Abstract
Background
Elevated post-prandial blood glucose during pregnancy has been associated with adverse pregnancy and offspring outcomes, such as maternal gestational diabetes and excessive foetal growth. The ROLO Study is a randomized controlled trial (RCT) investigating the effect of a low glycaemic index (GI) diet in pregnancy to prevent foetal macrosomia (birth weight > 4000 g). We described the impact of a low-GI diet on the maternal and feto-placental unit metabolism by studying how the ROLO intervention affected maternal and cord blood metabolomes.
Methods
Fasting maternal plasma samples pre- and post-intervention of 51 pregnant women and 132 cord blood samples were measured with a targeted metabolomics approach using liquid-chromatography coupled to tandem mass spectrometry. The differences between RCT groups were explored via multivariate models with covariates correction. Significance was set at Bonferroni-corrected level of 0.05.
Results
A total of 262 metabolites species, sums and ratios were investigated. While no metabolite reached statistical significance after Bonferroni correction, many maternal phospholipids and acylcarnitines were elevated in the intervention group at uncorrected 0.05 alpha level. Most species contained saturated and monounsaturated fatty acid chains with 16 or 18 carbon atoms. In cord blood, no differences were identified between RCT groups.
Conclusions
A low-GI diet in pregnancy was associated with a trend to modest but consistent changes in maternal lipid and fatty acid metabolism. The intervention seemed not to affect foetal metabolism. Our exploratory findings may be used to direct further investigations about low GI diets before and during pregnancy, to improve patient care for pre-conceptional and pregnant women with lipid dysregulations and potentially modulate the offspring’s risk for future metabolic diseases.
Trial registration
Current Controlled Trials ISRCTN54392969.
Similar content being viewed by others
Background
Pregnancy is a period of major endocrine and metabolic changes which modulate both maternal and child’s health [10]. Pregnancy exposures such as gestational diabetes mellitus (GDM), elevated maternal pre-pregnancy body-mass-index (BMI) and gestational weight gain (GWG) are risk factors for type 2 diabetes, overweight, and metabolic syndrome not only in the mother [3, 10, 27] but also in the offspring, as suggested by the numerous indications for the Developmental Origins of Health and Disease (DOHaD) hypothesis [12, 24]. Therefore, it is important to understand the mechanisms driving these changes and to build the foundation for acting timely to prevent the onset of disease in mothers and children.
One possible intervention strategy involves targeting maternal blood glucose levels. Elevated fasting and post-prandial blood glucose levels, even in absence of overt pre-existing diabetes or GDM, have been associated with adverse outcomes for mother and child [33]. Nutritional and dietary measures to ameliorate glycaemic control are standard in pregnant women with diabetes and GDM [21]. One dietary parameter of interest is the glycaemic index (GI). The GI of a carbohydrate-containing food, expressed on a scale from 0 to 100, quantifies the peak in the blood sugar concentrations after ingestion of the food [25]; therefore, the consumption of low GI foods is considered desirable to achieve good glycaemic control.
Several randomized control trials to investigate the effect of low-GI diet on maternal and new-born outcomes have been conducted, reporting favourable effects on maternal glycaemic control but heterogeneous results regarding offspring outcomes [48]. In particular, there is a lack of knowledge regarding how a low-GI diet may impact maternal and feto-placental metabolism at a molecular level in a real-environment clinical setting. In this study, we aim to provide insights into this question using a metabolomics approach. Metabolomics is the omics branch investigating small (< 1.5 kDa) intermediates and products of metabolic reactions and is an established tool in metabolism research, with potential applications in precision medicine and personalized patient care [2, 23, 37]. Ultimately, this exploratory study could inform clinical practise on treatments for pregnant women, aimed at increasing maternal wellbeing and decreasing the offspring’s risk for future metabolic conditions.
Materials and methods
Study participants and data collection
This was a secondary analysis conducted on data from the ROLO study. The ROLO study (Randomised cOntrol trial of LOw glycaemic index diet versus no dietary intervention to prevent recurrence of foetal macrosomia, 2007–2011, Dublin, Ireland) tested the hypothesis of a low-GI diet in pregnant women to reduce birth weight in secundigravida with a previous macrosomic child (birth weight > 4000 g); the intervention group (n = 394) received an educational session about low-GI diet at the beginning of the second trimester, while the standard group (n = 406) received standard care only (trial registration: Current Controlled Trials ISRCTN54392969) [46].
Recruitment and the first study visit took place at the end of the first pregnancy trimester (median: 13th gestation week) and rapidly followed by the educational session (median: 15th week); additional visits were held at 28th and 34th weeks of gestation.
Maternal age at delivery, early pregnancy weight and BMI, weight at 34th week, gestational age at delivery, newborn’s sex, weight and length were documented. Gestational weight gain (GWG) was defined as weight at last measured visit (38th or 40th gestational week) after subtraction of early pregnancy weight; for cases with missing weight at 38th or 40th week, GWG was imputed by adding the overall ROLO median GWG between 34th and 38th week to the weight measured at 34th week. Newborn’s ponderal index at birth was calculated as 100 ∙ birth weight (g) / birth length3 (cm3).
