Abstract
Background
Whether and to what extent serum uric acid (SUA) mediates the association between combined lifestyle behaviors and type 2 diabetes mellitus (T2DM) remain unclear. This study aimed to investigate the role of SUA in the relationship between healthy lifestyle scores (HLS) and the incidence of T2DM.
Methods
This prospective study used data from Zhejiang Metabolic Syndrome cohort. A HLS (5-point scale including healthy waist circumference (WC), never smoking, high physical activity, healthy diet and moderate alcohol intake) was estimated in 13,919 participants, who had SUA at baseline examination in 2009–2014, and were followed-up to 2021–2022 to ascertain incident of T2DM. Cox proportional hazards models and mediation analysis were used to examine the associations between HLS, SUA and T2DM.
Results
We included 13,919 participants aged 18 years or older without diabetes at baseline (mean age 54.6 [SD 13.9] years, 58.7% female). During a median follow-up of 9.94 years, 645 cases of T2DM occurred. Compared with participants with a poor HLS, those with 4–5 low-risk lifestyle factors showed a 60% reduction in the risk of developing T2DM (adjusted HR, 0.40; 95% CI: 0.28–0.57). Further, the population-attributable risk percent (95% CI) of T2DM for poor adherence to the overall healthy lifestyle (< 4 low-risk factors) was 43.24% (30.02%, 56.46%). The HLS was inversely associated with SUA level. With per score increased in HLS, the beta (95% CI) of SUA (log transformed) was − 0.03 (− 0.03, − 0.02), and the odds ratio (95% CI) of hyperuricemia was 0.82 (0.77, 0.86). The relationship between the HLS and risk of T2DM was mediated by SUA with a 13.06% mediation effect. There was no significant combined effect of HLS and SUA on risk of T2DM (P = 0.097).
Conclusions
The relationship between overall healthy lifestyle behaviors and T2DM was reconfirmed and the association appeared to be mediated by SUA. The mediation effect of baseline SUA was more pronounced among women who were below 60 years old.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus is one of the common metabolic diseases in the world. Approximately 536.6 million people worldwide in 2021 are affected by T2DM, and the number is projected to increase to 783.2 million by 2045 [1]. Given the increased health burden related to morbidity and mortality, T2DM has now become a major global health challenge.
It is well documented that lifestyle risk factors such as poor diet, physical inactivity, obesity, smoking, and excessive alcohol drinking cause adverse effects on health outcomes [2,3,4]. Previous studies have established a healthy lifestyle score to investigate the associations between combined lifestyle factors and health outcomes. Adherence to multiple healthy lifestyle habits has been associated with lower risk of T2DM [5,6,7], a long-life expectancy free of major chronic diseases [8], and lower risk for mortality [9, 10].
The inverse association of HLS with incident T2DM, is substantially explained by differences in lifestyle-related plasma metabolites measured years before the T2DM clinical diagnosis [7]. SUA is the final product of purine metabolism, and elevated SUA is associated with increased fasting plasma glucose (FPG) in patients with prediabetes [11] and increase risk of new-onset impaired fasting glucose (IFG) and diabetes mellitus [12]. Simultaneously, considerable evidence suggests that people who adhere to a healthy lifestyle, such as high physical activity, no smoking, and healthy dietary pattern, have apparently reduced risk of hyperuricemia [13,14,15].
However, to our best knowledge, the study to explore the association of joint lifestyle factors with SUA levels is limited. Whether and to what extent SUA mediates the association between combined lifestyle behaviors and T2DM remain unclear. Hence, this study examined the association between combined lifestyle factors, including smoking status, alcohol consumption, diet behavior, physical activity and WC, and risk of T2DM. In addition, we also evaluated the potential mediation effect of SUA in the association between overall lifestyle factors and risk of T2DM.
Materials and methods
Study population
The subjects in this study were recruited from the Zhejiang Metabolic Syndrome cohort, a community-based prospective cohort study conducted in Zhejiang province located in Southeast China between 2009 and 2014. Details of the cohort are described elsewhere [16]. The participants were recruited from three counties of Zhejiang, and were followed up until 1 February 2021 and 30 June 2022, respectively.
The participants who were included into the study were aged ≥ 18 years. The exclusion criteria of the subjects for this analysis were as follows [1]: diagnosed with T2DM at baseline; [2] presence of severe chronic diseases at baseline such as cancer, coronary heart disease (CHD), stroke; [3] missing value of lifestyle factors or age; [4] lost to follow-up. Finally, a total of 13,919 participants were included in this study. The detailed participant selection process is shown in Additional file 1: Fig. S1.
