Abstract
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection is the cause of coronavirus disease 2019 (COVID-19); a severe respiratory distress that has emerged from the city of Wuhan, Hubei province, China during December 2019. COVID-19 is currently the major global health problem and the disease has now spread to most countries in the world. COVID-19 has profoundly impacted human health and activities worldwide. Genetic mutation is one of the essential characteristics of viruses. They do so to adapt to their host or to move to another one. Viral genetic mutations have a high potentiality to impact human health as these mutations grant viruses unique unpredicted characteristics. The difficulty in predicting viral genetic mutations is a significant obstacle in the field. Evidence indicates that SARS-CoV-2 has a variety of genetic mutations and genomic diversity with obvious clinical consequences and implications. In this review, we comprehensively summarized and discussed the currently available knowledge regarding SARS-CoV-2 outbreaks with a fundamental focus on the role of the viral proteins and their mutations in viral infection and COVID-19 progression. We also summarized the clinical implications of SARS-CoV-2 variants and how they affect the disease severity and hinder vaccine development. Finally, we provided a massive phylogenetic analysis of the spike gene of 214 SARS-CoV-2 isolates from different geographical regions all over the world and their associated clinical implications.
Similar content being viewed by others
Background
The first two decades of the 21st century have been challenged with several new viral outbreaks including avian influenza virus H5N1 (2006), swine influenza virus H1N1 (2009), severe acute respiratory syndrome coronavirus (SARS-CoV) in 2003, Middle East respiratory syndrome coronavirus (MERS-CoV) in 2012, Ebola virus in 2014, Zika virus (2016), and the most recently emerged coronavirus disease 2019 (COVID-19) in 2019. COVID-19 was declared a public health international emergency by the World Health Organization (WHO) on January 31, 2020. It has affected nearly 189 countries/territories with more than 761,071,826 confirmed cases, and around 6,879,677 human deaths and a total of 13,260,401,200 vaccine doses have been administered since March 20, 2023 (WHO, 2023) [1].
Coronaviruses (CoVs) are a family of enveloped, single-stranded, and positive-sense Ribonucleic acid (RNA) viruses (Fig. 1A). CoVs infect many mammals including humans and cause a wide variety of diseases including respiratory, enteric, hepatic, and neurological diseases [2]. They are zoonotic infections with animal origin and have the largest non-segmented RNA viral genome (∼ 30 kb). CoVs belong to the order Nidovirales in the family Coronaviridae and sub-family Orthocoronavirinae and include four genera: alpha-, beta-, gamma-, and delta-coronaviruses [3, 4].
Schematic diagram showing the viral particle structure of SARS-CoV-2 (A), and the genome organization of SARS-CoV-2 genes (B). The structural components of the spike (S) protein; S2 contains signal peptide (SP), N-terminal domain (NTD), and receptor binding domain (RBD). The S1 contains fusion peptide (FP), heptad repeat domains (HR1 and HR2), trans-membrane domain (TMD) and cytoplasmic domain (CD). The arrowhead indicated the furin and TMPRSS2 cleavage sites. (B) The genome organization of SARS-CoV-2 genes
Because of high genomic recombination, CoVs are rapidly evolving and affect a wide host range. It has been reported that all CoVs genera can infect animals [5]. Generally, Alphacoronavirus and Betacoronavirus infect mammals while Gammacoronavirus, and Deltacoronavirus infect both birds and mammals [6]. Interestingly, CoVs infection in human is only associated with Alphacoronaviruses and Betacoronaviruses genera [7]. CoVs that are able to infect human include: Human coronavirus NL63 (HCoV-NL63), Human coronavirus 229E (HCoV-229E), Human coronavirus OC43 (HCoV-OC43), Human coronavirus HKU1 (HCoV-HKU1), SARS-CoV, MERS-CoV, and SARS-CoV-2. HCoV-NL63 and HCoV-229E belong to Alphacoronaviruses, while HCoV-OC43, HCoV-HKU1, SARS-CoV, MERS-CoV, and SARS-CoV-2 belong to the Betacoronavirus [7, 8].
Human coronaviruses are commonly transmitted via the respiratory tract and most of them cause a mild infection like respiratory distress and diarrhea. Based on their pathogenicity, two alpha-CoVs (HCoV-229E and HCoV-NL63) and two beta-CoVs (HCoV-OC43 and HCoV-HKU1) cause a mild infection, while SARS-CoV, MERS-CoV, and SARS-CoV-2 are highly pathogenic to humans and cause severe infection in the lower respiratory system with the high potentiality of fatal respiratory diseases [7, 9,10,11,12].
Three Human CoVs devastating outbreaks have been recorded until now: the 2003 SARS-CoV pandemic, the 2012 MERS pandemic, and the 2019 SARS-CoV-2 pandemic [13,14,15,16]. SARS-CoV-2 infection was initially described in 2019 in Wuhan, China as severe respiratory distress with suspected animal origin. The intermediate host for SARS-CoV-2 is largely unknown. Recent reports indicate that SARS-CoV-2 has undergone several mutations [17,18,19,20,21]. These mutations greatly impact not only disease manifestations and outcomes, but also the performance of vaccines, therapeutic medications, diagnostic tools, and other public health managements. In this review, we aimed to survey and summarize the currently available information about the SARS-CoV-2 outbreak, viral proteins, and genomic mutations, and their functions during infection.
COVID-19 in children
Compared to other age groups, COVID-19 is less common in children and infection is mainly asymptomatic. It has been reported that around 86% of COVID‐19 infected children in China remained undiagnosed which may constitute a risk for infection in elderly people [22]. Therefore, a small number of COVID-19 cases has been reported among children [23].
In a retrospective study of respiratory infections conducted in January 2020 (early in the epidemic) in central Wuhan showed that among 366 children, SARS-CoV-2 was detected in only 6 (1.6%) children [24]. The Chinese novel coronavirus pneumonia emergency response epidemiology team analyzed 72,314 subjects and reported that only 2% out of 44 672 COVID-19 patients were children (0‐19 years), of them 0.9% were under the age of 10 years [22]. In Italy only 1.2% of 22,512 Italian COVID‐19 cases were children and no deaths among the children or adults below the age of 30 years were reported [25]. In the United States, by March 2020, only 5% of 4226 cases were children. Generally, children constitute < 1% of hospitalized US patients [22].
Generally, the symptoms in children are less severe than in adults. A study from the Wuhan Children’s hospital reported cough, pharyngeal erythema, and a fever of at least 37.5 °C to be the most common symptoms [26]. Similarly, another study analyzed 2143 COVID-19 children’s cases and reported that the most common symptoms included fever, cough, sore throat, sneezing, myalgia, fatigue, and sometimes wheezing [27]. The other reported minor symptoms included diarrhea in 8.8% of the infected children, fatigue (7.6%), rhinorrhea (7.6%), and vomiting (6.4%) [26]. Another cohort study was performed including National Health Service (NHS) hospitals in England, Wales, and Scotland. It compared the rate of children and young people admission between the first and second wave of the disease in the UK. It showed that the severity of infection had not changed and that about 20% of the admitted children had asymptomatic/incidental SARS-CoV-2 infection [28]. In conclusion, the prevalence and the severity of COVID-19 are minor in children as compared to elderly people.
Organs impairment in COVID-19
COVID-19 is a multi-organ destroying disease that damages the lungs as the primary organ and affects other organs such as the heart, kidney, and liver. Long-term deterioration to the alveoli in the lungs with consequent respiratory complications was attributed to lung inflammation resulting from COVID-19 infection. Direct and indirect cardiovascular disorders following COVID-19 infection were recorded, including myocardial injury, acute coronary syndrome, cardiac arrhythmias, cardiomyopathy, cardiogenic shock, and thromboembolic difficulties [29]. Moreover, the out-of-hospital cardiac arrest elevated approximately by 60% throughout COVID-19 pandemic in relation to the comparable time in 2019 [29]. Regarding the brain, Covid-19 can lead to strokes, seizures, and temporary paralysis and may also elevate the danger of Parkinson’s disease and Alzheimer’s disease [30].
Initially, a low incidence of acute kidney diseases was reported in COVID-19 patients whereas more recent reports indicate the opposite outcome. It was documented in a study of 59 patients with Covid-19 that 34% of patients developed extensive albuminuria on the first day of hospital stay and 63% of them revealed proteinuria during their hospitalization. Furthermore, inflammation and edema in the kidney as indicated by diminished renal density on CT scan have also been revealed in some patients. Lately, blood in urine, blood urea nitrogen, and upregulated serum creatinine were reported. Despite the mechanism of renal involvement is not elucidated, hypotheses were proposed including cytokine storm or direct cell destruction by SARS-CoV-2 infection. Another outcome that suggests renal involvement in COVID-19 is the virus appearance in the urine samples of many infected patients [31].
Abnormalities of liver functions have been reported in COVID-19 infected patients [32]. The levels of Alanine aminotransferase (ALT), Aspartate transaminase (AST), bilirubin, and Lactate dehydrogenase (LDH) were significantly elevated in severe cases compared with milder cases [33,34,35,36,37,38]. However, autopsy examination showed that the COVID-19 patient did not report serious macroscopic changes in the liver appearance [39]. In another study, examination of a liver biopsy from dead COVID-19 patients revealed moderate micro-vesicular steatosis, and mild portal and lobular activities [40]. Zhang et al. [41] have shown mild sinusoidal dilatation and a low level of infiltrating lymphocytes in the liver tissues. In addition to that the expression of angiotensin converting enzme 2 (ACE2) receptors in the liver cells is very weak and SARS-CoV-2 infection of the hepatocytes affects liver functions insignificantly [42]. However, the changes that occurred in the liver tissues of COVID-19 patients could be the result of other pathological causes such as hypoxemia, thrombi formation, inflammatory mediators’ secretion, or drug-induced liver injuries [43,44,45,46]. Given the fact that severe COVID-19 cases are associated with hypoxemia, liver tissues may also be affected accordingly leading to abnormalities of liver functions. Another explanation for the damage to the liver is the administration of nonsteroidal anti-inflammatory drugs as analgesics by patients before hospital administration [47, 48].