Maternal fasting blood samples were collected at recruitment and again at the 28th week. Cord blood was collected at delivery. Total, HDL and LDL cholesterol were measured via Roche cholesterol oxidase method and direct HDL Roche 3rd generation method, respectively, on the cobas C702 module of the Roche Cobas 8000 analyser (Roche Diagnostics GmbH, Penzberg, Germany); the Friedewald equation was used to estimate LDL-cholesterol concentrations [7].
Three-days food diaries were collected in each pregnancy trimester and evaluated by a research dietitian via WISP software version 3.0 (Tinuviel Software, Llanfechell, UK) [32]. From these data, the absolute GI intake and the proportion of energy derived from saturated, monounsaturated and polyunsaturated fat intake, expressed as percentage of total energy intake (% kcal), were derived.
Metabolomics measurements
For subgroups of evaluable mother/child pairs, aliquots of the collected samples were provided for metabolomics analysis. Plasma samples were measured in a targeted approach using liquid chromatography coupled to tandem mass spectrometry (LC/MS-MS) in the laboratory of the Division of Metabolic and Nutritional Medicine, Dr. von Hauner Children’s Hospital (LMU Munich). Five classes of metabolites were analysed: amino acids (AA), non-esterified fatty acids (NEFA), acylcarnitines (AC), branched chain keto acids (BCKA) and intermediates of TCA cycle (TCA), and phospholipids (PL) (including sphingomyelins (SM), diacyl-phosphatidylcholines (PCaa), acyl-alkyl-phosphatidylcholines (PCae) and lysophosphatidylcholines (LPC)). After preparation, samples were randomly distributed in 4 96-wells batches with maternal blood (1–4) and 3 batches with cord blood (5–7). In each batch, up to 80 test samples were measured together with 6 quality control (QC) samples (prepared as pooled mixture of the samples from batch 1, for maternal blood, or from batch 5, for cord blood) and 10 standards used for quantification. The injection of the samples was randomized in each run, with QC and standards being injected regularly every 6–7 test samples. Measurements and QC were performed separately for each blood source.
Samples preparation
Proteins of 50 μL plasma were precipitated on a plate with PTFE filter elements by adding 450 μL methanol including internal standards (ISD). After centrifugation the filtrate was split into aliquots for the analyses of individual methods.
Amino acids
Fifty μL of the filtrate was used for the derivatization to AA butyl ester with hydrochloric acid in 1-butanol according to the method described by Harder et al. [15]. A set of labeled amino acid standards (set A, Cambridge Isotope Laboratories) mixed with L-Asparagine (15 N2, 98%, Cambridge Isotope Laboratories) and L-Tryptophan (Indole-D5, 98%, Cambridge Isotope Laboratories) was used as internal standard (ISD). After evaporation, the residues were dissolved in water/methanol (80:20) with 0.1% formic acid and determined by LC-MS/MS equipped with 150 × 2.1 mm, 3.5 μm particle size C18 HPLC column (X-Bridge, Waters, Milford, USA) and 0.1% heptafluorobutyric acid as ion pair reagent in mobile phase A (water) and B (methanol). MS detection was performed with a triple quadrupole mass spectrometer (API2000, Sciex, Darmstadt, Germany) with atmospheric pressure chemical ionization source (APCI) operating in positive ion ionization mode.
NEFA
Fifty μL of the filtrate was diluted with100 μL methanol and injected to a LC-MS/MS operating in negative electrospray ionization (ESI) mode for identification of NEFA as described by Hellmuth et al. [16]. Uniformly 13C-labeled palmitic acid was used as ISD. Samples were injected to an HPLC system (1200, Agilent, Waldbronn, Germany) with a UPLC diphenyl column (Pursuit UPS Diphenyl, Agilent, Waldbronn, Germany). Five mM ammonium acetate and 2.1 mM acetic acid in water were used as mobile phase A and acetonitrile/isopropanol (80/20) as mobile phase B. A hybrid triple quadrupole mass spectrometer (4000 QTRAP, Sciex, Darmstadt, Germany) operating in negative ESI multiple reaction monitoring mode (MRM) mode was used for MS detection. This method allows for the separation of NEFA species differing in chain length and number of double bonds, but not in the position of double bonds. The analytical process was post-processed using Analyst software version 1.6.2.
BCKA and TCA
Organic and keto-acids were measured by a modified method based on previously published procedures [4, 30]. D3-methylmalonic acid (Cambridge Isotope Laboratories, Teweeksbury, MA, USA) was used as ISD. One hundred μL of the supernatant were evaporated to dryness and re-suspended in 50 μL water. Five μL of the extracted samples were injected by HPLC system (1200, Agilent, Waldbronn, Germany) on a Kinetex F5 core-shell HPLC column, 150 × 2.1 mm, 2.6 μm particle size (Kinetex F5, Phenomenex, Aschaffenburg, Germany) for chromatographic separation of molecular species. The mobile phase A was water with 1% formic acid and mobile phase B was composed of methanol/isopropanol (50/50) with 1% formic acid. A gradient elution at a flow rate of 250 μL/min was held constant for 1 min with 1% B, raised to 65% B within 6 min, and turned back to initial conditions of 1%B within 0.5 min. The triple quadrupole mass spectrometer (4000QTRAP, Sciex, Darmstadt, Germany) was operated in negative scheduled MRM mode using ESI.