Data collection and assessment
Each participant underwent a face-to-face questionnaire-based interview, clinical health examination, and routine biochemical determination at baseline and first follow-up, as previously reported [16].
Demographic data were collected using a standard structured questionnaire. Variables included age, sex, smoking and alcohol consumption behavior, physical activity, history of T2DM and hypertension, and family history of T2DM, hypertension, CHD, and stroke. Smoking behavior was grouped as current, former, and never. Current smoking was defined as smoking at least one cigarette per day and lasting for more than half a year. Former smoking was defined as stopping smoking for at least half a year [17]. Alcohol drinking was classified into three categories as never, moderate (< 3 times/week) and heavy drinking (≥ 3 times/week) according to frequency on average in the past 12 months. International Physical Activity Questionnaire (IPAQ) was used for the assessment of the average amount of time per week engaged in exercise activities [18]. The energy expended for each activity in metabolic equivalent (MET) hours per week (MET-h/week) was calculated according to the instruction. We defined high physical activity level as the highest sex-specific quartile. Trained interviewers inquired about dietary intake using the semi-quantitative food frequency questionnaire (FFQ). Participants were asked the frequency and consumption of several food on average during the previous year. Each food intake was calculated by the product of the frequency of intake and the amount consumed at each frequency unit. The red meat intake contained pork, beef, and lamb.
Anthropometric data, including weight, height, and waist circumference (WC), were measured by well-trained investigators following a standard protocol. Height and weight were measured using a scale, with the subjects wearing light clothing and without shoes. WC was measured at the midpoint between the iliac crest and lowest rib. Blood pressure was measured in the sitting position with a mercury sphygmomanometer. Systolic blood pressure (SBP) and diastolic blood pressure (DBP)were recorded as the average of three repeated measurements with 30-s intervals. Hypertension was defined as SBP ≥ 140 mmHg or DBP ≥ 90 mmHg or diagnosis with hypertension by their doctors or current use of antihypertensive medication according to the National High Blood Pressure Education Program [19].
Biochemical data were collected from each subject after a 12-h overnight fast. Biochemical variables, including SUA, triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C), were determined using biochemical auto-analyzer (Hitachi 7060, Tokyo, Japan). Fasting plasma glucose (FPG) was analyzed by the glucose oxidase method with a Beckman Glucose Analyzer (Beckman Instruments, Irvine, CA, USA).
Determination of healthy lifestyle scores (HLS)
Five lifestyle factors were included in this study based on previous studies and Dietary Guidelines for Chinese Residents: smoking, alcohol intake, physical activity, dietary habits, and body composition [20, 21]. In our study, never smoking was defined low-risk, compared with current or past smoking. Never and moderate drinking was defined as low-risk for alcohol intake. Based on the calculated MET-h/week, high physical activity level, defined as highest sex-specific quartile, was considered low-risk. For dietary habits, we generated a dietary score ranging from 0 to 3 based on three components: fruits, vegetables and red meat. Healthy dietary habit was considered low-risk and was defined as meeting at least two ideal diet components, classified as the highest quartile consumption of fruits and vegetables and the lowest quartile consumption of red meat. For body composition, low-risk WC was defined as < 90 cm for male and < 85 cm for female, which was indicator for abdominal obesity [22]. Finally, we constructed the overall HLS by summing the numbers of present low-risk lifestyle behaviors in each participant. The score ranged from 0 to 5, with higher score indicating healthier lifestyle.
Definition of T2DM and hyperuricemia
The incidence of T2DM was identified through the local chronic disease surveillance system. According to the criteria of the American Diabetes Association [23], participants were considered to have T2DM when meeting at least one of the following criteria: (1) FPG ≥ 7.0 mmol/L (126 mg/dL); (2) self-reported T2DM diagnosed by a physician; or (3) currently taking antidiabetic medication. Hyperuricemia at baseline was SUA ≥ 420 µmol/L in males and SUA ≥ 360 µmol/L in females [24].
