammatory responses. Experimental studies indicate that these properties and responses may promote HDL dysfunction via oxidative pathways. By affecting protein and lipid components of the HDL particle, its anti-atherosclerotic characteristics including cholesterol efflux capacity, as well as other anti-oxidative and anti-inflammatory features might be impaired.
Conclusion
Current literature suggests that PM promotes HDL dysfunction via oxidative pathways. However, as relatively few studies so far have evaluated the impact of particulate air pollution on HDL functionality, more human epidemiological as well as experimental studies are needed to strengthen any possible causal relationship and determine any relevance to atherosclerosis.
Graphical abstract

Similar content being viewed by others
Background
Ambient air pollution is a major public health issue, and is associated with both increased morbidity and mortality [1, 2]. Several studies confirm the link between exposure to particulate matter (PM) and the progression of cardiovascular disease (CVD) [1].
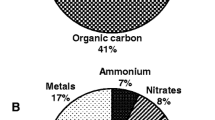
PM is a mixture of particles and liquid droplets suspended in the air, which possesses a variety of organic and inorganic substances [3]. They are classified according to their aerodynamic equivalent diameter into coarse PM10–2.5 (10 μm, > 2.5 μm), fine PM2.5–0.1 (2.5 μm, > 0.1 μm) and ultrafine particles (UFP), (< 0.1 μm). The biological effects of PM are dependent on the composition and size of the particles [3]. Exposure to PM has been linked to several biological processes being central for CVD [1], including atherosclerosis, vasomotor dysfunction, increased blood clot formation, and alterations in heart rhythm [4].
PM-induced ROS and inflammatory reactions linked to atherosclerosis
The prevailing theory regarding the biological mechanism linking PM and CVD is an activation of inflammatory pathways and oxidative stress [2], which may contribute to an initiation of atherogenesis and promotion of atherosclerosis. Human studies show a correlation between PM exposure and increased systemic oxidative stress, based on detection of biomarkers on oxidative alterations in proteins, lipids and DNA in urine or blood [5]. The presence of oxidation in the vascular system is of great relevance, as it may imply involvement of oxidative modifications of plasma lipoproteins which are key players in atherogenesis [6]. It has been demonstrated that ambient PM exhibit pro-inflammatory effects in endothelial cells, macrophages and epithelial cells through generation of reactive oxygen species (ROS) and oxidative stress [7,8,9]. Furthermore, exposure to PM has been associated with increasing levels of pro-inflammatory markers including interleukin (IL)-1β, IL-6 and tumour necrosis factor (TNF)-α [1, 10].
PM has been suggested to induce atherosclerosis either by: i) activation of a lung autonomic reflex, ii) triggering inflammation in the lungs resulting in systemic “spill over” of pro-inflammatory mediators, and/or iii) the translocation of particles or adhered constituents into circulation, thereby reacting with endothelial cells as well as components in the blood, including, lipoproteins [1, 11]. The particles’ reactivity, including surface charge and adhered chemical groups such as polycyclic aromatic hydrocarbons (PAHs) and redox-active metals, are central for these initial reaction steps, and they will thus determine the particle toxicity [11]. Recent studies propose that the key triggering events involved in PM-mediated activation of pro-inflammatory responses occur via direct interaction with molecular targets and lipid layer of cell membranes, activation of cellular receptors, and via reactive metabolites, including ROS with subsequent oxidative stress [12, 13]. Reactive electrophilic metabolites as well as ROS generated directly by PM components or via activation of specific enzymes like NADPH oxidase and myeloperoxidase (MPO) may trigger the release of pro-inflammatory cytokines. PM may also trigger macrophages to release ROS in addition to cytokines [12, 14, 15]. This may be a beneficial physiological response targeting pathogens, including bacteria, mold and virus [2]. However, if sustained over longer periods such pro-inflammatory reactions may promote detrimental effects on the vascular wall.
Atherosclerosis and the role of lipoproteins
Atherosclerosis is well-known as a chronic, low-grade inflammatory process in the arterial wall that predisposes to acute CVDs like myocardial infarction and stroke [16]. Central steps in atherogenesis include development of: i) endothelial dysfunction, ii) increased expression of adhesion molecules and increased permeability, iii) deposition and oxidation of low-density lipoprotein (LDL) in the arterial intima and iv) recruitment of monocytes transforming into macrophages which scavenge the oxidized LDL (ox-LDL) and ultimately transform into foam cells. This may lead to fatty streak formation – a characteristic feature of atherosclerosis [17] (Fig. 1).
Anti-atherogenic features of HDL. Atherosclerosis is an inflammatory condition initiated by accumulation and subsequent oxidation of LDL in the arterial intima. Ox-LDL promotes differentiation of monocytes into macrophages that scavenge ox-LDL and transform into foam cells. Macrophages express cytokines which stimulate the endothelium to express adhesion molecules leading to interaction with circulating monocytes. 1) HDL inhibits expression of adhesion molecules on the epithelium and thereby inhibits monocyte chemotaxis and formation of foam cells. 2) HDL mediates cholesterol efflux and thereby decreases the accumulation of foam cells. 3) The primarily antioxidative effect of HDL is inhibition of oxidation of LDL. HDL: high-density lipoprotein; LDL: low-density lipoprotein; ox-LDL: oxidized low-density lipoprotein. (Inspired by Barter et al. 2004)
Atherosclerosis involves lipid transport characterized by excessive cholesterol in the arterial intima, a process in which the plasma lipoproteins LDL and high-density lipoprotein (HDL) play an essential role. HDL-cholesterol (HDL-C) has often been correlated with a reduced risk of CVD, whereas elevated levels of LDL-cholesterol (LDL-C) have been associated with an increased risk [18, 19].