Comorbidities associated with COVID-19 severity
Although limited data are available about COVID-19, it was documented that comorbidities propagate the probability of infection [49]. People at high risk of severe infection include old age with chronic diseases as well as patients with uncontrolled medical conditions such as diabetes mellitus; hypertension; cancer; liver, kidney, lung disorders; smokers; people receiving grafts; and patients under chronic steroids’ treatments. A meta-analysis investigation was performed on COVID-19 comorbidities with a total of 1786 patients [50]. Hypertension was the most prevalent comorbidity (15.8%). Cardiovascular and cerebrovascular disorders (11.7%) and diabetes (9.4%) are also the most common comorbidities [50, 51]. Meanwhile, the same study reported that coexisting infections with HIV and hepatitis B (1.5%), malignancy (1.5%), respiratory illnesses (1.4%), renal disorders (0.8%), and immunodeficiencies (0.01%) were the less common comorbidities. A study in Australia including 1625 patients diagnosed with SARS-CoV-2 infection was performed. It has been documented that there was a significant correlation between comorbidities, including chronic respiratory disease, chronic cardiac disease, and morbid obesity with the disease severity and intensive care unit (ICU) admission [52]. Another cohort study of 7337 COVID-19 individuals with and without type 2 diabetes demonstrated that those with type 2 diabetes necessitated intensive interventions during their hospital stay compared with nondiabetic patients [53]. The previous study concluded that there was a general declined multiple adverse effects and death for patients with blood glucose, particularly for those in the range of 3.9 to 10.0 mmol/L [53]. Reduced blood glucose control was ascribed with significantly higher risk of complications and mortality [53]. Chronic obstructive pulmonary disease (COPD) is another comorbidity that has been related to the severity of the disease. A meta-analysis of multiple studies in China reported that patients suffering from COPD who were diagnosed with COVID-19 revealed a four-fold increase in death [54]. The same study found no significant correlation between smoking and COVID-19 severity outcomes [53]. A prothrombotic coagulopathy may be the cause of patients’ infection with SARS-CoV-2 who suffers from respiratory failure and acute respiratory distress syndrome (ARDS) [55]. Dispersed microthrombi in the pulmonary vasculature were discovered during the autopsy of COVID-19-related deaths, indicating an occlusive reason of respiratory failure [55]. It has been noted that 38 to 100% progress in three cases with COVID-19-related ARDS and respiratory failure, after intravenous (IV) antithrombotic alteplase treatment [55]. However, the outcomes were only temporary in two out of the three cases, as recovery failed after treatment [55]. Subsequently, further research on the use of anti-thrombolytic therapy is required. Different study was done on 342 hospitalized patients with COVID-19. It has been revealed that no relation was detected between proteinuria, which is also an indicator of chronic kidney disease (CKD), and COVID-19 severity [56].
A cohort study of 2007 COVID-19 cases reported that cancer patients had a greater risk of severe complications than those without cancer (39% vs. 8%, p = 0·0003) [57]. The American Association for Cancer Research delivered a report proving the effect of COVID-19 on cancer patients [58]. Although the case fatality rate in the case of COVID19 is relatively low in the general population, it could be doubled among cancer patients [59]. In a retrospective case study on 28 COVID19-infected cancer patients, 53.6% of the patients suffered from severe manifestations and the mortality rate reached 28.6%. Marked deterioration of the patient clinical courses occurred when the antitumor treatment was administered [60]. In conclusion, cancer patients with COVID-19 infection, particularly those with lung cancer, show deteriorating conditions and poor outcomes. Blanco-Melo, et al. [24] reported in a retrospective case study involving 138 patients that 41.3% of the patients have acquired the COVID-19 infection during hospitalization. They found that 5 patients of this cohort were from the oncology department. It is recommended that cancer patients undergoing antitumor care should be actively tested for COVID-19 infection and should not be allowed to take immunosuppressive therapies or at least decrease their dosages in cases of infection with SARS-CoV-2 [60].
SARS-CoV-2 genomic structure and proteins
Genomic structure
SARS-CoV-2 belongs to Sarbecovirus in the genus Betacoronavirus and has a 26 to 32 kb length positive single-stranded RNA genome encoding 9860 amino acids (aa). The SARS-CoV-2 genome contains two untranslated regions (UTRs); 265 nucleotides at 5′ end and 358 nucleotides at 3′ end, and 6 to 11 open reading frames (ORFs) including ORF1a/b, Spike(S), Envelope(E), Membrane or Matrix (M), Nucleocapsid (N), ORF3b and ORF8 [24, 51] (Fig. 1A and B). There are several stem-loop structures in the SARS-CoV-2 genome that are critical for replication and transcription of the viral genome. The ORF1a/b at the 5′ end is the longest among SARS-CoV-2 ORFs comprises a two-thirds of the virus genome and encode two polyproteins, ORF1a and ORF1ab, that are further processed into 16 non-structural proteins (NSP)1–16 [24, 61]. The S, E, M, and N proteins located at the 3-teminus of the SARS-CoV-2 genome are the major viral structural proteins (SPs) [62, 63]. The ORF1a and ORF1a/b proteins are critical for viral transcription and replication, whereas S, E, and M proteins mediate cellular entry, morphogenesis, assembly, and budding of the virus particles, respectively.
SARS-CoV-2 proteins
SARS-CoV-2 SPs
Spike (S) protein
The S protein of SARS-CoV-2 is a glycoprotein located at the surface of viral particle (Fig. 1A). It is the viral fusion protein that mediates viral attachment and internalization to the host cells via binding to ACE2 receptors expressed on the surface of the host cell [64,65,66]. The S protein is a type I membrane glycoprotein and has a crown shape which gives coronaviruses their major morphological characteristics. It is the major determinant of antiviral immune repose and critical for developing viral-neutralizing antibodies against coronaviruses [67]. It is 1300 aa in length and 150 KDa in size and has three major domains: an extracellular domain, a trans-membrane domain (TMD), and an intracellular domain. It is composed of two subunits, a receptor-binding subunit (S1) which binds to the receptor on the host cell surface and mediates viral attachment, and a membrane-fusion subunit (S2) which fuses the host and viral membranes, allowing viral entry into host cells [68, 69] (Fig. 1B). The SARS-CoV-2 S2 subunit is highly conserved with 90% sequence identity to human SARS-CoV and bat SARS-like CoVs, while the S1 subunit is less conserved with 70% sequence identity to other SARS-CoVs [62, 68]. The receptor-binding domain (RBD) of the subunit S1 directly interacts with the peptidase domain of ACE2 receptors. Therefore, RBD is the critical determinant of viral host range, tropism, and infectivity [64, 69].
The membrane (M) protein
SRAS-CoV-2 M glycoprotein is a type III trans-membrane glycoprotein and the most abundant protein on the surface of viral particles. It has 39.2%, 90.1%, 98.2%, and 98.6% homology to that of MERS, SARS-CoV-1, pangolin SARS-CoV, and bat SARS-CoV, respectively [22, 70, 71]. The M protein of SARS-CoV-2 is 25 to 35 KDa in molecular weight and 230 aa in length. It is composed of three major domains; a long C-terminus domain that is imbedded inside the envelope, a triple trans-membrane spanning domain, and a short N-terminus domain protruding outside the viral particle [67, 70, 71] (Fig. 1A).
The M protein is essential for the formation and assembly of the virus particles. The Mutated M protein has been shown to lack the ability to form virus-like particles [67, 72]. Throughout interacting with other viral SPs such as S, E, and N proteins, the M protein mediates a variety of critical functions during coronavirus infection including proliferation, replication, and immune evasion [70]. The binding of the M protein to the N protein has been shown to stabilize the N protein-RNA complex and promote viral assembly [73, 74]. Using in silico analysis has revealed that the M protein of SARS-CoV-2 has a Semi- sugars will eventually be exported transporter (SWEET) sugar transporter-like structure and could influence the glycosylation of another viral glycoprotein like S glycoprotein [71]. Based on this result, it can be assumed that M protein could play a role during virus attachment and entry into the host cell [71].
The nucleocapsid (N) protein
The N protein has a molecular weight of 43–50 KDa with helical capsid symmetry that binds to genomic viral RNA to form helical ribonucleoproteins. It is composed of highly conserved three distinct domains; the N-terminal domain (NTD, residues 45–181) and the C-terminal domain (CTD, residues 248–365) that are linked by an intrinsically central disordered domain (a serine/arginine-rich domain). The N protein binds viral RNA by its NTD and the CTD which are rich in positive aa [75,76,77].
The N protein has been shown to play a critical role in the coronavirus life cycle throughout involving multiple functions including, replication, transcription, and packaging of the viral RNA genome [78,79,80]. Serological analysis of sera from SARS-infected patients revealed a high level of N protein-specific IgG antibodies which indicated the high immunogenicity of this protein [79, 81]. Interestingly, antibodies against the SARS-CoV N protein are more effective than antibodies generated against other SPs because of their higher sensitivity and longer persistence [82, 83]. These results demonstrated that N protein can be used as a target to develop an effective vaccine against SARS-CoV-2 [80, 84, 85].