Statistical analyses
Participants were divided into four groups according to HLS (0–1, 2, 3, 4–5) to ensure statistical power. Continuous variables with normal distribution were described as means and standard deviations (SD), while continuous variables with skewed distribution were presented as median (interquartile range). Categorical variables were described as number (percentages). Comparisons of the characteristics among the four HLS groups were performed using one-way ANOVA for continuous variables, and chi-square test or Fisher exact test for categorical variables. Person-years of follow-up were calculated from the date at baseline to the first occurrence of T2DM, mortality, or the end of the study, whichever came first. Incidence of T2DM was calculated as the number of incident cases divided by the total person-years of follow-up.
Multiple Cox regression model was used to calculate the hazard ratio (HR) and its confidence interval (95% CI) to examine the association between HLS and the risk of T2DM in the following two ways: (1) as a categorical variable (0–1, 2, 3, 4–5 points), with the lowest HLS group as reference group; (2) as a continuous variable (per point increase). The proportional hazard assumption was tested using the Schoenfeld residual, and the results showed no violation on the assumptions. To adjust for the potential confounding bias and to examine the consistency of the results, we constructed two sets of models: Model 1 adjusted for age, sex, family history of T2DM, family history of hypertension, prevalence of hypertension, use of antihypertensive medication, and use of lipid-lowing medication; Model 2 additionally adjusted for TG, HDL-C, FPG. Further,. We used restricted cubic splines with four knots at the 5th, 35th, 65th, and 95th centiles to flexibly model the dose–response relationships of HLS with T2DM with a smoothly joined piecewise polynomial, and test for potential non-linearity by using a likelihood ratio [25]. We also calculated the population-attributable risk percent (PAR%) to estimate the proportion of T2DM that could theoretically be avoided if all participants had adhered to four or more low-risk lifestyle behaviors [26].
Once the temporal relationships of HLS with T2DM was established, we performed a series of analyses to examine whether the association between HLS (X) and T2DM (Y) were mediated by baseline SUA levels or hyperuricemia (M): (1) the association between HLS (X) and baseline SUA levels (continuous, nature log transformed) and hyperuricemia (M) was examined using linear regression model or logistic regression model, with all the covariates adjusted; (2) the associations between baseline SUA levels or hyperuricemia (M) and T2DM (Y) were examined by three sets of Cox proportional hazard models with all the covariates adjusted: (a) SUA level as a categorical variable based on sex-specific quartiles (cut-points were 312, 363 and 423 µmol/L in males, and 231, 271 and 317 µmol/L in females), with the lowest quartile group as reference group; (b) SUA level as a continuous variable (per SD increase); and (c) hyperuricemia as a dichotomous variable; (3) the mediation effect of baseline SUA levels or hyperuricemia (M) in the association between HLS (X) and T2DM (Y) was examined by causal mediation analysis using the model-based approach [27, 28], adjusted for age, sex, family history of hypertension, use of antihypertensive medication, and use of lipid-lowing medication, which were sufficient to control for exposure-outcome, mediator-outcome, and exposure-mediator confounding [29, 30]. A bootstrap analysis with 1,000 replications was applied to compute the CIs of the proportions of mediations. The linear trend test for HLS was performed by treating the number of low-risk factors as a continuous variable; for SUA by assigning the sex-specific median to each category and then modeling this as a continuous variable in the model. To evaluate whether there was a combined effect of HLS and SUA on T2DM, we further stratified the analyses by hyperuricemia status and HLS. The interaction effect between HLS and SUA was assessed by including interaction terms in the multivariable model and tested with the likelihood ratio test.
Subgroup analyses were conducted by stratification according to sex (male or female) and age (< 60 or ≥ 60 years). To test the robustness of our results, we performed mediation analysis that additionally adjusted for baseline FPG. In addition, we generated the new HLS without low-risk drinking behavior, due to lack of amount of consumption which may involve inaccurate classification, and reevaluated the association of HLS and T2DM.
All of the statistical analyses were performed using R software version 4.0.3. All P values were two-sided, and P < 0.05 was defined as statistically significant. The borderline significance was defined as the P > 0.05, but < 0.10 (0.05 ≤ P < 0.10).
Results
Baseline characteristics
Baseline characteristics of the study sample according to HLS are summarized in Table 1. Overall, the mean age was 54.6 years (SD 13.9) and 58.7% of the sample were females. Moreover, 2775 (19.9%) individuals had an ideal HLS (4–5 points), and 1248 (9.0%) individuals had a poor HLS (0–1 points). Participants with lower HLS were more likely to be older, with higher levels of SPB, DPB, SUA, FPG, TG, and with lower levels of HDL-C.