HDL is a highly heterogenous group, consisting of components differing in size, density and composition [20], acting via numerous pathophysiological mechanisms [21]. Of great importance is the capability of mediating reverse cholesterol transport (RCT) by which HDL scavenges cholesterol from the peripheral vasculature and transports it to the liver. The cholesterol efflux capacity (CEC) is a key feature as it serves as the first step of RCT in the arterial wall. Additionally, HDL possesses significant anti-inflammatory and antioxidant activity facilitated by various enzymes (e.g. paraoxonase). The anti-inflammatory characteristics result in an inhibition of monocyte chemotaxis, while the antioxidant activity mainly provides a protective effect against ox-LDL and thereby reduces cellular uptake by the monocyte-macrophage system [22]. It has also been demonstrated that HDL has beneficial effects on platelet- and endothelial function via nitrogen oxide (NO), a potent vasodilator and anti-platelet agent [23]. Thus, HDL is evidently acting in an atheroprotective matter in multiple ways.
The oxidation of LDL plays a central role in the initiation and progression of atherosclerosis. Apart from leading to the formation of foam cells, the presence of ox-LDL also stimulates cellular proliferation, migration, necrosis and inflammatory changes [24]. The biological effects of ox-LDL have been investigated in numerous studies, while the role of oxidized HDL (ox-HDL) in the context of atherosclerosis and CVD is less known. The relationship between HDL and CVD is complex as the HDL-C levels do not necessarily depict HDL function and thereby its impact on CV health [25]. Thus, newer research has set focus on the functional aspect of the lipoprotein rather than the cholesterol component itself [26].
In recent years, the literature has been growing regarding the role of HDL functionality as a possible mechanistic explanation linking the effects of PM to atherosclerosis. However, no scientific overview of the existing knowledge has been undertaken. Therefore, we will review the current epidemiological and experimental literature on PM and HDL functionality, and summarize the present understanding of the potential mechanisms involved.
Methods
Search strategy and study selection
The objective was to determine the association between PM and HDL functionality by summarizing the findings of epidemiological and experimental studies. Thus, we conducted a PubMed search prior to April 3rd 2020 using the following search terms: (“Lipoproteins, HDL”[Mesh] OR “Cholesterol, HDL”[Mesh]) AND (“Particulate Matter”[Mesh] OR “Air Pollution”[Mesh] OR “Air Pollutants”[Mesh] OR “Inhalation Exposure”[Mesh]). Using this approach 67 publications were found. These were screened at the abstract level. All relevant epidemiological and human exposure studies as well as animal studies assessing the effects of particulate air pollution on HDL functionality were included, resulting in a total of two epidemiological [27, 28], two clinical [29, 30] and three animal studies [31,32,33]. Additional search strategies were also applied focusing on keywords (combinations of keywords): (“HDL” OR “high-density lipoprotein”) AND (“PM” OR “particulate matter” OR “air pollution” OR “inhalation exposure”). This resulted in 225 publications in PubMed. By screening article abstracts, one additional animal study assessing PM and HDL functionality was found [34]. Criteria of inclusion included: general population, language in English, exposure to PM, and outcomes related to HDL functionality parameters such as cholesterol efflux capacity, anti-oxidative and anti-inflammatory properties.
Results
In Tables 1, 2 and 3 an overview of the current studies on PM exposure and measures of various HDL functional properties is presented. Only a few studies have evaluated the impact of PM on HDL functionality. At present, there are two epidemiological studies, two clinical trials and four animal studies.
Epidemiological studies
Results from a study by Mathew et al. showed that exposure to even low levels of PM2.5 (9,1 ± 1,8 μg/m3) for a short period of time were linked to an impaired HDL functionality measured as cholesterol efflux capacity (n = 50) [27]. In the Beijing AIRCHD study, participants were followed up with 4 study visits in a 14-month period (n = 73). Average daily concentration of ambient PM2.5 was high (62,9 μg/m3 (8,1–331,0 μg/m3)). Significant decreases in HDL cholesterol efflux capacity was associated with interquartile range increases in moving average concentrations of PM2.5 during the 1 to 7 days before each participant’s clinical visit. Higher ambient air pollutant levels were also associated with elevated HDL oxidation index (HOI) as well as reduced circulating levels of HDL-C. Furthermore, parameters of systemic oxidative stress and inflammation were found elevated in blood (ox-LDL, malondialdehyde and high-sensitivity C-reactive protein (hs-CRP)) [28], supporting the theory that this may be the mechanistic pathway for PM’s hazardous effects on HDL.
Clinical trials
Maiseyeu et al. were the first to investigate the effects of PM on HDL function in humans (n = 32) [29]. Their controlled exposure study showed that brief inhalation of coarse PM (76,2 ± 51,5 μg/m3) from a rural source did not lead to development of HDL dysfunction as no alterations were found in HDL-cholesterol efflux capacity, HDL oxidation index or paraoxonase (PON) activity. The role of fine PM and impaired HDL functionality was studied by Ramanathan et al. in a clinical trial that explored the effects of fine PM (150 μg/m3) on HDL functionality in humans (n = 30) [30]. They found that brief exposures to concentrated PM2.5 induced acute adverse effects on the antioxidative properties of HDL (measured as HDL oxidation index). The changes in HDL functionality were, however, small, transient, and of short duration. A brief exposure to PM2.5 induced negative effects on HDL functionality that resolved within 24 h after exposure among those with lower HDL oxidation index pre-exposure values. They also assessed paraoxonase activity but did not find any alterations. The PM2.5 levels used in the study were considered significantly higher than in most cities but might be observed for short durations of time.