The envelope (E) protein
The SARS-CoV E protein is a short less abundant viral membrane protein and the smallest structural protein in the viral particle with 74–109 aa length and molecular weight 8.4–10.9 KDa [86,87,88,89]. It consists of three domains: negatively charged hydrophilic NTD, uncharged hydrophobic TMD, and variably charged hydrophilic CTD [86, 87]. The CTD of E protein has a post-synaptic density protein-95/Discs Large/Zonula occludens-1 (PDZ)-binding motif (PBM) which binds to Protein Associated with Caenorhabditis elegans Lin-7 protein 1 (PALS1) [90]. PALS1 is a tight junction-associated protein that belongs to PDZ domain-containing proteins that work as scaffolds for signaling proteins [86, 88, 90, 91].
Consequently, the E protein has been shown to be necessary for the production and maturation of virus particles through interaction with other viral proteins [86, 87]. The interaction of the E protein with the viral M protein is important for viral assembly [87, 92, 93]. Similarly, the TMD of E protein has been proven as a crucial motif for virus release and must be expressed along with viral N, and M proteins for efficient assembly and release of virus-like particles [93,94,95]. Moreover, SARS-CoV E protein is a determinant of viral pathogenesis throughout its role in the elevation of viral virulence and exacerbation of the antiviral immune response [96, 97]. Pending of E protein PDZ-binding motif to cellular protein syntenin leads to redistribution of syntenin from the nucleus to cellular cytoplasm and activation of p38 MAPK pathway which leads to the overexpression of inflammatory cytokines and exacerbation of the virus infection [96]. Interestingly, viral-associated immunopathology was significantly alleviated in cells infected with SARS-CoVs that is lacking E protein PBM and in cells where syntenin has been silencing by using syntenin-specific siRNAs [86, 96].
NSPs
The SARS-CoV-2 genome encodes for NSP1-NSP16 that regulate viral transcription and replication. These NSPs are encoded by ORF 1a/b which is located at the 5′ end of the viral genome (Fig. 1B). The ORF 1a/b initially translated into two primary polyproteins, ORF1a and ORF1ab, that are sequentially processed to 16 NSPs throughout autoproteolytic cleavage [61, 68]. NSP1–NSP10 and NSP12–NSP16 are products of ORF 1a/b while NSP11 is processed from the cleavage of ORF 1a [98, 99]. Coronaviruses NSPs are indispensable for replication and transcription of the viral RNA genome as shown in Table 1.
SARS-CoV-2 genetic diversity and their clinical implications
Sequencing of the whole genome of SARS-CoV-2 revealed that the virus has 96.2% similarity to that of a bat SARS-related coronavirus (SARSr-CoV; RaTG13) collected in Yunnan province, China, but has low similarity to that of SARS-CoV-1 (∼ 79%) and MERS-CoV (∼ 50%) [68, 100]. Although, antigenic drift has been frequently reported in human coronaviruses such as HCoV-229E [101], HCoV-OC43 [102], and SARS-CoV-1 [103, 104], to date there is no antigenic drift reported on SARS-CoV-2 [105]. However, emerging evidence indicated that antigenic or vaccine escape SARS-CoV-2 mutants with high immunological resistance are likely to appear [105, 106]. The emergence of viral antigenic mutants will greatly affect the development of vaccines and immunotherapeutic agents.
SARS-CoV-2 lineages and clades
Based on genetic analysis of the publicly available SARS-CoV-2 genome sequences, there are two major lineages of SARS-CoV-2 designated as linage A and B [107], or S and L, respectively [108]. The lineage B is the most prevalent (∼ 70%), while the lineage A is less dominant (∼ 30%) and has a high correlation to animal coronaviruses [107, 108]. Based on single nucleotide polymorphisms (SNPs) analysis there is a higher mutation rate in the L lineage of SARs-CoV-2 viruses than S lineage [108].
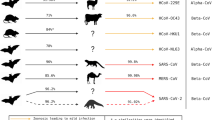
The lineage or clade is a group of viruses that come from one ancestor and are genetically similar. Also, the viruses that showed different specific mutations were assigned as lineage or clade. Figure 2 shows two major lineages from which various virus groups (sublineages) that are similar (not identical) to each other are formed.
The phylogenetic analysis of the full spike (S) protein genes coding region of 214 SARS-CoV-2 sequences deposited in GenBank from various countries all over the world. The tree was constructed using the maximum-likelihood method in the MEGA6 software. The evolutionary distances were computed by General Time Reversible model and bootstrap 1,000 replicates with complete deletion of the gap and missing data. The SARS-CoV-2 sequences from Wuhan, China (blue), bat RaTG13 (pink), mink (green) and Egypt (red). The accession numbers, source of sequence, date and country of origin are shown in the sequence labels
Based on the geographical occurrence (Fig. 2), the frequencies of the predominant mutations and genome sequence identities, SARS-CoV-2 lineages A and B were proposed to be classified into several sub-lineages including sub-lineages A.1 (A.1.1 and A.1.3), A.2, A.3, A.4, A.5, A.6, B.1 (B.1.1, B.1.3, B.1.5, B.1.6, B.1.7, B.1.12, B.1.19, B.1.22, B.1.23, B.1.26, B.1.29, B.1.30 B.1.31, B.1.32, B.1.33, B.1.34 B.1.35, B.1.36, B.1.37, B.1.38, B.1.39, B.1.40, B.1.41, B.1.43 B.1.66, B.1.67, B.1.69, B.1.70, B.1.71), B.2 (B.2.6, B.2.2, B.2.7, B.2.4, B.2.5, B.2.1), B.3, B.4, B.5, B.6. B.7, B.9, B.10, B.13, B.14, B.15, and B.16 [109]. Similarly, there are five designated clades of SARS-CoV-2: O, V, G, GR, and GH clade. The clade G and its mutated GR and GH are predominantly circulated and occupied ∼ 74% of the obtained genome sequences [110,111,112].
SARS-CoV-2 genome mutations
Several mutations have been reported in the SARS-CoV-2 genome [113,114,115]. The viral spike protein G614 mutant is the most common and pathogenic mutation of SARS-CoV-2 [116]. Most of the G614 SARS-CoV-2 mutants belong to the G clade and patients infected with this mutant show higher virus load and low cycle threshold (Ct) value than those infected with SARS-CoV-2 D614 mutant but the severity of the disease did not change in comparison with SARS-CoV-2 viruses bearing a D614 mutation [117]. The D614G variant frequently occurs in sub-lineages B.1, B.1.1, B.1.1.1, B.1.1.10, B.1.5, and B.1.5.4. While lineages B, B.2, B.2.1, and B.2.5 have G251V substitution in the NSP3, the sub-lineages A.1, A.2, and A.5 are associated with L84S mutation in the ORF8 [118]. Nine lineages have been identified in Malaysians including B.6, B, B.1.1, B.1, A, B.1.1.1, B.2, B.1.36, and B.3 according to their incidence in 115 SARS-CoV-2 sequences. Among these lineages, only B.1, B.1.1, B.1.1.1, and B.1.36 lineages have the D614G mutation in the S protein that may increase the SARS-CoV-2 infectivity [119].
Similarly, three deletions have been reported in the genomes of SARS-CoV-2 from Japan (Aichi), the USA (Wisconsin), and Australia (Victoria) [120]. Two of these deletions (3 nt and 24 nt) were in the ORF1ab polyprotein, and one deletion (10 nt) was in the 3′ end of the genome. In addition, there are 93 nucleotide substitutions induced 42 aa mutations in the entire genome including the ORF1ab polyprotein (29 aa), the N protein (8 aa), the M protein (1 aa), and the S (4 aa) surface glycoprotein. It is worth noting that D354, Y364, and F367 aa mutations located in the SARS-CoV-2 S surface glycoprotein RBD may affect the virus antigenicity. aa analysis revealed that the six critical aa (L455, F486, Q493, S494, N501, and Y505) in the RBD of the S protein were completely conserved between SARS-CoV-2 and GD Pangolin-CoV. While only one aa residue was conserved among SARS-CoV-2, SARS-CoV (Y505), and SARSr-CoV; RaTG13 (L455) [108]. Thus SARS-CoV-2 exhibited a higher binding affinity to ACE2 receptors than SARS-CoV [69]. The aa motifs such as G493 and N501 show favorable interaction and compatibility with human ACE2 receptors [65]. Moreover, SARS-CoV-2 has more transmissibility than SARS-CoV which leads to a speedy increase in the confirmed cases worldwide [11]. Two groups of aa mutations in SARS-CoV-2 RBD were identified: the first group possesses F342L and R408I, and the second group has N354D, D364Y, V367F, and W436R aa mutations. The frequency of F342L in RBD among 6 isolates indicated their evolving as a novel sub-lineage and supposed worthy for virus transmission.
In addition to the S protein, mutations in other viral SPs have been shown to modulate virus infection and disease progression [121]. R203K, G204R, R203M, and T205I mutations in viral N protein increased virus infectivity, and disease severity [122, 123]. Similarly, mutations in E (e.g., T9I) and M (e.g., I82T) proteins have been emerged recently. These mutations to impact virus thermodynamic properties and modulate virus infection [124,125,126].
SARS-CoV-2 variants
Multiple variants of SARS-CoV-2 are continually reported worldwide including variants from the United Kingdom, South Africa, and Brazil [127, 128]. Most of these variants have greatly altered transmission, virulence, infection outcome, and infection control strategies, especially diagnostic tests, and vaccines development as shown in Table 2.