Associations between HLS and T2DM risk
During a total of 134,076 person-years (median follow-up period 9.94 years), 645 participants (230 male, 415 female) were diagnosed with T2DM. The association between individual lifestyle factors and the risk of T2DM after adjusting for other lifestyles is shown in Additional file 1: Table S1. WC less than 90 cm in male or less than 85 cm in female, and ≥ 2 ideal components of dietary score, were individually associated with a lower risk of incident T2DM. When healthy lifestyle behaviors were considered jointly, a dose–response relationship of the HLS with risk of T2DM was observed (Table 2, Additional file 1: Fig. S2).
The risk of T2DM decreased dramatically with increasing number of the healthy lifestyle behaviors (P for trend < 0.001). After adjusted for age, sex, family history of diabetes and hypertension, prevalence of hypertension, use of antihypertensive and lipid-lowing medication, compared with participants with a one or less low-risk lifestyle factors, those with 3 factors had 39% lower risk of incident T2DM (HR, 0.61; 95% CI 0.47–0.81), and those with 4–5 factors showed a 64% reduction in the risk of developing T2DM (HR, 0.36; 95% CI 0.26–0.51). Moreover, when treating HLS as a continuous variable, T2DM risk decreased by 26% with per point increase in HLS (HR, 0.74; 95% CI 0.67–0.81). Additional adjustment for TG, HDL-C, and FPG, at baseline did not materially alter the association (for 3 factors: HR, 0.73; 95% CI 0.55–0.96; for 4–5 factors: HR, 0.40; 95% CI 0.28–0.57). The PAR% of nonadherence to four or more low-risk lifestyle factors was 43.24% (95% CI 30.02–56.46%). In addition, the estimated PAR% was 25.40% (95% CI 7.04%, 43.77%) for dietary score and 18.54% (95% CI 12.94%, 24.14%) for WC. The consistent association was still observed after excluding the alcohol drinking factor (per score increase adjusted HR, 0.70; 95% CI 0.63–0.77) (Additional file 1: Table S2).
Associations between baseline SUA level and T2DM risk
The population was classified into four groups (Q1-Q4) according to quartiles of baseline SUA levels: 74-, 312-, 363-, 423–768 µmol/L for male, and 74-, 231-, 271-, 317–859 µmol/L for female. The results of Cox proportional hazard model were shown in Table 3.
Compared with participants at the lowest quartile of SUA, those at the highest quartiles had a 35% (95% CI 1.07–1.70) higher risk of T2DM, after adjusted for all covariates mentioned above. Per SD increasement in SUA was associated with a 18% higher risk of T2DM (95% CI 1.08–1.29). There was also a statistically significant association between hyperuricemia and T2DM risk. Compared with participants without hyperuricemia, those with hyperuricemia had a 43% higher risk of T2DM (95% CI 1.19–1.72).
Associations between HLS and SUA
The results of regression models for the association between baseline SUA and HLS (Table 4) showed that participants with healthier healthy lifestyles had significantly lower SUA levels.
Compared with participants with 0 to 1 low-risk lifestyle behavior, HLS was negatively associated with SUA levels (per point increase in HLS: β = − 0.03, p < 0.001) and with hyperuricemia (per point increase in HLS: OR = 0.82, p < 0.001), after adjusted for age, sex, family history of diabetes and hypertension, prevalence of hypertension, use of antihypertensive or lipid-lowing medication, TG, HDL-C and FPG.
Mediation effect of SUA in the association of HLS with T2DM risk
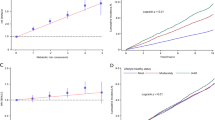
There was no significant combined effect of HLS and SUA on risk of T2DM (P = 0.097, Additional file 1: Fig. S3). The mediation analysis (Table 5, Fig. 1) showed that the association of HLS with risk of T2DM was partially mediated by baseline SUA levels (indirect effect: β = − 0.002, p < 0.001, proportion of mediation = 14.28%) after adjusted for age, sex, family history of hypertension, use of anti-hypertensive medication and use of lipid-lowing medication. Similar mediation effect was for hyperuricemia (indirect effect: β = − 0.003, p < 0.001, proportion of mediation = 15.71%).