Animal studies
Araujo et al. reported that the degree of HDL function seems to be dependent on particle-size as ultrafine (113 μg/m3) led to a greater degree of HDL dysfunction (measured as impaired anti-inflammatory capacity) than PM2.5 (439 μg/m3) in an experiment with Apo-E-deficient mice after whole-body exposure (for 40 days) [31]. Additionally, ultrafine particles resulted in larger early atherosclerotic lesions compared to PM2.5. The alterations in HDL functionality were found in the absence of changes in HDL-C levels. An experimental study by Li et al. showed that inhalation exposure to ultrafine particles (360 μg/m3 for 10 weeks) promoted pro-atherogenic lipid metabolism and reduced HDL antioxidative properties (significantly increased HDL oxidation index) in fat-fed LDL receptor-null mice [32]. The decreased antioxidative capacity of HDL was associated with a decrease in paraoxonase activity. Experiments measuring monocyte chemotaxis show marked correlation between impairment of HDL-antioxidant property and impaired anti-inflammatory feature [33, 35]. Hence, HDL oxidation index may serve as a measure of both HDL antioxidant and anti-inflammatory features [30]. A study by Yin et al., where Apo-E-deficient mice were exposed to diesel exhaust (DE) by simple inhalation (≈250 μg/m3 of PM2.5 for 2 weeks) revealed an induction of dysfunctional pro-oxidative HDL without affecting the quantitative levels [33]. Several markers of lipid peroxidation in the blood and liver were strongly correlated with the degree of dysfunction. Paraoxonase activity was found to be significantly reduced, whereas no significant association was found with myeloperoxidase. A recent study aimed to investigate the preventive effect of exercise training on vascular endothelial dysfunction induced by fine PM [34]. Exercise training promoted HDL function, whereas exposure to PM2.5 (3 mg/kg on day 1, 3 and 5) did not significantly alter HDL function in Wistar rats. It is, however, important to note that the route of exposure was intratracheal installation and not inhalation as in the previously featured studies.
Discussion
The current literature on PM-exposure and HDL functionality suggest that fine and ultrafine PM may impair functional properties of HDL via oxidative pathways [27, 28, 30,31,32,33]. Accumulating evidence links particles to atherosclerosis, in particular those with a high amount of organic chemicals [3, 6, 31, 36]. The particles may directly or indirectly react with protein and lipid components of HDL resulting in a dysfunctional phenotype without atheroprotective features (Fig. 2). In some studies, PM exposure was found to be associated with reduced HDL-C levels as well as altered HDL functionality [28, 32]. However, other studies report alteration in HDL functional properties without affecting the quantitative levels [31, 33].
HDL functionality
A number of studies have found elevated PM exposure to be negatively correlated with the level of HDL-C [28, 32, 37,38,39,40,41,42,43]. However, the literature is somewhat inconsistent on this issue, as some studies find exposure to PM associated with an increase in HDL-C [44,45,46], while others find no statistical association [47,48,49,50]. Various studies have shown a significant increased incidence of atherosclerosis in individuals despite elevated levels of HDL-C [51]. Furthermore, HDL-C level raising therapies, as applied in multiple clinical trials, have failed to reduce CV events [52]. This may indicate that the HDL-C levels as such are not an obligatory link between PM and atherosclerosis.
Some have suggested that HDL particle number (HDL-P) may be a better indicator of the atheroprotective effect than HDL-C levels alone [53]. In a cross-sectional study, Bell et al. reported significant decreases in HDL particle number in relation to PM2.5 exposure [49]. They suggest that a reduction in smaller HDL particles supports the notion that changes in cholesterol efflux capacity might explain the link between air pollution and CVD, as the smaller particles accept cholesterol more efficiently than larger particles [54].
Other researchers have hypothesized that not all HDL is functionally similar. They suggest that the HDL functional properties might play a more significant role in atheroprotection than the cholesterol level itself [55]. HDL may render into a form characterized by impaired cholesterol efflux capacity. This dysfunctional form has reduced anti-inflammatory or even gained pro-inflammatory properties. Such changes have been seen in clinical conditions associated with inflammation and oxidative stress [51]. Accordingly, dysfunctional HDL has been found to be associated with increased incidence of CVD [51, 56]. For this reason, recent studies have placed focus on HDL function independent of cholesterol levels.
Mechanistic considerations
A number of in vitro and in vivo studies have proven that pro-inflammatory and oxidative stimuli can rapidly convert HDL to a dysfunctional form, whereby it loses its atheroprotective features. The changes in HDL function are transient and more easily detected in individuals with high antioxidative capacity [30]. During acute-phase response, proteins like serum amyloid A (SAA) and ceruloplasmin bind to HDL which might limit its ability to promote cholesterol efflux as well as the antioxidant capacity [57]. Systemic inflammation can also impede functional properties of HDL by changing the proteome and lipidome [25]. HDL components, such as apolipoproteins and enzymes, might be targets for oxidative modifications that stimulate atherosclerotic processes [6, 58]. Thus, it is tempting to speculate that PM may directly or indirectly have similar effects. Myeloperoxidase is found to be elevated with increased PM exposure [59,60,61]. As myeloperoxidase induces oxidative damage on biological molecules, one plausible pathway for PM’s adverse effects on HDL function may be through myeloperoxidase-induced oxidative modification [27]. Oxidation of apolipoprotein-AI (Apo-AI) by myeloperoxidase and other reactive intermediates, weakens its capacity to promote reverse cholesterol transport. Oxidized Apo-AI is unable to activate lecithin cholesterol acyltransferase (LCAT) which is important for increasing the cholesterol efflux capacity [17, 62]. However, reduced HDL functionality without a corresponding increase in myeloperoxidase activity has been reported [27].