WHO’s virus evolution working group (VEWG) classified SARS-CoV-2 into two major variants: a variant of concern (VOC) and a variant of interest (VOI). VOC is characterized by increased transmission, changed clinical manifestations, and decreased efficiency to available vaccines, therapeutics, and public health measurements. The VOI has been reported in many countries to be responsible for community transmission of COVID-19 [129,130,131]. Each of the Global Initiative on Sharing All Influenza Data (GISAID), NEXTstrain, Pango, and WHO have designated their unique nomenclature systems for naming and tracking the VOC and VOI as shown in Table 3. To avoid community or country variants confusion, WHO has recommended using of Greek letters (Alpha, Beta, Gamma…etc.) [131].
The B.1.1.7 lineage (alpha variant)
The VOC 2020/12/01 (20I/501Y.V1) variant also known as alpha or GR/501Y.V1 is a highly transmissible SARS-CoV-2 mutated virus and belongs to lineage B.1.1.7 [132]. This variant was first detected in the United Kingdom in Sep. 2020, and subsequently detected in the United States and Canada [132, 133]. This variant has an unusually large number of mutations (e.g., N501Y, A570D, and D614G in RBD, 69–70, and 144 deletions in S1, P681H near S1/S2 cleavage site, T716I, S982A, and D1118H in S2 (ECDC, 2020; CDC, 2021).
The B.1.351 lineage (Beta variant)
Beta Variant (also known as 20 H/501Y.V2, or GH/501Y.V2 variant) has been detected in South Africa in Oct. 2020 and belongs to the lineage B.1.351 [128]. Although it has some mutations (K417T, E484K, and N501Y in S1 protein RBD) like 20I/501Y.V1, it emerged independently from the 20I/501Y.V1 variant (CDC, 2021).
P.1 variant (Gamma variant)
The Brazilian P.1 variant (also known as 20 J/501Y.V3, Gamma, or GR/501Y.V3 variant) was detected in 42% of the sequenced samples in the Amazon region of Brazil in which 75% of the population was SARS-CoV-2 infected in Oct. 2020 [134]. The Gamma variant also has been detected in a traveler returning from Brazil to Italy, and in 4 Brazilian travelers in Tokyo, Japan as well as in the UK [127, 135, 136]. It has 17 unique mutations with 3 (K417T, E484K, and N501Y) of them in the RBD of S protein and 3 deletions and was clustered in B.1.1.28 lineage [137] (CDC, 2021). In addition, two SARS-CoV-2 sequences were identified in Nigeria belonging to the B.1.1.207 lineage and sharing only P681H mutation with the B.1.1.7 lineage coronaviruses (CDC, 2021).
The B.1.617.2 (Delta variant)
The B.1.617 lineage, also known as G/452.V3 or 21 A/S:478 K identified independently in Maharashtra, India where WHO designated B.1.617 and its sub-lineages, B.1.617.1 (Kappa), B.1.617.2 (Delta), and B.1.617.3 as VOC. The B.1.617 has seven mutations in the spike protein including D111D, G142D, L452R, E484Q, D614G, P614R, and P681R [138]. The double B.1.617 mutations in the spike protein RBD, E484Q, and L452R, are responsible for increasing transmission and infectivity, immune response evasion, and high affinity to the human (h)ACE2 receptors [139, 140].
The B.1.1.529 (omicron variant)
The B.1.1.529 lineage was also recognized as GR/484A or 21 K. The Omicron variant was the most prevalent lineage during 2022. It possesses five sub-lineages with BA.1 being the initial subtype that appeared in South Africa during winter 2021–2022 [4].
The B.1.427/B.1.429 lineage (Epsilon variant)
The B.1.427 and B.1.429 lineages (or GH/452R.V1, or 20 C/S:452R, or Epsilon variant) originated in California. They are characterized by S13I and W152C mutations in the NTD and the L452R mutation in the RBD of spike protein [141].
Conclusions and recommendations
SARS-CoV-2 outbreak is still a major global public health problem. Finding novel therapeutic targets is necessary to combat the SARS-CoV-2 outbreak and its associated pathogenesis. New evidence indicated that viral proteins and their mutations are promising targets to inhibit SARS-CoV-2 infection as they are the main determinants of infection severity and outcome. A better understanding of the role of SARS-CoV-2 proteins and their mutations in COVID-19 progression is mandatory not only to uncover the mystery behind the variations in the outcomes of SARS-CoV-2 infection but also to design an effective vaccine and treatment regimens for SARS-CoV-2 infections and COVID-19 respectively. SARS-CoV-2 variants with public health concerns are continually reported worldwide. The emergence of these variants not only affects viral transmission and virulence, but also hinders vaccine development and production. Tracking and investigating the emerging SARS-CoV-2 variants are valuable tools to tackle the risk of SARS-CoV-2 transmission and to develop an effective vaccine. Future studies are required to investigate and understand the mechanisms behind the emergence of SARS-CoV-2 mutations and variants. Such studies would result in a novel approach toward overcoming the SARS-CoV-2 infection and pandemic.
Data availability
Not applicable.
Abbreviations
- COVID-19:
-
Coronavirus disease-2019
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus-2
- MERS-CoV:
-
Middle East respiratory syndrome coronavirus
- CoVs:
-
Coronaviruses
- HCoV-NL63:
-
Human coronavirus NL63,HCoV-229E,Human coronavirus 229E
- HCoV-OC43:
-
Human coronavirus OC43
- HCoV-HKU1:
-
Human coronavirus HKU1
- ACE2:
-
Angiotensin-converting enzyme 2
- ARDS:
-
Acute respiratory distress syndrome
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate transaminase
- LDH:
-
Lactate dehydrogenase
- NSP:
-
Non-structural proteins
- UTRs:
-
Untranslated regions
- VOC:
-
A variant of concern
- VOI:
-
A variant of interest
References
World Health Organization (WHO). WHO coronavirus (COVID-19) dashboard. 2023. Available at: https://covid19.who.int/. Accessed 28 March 2023.
Haake C, Cook S, Pusterla N, Murphy B. Coronavirus infections in companion animals: virology, epidemiology, clinical and pathologic features. Viruses. 2020;12(9):1023.
Li F. Structure, function, and evolution of Coronavirus Spike proteins. Annu Rev Virol. 2016;3:237–61.
Obeid D, Al-Qahtani A, Almaghrabi R, Alghamdi S, Alsanea M, Alahideb B, Almutairi S, Alsuwairi F, Al-Abdulkareem M, Asiri M, Alshukairi A. Analysis of SARS-CoV-2 genomic surveillance data during the Delta and Omicron waves at a Saudi tertiary referral hospital. J Infect Public Health. 2023;16(2):171–81.
Rao SS, Parthasarathy K, Sounderrajan V, Neelagandan K, Anbazhagan P, Chandramouli V. Susceptibility of SARS Coronavirus-2 infection in domestic and wild animals: a systematic review. 3 Biotech. 2023;13(1):5.
Lewitus E, Bai H, Rolland M. Design of a pan-betacoronavirus vaccine candidate through a phylogenetically informed approach. Sci Adv. 2023;9(3):eabq4149.
Meta Djomsi D, Lacroix A, Soumah AK, Kinganda Lusamaki E, Mesdour A, Raulino R, Peeters M. Coronaviruses are abundant and genetically diverse in West and Central African bats, including viruses closely related to human coronaviruses. Viruses. 2023;15(2):337.
Amanat F, Clark J, Carreno JM, Strohmeier S, Yellin T, Meade PS, Krammer F. (2023) Immunity to seasonal coronavirus spike proteins does not protect from SARS-CoV-2 challenge in a mouse model but has no detrimental effect on protection mediated by COVID-19 mRNA vaccination J Virol e01664-22.
Su S, Wong G, Shi W, Liu J, Lai AC, Zhou J, Gao GF. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol. 2016;24(6):490–502.
Ye ZW, Yuan S, Yuen KS, Fung SY, Chan CP, Jin DY. Zoonotic origins of human coronaviruses. Int J Biol Sci. 2020;16(10):1686.
Tian X, Li C, Huang A, Xia S, Lu S, Shi Z, Lu L, Jiang S, Yang Z, Wu Y, Ying T. Potent binding of 2019 novel coronavirus spike protein by a SARS coronavirus-specific human monoclonal antibody. Emerg Microbes Infect. 2020;9:382–5.
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W, China Novel Coronavirus I, Research T. (2020) A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 382:727–733.
Arora P, Jafferany M, Lotti T, Sadoughifar R, Goldust M. Learning from history: coronavirus outbreaks in the past. Dermatol ther. 2020;33:e13343.
Keshvardoost S, Bahaadinbeigy K, Fatehi F. Role of Telehealth in the management of COVID-19: lessons learned from previous SARS, MERS, and Ebola outbreaks. Telemed J E Health: Official J Am Telemedicine Association. 2020;26:850–2.
Peeri NC, Shrestha N, Rahman MS, Zaki R, Tan Z, Bibi S, Baghbanzadeh M, Aghamohammadi N, Zhang W, Haque U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020;49:717–26.
Bandyopadhyay SS, Halder AK, Saha S, Chatterjee P, Nasipuri M, Basu S. (2023) Assessment of GO-Based Protein Interaction Affinities in the Large-Scale Human–Coronavirus Family Interactome. Vaccines 11(3): 549.