Mediation effect of (A) baseline SUA, (B) baseline hyperuricemia on the association of healthy lifestyle scores and T2DM. *represent coefficients different from 0, P < 0.001. †The levels of SUA were nature log-transformed. @Hyperuricemia was defined as SUA ≥ 420 µmol/L for men and SUA ≥ 360 µmol/L for women
After adjusting for FPG, the proportion of mediation was reduced, indicating that FPG might play a role between SUA and T2DM (Fig. 2, Additional file 1: Table S3). The analysis after stratified by sex and age found that the mediation effect of SUA between HLS and risk of T2DM was more pronounced among females and individuals aged below 60 years (Fig. 2, Additional file 1: Table S4, Additional file 1: Table S5).
Mediation effect of baseline SUA or hyperuricemia on the association of HLS and T2DM: (A) additionally adjustment for FPG or not, (B) stratified by sex, (C) stratified by age(years), respectively. The levels of SUA were nature log-transformed. Hyperuricemia was defined as SUA ≥ 420 µmol/L for men and SUA ≥ 360 µmol/L for women. HLS, healthy lifestyle scores; T2DM, type 2 diabetes mellitus; SUA, serum uric acid
Discussion
In this population-based cohort study with 9.94-year follow-up, the HLS, a composite healthy lifestyle measure of smoking, alcohol consumption, physical activity, diet, and body composition, was inversely associated with the risk of T2DM, and such association was partially mediated by the level of SUA at baseline. For adoption of each additional low-risk lifestyle behavior, the risk of T2DM decreases by 23%, and 43% of T2DM could have been avoided if the population possess 4–5 healthy lifestyle behaviors. Individuals with more healthy lifestyle behaviors are more likely to have lower level of SUA, which partially contributes to the lower risk of T2DM.
There has been preponderant evidence on the impact of individual lifestyle behaviors. For example, there is evidence that SUA is linked to dietary factors [31, 32], and adiposity and alcohol consumption are associated with a higher SUA [33]. Mean change in BMI, but not in WC, was statistically significantly associated with change in SUA over a 1-year follow-up in males [34]. For smoking, consensus has yet to be reached regarding its effect on serum urate levels [35, 36]. To date, few studies have attempted to examine the association between combined healthy lifestyle and SUA. Our study provided novel evidence that the SUA level decreases with increase in healthy lifestyle behaviors. Lifestyle interventions can reshape the gut microbiota [37]. Faecalibacterium [38] and Clostridium [39], as an intestinal microbial preparation, can produce butyric acid by fermenting dietary fiber in the intestine. Intestinal butyric acid amounts were related to uric acid metabolism in humans [40]. Escherichia-Shigella could secrete xanthine deaminase, which can convert hypoxanthine and xanthine into uric acid [41].
Our mediation analyses revealed that uric acid in plasma may be a potential pathway of mechanism in the inverse association between combined lifestyle behavior and risk of T2DM. Previous studies have revealed the mediation effect of SUA [42], and obesity [43] in the association between individual lifestyle factors and risk of T2DM. There is also evidence on the role of plasma metabolites in explaining the association of overall lifestyle and incident T2DM [7]. The strong association between HLS with metabolites profiles reflected several metabolic pathways. And most of the identified HLS-related metabolites were also prospectively associated to T2DM [7]. The mediation mechanism of SUA between HLS and risk of T2DM could be associated with gut microbiota [40, 44]. Moreover, the mediation effect of SUA in inverse association between HLS and risk of T2DM was greater among females and those aged below 60. It’s because gut microbiota could affect material metabolism in sex and age differences [45,46,47]. According to our study, women who were below 60 years old should pay more attention to healthy lifestyle behavior to stable their SUA levels so that the prevention of T2DM.
The major strengths of this study are the prospective cohort study design and long follow-up period. To the best of our knowledge, this is the first study to investigate the mediating role of SUA in the relationship between combined healthy lifestyle and diabetes. There are also several limitations to our study. First, this study cannot establish causal relationship between HLS and SUA due to their data both from baseline. Future studies with repeatedly measured data are required to replicate our findings. Second, the information on lifestyle factors, except for WC, was self-reported, which may introduce information bias. However, the standard structured questionnaire and well-trained investigators increased the accuracy and reliability of the data. Third, although this simple additive method to develop HLS has been widely used, the underlying assumption is that the associations between different lifestyle factors and outcomes are the same, which may not be true. It’s necessary to generate a weighted HLS and examined the associations in a larger representative population. In addition, low-risk alcohol consumption was classified based on frequency rather than amount of consumption, which may involve misclassification. However, the inverse association between HLS and T2DM was still observed after excluding the alcohol drinking factor. Finally, we did not adjust for socioeconomic status in the analysis, which may raise concerns of unmeasured confounding. Several residual confounding could not be excluded due to the observational study design. Clinical trials and gut microbiota are definitely needed to verify the role of SUA in the association of lifestyle and T2DM.