In addition to the apolipoproteins, HDL-associated enzymes like paraoxonase, lecithin cholesterol acyltransferase and platelet activating factor acetyl hydrolase (PAF-AH) contribute to the antioxidative features of HDL [23]. Paraoxonase is important in the protection of LDL from oxidative damage, and its expression seems to be downregulated in the presence of oxidative stress [63]. Studies in both animal and human find an association between decreased paraoxonase activity and increased risk of developing atherosclerosis [64]. Accordingly, in LDLR−/− mice exposed to ultrafine particles, a decreased paraoxonase activity was associated with a larger atherosclerotic lesion size [32, 33]. However, other studies did not observe altered paraoxonase activity following exposure to PM [29, 30].
Exposure to PM has been associated with development of dysfunctional HDL in several studies [27, 28, 30,31,32,33]. Association was found for ultrafine and fine PM, and the effects of PM on HDL functionality seem to be associated with smaller particle size. This is further supported by the finding in one small study where coarse PM was not associated with impaired HDL functionality [29]. Ultrafine particles also seem to give larger early atherosclerotic lesions in mice than PM2.5. This may in part be due to a larger deposition in the lower airways, but the relative smaller size of ultrafine particles will also result in higher particle number and larger surface per mass [31, 65, 66]. Irrespectively, it is interesting to note that ultrafine particles not only produced more proatherogenic effects than PM2.5, but also resulted in a larger degree of HDL dysfunction. Thus, this finding supports the hypothesis of HDL dysfunction as a mechanistic link between PM exposure and atherosclerosis.
In addition to studies assessing the hazardous effects of PM on HDL, there is also a study evaluating the protective capacity of HDL against exposure to PM [67]. The results showed that unmodified HDL inhibited oxidative effects in bovine aortic endothelial cells and RAW264.7 macrophages exposed to diesel exhaust particles in vitro. In contrast, dysfunctional HDL failed to inhibit diesel exhaust particle-induced oxidation and oxidative cellular effects and instead, the exposure promoted further oxidation. These results strengthen the hypothesis that normal HDL protect against adverse effects of air pollution.
Susceptibility and co-exposures
There are genetically susceptible individuals with low antioxidative capacity in the blood which might represent a population with an increased risk of PM-related CVD. Some genetic disorders which alter critical enzymes, lipid transfer proteins or receptors crucial for the metabolism and function of HDL may impair the functional aspects of the lipoprotein [68]. The well-established risk factors for atherosclerosis - hypertension, dyslipidaemia and obesity – are all characterized by systemic inflammation and oxidative stress [69]. Such conditions might explain why HDL renders dysfunctional in patients with metabolic syndrome [70].
It is interesting to note that cigarette smoking has also been a suggested contributor to CVD via alterations in lipid profiles with impact on HDL [71]. Evidence suggests that smoking reduces HDL-C levels by altering critical enzymes of lipid transport. Smoking is reported to reduce the activity of lecithin cholesterol acyltransferase, which might impede maturation of HDL and lead to a rapid clearance of nascent HDL [56]. The anti-oxidative and anti-inflammatory capacity of HDL, as well as the cholesterol efflux capacity, have been found to be impaired by cigarette smoking [72]. It is well documented that smoking cessation reduces the risk of CVD. Interestingly, smoking cessation improves HDL functionality in coronary artery disease patients in the absence of changes in HDL-C levels, Apo-AI levels or HDL subfractions [72, 73]. Overall, smoking-induced reduction in HDL-C levels and in particular, HDL function seems to be important for atherosclerosis. It is tempting to hypothesize that a similar mechanism may also apply to PM in ambient air and that smokers may represent a particularly sensitive group.
Methodological considerations
Human exposure and epidemiological studies
Particulate matter air pollution as a risk factor for CVD is relatively modest compared to other well-established factors linked to personal lifestyle, including physical inactivity, unhealthy diet, smoking and excessive alcohol use [1]. Nonetheless, the ubiquitous nature and therefore the magnitude of populations affected, makes PM air pollution a serious threat to human health. Overall, the epidemiological and clinical data suggest a possible association between PM-exposure and dysfunctional HDL. The number of available studies is limited and focus only on the effects of short-term particle exposure. A major strength of the studies is, however, their strong research designs as randomized controlled trials and prospective follow-up studies. The inclusion of non-smoking populations limits confounding by tobacco smoke.
Animal studies
There are obvious genetic and environmental factors to take into consideration when extrapolating from animal studies to human. Most importantly, atherosclerosis is not as common in rodents as in humans. Even in the often-used atherosclerosis-prone ApoE−/− (knock-down) mouse model, plaques formed do not rupture [74]. Regarding air pollution particles, the horizontally-positioned respiratory system in rodents presents obvious problematic implications for particle deposition and removal. Thus, results from animal experiments are not directly comparable with the health effects observed in human studies. However, the impact of animal studies may be improved with the combined use of human in vitro studies on specific processes in cells considered to be central in atherosclerosis.