Harvey WT, Carabelli AM, Jackson B, Gupta RK, Thomson EC, Harrison EM, Ludden C, Reeve R, Rambaut A, Peacock SJ, Robertson DL, Consortium C-GU. SARS-CoV-2 variants, spike mutations and immune escape. Nat Rev Microbiol. 2021;19:409–24.
Prajapat M, Handa V, Sarma P, Prakash A, Kaur H, Sharma S, Bhattacharyya A, Kumar S, Sharma AR, Avti P, Medhi B. Update on geographical variation and distribution of SARS-nCoV-2: a systematic review. Indian J Pharmacol. 2021;53:310–6.
Singh J, Pandit P, McArthur AG, Banerjee A, Mossman K. Evolutionary trajectory of SARS-CoV-2 and emerging variants. Virol J. 2021;18:166.
Rais Y, Fu Z, Drabovich AP. Mass spectrometry-based proteomics in basic and translational research of SARS-CoV-2 coronavirus and its emerging mutants. Clin Proteomics. 2021;18:19.
World Health Organization (WHO). WHO Tracking SARS-CoV-2 Variants. 2020. Available online: www.who.int/en/activities/tracking-SARS-CoV-2-variants (accessed on 10 March 2023).
Ahmed SF, Quadeer AA, McKay MR. (2020) Preliminary identification of potential vaccine targets for the COVID-19 coronavirus (SARS-CoV-2) based on SARS-CoV Immunological studies. Viruses 12.
Chan JF, Kok KH, Zhu Z, Chu H, To KK, Yuan S, Yuen KY. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect. 2020;9:221–36.
Blanco-Melo D, Nilsson-Payant BE, Liu WC, Uhl S, Hoagland D, Moller R, Jordan TX, Oishi K, Panis M, Sachs D, Wang TT, Schwartz RE, Lim JK, Albrecht RA, tenOever BR. Imbalanced host response to SARS-CoV-2 Drives Development of COVID-19. Cell. 2020;181:1036–45. e1039.
Livingston E, Bucher K. Coronavirus Disease 2019 (COVID-19) in Italy. JAMA. 2020;323:1335.
Alteri C, Cento V, Antonello M, Colagrossi L, Merli M, Ughi N, Renica S, Matarazzo E, Di Ruscio F, Tartaglione L, Colombo J, Grimaldi C, Carta S, Nava A, Costabile V, Baiguera C, Campisi D, Fanti D, Vismara C, Fumagalli R, Scaglione F, Epis OM, Puoti M, Perno CF. Detection and quantification of SARS-CoV-2 by droplet digital PCR in real-time PCR negative nasopharyngeal swabs from suspected COVID-19 patients. PLoS ONE. 2020;15:e0236311.
Azkur AK, Akdis M, Azkur D, Sokolowska M, van de Veen W, Bruggen MC, O’Mahony L, Gao Y, Nadeau K, Akdis CA. Immune response to SARS-CoV-2 and mechanisms of immunopathological changes in COVID-19. Allergy. 2020;75:1564–81.
Swann OV, Pollock L, Holden KA, Munro AP, Bennett A, Williams TC, ISARIC4C Investigators. Comparison of UK paediatric SARS-CoV-2 admissions across the first and second pandemic waves. Pediatr Res. 2023;93(1):207–16.
Tsai PH, Lai WY, Lin YY, Luo YH, Lin YT, Chen HK, Yang YP. Clinical manifestation and disease progression in COVID-19 infection. J Chin Med Assoc. 2021;84(1):3–8.
Birman D. Investigation of the effects of Covid-19 on different organs of the body. EJCMPR. 2023;2(1):24–36.
Otaghvar HA, Afsordeh K, Hosseini M, Mazhari N, Dousti M. Causes of wound dehiscence in trauma patients with penetrating and non-penetrating abdominal wound in Rasool Akram Hospital within 2017–2020. J Surg Trauma. 2020;8(4):156–60.
Jothimani D, Venugopal R, Abedin MF, Kaliamoorthy I, Rela M. COVID-19 and the liver. J Hepatol. 2020;73(5):1231–40.
Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, Yu J, Kang M, Song Y, Xia J, Guo Q, Song T, He J, Yen HL, Peiris M, Wu J. SARS-CoV-2 viral load in Upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–9.
Sun Y, Dong Y, Wang L, Xie H, Li B, Chang C, Wang FS. Characteristics and prognostic factors of disease severity in patients with COVID-19: the Beijing experience. J Autoimmun. 2020;112:102473.
Cai Q, Huang D, Yu H, Zhu Z, Xia Z, Su Y, Li Z, Zhou G, Gou J, Qu J, et al. COVID-19: abnormal liver function tests. J Hepatol. 2020;73:566–74. [CrossRef] [PubMed].
Chen LY, Chu HK, Bai T. Liver damage at admission is an independent prognostic factor for COVID-19. J Dig Dis. 2020;21:512–8. [CrossRef].
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, et al. Clinical characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–20. [CrossRef].
Wang Y, Liu S, Liu H, Li W, Lin F, Jiang L, Li X, Xu P, Zhang L, Zhao L, et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J Hepatol. 2020;73:807–16. [CrossRef].
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang FS. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respiratory Med. 2020;8:420–2.
Zhang Y, Zheng L, Liu L, Zhao M, Xiao J, Zhao Q. Liver impairment in COVID-19 patients: a retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver International: Official J Int Association Study Liver. 2020;40:2095–103.
Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–7.
McConnell MJ, Kondo R, Kawaguchi N, Iwakiri Y. COVID-19 and Liver Injury: role of inflammatory endotheliopathy, platelet dysfunction, and thrombosis. Hepatol Commun. 2022;6:255–69. [CrossRef].
Dawood DRM, Salum GM, El-Meguid MA. The impact of COVID-19 on Liver Injury. Am J Med Sci. 2022;363:94–103. [CrossRef] [PubMed].
Wijarnpreecha K, Ungprasert P, Panjawatanan P, Harnois DM, Zaver HB, Ahmed A, Kim D. COVID-19 and liver injury: a meta-analysis. European journal of gastroenterology & hepatology; 2020.
Khreefa Z, Barbier MT, Koksal AR, Love G, Del Valle L. Pathogenesis and mechanisms of SARS-CoV-2 infection in the intestine, liver, and pancreas. Cells. 2023;12(2):262.
Sun J, Aghemo A, Forner A, Valenti L. COVID-19 and liver disease. Liver International: Official J Int Association Study Liver. 2020;40:1278–81.
Olry A, Meunier L, Délire B, Larrey D, Horsmans Y, Le Louët H. Drug-Induced Liver Injury and COVID-19 infection: the rules remain the same. Drug Saf. 2020;43:615–7.
Sanyaolu A, Okorie C, Marinkovic A, Patidar R, Younis K, Desai P, Altaf M. Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med. 2020;2:1069–76.
Paudel SS. A meta-analysis of 2019 novel coronavirus patient clinical characteristics and comorbidities. Res Square. 2020. https://doi.org/10.21203/rs.3.rs-21831/v1.
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62.
Alainah O, Hai P, Lucy T, Ernesta S. Demographics, comorbidities and risk factors for severe disease from the early SARS-CoV ‐2 infection cases in Queensland, Australia. Intern Med J. 2023;1–9. https://doi.org/10.1111/imj.16276.
Zhu L, She ZG, Cheng X, Qin JJ, Zhang XJ, Cai J, Li H. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;31(6):1068–77.
Zhao Q, Meng M, Kumar R, Wu Y, Huang J, Lian N, Lin S. The impact of COPD and smoking history on the severity of COVID-19: a systemic review and meta‐analysis. J Med Virol. 2020;92(10):1915–21.
Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK et al. (2020) Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost https://doi.org/10.1111/jth.14828 [Accessed May 30, 2020, https://onlinelibrary.wiley.com/doi/full/10.1111/jth.14828].
Fukui A, Takeshita K, Nakashima A, et al. The relation between proteinuria and the severity of COVID-19. Clin Exp Nephrol. 2023. https://doi.org/10.1007/s10157-023-02428-9.
Liang W, Guan W, Chen R, Wang W, Li J, Xu K, He J. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–7.
Williams PA, Zaidi SK, Sengupta R. AACR report on the impact of COVID-19 on cancer research and patient care. Clin Cancer Res. 2022;28(4):609–10.
Angeletti S, Benvenuto D, Bianchi M, Giovanetti M, Pascarella S, Ciccozzi M. COVID-2019: the role of the nsp2 and nsp3 in its pathogenesis. J Med Virol. 2020;92:584–8.
Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan. China Ann Oncol (March; 2020. p. S0923753420363833.
Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, Tan KS, Wang DY, Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7:11.
Han Q, Lin Q, Jin S, You L. Coronavirus 2019-nCoV: a brief perspective from the front line. J Infect. 2020;80:373–7.
Kumar S, Nyodu R, Maurya VK, Saxena SK. Morphology, Genome Organization, replication, and Pathogenesis of severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). In: Saxena SK, editor. Coronavirus Disease 2019 (COVID-19): Epidemiology, Pathogenesis, diagnosis, and therapeutics. Singapore: Springer Singapore; 2020. pp. 23–31.
Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181:281–e292286.
Wan Y, Shang J, Graham R, Baric RS, Li F. (2020) Receptor recognition by the Novel Coronavirus from Wuhan: an analysis based on Decade-Long Structural studies of SARS Coronavirus. J Virol 94.
Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, Hu Y, Tao ZW, Tian JH, Pei YY, Yuan ML, Zhang YL, Dai FH, Liu Y, Wang QM, Zheng JJ, Xu L, Holmes EC, Zhang YZ. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–9.