Conclusions
Our findings suggest that adherence to overall healthy lifestyle behaviors was associated with a lower risk of T2DM and support the importance of programs and interventions targeting at promoting health behaviors to reduce the risk of T2DM. In addition, our data showed significant partial mediation effect of SUA in the associations between lifestyle behaviors and T2DM. Further studies are warranted to confirm our findings.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SUA:
-
Serum uric acid
- T2DM:
-
Type 2 diabetes mellitus
- HLS:
-
Healthy lifestyle scores
- WC:
-
Waist circumference
- FPG:
-
Fasting plasma glucose
- IFG:
-
Impaired fasting glucose
- CHD:
-
Coronary heart disease
- IPAQ:
-
International Physical Activity Questionnaire
- FFQ:
-
Food frequency questionnaire
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- BMI:
-
Body mass index
- TG:
-
Triglycerides
- TC:
-
Total cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- SD:
-
Standard deviations
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- PAR%:
-
Population-attributable risk percent
References
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119.
Jones P, Karim Sulaiman S, Gamage KN, Tokas T, Jamnadass E, Somani BK. Do lifestyle factors including smoking, alcohol, and exercise impact your risk of developing kidney stone disease? Outcomes of a systematic review. J Endourol. 2021;35(1):1–7.
McMaster M, Kim S, Clare L, Torres SJ, Cherbuin N, D’Este C, et al. lifestyle risk factors and cognitive outcomes from the multidomain dementia risk reduction randomized controlled trial, body brain life for cognitive decline (BBL-CD). J Am Geriatr Soc. 2020;68(11):2629–37.
van Namen M, Prendergast L, Peiris C. Supervised lifestyle intervention for people with metabolic syndrome improves outcomes and reduces individual risk factors of metabolic syndrome: a systematic review and meta-analysis. Metabolism. 2019;101:153988.
Patel YR, Gadiraju TV, Gaziano JM, Djousse L. Adherence to healthy lifestyle factors and risk of death in men with diabetes mellitus: the physicians’ health study. Clin Nutr. 2018;37(1):139–43.
Khan TA, Field D, Chen V, Ahmad S, Mejia SB, Kahleova H, et al. Combination of multiple low-risk lifestyle behaviors and incident type 2 diabetes: a systematic review and dose-response meta-analysis of prospective cohort studies. Diabetes Care. 2023;46(3):643–56.
Delgado-Velandia M, Gonzalez-Marrachelli V, Domingo-Relloso A, Galvez-Fernandez M, Grau-Perez M, Olmedo P, et al. Healthy lifestyle, metabolomics and incident type 2 diabetes in a population-based cohort from Spain. Int J Behav Nutr Phys Act. 2022;19(1):8.
Li Y, Schoufour J, Wang DD, Dhana K, Pan A, Liu X, et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ. 2020;368:l6669.
Shi Z, Zhang T, Byles J, Martin S, Avery JC, Taylor AW. Food habits, lifestyle factors and mortality among oldest old Chinese: the Chinese longitudinal healthy longevity survey (CLHLS). Nutrients. 2015;7(9):7562–79.
Matheson EM, King DE, Everett CJ. Healthy lifestyle habits and mortality in overweight and obese individuals. J Am Board Fam Med. 2012;25(1):9–15.
Anothaisintawee T, Lertrattananon D, Thamakaison S, Reutrakul S, Ongphiphadhanakul B, Thakkinstian A. Direct and indirect effects of serum uric acid on blood sugar levels in patients with prediabetes: a mediation analysis. J Diabetes Res. 2017;2017:6830671.
Bombelli M, Quarti-Trevano F, Tadic M, Facchetti R, Cuspidi C, Mancia G, et al. Uric acid and risk of new-onset metabolic syndrome, impaired fasting glucose and diabetes mellitus in a general Italian population: data from the Pressioni Arteriose Monitorate E Loro Associazioni study. J Hypertens. 2018;36(7):1492–8.