Conclusion
Epidemiological and clinical studies when combined with experimental animal and in vitro studies, support the notion that fine and ultrafine PM may promote HDL dysfunction via oxidative pathways. Combined, these studies suggest a causal pathway between air pollution, PM-induced dysfunctional HDL and atherosclerosis. Several mechanisms have been proposed, but the underlying biological pathways remain to be fully elucidated. One central theory suggests PM promotes atherosclerosis as a result of its systemic oxidative and inflammatory effects. This type of inflammatory milieu can affect plasma lipoproteins and may increase the atherogenic effect of LDL while reducing the atheroprotective effect of HDL. Recent studies have challenged the well-established idea that higher levels of HDL-C are always beneficial and lower levels of HDL-C are always detrimental. Ultimately, it has become clear that the functional properties of HDL are more important than the levels per se [75]. As shown in this review, there are studies suggesting that fine and ultrafine PM may promote HDL dysfunction via oxidative pathways. By affecting the protein and lipid components of HDL, cholesterol efflux capacity, as well as other anti-oxidative and anti-inflammatory features might be impaired.
Perspectives and future studies
As the current literature on PM exposure and HDL function is very limited, there is a need for more epidemiological as well as experimental studies to strengthen any possible causal relationship and determine any association to atherosclerosis as well as its possible underlying mechanisms. It would be interesting to explore whether short-time exposures can induce changes in HDL function or whether long-term exposures are essential. Studies so far have only been assessing the role of PM on HDL function in healthy populations. It is thus important to study genetically susceptible groups or other groups considered to have an increased risk of PM-related CVD like the elderly, individuals with metabolic syndrome, and those with diabetes [1]. Assessing HDL function in individuals with high exposure from ambient air or due to occupational settings (e.g. truck drivers or welders) might give additional insight. On the clinical side, one should examine how HDL functionality in CVD-patients is affected by PM exposure, and explore the efficacy of preventive measures like treatment with statins and antioxidants. Such studies may yield a better understanding of the PM-mediated pathogenesis and may lead to the identification of new biomarkers of PM-induced systemic effects, as well as a potential therapeutic target for treatment of atherosclerosis.
Availability of data and materials
Not applicable.
Abbreviations
- ABCA1:
-
ATP-binding cassette transporter A1
- ABCG1:
-
ATP-binding cassette transporter G1
- Apo:
-
Apolipoprotein
- CEC:
-
Cholesterol efflux capacity
- CETP:
-
Cholesterol ester transfer protein
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular disease
- DE:
-
Diesel exhaust
- FA:
-
Filtered air
- HDL:
-
High-density lipoprotein
- HDL-C:
-
High-density lipoprotein cholesterol
- HOI:
-
High-density lipoprotein oxidation index
- hs-CRP:
-
High-sensitivity C-reactive protein
- IL-1β:
-
Interleukin-1β
- IL-6:
-
Interleukin-6
- LCAT:
-
Lecithin-cholesterol acyltransferase
- LDL:
-
Low-density lipoprotein
- LDL-C:
-
Low-density lipoprotein cholesterol
- MPO:
-
Myeloperoxidase
- ox-HDL:
-
Oxidized high-density lipoprotein
- ox-LDL:
-
Oxidized low-density lipoprotein
- PAF-AH:
-
Platelet activating factor acetyl hydrolase
- PAH:
-
Polycyclic aromatic hydrocarbons
- PM:
-
Particulate matter
- PON:
-
Paraoxonase
- RCT:
-
Reverse cholesterol transport
- ROS:
-
Reactive oxygen species
- SAA:
-
Serum amyloid A
- TNF-α:
-
Tumor necrosis factor-α
- UFP:
-
Ultrafine particles
- VLDL:
-
Very-low-density lipoprotein
References
Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–78.
Franklin BA, Brook R, Arden Pope C 3rd. Air pollution and cardiovascular disease. Curr Probl Cardiol. 2015;40(5):207–38.
Pope CA 3rd, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc. 2006;56(6):709–42.
Jørgensen A, Møller, Loft. Luftforurening og hjerte-kar-sygdomme Københavns universitet, institut for folkesundhedsvidenskab 2017. Available from: https://hjerteforeningen.dk/wp-content/uploads/2018/01/rapport-luftforurening-og-hjerte-kar-sygdomme-19102017-final-version.pdf.
Moller P, Loft S. Oxidative damage to DNA and lipids as biomarkers of exposure to air pollution. Environ Health Perspect. 2010;118(8):1126–36.
Araujo JA, Nel AE. Particulate matter and atherosclerosis: role of particle size, composition and oxidative stress. Part Fibre Toxicol. 2009;6(1):24.
Gong KW, Zhao W, Li N, Barajas B, Kleinman M, Sioutas C, et al. Air-pollutant chemicals and oxidized lipids exhibit genome-wide synergistic effects on endothelial cells. Genome Biol. 2007;8(7):R149.
Li N, Alam J, Venkatesan MI, Eiguren-Fernandez A, Schmitz D, Di Stefano E, et al. Nrf2 is a key transcription factor that regulates antioxidant defense in macrophages and epithelial cells: protecting against the proinflammatory and oxidizing effects of diesel exhaust chemicals. J Immunol. 2004;173(5):3467–81.
Hiura TS, Kaszubowski MP, Li N, Nel AE. Chemicals in diesel exhaust particles generate reactive oxygen radicals and induce apoptosis in macrophages. J Immunol. 1999;163(10):5582–91.
Tsai DH, Amyai N, Marques-Vidal P, Wang JL, Riediker M, Mooser V, et al. Effects of particulate matter on inflammatory markers in the general adult population. Part Fibre Toxicol. 2012;9:24.
Holme JA, Brinchmann BC, Refsnes M, Lag M, Ovrevik J. Potential role of polycyclic aromatic hydrocarbons as mediators of cardiovascular effects from combustion particles. Environ Health. 2019;18(1):74.