Phospholipids
Phospholipids were analyzed as described by Uhl et al. [45] using LPC (13:0) and PC (14:0/14:0) (Avanti Polar Lipids, Alabaster, Alabama, USA) as ISD. Thirty μL of the centrifuged supernatant were mixed for 20 min at 600 rpm with 500 μl methanol containing 1.2 mM ammonium acetate. Phospholipids were analyzed by flow-injection analysis (FIA) in a triple quadrupole mass spectrometer (QTRAP4000, Sciex, Darmstadt, Germany) coupled to a LC system (1200 Agilent, Waldbronn, Germany). ESI was used in positive ionization mode. MS/MS analysis was run in positive MRM mode with 184 Da (choline head group) as product ion for the PL. Analyst 1.6.2 software, followed by in-house processing with the statistical software R [44], was used for post-processing. The number of carbon atoms (XX) and double bonds (Y) is expressed in the form C XX:Y.
Acylcarnitines
D3-carnitine-C2, D3-carnitine-C8 and D3-carnitine-C16 (all Cambridge Isotope Laboratories, Teweeksbury, MA, USA) were used as ISDs. FIA with isocratic elution with 76% isopropanol, 19% methanol and 5% water was used to measure acylcarnitines. The mass spectrometer (4000 QTRAP, Sciex, Darmstadt, Germany) was equipped with ESI and operated in positive ionization mode.
Quality control
To ensure precision of the measured samples, 6 QC samples, pooled from the test samples, were measured in each batch. Batches with a coefficient of variation (CV) > 25% were excluded. If at least 75% of the batches for a metabolite passed the intra-batch quality control, the inter-batch CV was calculated, and the metabolite was kept if CV < 30%. In each batch, at most one QC sample was allowed to be an outlier (defined as measurement further away than 1.5 interquartile range (IQR) from the next measurement) and removed.
After quality control, 6 sums and ratios were additionally calculated: sums of PCaa, PCae, total PC, total SM, ratio of total SM to total PC, ratios of NEFA 18:1/18:0 and 16:1/16:0 depicting SCD-1 activity [6], and five ratios of AC 2:0 to mid-chain AC (AC 14:0, 16:0, 16:1, 18:0, 18:1) depicting fatty acid oxidation (FAO) [29].
Statistical treatment
Data preparation
QC and statistical treatment of the data were performed using the statistical software R version 3.4.3 [44].
To ensure interpretability of the results, only subjects with covariates information, mothers with longitudinal metabolomics data (full set analysis) and babies born after the 37th gestational weeks were included. The final sample sizes for maternal and cord analyses were thus 51 and 132 subjects, respectively. Metabolomics outliers identification and removal was performed before models calculation within each blood source and visit time point; outliers were defined as concentration values further away than 3 standard deviations from the next measurements.
Covariables are presented descriptively as median (IQR) or as absolute number (percentage), stratified by blood source and RCT arms. Variables were compared in the two RCT arms using Mann Whitney U-tests.
Main models
For each metabolite, a generalized additive model (GAM) was calculated using the function gam() from the R package mgcv [47]. In the following notations, s(∙) indicates a non-linear effect and 1|∙ the random intercept.
The models for maternal metabolites were calculated as follows: metabolite at 28 weeks ~ RCT group + maternal BMI + metabolite at 13 weeks + s (sample storage time) + 1|batch number. Full results are presented in Additional file 1. Maternal age was included in a first step, but since preliminary results showed weak to no associations with maternal age, the variable was removed to preserve statistical power. For some metabolites of interest, a sensitivity analysis was conducted by re-calculating the models after trimming the highest and lowest 5 concentration values. Additional univariate and multivariate sensitivity analyses (including the association of selected metabolites with dietary fat intakes) and their results are presented in Additional file 2.
The models for cord metabolites were calculated as follows: metabolite ~ RCT group + maternal BMI + gestational age + foetal sex + s (sample storage time) + 1|batch number. As sensitivity analysis, the following covariates were included one at a time in the model: ponderal index (PI) of the new-born, maternal GWG, cord HDL, LDL and total cholesterol. Since the results did not substantially change, these are not presented. Additionally, the calculation of the main model was repeated by including only those maternal/child dyads for which also maternal blood was analysed.
Significance and reported values
From these models, the standardized beta estimates, uncorrected and Bonferroni-corrected p-values and 95% confidence interval of the beta estimate for the RCT variable are reported. Associations with Bonferroni-corrected p-values < 0.05 were defined as ‘significant’, associations with uncorrected p-values < 0.05 were defined as ‘trends’. False discovery rate (FDR) p-values correction was also applied, but, since the significant metabolites did not differ between the two approaches, we used only Bonferroni due to its easier interpretation. Metabolites with uncorrected RCT p-value < 0.05 were visually inspected via grouped boxplots. Results of these models are presented in graphical form via Manhattan plots.