Dong X, Li Y, Zhang L, Liu X, Tu R, Wang Y, et al. Independent and interactive effect of sitting time and physical activity on prevalence of hyperuricemia: the Henan Rural Cohort Study. Arthritis Res Ther. 2021;23(1):7.
Kim Y, Kang J. Association of urinary cotinine-verified smoking status with hyperuricemia: analysis of population-based nationally representative data. Tob Induc Dis. 2020;18:84.
Zhang T, Rayamajhi S, Meng G, Zhang Q, Liu L, Wu H, et al. Dietary patterns and risk for hyperuricemia in the general population: Results from the TCLSIH cohort study. Nutrition (Burbank, Los Angeles County, Calif). 2022;93:111501.
Zheng R, Yang M, Bao Y, Li H, Shan Z, Zhang B, et al. Prevalence and determinants of metabolic health in subjects with obesity in Chinese population. Int J Environ Res Public Health. 2015;12(11):13662–77.
He H, Pan L, Pa L, Cui Z, Ren X, Wang D, et al. Data resource profile: the china national health survey (CNHS). Int J Epidemiol. 2018;47(6):1734–5.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95.
Cuddy ML. Treatment of hypertension: guidelines from JNC 7 (the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure 1). J Pract Nurs. 2005;55(4):17–21; quiz 2–3.
Zhu N, Yu C, Guo Y, Bian Z, Han Y, Yang L, et al. Adherence to a healthy lifestyle and all-cause and cause-specific mortality in Chinese adults: a 10-year prospective study of 0.5 million people. Int J Behav Nutr Phys Act. 2019;16(1):98.
Yang YX, Wang XL, Leong PM, Zhang HM, Yang XG, Kong LZ, et al. New Chinese dietary guidelines: healthy eating patterns and food-based dietary recommendations. Asia Pac J Clin Nutr. 2018;27(4):908–13.
Gao M, Wei YX, Lyu J, Yu CQ, Guo Y, Bian Z, et al. [The cut-off points of body mass index and waist circumference for predicting metabolic risk factors in Chinese adults]. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi. 2019;40(12):1533–40.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013;36(Suppl 1):S67–74.
Iseki K, Ikemiya Y, Inoue T, Iseki C, Kinjo K, Takishita S. Significance of hyperuricemia as a risk factor for developing ESRD in a screened cohort. Am J Kidney Dis. 2004;44(4):642–50.
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551–61.
Wang JB, Jiang Y, Wei WQ, Yang GH, Qiao YL, Boffetta P. Estimation of cancer incidence and mortality attributable to smoking in China. Cancer Causes Control. 2010;21(6):959–65.
Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. Mediation: R package for causal mediation analysis. J Stat Softw. 2014;59(5).
Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods. 2010;15(4):309–34.
Pan WC, Wu CD, Chen MJ, Huang YT, Chen CJ, Su HJ, et al. Fine particle pollution, alanine transaminase, and liver cancer: a taiwanese prospective cohort study (REVEAL-HBV). J Natl Cancer Inst. 2016;108(3):djv341.
Zhu Y, Hedderson MM, Quesenberry CP, Feng J, Ferrara A. Central obesity increases the risk of gestational diabetes partially through increasing insulin resistance. Obesity (Silver Spring, Md). 2019;27(1):152–60.
Beydoun MA, Fanelli-Kuczmarski MT, Canas JA, Beydoun HA, Evans MK, Zonderman AB. Dietary factors are associated with serum uric acid trajectory differentially by race among urban adults. Br J Nutr. 2018;120(8):935–45.
Xiong Z, Zhu C, Qian X, Zhu J, Wu Z, Chen L. Serum uric acid is associated with dietary and lifestyle factors in elderly women in suburban Guangzhou in Guangdong province of south China. J Nutr Health Aging. 2013;17(1):30–4.
He H, Pan L, Ren X, Wang D, Du J, Cui Z, et al. The effect of body adiposity and alcohol consumption on serum uric acid: a quantile regression analysis based on the china national health survey. Front Nutr. 2021;8:724497.
Ishizaka N, Ishizaka Y, Toda A, Tani M, Koike K, Yamakado M, et al. Changes in waist circumference and body mass index in relation to changes in serum uric acid in Japanese individuals. J Rheumatol. 2010;37(2):410–6.