Ovrevik J, Refsnes M, Lag M, Holme JA, Schwarze PE. Activation of Proinflammatory responses in cells of the airway mucosa by particulate matter: oxidant- and non-oxidant-mediated triggering mechanisms. Biomolecules. 2015;5(3):1399–440.
Bock KW. Human AHR functions in vascular tissue: Pro- and anti-inflammatory responses of AHR agonists in atherosclerosis. Biochem Pharmacol. 2019;159:116–20.
Xia T, Korge P, Weiss JN, Li N, Venkatesen MI, Sioutas C, et al. Quinones and aromatic chemical compounds in particulate matter induce mitochondrial dysfunction: implications for ultrafine particle toxicity. Environ Health Perspect. 2004;112(14):1347–58.
Ovrevik J, Refsnes M, Lag M, Brinchmann BC, Schwarze PE, Holme JA. Triggering mechanisms and inflammatory effects of combustion exhaust particles with implication for carcinogenesis. Basic Clin Pharmacol Toxicol. 2017;121(Suppl 3):55–62.
Stachyra K, Kiepura A, Olszanecki R. Air pollution and atherosclerosis - a brief review of mechanistic links between atherogenesis and biological actions of inorganic part of particulate matter. Folia Med Cracov. 2017;57(3):37–46.
Hopkins PN. Molecular biology of atherosclerosis. Physiol Rev. 2013;93(3):1317–542.
Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. Jama. 2005;293(15):1868–74.
Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356,222 primary screenees of the multiple risk factor intervention trial (MRFIT). Jama. 1986;256(20):2823–8.
Siddiqi HK, Kiss D, Rader D. HDL-cholesterol and cardiovascular disease: rethinking our approach. Curr Opin Cardiol. 2015;30(5):536–42.
Luscher TF, Landmesser U, von Eckardstein A, Fogelman AM. High-density lipoprotein: vascular protective effects, dysfunction, and potential as therapeutic target. Circ Res. 2014;114(1):171–82.
Navab M, Ananthramaiah GM, Reddy ST, Van Lenten BJ, Ansell BJ, Fonarow GC, et al. The oxidation hypothesis of atherogenesis: the role of oxidized phospholipids and HDL. J Lipid Res. 2004;45(6):993–1007.
Bandeali S, Farmer J. High-density lipoprotein and atherosclerosis: the role of antioxidant activity. Curr Atheroscler Rep. 2012;14(2):101–7.
Stocker R, Keaney JF Jr. Role of oxidative modifications in atherosclerosis. Physiol Rev. 2004;84(4):1381–478.
Karathanasis SK, Freeman LA, Gordon SM, Remaley AT. The changing face of HDL and the best way to measure it. Clin Chem. 2017;63(1):196–210.
Wolska A, Levine SJ, Remaley AT. Where there is smoke, there is fire. Arterioscler Thromb Vasc Biol. 2019;39(3):306–8.
Mathew AV, Yu J, Guo Y, Byun J, Chen YE, Wang L, et al. Effect of ambient fine particulate matter air pollution and colder outdoor temperatures on high-density lipoprotein function. Am J Cardiol. 2018;122(4):565–70.
Li J, Zhou C, Xu H, Brook RD, Liu S, Yi T, et al. Ambient air pollution is associated with HDL (high-density lipoprotein) dysfunction in healthy adults. Arterioscler Thromb Vasc Biol. 2019;39(3):513–22.
Maiseyeu A, Yang HY, Ramanathan G, Yin F, Bard RL, Morishita M, et al. No effect of acute exposure to coarse particulate matter air pollution in a rural location on high-density lipoprotein function. Inhal Toxicol. 2014;26(1):23–9.
Ramanathan G, Yin F, Speck M, Tseng CH, Brook JR, Silverman F, et al. Effects of urban fine particulate matter and ozone on HDL functionality. Part Fibre Toxicol. 2016;13(1):26.
Araujo JA, Barajas B, Kleinman M, Wang X, Bennett BJ, Gong KW, et al. Ambient particulate pollutants in the ultrafine range promote early atherosclerosis and systemic oxidative stress. Circ Res. 2008;102(5):589-96. https://doi.org/10.1161/CIRCRESAHA.
Li R, Navab M, Pakbin P, Ning Z, Navab K, Hough G, et al. Ambient ultrafine particles alter lipid metabolism and HDL anti-oxidant capacity in LDLR-null mice. Biochem Biophys Res Commun. 2013;54(6):1608–15.
Yin F, Lawal A, Ricks J, Fox JR, Larson T, Navab M, et al. Diesel exhaust induces systemic lipid peroxidation and development of dysfunctional pro-oxidant and pro-inflammatory high-density lipoprotein. Arterioscler Thromb Vasc Biol. 2013;33(6):1153–61.
Feng B, Qi R, Gao J, Wang T, Xu H, Zhao Q, et al. Exercise training prevented endothelium dysfunction from particulate matter instillation in Wistar rats. Sci Total Environ. 2019;694:133674.
Navab M, Hama SY, Hough GP, Subbanagounder G, Reddy ST, Fogelman AM. A cell-free assay for detecting HDL that is dysfunctional in preventing the formation of or inactivating oxidized phospholipids. J Lipid Res. 2001;42(8):1308–17.
Lee KK, Miller MR, Shah ASV. Air pollution and stroke. J Stroke. 2018;20(1):2–11.
Chuang KJ, Yan YH, Chiu SY, Cheng TJ. Long-term air pollution exposure and risk factors for cardiovascular diseases among the elderly in Taiwan. Occup Environ Med. 2011;68(1):64–8.