Results
Covariates
The covariates, stratified for the two subpopulations (maternal blood samples/cord blood samples), are presented in Table 1. Maternal samples from 51 mothers (control/intervention: 26/25) and 132 cord blood samples (68/64) were included in the analysis; both maternal and cord blood were analysed for 48 mother/child dyads. Only GI in trimester 2 (i.e. after the intervention) and gestational age were significantly different between the RCT arms.
Metabolites
Two hundred twenty-nine analytes were used in the analyses for maternal blood, 197 in cord blood. A total of 257 analytes passed the quality control in at least one of the blood sources, 170 of which in both. These were: sum of hexoses (H1), 22 AA, 33 NEFA, 26 AC (including free carnitine), 8 TCA, 2 BCKA, 7 LPC, 24 PCaa, 26 PCae, and 21 SM. In both blood sources it was additionally possible to investigate sums and ratios.
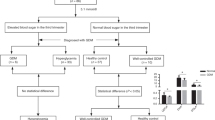
RCT and maternal blood
After Bonferroni correction, no significant differences were found (see Fig. 1 and Additional file 1). However, 40 metabolites were higher in intervention than control arm at uncorrected 0.05 level (see Table 2): two NEFA (16:1 and 18:1), eight mid-chain AC (with chain length from 8 to 18 carbon atoms), three LPC (with chain lengths of 16 and 18 carbon atoms), 15 PCaa and PCae (13 of which containing a 16- or 18-carbon atom saturated or monounsaturated fatty acid (FA) chain), and 12 SM (with saturated or monounsaturated FA chains). The sum of SM and two FAO markers were also significantly higher (uncorrected 0.05 level) in the intervention group; no other sum or ratio was different between the groups.
Manhattan plot for the association of maternal metabolites with the RCT arm. Associations were calculated via generalized additive model with correction for maternal BMI, baseline metabolite levels, sample storage time (non-linear effect) and random intercept for batch number. The full list of legend abbreviations is available in the methods section
RCT and cord blood
No significant difference was found (see Fig. 2), and weak trends for elevated values in the intervention group were identified for only 3 metabolites: NEFA 14:1 and 15:1 and AC 20:0 (see Additional file 1). The subanalysis including only overlapping mother/child dyads delivered a similar picture, with PCaa 30:0, AC 4:0 and the branched-chain AA (BCAA) Valine (Val) showing a trend for lower values in the intervention group. Val, in particular, was more strongly different than the other two analytes (uncorrected p = 0.005). This subpopulation did not significantly differ in the baseline characteristics from the total population.
Manhattan plot for the association of cord metabolites with the RCT arm. Associations were calculated via generalized additive model with correction for maternal BMI, gestational age, foetal sex, sample storage time (non-linear effect) and random intercept for batch number. The full list of legend abbreviations is available in the methods section
Discussion
In this study, we explored the impact of a dietary intervention promoting a low-GI diet during pregnancy on the metabolome of pregnant women and cord blood of their offspring. We found that the low-GI diet was associated with consistently higher concentrations of phospholipids (PL) and acylcarnitines (AC) in maternal blood (though non-significant after correction for multiple testing), while cord blood metabolome was not substantially affected by the intervention.
Maternal blood
All changes identified in maternal blood between control and intervention groups were related to fatty acids (FA), either non-esterified or in the form of acyl esters or PL chains. PLs are membranes lipids whose abundance is associated with both endogenous metabolism and dietary intake [14, 22]. The amount and composition of dietary fat consumed by the mothers did not change over pregnancy or due to the intervention, thus an exogenous change in fat intake can be excluded. It is possible that the low-GI diet modifies metabolism towards the release of fat from adipose tissue, hence the usage of fat as source of energy (as seen in the higher FAO markers and AC) and their transport (via PL).
A recent study by Hernandez-Alonso et al. found that a low-GI diet over 6 months was associated with changes in amino acid concentrations (both positively and negatively) and with a marked decrease in phospholipids, particularly SM and LPC, when compared both intra-subject to the patient’s own baseline levels or inter-subjects against patients following high GI or low fat diets [17]. In our results, subjects in the intervention group showed no differences regarding AA, but higher levels of phospholipids, especially those containing FA with 16 and 18 carbon atoms chains, than subjects in the control group. To evaluate these discrepancies, it should be noted that the populations and study design largely differed: Hernandez-Alonso et al. investigated overweight and obese men and women in a calories-restricted setting for over 6 months, while our population was composed of pregnant women in the second half of gestation who embraced an isocaloric, low-GI diet for 12 weeks. In particular, a 6 months calories-restricted diet can be seen as a prolonged catabolic state, while in pregnancy a first anabolic state spanning until the end of the first trimesters is followed by an accelerated catabolic state in the third trimester [19, 20, 29]; therefore, our data, collected at the end of the second trimester, might represent the peak of the anabolic phase or the begin of the catabolic phase.