Kim SK, Choe JY. Association between smoking and serum uric acid in Korean population: data from the seventh Korea national health and nutrition examination survey 2016. Medicine (Baltimore). 2019;98(7):e14507.
Fanning N, Merriman TR, Dalbeth N, Stamp LK. An association of smoking with serum urate and gout: a health paradox. Semin Arthritis Rheum. 2018;47(6):825–42.
Sivasankari R, Usha B. Reshaping the gut microbiota through lifestyle interventions in women with PCOS: a review. Indian J Microbiol. 2022;62(3):351–63.
Wei W, Jiang WB, Tian Z, Wu HY, Ning H, Yan GC, et al. Fecal g. Streptococcus and g. Eubacterium_coprostanoligenes_group combined with sphingosine to modulate the serum dyslipidemia in high-fat diet mice. Clin Nutr. 2021;40(6):4234–45.
Dwidar M, Park JY, Mitchell RJ, Sang BI. The future of butyric acid in industry. Sci World J. 2012;2012:471417.
Chu Y, Sun S, Huang Y, Gao Q, Xie X, Wang P, et al. Metagenomic analysis revealed the potential role of gut microbiome in gout. NPJ Biofilms Microbiomes. 2021;7(1):66.
Xi HL, Schneider BL, Reitzer L. Purine catabolism in Escherichia coli and function of xanthine dehydrogenase in purine salvage. J Bacteriol. 2000;182(19):5332–41.
Wannamethee SG, Shaper AG, Alberti KG. Physical activity, metabolic factors, and the incidence of coronary heart disease and type 2 diabetes. Arch Intern Med. 2000;160(14):2108–16.
Hodge AM, Karim MN, Hebert JR, Shivappa N, de Courten B. Association between diet quality indices and incidence of type 2 diabetes in the melbourne collaborative cohort study. Nutrients. 2021;13(11):4162.
Wei S, Brejnrod AD, Trivedi U, Mortensen MS, Johansen MY, Karstoft K, et al. Impact of intensive lifestyle intervention on gut microbiota composition in type 2 diabetes: a post-hoc analysis of a randomized clinical trial. Gut Microbes. 2022;14(1):2005407.
Li Y, Chen T, Li Y, Tang Y, Huang Z. Gut microbiota are associated with sex and age of host: Evidence from semi-provisioned rhesus macaques in southwest Guangxi, China. Ecol Evol. 2021;11(12):8096–122.
Takagi T, Naito Y, Inoue R, Kashiwagi S, Uchiyama K, Mizushima K, et al. Differences in gut microbiota associated with age, sex, and stool consistency in healthy Japanese subjects. J Gastroenterol. 2019;54(1):53–63.
Xu X, Zhang Z. Sex- and age-specific variation of gut microbiota in Brandt’s voles. PeerJ. 2021;9:e11434.
Acknowledgements
The authors would like to thank all the participants and investigators that took part in this study.
Funding
This research was supported by Zhejiang Provincial Public Welfare Fund project of China [No. LGF21H260009] and by Zhoushan Science & Technology Plan Project [No. 2021C31082]. The funder had no role in the design of the study, collection, analysis, interpretation of data, writing of the report, and the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
XH: Conceptualization, Formal analysis, Writing-original, draft, Writing-editing. WS, SY, CH, HR, CL: Investigation, Resources. JY: Writing-review & editing. CL, YX: Funding acquisition. YX: Conceptualization, Writing-original draft, Writing editing. YZ: Conceptualization, Writing-review & editing. All authors read and critically revised the manuscript and gave final approval.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the institutional review board at the Zhejiang University, Zhejiang, China. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1
Flowchart of participants included in the study. Figure S2 Dose–response relationship of HLS with risk of T2DM. Figure S3 The combined effect of HLS and hyperuricemia on T2DM. Table S1. Adjusted HR for association between single healthy lifestyle behavior and T2DM. Table S2. Adjusted HR of T2DM according to new HLS without alcohol behavior. Table S3. Association of HLS with T2DM mediated by SUA after additionally adjusting for FPG. Table S4. Association of HLS with T2DM mediated by SUA stratified by sex. Table S5. Association of HLS with T2DM mediated by SUA stratified by age.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
He, X., Shao, W., Yu, S. et al. Healthy lifestyle scores associate with incidence of type 2 diabetes mediated by uric acid. Nutr Metab (Lond) 20, 47 (2023). https://doi.org/10.1186/s12986-023-00763-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12986-023-00763-y