Mousavizadeh L, Ghasemi S. Genotype and phenotype of COVID-19: their roles in pathogenesis. Journal of microbiology, immunology, and infection = Wei. mian yu gan ran za zhi; 2020.
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–74.
Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, Graham BS, McLellan JS. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–3.
Liu X, Wang XJ. Potential inhibitors against 2019-nCoV coronavirus M protease from clinically approved medicines. J Genet Genomics. 2020;47:119–21.
Thomas S. The structure of the membrane protein of SARS-CoV-2 resembles the Sugar Transporter SemiSWEET. Pathog Immun. 2020;5:342–63.
de Haan CA, Kuo L, Masters PS, Vennema H, Rottier PJ. Coronavirus particle assembly: primary structure requirements of the membrane protein. J Virol. 1998;72:6838–50.
Escors D, Ortego J, Laude H, Enjuanes L. The membrane M protein carboxy terminus binds to transmissible gastroenteritis coronavirus core and contributes to core stability. J Virol. 2001;75:1312–24.
Narayanan K, Maeda A, Maeda J, Makino S. Characterization of the coronavirus M protein and nucleocapsid interaction in infected cells. J Virol. 2000;74:8127–34.
Chen CY, Chang CK, Chang YW, Su e SC, Bai HI, Riang L, Hsiao CD, Huang TH. Structure of the SARS coronavirus nucleocapsid protein RNA-binding dimerization domain suggests a mechanism for helical packaging of viral RNA. J Mol Biol. 2007;368:1075–86.
Huang Q, Yu L, Petros AM, Gunasekera A, Liu Z, Xu N, Hajduk P, Mack J, Fesik SW, Olejniczak ET. Structure of the N-terminal RNA-binding domain of the SARS CoV nucleocapsid protein. Biochemistry. 2004;43:6059–63.
Zeng W, Liu G, Ma H, Zhao D, Yang Y, Liu M, Mohammed A, Zhao C, Yang Y, Xie J, Ding C, Ma X, Weng J, Gao Y, He H, Jin T. Biochemical characterization of SARS-CoV-2 nucleocapsid protein. Biochem Biophys Res Commun. 2020;527:618–23.
Chang CK, Hou MH, Chang CF, Hsiao CD, Huang TH. The SARS coronavirus nucleocapsid protein–forms and functions. Antiviral Res. 2014;103:39–50.
Cong Y, Ulasli M, Schepers H, Mauthe M, V’kovski P, Kriegenburg F, Thiel V, de Haan CAM, Reggiori F. Nucleocapsid Protein Recruitment to replication-transcription complexes plays a crucial role in Coronaviral Life Cycle. J Virol. 2020;94:e01925–01919.
Sheikh A, Al-Taher A, Al-Nazawi M, Al-Mubarak AI, Kandeel M. Analysis of preferred codon usage in the coronavirus N genes and their implications for genome evolution and vaccine design. J Virol Methods. 2020;277:113806.
Leung DT, Tam FC, Ma CH, Chan PK, Cheung JL, Niu H, Tam JS, Lim PL. Antibody response of patients with severe acute respiratory syndrome (SARS) targets the viral nucleocapsid. J Infect Dis. 2004;190:379–86.
Tan YJ, Goh PY, Fielding BC, Shen S, Chou CF, Fu JL, Leong HN, Leo YS, Ooi EE, Ling AE, Lim SG, Hong W. Profiles of antibody responses against severe acute respiratory syndrome coronavirus recombinant proteins and their potential use as diagnostic markers. Clin Diagn Lab Immunol. 2004;11:362–71.
Shi Y, Yi Y, Li P, Kuang T, Li L, Dong M, Ma Q, Cao C. Diagnosis of severe acute respiratory syndrome (SARS) by detection of SARS coronavirus nucleocapsid antibodies in an antigen-capturing enzyme-linked immunosorbent assay. J Clin Microbiol. 2003;41:5781–2.
Dutta NK, Mazumdar K, Gordy JT. The nucleocapsid protein of SARS–CoV-2: a target for Vaccine Development. J Virol. 2020;94:e00647–00620.
Kang S, Yang M, Hong Z, Zhang L, Huang Z, Chen X, He S, Zhou Z, Zhou Z, Chen Q, Yan Y, Zhang C, Shan H, Chen S. (2020) Crystal structure of SARS-CoV-2 nucleocapsid protein RNA binding domain reveals potential unique drug targeting sites. bioRxiv:2020.2003.2006.977876.
Schoeman D, Fielding BC. Coronavirus envelope protein: current knowledge. Virol J. 2019;16:69.
Ruch TR, Machamer CE. The coronavirus E protein: assembly and beyond. Viruses. 2012;4:363–82.
Li Y, Surya W, Claudine S, Torres J. Structure of a conserved golgi complex-targeting signal in coronavirus envelope proteins. J Biol Chem. 2014;289:12535–49.
Torres J, Parthasarathy K, Lin X, Saravanan R, Kukol A, Liu DX. Model of a putative pore: the pentameric alpha-helical bundle of SARS coronavirus E protein in lipid bilayers. Biophys J. 2006;91:938–47.
Teoh KT, Siu YL, Chan WL, Schlüter MA, Liu CJ, Peiris JS, Bruzzone R, Margolis B, Nal B. The SARS coronavirus E protein interacts with PALS1 and alters tight junction formation and epithelial morphogenesis. Mol Biol Cell. 2010;21:3838–52.
Kuo L, Hurst KR, Masters PS. Exceptional flexibility in the sequence requirements for coronavirus small envelope protein function. J Virol. 2007;81:2249–62.
Boscarino JA, Logan HL, Lacny JJ, Gallagher TM. Envelope protein palmitoylations are crucial for murine coronavirus assembly. J Virol. 2008;82:2989–99.
Boson B, Legros V, Zhou B, Siret E, Mathieu C, Cosset FL, Lavillette D, Denolly S. The SARS-CoV-2 envelope and membrane proteins modulate maturation and retention of the spike protein, allowing assembly of virus-like particles. J Biol Chem; 2020.
Siu YL, Teoh KT, Lo J, Chan CM, Kien F, Escriou N, Tsao SW, Nicholls JM, Altmeyer R, Peiris JS, Bruzzone R, Nal B. The M, E, and N structural proteins of the severe acute respiratory syndrome coronavirus are required for efficient assembly, trafficking, and release of virus-like particles. J Virol. 2008;82:11318–30.
Ruch TR, Machamer CE. The hydrophobic domain of infectious bronchitis virus E protein alters the host secretory pathway and is important for release of infectious virus. J Virol. 2011;85:675–85.
Jimenez-Guardeño JM, Nieto-Torres JL, DeDiego ML, Regla-Nava JA, Fernandez-Delgado R, Castaño-Rodriguez C, Enjuanes L. The PDZ-binding motif of severe acute respiratory syndrome coronavirus envelope protein is a determinant of viral pathogenesis. PLoS Pathog. 2014;10:e1004320.
Yang Y, Xiong Z, Zhang S, Yan Y, Nguyen J, Ng B, Lu H, Brendese J, Yang F, Wang H, Yang XF. Bcl-xL inhibits T-cell apoptosis induced by expression of SARS coronavirus E protein in the absence of growth factors. Biochem J. 2005;392:135–43.
Masters PS. The molecular biology of coronaviruses. Adv Virus Res. 2006;66:193–292.
Ziebuhr J, Snijder EJ, Gorbalenya AE. Virus-encoded proteinases and proteolytic processing in the Nidovirales. J Gen Virol. 2000;81:853–79.
Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. Addendum: a pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;588:E6.
Ren L, Zhang Y, Li J, Xiao Y, Zhang J, Wang Y, Chen L, Paranhos-Baccala G, Wang J. Genetic drift of human coronavirus OC43 spike gene during adaptive evolution. Sci Rep. 2015;5:11451.
Chibo D, Birch C. Analysis of human coronavirus 229E spike and nucleoprotein genes demonstrates genetic drift between chronologically distinct strains. J Gen Virol. 2006;87:1203–8.
Song HD, Tu CC, Zhang GW, Wang SY, Zheng K, Lei LC, Chen QX, Gao YW, Zhou HQ, Xiang H, Zheng HJ, Chern SW, Cheng F, Pan CM, Xuan H, Chen SJ, Luo HM, Zhou DH, Liu YF, He JF, Qin PZ, Li LH, Ren YQ, Liang WJ, Yu YD, Anderson L, Wang M, Xu RH, Wu XW, Zheng HY, Chen JD, Liang G, Gao Y, Liao M, Fang L, Jiang LY, Li H, Chen F, Di B, He LJ, Lin JY, Tong S, Kong X, Du L, Hao P, Tang H, Bernini A, Yu XJ, Spiga O, Guo ZM, Pan HY, He WZ, Manuguerra JC, Fontanet A, Danchin A, Niccolai N, Li YX, Wu CI, Zhao GP. Cross-host evolution of severe acute respiratory syndrome coronavirus in palm civet and human. Proc Natl Acad Sci U S A. 2005;102:2430–5.
Guan Y, Zheng BJ, He YQ, Liu XL, Zhuang ZX, Cheung CL, Luo SW, Li PH, Zhang LJ, Guan YJ, Butt KM, Wong KL, Chan KW, Lim W, Shortridge KF, Yuen KY, Peiris JS, Poon LL. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science. 2003;302:276–8.
Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, Hengartner N, Giorgi EE, Bhattacharya T, Foley B, Hastie KM, Parker MD, Partridge DG, Evans CM, Freeman TM, de Silva TI, Sheffield C-GG, McDanal C, Perez LG, Tang H, Moon-Walker A, Whelan SP, LaBranche CC, Saphire EO, Montefiori DC. Tracking changes in SARS-CoV-2 spike: evidence that D614G increases infectivity of the COVID-19 Virus. Cell. 2020;182:812–27. e819.
Nechipurenko YD, Anashkina AA, Matveeva OV. Change of antigenic determinants of SARS-CoV-2 Virus S-Protein as a possible cause of antibody-dependent enhancement of virus infection and cytokine storm. Biophys (Oxf). 2020;65:703–9.
Rambaut A, Holmes EC, O’Toole A, Hill V, McCrone JT, Ruis C, du Plessis L, Pybus OG. A dynamic nomenclature proposal for SARS-CoV-2 lineages to assist genomic epidemiology. Nat Microbiol. 2020;5:1403–7.
Tang X, Wu C, Li X, Song Y, Yao X, Wu X, Duan Y, Zhang H, Wang Y, Qian Z, Cui J, Lu J. On the origin and continuing evolution of SARS-CoV-2. Natl Sci Rev. 2020;7:1012–23.
Rambaut A, Holmes EC, O’Toole Á, Hill V, McCrone JT, Ruis C, du Plessis L, Pybus OG. A dynamic nomenclature proposal for SARS-CoV-2 lineages to assist genomic epidemiology. Nat Microbiol. 2020;5:1403–7.
Mercatelli D, Giorgi FM. Geographic and genomic distribution of SARS-CoV-2 mutations. Front Microbiol. 2020;11:1800.
Forster P, Forster L, Renfrew C, Forster M. Phylogenetic network analysis of SARS-CoV-2 genomes. Proc Natl Acad Sci U S A. 2020;117:9241–3.
Shen S, Zhang Z, He F. (2020) The phylogenetic relationship within SARS-CoV-2s: an expanding basal clade. Mol Phylogenet Evol:107017.
Wang R, Chen J, Gao K, Hozumi Y, Yin C, Wei G-W. Analysis of SARS-CoV-2 mutations in the United States suggests presence of four substrains and novel variants. Commun Biology. 2021;4:228.
Guruprasad L. (2021) Human SARS CoV-2 spike protein mutations. Proteins.
Becerra-Flores M, Cardozo T. SARS-CoV-2 viral spike G614 mutation exhibits higher case fatality rate. Int J Clin Pract. 2020;74:e13525.
Plante JA, Liu Y, Liu J, Xia H, Johnson BA, Lokugamage KG, Zhang X, Muruato AE, Zou J, Fontes-Garfias CR, Mirchandani D, Scharton D, Bilello JP, Ku Z, An Z, Kalveram B, Freiberg AN, Menachery VD, Xie X, Plante KS, Weaver SC, Shi PY. (2020) Spike mutation D614G alters SARS-CoV-2 fitness. Nature.
Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, Hengartner N, Giorgi EE, Bhattacharya T, Foley B, Hastie KM, Parker MD, Partridge DG, Evans CM, Freeman TM, de Silva TI, McDanal C, Perez LG, Tang H, Moon-Walker A, Whelan SP, LaBranche CC, Saphire EO, Montefiori DC. Tracking changes in SARS-CoV-2 spike: evidence that D614G increases infectivity of the COVID-19 Virus. Cell. 2020;182:812–e827819.
Castillo AE, Parra B, Tapia P, Lagos J, Arata L, Acevedo A, Andrade W, Leal G, Tambley C, Bustos P, Fasce R, Fernández J. Geographical distribution of genetic variants and lineages of SARS-CoV-2 in Chile. Front Public Health. 2020;8:562615.
Chong YM, Sam IC, Chong J, Kahar Bador M, Ponnampalavanar S, Syed Omar SF, Kamarulzaman A, Munusamy V, Wong CK, Jamaluddin FH, Chan YF. SARS-CoV-2 lineage B.6 was the major contributor to early pandemic transmission in Malaysia. PLoS Negl Trop Dis. 2020;14:e0008744.
Phan T. Genetic diversity and evolution of SARS-CoV-2. Infect Genet Evol. 2020;81:104260–104260.
Carabelli AM, Peacock TP, Thorne LG, Harvey WT, Hughes J, Robertson DL. (2023) SARS-CoV-2 variant biology: immune escape, transmission and fitness. Nat Rev Microbiol, 21(3): 162–177.
Wu H, Xing N, Meng K, Fu B, Xue W, Dong P, Zhu Z. Nucleocapsid mutations R203K/G204R increase the infectivity, fitness, and virulence of SARS-CoV-2. Cell Host Microbe. 2021;29(12):1788–801.
Johnson BA, Zhou Y, Lokugamage KG, Vu MN, Bopp N, Crocquet-Valdes PA, Menachery VD. Nucleocapsid mutations in SARS-CoV-2 augment replication and pathogenesis. PLoS Pathog. 2022;18(6):e1010627.
Mou K, Abdalla M, Wei DQ, Khan MT, Lodhi MS, Darwish DB, Tu X. Emerging mutations in envelope protein of SARS-CoV-2 and their effect on thermodynamic properties. IMU. 2021;25:100675.
Abavisani M, Rahimian K, Mahdavi B, Tokhanbigli S, Mollapour Siasakht M, Farhadi A, Meshkat Z. Mutations in SARS-CoV-2 structural proteins: a global analysis. Virol J. 2022;19(1):1–19.
Syed AM, Ciling A, Taha TY, Chen IP, Khalid MM, Sreekumar B, Doudna JA. Omicron mutations enhance infectivity and reduce antibody neutralization of SARS-CoV-2 virus-like particles. PNAS. 2022;119(31):e2200592119.
Fujino T, Nomoto H, Kutsuna S, Ujiie M, Suzuki T, Sato R, Fujimoto T, Kuroda M, Wakita T, Ohmagari N. (2021) Novel SARS-CoV-2 variant identified in travelers from Brazil to Japan. Emerg Infect Dis 27.
Tegally H, Wilkinson E, Giovanetti M, Iranzadeh A, Fonseca V, Giandhari J, Doolabh D, Pillay S, San EJ, Msomi N, Mlisana K, von Gottberg A, Walaza S, Allam M, Ismail A, Mohale T, Glass AJ, Engelbrecht S, Van Zyl G, Preiser W, Petruccione F, Sigal A, Hardie D, Marais G, Hsiao M, Korsman S, Davies M-A, Tyers L, Mudau I, York D, Maslo C, Goedhals D, Abrahams S, Laguda-Akingba O, Alisoltani-Dehkordi A, Godzik A, Wibmer CK, Sewell BT, Lourenço J, Alcantara LCJ, Pond SLK, Weaver S, Martin D, Lessells RJ, Bhiman JN, Williamson C, de Oliveira T. (2020) Emergence and rapid spread of a new severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) lineage with multiple spike mutations in South Africa. medRxiv:2020.2012.2021.20248640.
O’Toole Á, Hill V, Pybus OG, Watts A, Bogoch II, Khan K, Messina JP, Tegally H, Lessells RR, Giandhari J, Pillay S, Tumedi KA, Nyepetsi G, Kebabonye M, Matsheka M, Mine M, Tokajian S, Hassan H, Salloum T, Merhi G, Koweyes J, Geoghegan JL, de Ligt J, Ren X, Storey M, Freed NE, Pattabiraman C, Prasad P, Desai AS, Vasanthapuram R, Schulz TF, Steinbrück L, Stadler T, Parisi A, Bianco A, de García D, Buenestado-Serrano S, Borges V, Isidro J, Duarte S, Gomes JP, Zuckerman NS, Mandelboim M, Mor O, Seemann T, Arnott A, Draper J, Gall M, Rawlinson W, Deveson I, Schlebusch S, McMahon J, Leong L, Lim CK, Chironna M, Loconsole D, Bal A, Josset L, Holmes E, St George K, Lasek-Nesselquist E, Sikkema RS, Oude Munnink B, Koopmans M, Brytting M, Sudha Rani V, Pavani S, Smura T, Heim A, Kurkela S, Umair M, Salman M, Bartolini B, Rueca M, Drosten C, Wolff T, Silander O, Eggink D, Reusken C, Vennema H, Park A, Carrington C, Sahadeo N, Carr M, Gonzalez G, de Oliveira T, Faria N, Rambaut A, Kraemer MUG. (2021) Tracking the international spread of SARS-CoV-2 lineages B.1.1.7 and B.1.351/501Y-V2. Wellcome open research 6:121.
Elbe S, Buckland-Merrett G. (2017) Data, disease and diplomacy: GISAID’s innovative contribution to global health. Global challenges (Hoboken, NJ) 1:33–46.
World Health Organization (WHO). (2022) Tracking SARS-CoV-2 Variants. https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/.
Galloway SE, Paul P, MacCannell DR, Johansson MA, Brooks JT, MacNeil A, Slayton RB, Tong S, Silk BJ, Armstrong GL, Biggerstaff M, Dugan VG. (2021) Emergence of SARS-CoV-2 B.1.1.7 Lineage - United States, December 29, 2020-January 12, 2021. MMWR Morbidity and mortality weekly report 70:95–99.
Wise J. Covid-19: New coronavirus variant is identified in UK. BMJ (Clinical Res ed). 2020;371:m4857.
Gröhs Ferrareze PA, Franceschi VB, de Menezes Mayer A, Caldana GD, Zimerman RA, Thompson CE. (2021) E484K as an innovative phylogenetic event for viral evolution: genomic analysis of the E484K spike mutation in SARS-CoV-2 lineages from Brazil. bioRxiv:2021.2001.2027.426895.