All AA modulated by low-GI diet in Hernandez-Alonso’s study have been observed to decrease during gestation [29]; this progression has been linked to the increased placental uptake for foetal protein synthesis [29] and it is possible that the foetal needs might dominate over their regulation due to low-GI diet. Maternal phospholipids, especially PL and SM, have been observed to rise during pregnancy [29, 41]; this rise has been attributed to oestrogens [42] and similar differences in phospholipids have also been observed in young adult women taking hormonal contraceptives [38]. Moreover, a systematic review conducted by Goff et al. in 2013 found that low-GI diet reduces total and LDL cholesterol but does not affect HDL cholesterol [13] (meta-analysis estimate for reduction in LDL for a low-GI diet of 9–20 weeks from a total population of 1281 study subjects: − 0.16 mmol/l, 95% CI: − 0.24 to − 0.08). These results refer to intra-subject differences pre- and post-intervention. In our data, neither the absolute LDL concentrations at 28th week nor their difference to the baseline levels were different between the groups. During pregnancy, a marked increase in circulating lipoproteins occurs (e.g., LDL cholesterol is expected to increase from < 2.59 mmol/l in non-pregnant population to up to 5.8 mmol/l at the end of gestation) [1], as the high foetal demand for cholesterol is matched solely by maternal supply during the first two trimesters [18]. It is plausible that, also in the case of phospholipids, the cholesterol- and phospholipids-lowering effect of a low-GI diet might be inhibited by the major endocrinologic changes enacted to provide for the increased needs of mother and foetus.
Nevertheless, some of the species higher in the intervention group (total SM, SM C42:2 and C42:3) were found to be associated with LDL lipoproteins in pregnant women in a recent publication by Rauschert et al. [36]. Moreover, the absolute differences in GI in the population under investigation were very modest (see Table 2), so it is possible that a more intensive dietary intervention beginning pre-conceptually might in fact be beneficial for prospective mothers with potential lipid dysregulations.
As for how such changes are enacted, an interesting study in mice by Stavrovskaya et al. [40] found that GI and fat composition work synergistically in affecting the FA composition of cardiolipins, a subclass of mitochondrial PLs; that is, the changes in the FA composition of cardiolipids were more pronounced if the diet was high GI and high in trans or saturated fat than if either component was present alone. In our data, we could not test this hypothesis due to lack of variability in the dietary fat intake. Nevertheless, our results, combined with the findings from Stavrovskaya et al., urge further investigation of the mechanisms linking fat intake and GI to lipids composition and fat metabolism.
Cord blood
Cord blood metabolome was largely unimpacted by the intervention. We did find a small difference in the concentration of Val between the RCT groups in the analysis of the overlapping subjects which might be indeed be ultimately linked to the lower maternal GI intake (BCAA levels correlate with and might cause insulin resistance [31], while a low GI diet should prevent it); however, since the finding was not replicated in the larger cohort and no other BCAA was different between the study groups, this result has to be interpreted carefully.
In general, data about the impact of lifestyle interventions on cord blood metabolome are scarce; however, our results from the ROLO cohort are in line with previous findings from the UPBEAT study [35], where a lifestyle intervention in pregnant women with obesity, while beneficial to the mothers, did not affect cord blood metabolome [34]. In particular, the enhanced availability of maternal lipids was not mirrored in higher transport to the foetus. This is not surprising, since placental FA transport is subject to complex regulatory mechanisms [5, 11, 39]. Nevertheless, there is the need of a deeper understanding of how maternal diet may influence placental transport, as the data to this regard are scarce [43].
Despite the ROLO trial found no effect of the intervention on birth and early infancy anthropometry measures [46], epidemiological studies show that the effects of in-utero exposures on metabolic health might become evident later in life [24, 26], e.g. because modulated via epigenetic changes [8, 28]. “Subtle but widespread” changes in the DNA methylation were found in the cord blood of babies from the ROLO study, as reported by Geraghty et al. [9]. In other words, the intervention might have not impacted foetal metabolism and early infancy anthropometry, but the in-utero exposure to a low-GI diet might still show its beneficial effects in later stages in life.
Strengths and limitations
The strengths of our analysis were the large panel of metabolites (268 analytes, sums and ratios) studied with the same LC-MS/MS targeted approach, the availability of data from both maternal and cord samples, and the extensive dietary data. A major limitation of our study was the small sample sizes, which nevertheless did not prevent from inspecting the trends in maternal and cord blood. The small magnitude of the difference in GI between the study group and the lack of hormonal measurements as confounding factors might also have obscured additional differences and associations from being identified.