Rice MB, Cavallari J, Fang S, Christiani D. Acute decrease in HDL cholesterol associated with exposure to welding fumes. 2011;53(1):17–21.
Yitshak Sade M, Kloog I, Liberty IF, Schwartz J, Novack V. The association between air pollution exposure and glucose and lipids levels. J Clin Endocrinol Metab. 2016;101(6):2460–7.
Wu XM, Broadwin R, Basu R, Malig B, Ebisu K, Gold EB, et al. Associations between fine particulate matter and changes in lipids/lipoproteins among midlife women. Sci Total Environ. 2019;654:1179–86.
Tan C, Wang Y, Lin M, Wang Z, He L, Li Z, et al. Long-term high air pollution exposure induced metabolic adaptations in traffic policemen. Environ Toxicol Pharmacol. 2018;58:156–62.
Lee S, Park H, Kim S, Lee EK, Lee J, Hong YS, et al. Fine particulate matter and incidence of metabolic syndrome in non-CVD patients: a nationwide population-based cohort study. Int J Hyg Environ Health. 2019;222(3):533–40.
Yang BY, Bloom MS, Markevych I, Qian ZM, Vaughn MG, Cummings-Vaughn LA, et al. Exposure to ambient air pollution and blood lipids in adults: the 33 communities Chinese health study. Environ Int. 2018;119:485–92.
Tomao E, Tiziana PB, Rosati V, Marcellini L, Tomei F. The effects of air pollution on the lipid balance of traffic police personnel. Ann Saudi Med. 2002;22(5–6):287–90.
O'Toole TE, Hellmann J, Wheat L, Haberzettl P, Lee J, Conklin DJ, et al. Episodic exposure to fine particulate air pollution decreases circulating levels of endothelial progenitor cells. Circ Res. 2010;107(2):200–3.
McGuinn LA, Schneider A, McGarrah RW, Ward-Caviness C, Neas LM, Di Q, et al. Association of long-term PM2.5 exposure with traditional and novel lipid measures related to cardiovascular disease risk. Environ Int. 2019;122:193–200.
Chuang KJ, Yan YH, Cheng TJ. Effect of air pollution on blood pressure, blood lipids, and blood sugar: a population-based approach. J Occup Environ Med. 2010;52(3):258–62.
Shanley RP, Hayes RB, Cromar KR, Ito K, Gordon T, Ahn J. “Particulate Air Pollution and Clinical Cardiovascular Disease Risk Factors”. 2015:1.
Bell G, Mora S, Greenland P, Tsai M, Gill E, Kaufman JD. Association of air Pollution Exposures with High-Density Lipoprotein Cholesterol and Particle Number. Arterioscler Thromb Vasc Biol. 2017;37(5):976–82.
Jiang S, Bo L, Gong C, Du X, Kan H, Xie Y, et al. Traffic-related air pollution is associated with cardio-metabolic biomarkers in general residents. Int Arch Occup Environ Health. 2016;89(6):911–21.
Ragbir S, Farmer JA. Dysfunctional high-density lipoprotein and atherosclerosis. Curr Atheroscler Rep. 2010;12(5):343–8.
Wright RS. Recent clinical trials evaluating benefit of drug therapy for modification of HDL cholesterol. Curr Opin Cardiol. 2013;28(4):389–98.
Mora S, Glynn RJ, Ridker PM. High-density lipoprotein cholesterol, size, particle number, and residual vascular risk after potent statin therapy. Circulation. 2013;128(11):1189–97.
Du XM, Kim MJ, Hou L, Le Goff W, Chapman MJ, Van Eck M, et al. HDL particle size is a critical determinant of ABCA1-mediated macrophage cellular cholesterol export. Circ Res. 2015;116(7):1133–42.
Kaufman JD, Adar SD, Barr RG, Budoff M, Burke GL, Curl CL, et al. Association between air pollution and coronary artery calcification within six metropolitan areas in the USA (the multi-ethnic study of atherosclerosis and air pollution): a longitudinal cohort study. Lancet. 2016;388(10045):696–704.
Rosenson RS, Brewer HB Jr, Ansell BJ, Barter P, Chapman MJ, Heinecke JW, et al. Dysfunctional HDL and atherosclerotic cardiovascular disease. Nat Rev Cardiol. 2016;13(1):48–60.
Van Lenten BJ, Navab M, Shih D, Fogelman AM, Lusis AJ. The role of high-density lipoproteins in oxidation and inflammation. Trends Cardiovasc Med. 2001;11(3–4):155–61.
Gur M, Aslan M, Yildiz A, Demirbag R, Yilmaz R, Selek S, et al. Paraoxonase and arylesterase activities in coronary artery disease. Eur J Clin Investig. 2006;36(11):779–87.
Ruckerl R, Hampel R, Breitner S, Cyrys J, Kraus U, Carter J, et al. Associations between ambient air pollution and blood markers of inflammation and coagulation/fibrinolysis in susceptible populations. Environ Int. 2014;70:32–49.
Li W, Wilker EH, Dorans KS, Rice MB, Schwartz J, Coull BA, et al. Short-term exposure to air pollution and biomarkers of oxidative stress: the framingham heart study. J Am Heart Assoc. 2016;5(5).
Newby DE, Mannucci PM, Tell GS, Baccarelli AA, Brook RD, Donaldson K, et al. Expert position paper on air pollution and cardiovascular disease. Eur Heart J. 2015;36(2):83–93b.