Conclusions
Our analysis showed that a low-GI dietary intervention in pregnancy was associated with modest but consistent increases in maternal plasma phospholipids and utilization of fat as source of fuel, while cord blood was not affected by this intervention. Our study was the first to investigate the effect of a low-GI diet in a pregnant population. Our results were partially in agreement with studies conducted on non-pregnant subjects, and we ascribe discrepancies in the findings to the pregnancy-specific metabolic adaptations enacted to ensure sufficient nutrients to the developing foetus, for which more research is needed. Our exploratory findings may be used to direct further investigations about low-GI diets before and during pregnancy, to improve patient care for pre-conceptional and pregnant women with lipid dysregulations and potentially modulate the offspring’s risk for future onset of metabolic diseases.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- AA:
-
Amino acids
- AC:
-
Acylcarnitine
- BMI:
-
Body-mass index
- CV:
-
Coefficient of variation
- FA:
-
Fatty acid
- FAO:
-
Fatty acid oxidation
- GDM:
-
Gestational diabetes mellitus
- GI:
-
Glycaemic index
- GWG:
-
Gestational weight gain
- ISD:
-
Internal standard
- LC:
-
Liquid chromatography
- LPC:
-
Lysophosphatidylcholine
- MS:
-
Mass spectrometry
- NEFA:
-
Non-esterified fatty acids
- PCaa:
-
Diacyl-phosphatidylcholine
- PCae:
-
Acyl-alkyl-phosphatidylcholine
- PL:
-
Phospholipids
- QC:
-
Quality control
- RCT:
-
Randomized controlled trial
- SM:
-
Sphingomyelin
References
Abbassi-Ghanavati M, Greer LG, Cunningham FG. Pregnancy and laboratory studies: a reference table for clinicians. Obstet Gynecol. 2009;114:1326–31.
Beger RD, Dunn W, Schmidt MA, Gross SS, Kirwan JA, Cascante M, Brennan L, Wishart DS, Oresic M, Hankemeier T, Broadhurst DI, Lane AN, Suhre K, Kastenmüller G, Sumner SJ, Thiele I, Fiehn O, Kaddurah-Daouk R, for “Precision M & Pharmacometabolomics Task Group”-Metabolomics Society I. Metabolomics enables precision medicine: “a white paper, community perspective”. Metabolomics. 2016;12:149.
Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet (London, England). 2009;373:1773–9.
Birkler RI, Stottrup NB, Hermannson S, Nielsen TT, Gregersen N, Botker HE, Andreasen MF, Johannsen M. A UPLC-MS/MS application for profiling of intermediary energy metabolites in microdialysis samples--a method for high-throughput. J Pharm Biomed Anal. 2010;53:983–90.
Desoye G. The human placenta in diabetes and obesity: friend or foe? The 2017 Norbert Freinkel award lecture. Diabetes Care. 2018;41:1362–9.
Flowers MT, Ntambi JM. Stearoyl-CoA desaturase and its relation to high-carbohydrate diets and obesity. Biochim Biophys Acta. 2009;1791:85–91.
Geraghty AA, Alberdi G, O’Sullivan EJ, O’Brien EC, Crosbie B, Twomey PJ, McAuliffe FM. Maternal blood lipid profile during pregnancy and associations with child adiposity: findings from the ROLO study. PLoS One. 2016;11:e0161206.
Geraghty AA, Lindsay KL, Alberdi G, McAuliffe FM, Gibney ER. Nutrition during pregnancy impacts Offspring’s epigenetic status-evidence from human and animal studies. Nutr Metab Insights. 2015;8:41–7.
Geraghty AA, Sexton-Oates A, O'Brien EC, Alberdi G, Fransquet P, Saffery R, McAuliffe FM. A Low Glycaemic Index Diet in Pregnancy Induces DNA Methylation Variation in Blood of Newborns: Results from the ROLO Randomised Controlled Trial. Nutrients. 2018;10(4):455. https://doi.org/10.3390/nu10040455.
Gilmore LA, Klempel-Donchenko M, Redman LM. Pregnancy as a window to future health: excessive gestational weight gain and obesity. Semin Perinatol. 2015;39:296–303.
Gil-Sanchez A, Koletzko B, Larque E. Current understanding of placental fatty acid transport. Curr Opin Clin Nutr Metab Care. 2012;15:265–72.
Gluckman PD, Hanson MA, Beedle AS. Early life events and their consequences for later disease: a life history and evolutionary perspective. Am J Hum Biol. 2007;19:1–19.
Goff LM, Cowland DE, Hooper L, Frost GS. Low glycaemic index diets and blood lipids: a systematic review and meta-analysis of randomised controlled trials. Nutr Metab Cardiovasc Dis. 2013;23:1–10.
Guerra A, Demmelmair H, Toschke AM, Koletzko B. Three-year tracking of fatty acid composition of plasma phospholipids in healthy children. Ann Nutr Metab. 2007;51:433–8.
Harder U, Koletzko B, Peissner W. Quantification of 22 plasma amino acids combining derivatization and ion-pair LC-MS/MS. J Chromatogr B Anal Technol Biomed Life Sci. 2011;879:495–504.
Hellmuth C, Weber M, Koletzko B, Peissner W. Nonesterified fatty acid determination for functional lipidomics: comprehensive ultrahigh performance liquid chromatography-tandem mass spectrometry quantitation, qualification, and parameter prediction. Anal Chem. 2012;84:1483–90.
Hernández-Alonso P, Giardina S, Cañueto D, Salas-Salvadó J, Cañellas N, Bulló M. Changes in Plasma Metabolite Concentrations after a Low-Glycemic Index Diet Intervention, vol. 63; 2019. p. 1700975.
Herrera E. Lipid metabolism in pregnancy and its consequences in the fetus and newborn. Endocrine. 2002;19:43–55.
Herrera E, Desoye G. Maternal and fetal lipid metabolism under normal and gestational diabetic conditions. Horm Mol Biol Clin Invest. 2016;26:109–27.
Herrera E, Ortega-Senovilla H. Maternal lipid metabolismduring normal pregnancy and its implications to fetal development. Clin Lipidol. 2010;5:899–911.
Hod M, Kapur A, Sacks DA, Hadar E, Agarwal M, Di Renzo GC, Roura LC, McIntyre HD, Morris JL, Divakar H. The International Federation of Gynecology and Obstetrics (FIGO) initiative on gestational diabetes mellitus: a pragmatic guide for diagnosis, management, and care#, vol. 131; 2015. p. S173–211.
Hodson L, Skeaff CM, Fielding BA. Fatty acid composition of adipose tissue and blood in humans and its use as a biomarker of dietary intake. Prog Lipid Res. 2008;47:348–80.
Hodyl NA, Muhlhausler B. Novel insights, challenges and practical implications of DOHaD-omics research, vol. 204; 2016. p. 108–10.
Hoffman DJ, Reynolds RM, Hardy DB. Developmental origins of health and disease: current knowledge and potential mechanisms. Nutr Rev. 2017;75:951–70.
Jenkins DJ, Wolever TM, Taylor RH, Barker H, Fielden H, Baldwin JM, Bowling AC, Newman HC, Jenkins AL, Goff DV. Glycemic index of foods: a physiological basis for carbohydrate exchange. Am J Clin Nutr. 1981;34:362–6.
Koletzko B, Godfrey KM, Poston L, Szajewska H, van Goudoever JB, de Waard M, Brands B, Grivell RM, Deussen AR, Dodd JM, Patro-Golab B, Zalewski BM. Nutrition during pregnancy, lactation and early childhood and its implications for maternal and long-term child health: the early nutrition project recommendations. Ann Nutr Metab. 2019;74:93–106.
Lauenborg J, Mathiesen E, Hansen T, Glumer C, Jorgensen T, Borch-Johnsen K, Hornnes P, Pedersen O, Damm P. The prevalence of the metabolic syndrome in a danish population of women with previous gestational diabetes mellitus is three-fold higher than in the general population. J Clin Endocrinol Metab. 2005;90:4004–10.
Lillycrop KA, Burdge GC. Maternal diet as a modifier of offspring epigenetics. J Dev Orig Health Dis. 2015;6:88–95.
Lindsay KL, Hellmuth C, Uhl O, Buss C, Wadhwa PD, Koletzko B, Entringer S. Longitudinal Metabolomic profiling of amino acids and lipids across healthy pregnancy. PLoS One. 2015;10:e0145794.
Luo B, Groenke K, Takors R, Wandrey C, Oldiges M. Simultaneous determination of multiple intracellular metabolites in glycolysis, pentose phosphate pathway and tricarboxylic acid cycle by liquid chromatography-mass spectrometry. J Chromatogr A. 2007;1147:153–64.
Lynch CJ, Adams SH. Branched-chain amino acids in metabolic signalling and insulin resistance. Nat Rev Endocrinol. 2014;10:723–36.
McGowan CA, McAuliffe FM. Maternal dietary patterns and associated nutrient intakes during each trimester of pregnancy. Public Health Nutr. 2013;16:97–107.
Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, Hadden DR, McCance DR, Hod M, McIntyre HD, Oats JJ, Persson B, Rogers MS, Sacks DA. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002.
Patel N, Hellmuth C, Uhl O, Godfrey K, Briley A, Welsh P, Pasupathy D, Seed PT, Koletzko B, Poston L. Cord metabolic profiles in obese pregnant women: insights into offspring growth and body composition. J Clin Endocrinol Metab. 2018;103:346–55.
Poston L, Bell R, Croker H, Flynn AC, Godfrey KM, Goff L, Hayes L, Khazaezadeh N, Nelson SM, Oteng-Ntim E, Pasupathy D, Patel N, Robson SC, Sandall J, Sanders TA, Sattar N, Seed PT, Wardle J, Whitworth MK, Briley AL. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 2015;3:767–77.
Rauschert S, Gazquez A, Uhl O, Kirchberg FF, Demmelmair H, Ruiz-Palacios M, Prieto-Sanchez MT, Blanco-Carnero JE, Nieto A, Larque E, Koletzko B. Phospholipids in lipoproteins: compositional differences across VLDL, LDL, and HDL in pregnant women. Lipids Health Dis. 2019;18:20.