Shao B, Oda MN, Oram JF, Heinecke JW. Myeloperoxidase: an oxidative pathway for generating dysfunctional high-density lipoprotein. Chem Res Toxicol. 2010;23(3):447–54.
Aviram M, Rosenblat M, Billecke S, Erogul J, Sorenson R, Bisgaier CL, et al. Human serum paraoxonase (PON 1) is inactivated by oxidized low density lipoprotein and preserved by antioxidants. Free Radic Biol Med. 1999;26(7–8):892–904.
Soran H, Younis NN, Charlton-Menys V, Durrington P. Variation in paraoxonase-1 activity and atherosclerosis. Curr Opin Lipidol. 2009;20(4):265–74.
Chalupa DC, Morrow PE, Oberdörster G, Utell MJ, Frampton MW. Ultrafine particle deposition in subjects with asthma. Environ Health Perspect. 2004;112(8):879–82.
Oberdorster G, Gelein RM, Ferin J, Weiss B. Association of particulate air pollution and acute mortality: involvement of ultrafine particles? Inhal Toxicol. 1995;7(1):111–24.
Yin F, Ramanathan G, Zhang M, Araujo JA. Prooxidative effects of ambient pollutant chemicals are inhibited by HDL. J Biochem Mol Toxicol. 2013;27(2):172–83.
Kosmas CE, Silverio D, Sourlas A, Garcia F, Montan PD, Guzman E. Primary genetic disorders affecting high density lipoprotein (HDL). Drugs Context. 2018;7:212546.
Stern MP. Diabetes and cardiovascular disease. The "common soil" hypothesis. Diabetes. 1995;44(4):369–74.
Khan AAMP, Straznicky NE, Nestel PJ, Wong G, Tan R, Huynh K, Ng TW, Mellett NA, Weir JM, Barlow CK, Alshehry ZH, Lambert GW, Kingwell BA, Meikle PJ. Weight loss and exercise Alter the high-density lipoprotein Lipidome and improve high-density lipoprotein functionality in metabolic syndrome: Arteriosclerosis, Thrombosis, and Vascular Biology; 2018.
Toh R. Assessment of HDL cholesterol removal capacity: toward clinical application. J Atheroscler Thromb. 2019;26(2):111–20.
Chen HY, Li SC, Chen LF, Wang W, Wang Y, Yan XW. The effects of cigarette smoking and smoking cessation on high-density lipoprotein functions: implications for coronary artery disease. Ann Clin Biochem. 2019;56(1):100–11. https://doi.org/10.1177/0004563218788386.
Takata K, Imaizumi S, Kawachi E, Suematsu Y, Shimizu T, Abe S, et al. Impact of cigarette smoking cessation on high-density lipoprotein functionality. Circ J. 2014;78(12):2955–62.
Lo Sasso G, Schlage WK, Boue S, Veljkovic E, Peitsch MC, Hoeng J. The Apoe(−/−) mouse model: a suitable model to study cardiovascular and respiratory diseases in the context of cigarette smoke exposure and harm reduction. J Transl Med. 2016;14(1):146.
Harada A, Toh R, Murakami K, Kiriyama M, Yoshikawa K, Miwa K, et al. Cholesterol uptake capacity: a new measure of HDL functionality for coronary risk assessment. J Appl Lab Med. 2019;2(2):186–200.
Acknowledgements
Not applicable.
Funding
GJH received financial support from NordForsk under the Nordic Programme on Health and Welfare. Project #75007: Understanding the link between air pollution and distribution of related health impacts and welfare in the Nordic countries (NordicWelfAir). Moreover, the work of GJH was funded by BERTHA - the Danish Big Data Centre for Environment and Health funded by the Novo Nordisk Foundation Challenge Programme (grant NNF17OC0027864).
Author information
Authors and Affiliations
Contributions
SANH performed the literature search and interpreted the information.
SANH drafted the first version of the manuscript under supervision of JAH and wrote the final version in collaboration with TS, JAH and GJH. All authors read, commented, and approved the final manuscript.
Authors’ information
Siri A. N. Holme is a student enrolled in the master’s degree program in Medicine at Aarhus University. She has a special interest in environmental and preventive medicine and wrote her Bachelor thesis on effects of air pollution particles on HDL functionality.
Torben Sigsgaard MD, PhD, FERS, is professor of Occupational and Environmental Medicine at Dept. of public Health, Aarhus University, since 2004. His main research is within the field of gene-environment interaction and the impact on respiratory health and aging. The studies range from toxicological investigations with human exposures under controlled environmental conditions via cohort studies to registry-based studies on the entire Danish population.
Jørn A. Holme DSc, PhD is chief scientist at Department of Environmental Health, Norwegian Institute of Public Health. His main research has been in the field of mechanistic toxicology; with the aim of improving risk evaluations, understanding individual susceptibility and/or elucidating roles of molecular biomarkers. During the last 20 years his primary focus has been on malignant and non-malignant diseases induced by air pollution particles, with a special interest in cardiovascular disease.
Gitte Juel Holst is a post-doctoral scholar at Aarhus University at Department of Public Health. She received a master’s degree in Health Science and completed her PhD degree from Aarhus University. She is interested in how the environment influences human health with emphasis on air quality and health and has worked with methods ranging from human experimental studies, various types of epidemiological designs and real-life intervention studies.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Holme, S.A.N., Sigsgaard, T., Holme, J.A. et al. Effects of particulate matter on atherosclerosis: a link via high-density lipoprotein (HDL) functionality?. Part Fibre Toxicol 17, 36 (2020). https://doi.org/10.1186/s12989-020-00367-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12989-020-00367-x