Rauschert S, Kirchberg FF, Marchioro L, Koletzko B, Hellmuth C, Uhl O. Early programming of obesity throughout the life course: a metabolomics perspective. Ann Nutr Metab. 2017a;70:201–9.
Rauschert S, Uhl O, Koletzko B, Mori TA, Beilin LJ, Oddy WH, Hellmuth CJBSD. Sex differences in the association of phospholipids with components of the metabolic syndrome in young adults, vol. 8; 2017b. p. 10.
Segura MT, Demmelmair H, Krauss-Etschmann S, Nathan P, Dehmel S, Padilla MC, Rueda R, Koletzko B, Campoy C. Maternal BMI and gestational diabetes alter placental lipid transporters and fatty acid composition. Placenta. 2017;57:144–51.
Stavrovskaya IG, Bird SS, Marur VR, Sniatynski MJ, Baranov SV, Greenberg HK, Porter CL, Kristal BS. Dietary macronutrients modulate the fatty acyl composition of rat liver mitochondrial cardiolipins. J Lipid Res. 2013;54:2623–35.
Svanborg A, Vikrot O. Plasma lipid fractions, including individual phospholipids, at various stages of pregnancy. Acta Med Scand. 1965;178:615–30.
Svanborg A, Vikrot O. The effect of estradiol and progesterone on plasma lipids in oophorectomized women. Acta Med Scand. 1966;179:615–22.
Symonds ME, Bloor I, Ojha S, Budge H. The placenta, maternal diet and adipose tissue development in the newborn. Ann Nutr Metab. 2017;70:232–5.
Team RC. R: a language and environment for statistical computing. Vienne: R Foundation for Statistical Computing; 2018.
Uhl O, Fleddermann M, Hellmuth C, Demmelmair H, Koletzko B. Phospholipid species in newborn and 4 month old infants after consumption of different formulas or breast Milk. PLoS One. 2016;11:e0162040.
Walsh JM, McGowan CA, Mahony R, Foley ME, McAuliffe FM. Low glycaemic index diet in pregnancy to prevent macrosomia (ROLO study): randomised control trial. BMJ. 2012;345:e5605.
Wood SN. Generalized additive models: an introduction with R (2nd edition); 2017.
Zhang R, Han S, Chen GC, Li ZN, Silva-Zolezzi I, Pares GV, Wang Y, Qin LQ. Effects of low-glycemic-index diets in pregnancy on maternal and newborn outcomes in pregnant women: a meta-analysis of randomized controlled trials. Eur J Nutr. 2018;57:167–77.
Acknowledgements
We thank Alexander Haag (LMU Munich) who performed the samples preparation and metabolomics measurements. We thank the ROLO study team for their work in data collection and all the ROLO study participants and their families for their collaboration. Finally, we thank Martina Totzauer and the two anonymous reviewers for their helpful comments and suggestions.
The data presented are part of the PhD thesis accomplished by Linda Marchioro at the Faculty of Medicine of the LMU Munich.
Funding
Funding was obtained by the following sources: European Union’s 7th Framework Program (FP7/2017–2013), Early Nutrition project, grant agreement No. 289346; European Research Council Advanced Grant ERC-2012-AdG No. 322605, META-GROWTH project; H2020 Programmes DYNAHEALTH- 633595 und Lifecycle-733206, Erasmus+ Programmes Early Nutrition eAcademy Southeast Asia-573651-EPP-1-2016-1-DE-EPPKA2-CBHE-JP and Capacity Building to Improve Early Nutrition and Health in South Africa-598488-EPP-1-2018-1-DE-EPPKA2-CBHE-JP, the European Joint Programming Initiative Project NutriPROGRAM, the German Ministry of Education and Research, Berlin (Grant Nr. 01 GI 0825), and German Research Council (DFG INST 409/224–1 FUGG). The ROLO Study received additional funding from the Health Research Board of Ireland, Centre for Diet and Health Research, and from the National Maternity Hospital Medical Fund.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: FMMA, BK. Collected the data: AAG, ECOB. Conducted experiments: OU. Analysed and interpreted the data: LM, ES. Contributed reagents/materials/analysis tools: FMMA, BK, OU. Wrote the paper: LM. Reviewed, edited, and approved the paper: all authors. Provided funding: FMMA, BK.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ROLO Study had received approval from the ethics committee of the National Maternity Hospital (June 2006) and all study participants were included in the study after giving written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest i.e. circumstances that involve the risk that the professional judgment or acts of primary interest may be unduly influenced by a secondary interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Results of the generalized additive models. (XLSX 83 kb)
Additional file 2:
Sensitivity analyses for maternal blood. (DOCX 25 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Marchioro, L., Geraghty, A.A., Uhl, O. et al. Effect of a low glycaemic index diet during pregnancy on maternal and cord blood metabolomic profiles: results from the ROLO randomized controlled trial. Nutr Metab (Lond) 16, 59 (2019). https://doi.org/10.1186/s12986-019-0378-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12986-019-0378-z