Maggi F, Novazzi F, Genoni A, Baj A, Spezia PG, Focosi D, Zago C, Colombo A, Cassani G, Pasciuta R, Tamborini A, Rossi A, Prestia M, Capuano R, Azzi L, Donadini A, Catanoso G, Grossi PA, Maffioli L, Bonelli G. (2021) Imported SARS-COV-2 variant P.1 detected in traveler returning from Brazil to Italy. Emerg Infect Dis 27.
Toovey OTR, Harvey KN, Bird PW, Tang JW-TW-T. (2021) Introduction of Brazilian SARS-CoV-2 484K.V2 related variants into the UK. The Journal of infection:S0163-4453(0121)00047– 00045.
Voloch CM, Silva F, de Rd LGP, Cardoso CC, Brustolini OJ, Gerber AL, Guimarães APC, Mariani D, Costa RMd, Ferreira OC, Cavalcanti AC, Frauches TS, de Mello CMB, Galliez RM, Faffe DS, Castiñeiras TMPP, Tanuri A, de Vasconcelos ATR. (2020) Genomic characterization of a novel SARS-CoV-2 lineage from Rio De Janeiro, Brazil. medRxiv:2020.2012.2023.20248598.
Barda N, Dagan N, Balicer RD. (2021) BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. Reply. N Engl J Med 384:1970.
Deng X, Garcia-Knight MA, Khalid MM, Servellita V, Wang C, Morris MK, Sotomayor-González A, Glasner DR, Reyes KR, Gliwa AS, Reddy NP, Sanchez San Martin C, Federman S, Cheng J, Balcerek J, Taylor J, Streithorst JA, Miller S, Sreekumar B, Chen PY, Schulze-Gahmen U, Taha TY, Hayashi JM, Simoneau CR, Kumar GR, McMahon S, Lidsky PV, Xiao Y, Hemarajata P, Green NM, Espinosa A, Kath C, Haw M, Bell J, Hacker JK, Hanson C, Wadford DA, Anaya C, Ferguson D, Frankino PA, Shivram H, Lareau LF, Wyman SK, Ott M, Andino R, Chiu CY. Transmission, infectivity, and neutralization of a spike L452R SARS-CoV-2 variant. Cell. 2021;184:3426–e34373428.
Starr TN, Greaney AJ, Addetia A, Hannon WW, Choudhary MC, Dingens AS, Li JZ, Bloom JD. Prospective mapping of viral mutations that escape antibodies used to treat COVID-19. Science. 2021;371:850–4.
Zhang W, Davis BD, Chen SS, Sincuir Martinez JM, Plummer JT, Vail E. Emergence of a Novel SARS-CoV-2 variant in Southern California. JAMA. 2021;325:1324–6.
Schubert K, Karousis ED, Jomaa A, Scaiola A, Echeverria B, Gurzeler L-A, Leibundgut M, Thiel V, Mühlemann O, Ban N. SARS-CoV-2 Nsp1 binds the ribosomal mRNA channel to inhibit translation. Nat Struct Mol Biol. 2020;27:959–66.
Yuan S, Peng L, Park JJ, Hu Y, Devarkar SC, Dong MB, Shen Q, Wu S, Chen S, Lomakin IB, Xiong Y. Nonstructural protein 1 of SARS-CoV-2 is a potent pathogenicity factor redirecting host protein synthesis Machinery toward viral RNA. Mol Cell. 2020;80:1055–e10661056.
Clark LK, Green TJ, Petit CM. Structure of nonstructural protein 1 from SARS-CoV-2. J Virol. 2021;95:e02019–02020.
Xia H, Cao Z, Xie X, Zhang X, Chen JY-C, Wang H, Menachery VD, Rajsbaum R, Shi P-Y. Evasion of type I Interferon by SARS-CoV-2. Cell Rep. 2020;33:108234–108234.
Thoms M, Buschauer R, Ameismeier M, Koepke L, Denk T, Hirschenberger M, Kratzat H, Hayn M, Mackens-Kiani T, Cheng J, Straub JH, Stürzel CM, Fröhlich T, Berninghausen O, Becker T, Kirchhoff F, Sparrer KMJ, Beckmann R. Structural basis for translational shutdown and immune evasion by the Nsp1 protein of SARS-CoV-2. Science. 2020;369:1249–55.
Davies JP, Almasy KM, McDonald EF, Plate L. (2020) Comparative multiplexed interactomics of SARS-CoV-2 and homologous coronavirus non-structural proteins identifies unique and shared host-cell dependencies. bioRxiv: the preprint server for biology:2020.2007.2013.201517.
Gordon DE, Jang GM, Bouhaddou M, Xu J, Obernier K, White KM, O’Meara MJ, Rezelj VV, Guo JZ, Swaney DL, Tummino TA, Hüttenhain R, Kaake RM, Richards AL, Tutuncuoglu B, Foussard H, Batra J, Haas K, Modak M, Kim M, Haas P, Polacco BJ, Braberg H, Fabius JM, Eckhardt M, Soucheray M, Bennett MJ, Cakir M, McGregor MJ, Li Q, Meyer B, Roesch F, Vallet T, Mac Kain A, Miorin L, Moreno E, Naing ZZC, Zhou Y, Peng S, Shi Y, Zhang Z, Shen W, Kirby IT, Melnyk JE, Chorba JS, Lou K, Dai SA, Barrio-Hernandez I, Memon D, Hernandez-Armenta C, Lyu J, Mathy CJP, Perica T, Pilla KB, Ganesan SJ, Saltzberg DJ, Rakesh R, Liu X, Rosenthal SB, Calviello L, Venkataramanan S, Liboy-Lugo J, Lin Y, Huang X-P, Liu Y, Wankowicz SA, Bohn M, Safari M, Ugur FS, Koh C, Savar NS, Tran QD, Shengjuler D, Fletcher SJ, O’Neal MC, Cai Y, Chang JCJ, Broadhurst DJ, Klippsten S, Sharp PP, Wenzell NA, Kuzuoglu-Ozturk D, Wang H-Y, Trenker R, Young JM, Cavero DA, Hiatt J, Roth TL, Rathore U, Subramanian A, Noack J, Hubert M, Stroud RM, Frankel AD, Rosenberg OS, Verba KA, Agard DA, Ott M, Emerman M, Jura N, von Zastrow M, Verdin E, Ashworth A, Schwartz O, d’Enfert C, Mukherjee S, Jacobson M, Malik HS, Fujimori DG, Ideker T, Craik CS, Floor SN, Fraser JS, Gross JD, Sali A, Roth BL, Ruggero D, Taunton J, Kortemme T, Beltrao P, Vignuzzi M, García-Sastre A, Shokat KM, Shoichet BK, Krogan NJ. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature. 2020;583:459–68.
Shin D, Mukherjee R, Grewe D, Bojkova D, Baek K, Bhattacharya A, Schulz L, Widera M, Mehdipour AR, Tascher G, Geurink PP, van der Wilhelm A, Ovaa H, Müller S, Knobeloch K-P, Rajalingam K, Schulman BA, Cinatl J, Hummer G, Ciesek S, Dikic I. (2020) Papain-like protease regulates SARS-CoV-2 viral spread and innate immunity. Nature 587:657–662.
Klemm T, Ebert G, Calleja DJ, Allison CC, Richardson LW, Bernardini JP, Lu BG, Kuchel NW, Grohmann C, Shibata Y, Gan ZY, Cooney JP, Doerflinger M, Au AE, Blackmore TR, van der Heden GJ, Geurink PP, Ovaa H, Newman J, Riboldi-Tunnicliffe A, Czabotar PE, Mitchell JP, Feltham R, Lechtenberg BC, Lowes KN, Dewson G, Pellegrini M, Lessene G, Komander D. Mechanism and inhibition of the papain-like protease, PLpro, of SARS-CoV-2. Embo j. 2020;39:e106275.
Armstrong LA, Lange SM, de Cesare V, Matthews SP, Nirujogi RS, Cole I, Hope A, Cunningham F, Toth R, Mukherjee R, Bojkova D, Gruber F, Gray D, Wyatt PG, Cinatl J, Dikic I, Davies P, Kulathu Y. (2020) Characterization of protease activity of Nsp3 from SARS-CoV-2 and its < em > in vitro inhibition by nanobodies. bioRxiv:2020.2012.2009.417741.
Wolff G, Limpens R, Zevenhoven-Dobbe JC, Laugks U, Zheng S, de Jong AWM, Koning RI, Agard DA, Grünewald K, Koster AJ, Snijder EJ, Bárcena M. A molecular pore spans the double membrane of the coronavirus replication organelle. Science. 2020;369:1395–8.
Claverie JM. (2020) A putative role of de-Mono-ADP-Ribosylation of STAT1 by the SARS-CoV-2 Nsp3 protein in the Cytokine Storm Syndrome of COVID-19. Viruses 12.
Frick DN, Virdi RS, Vuksanovic N, Dahal N, Silvaggi NR. Molecular basis for ADP-Ribose binding to the Mac1 domain of SARS-CoV-2 nsp3. Biochemistry. 2020;59:2608–15.
Virdi RS, Bavisotto RV, Hopper NC, Vuksanovic N, Melkonian TR, Silvaggi NR, Frick DN. (2020) Discovery of Drug-like ligands for the Mac1 domain of SARS-CoV-2 Nsp3. bioRxiv:2020.2007.2006.190413.
Alsaadi EAJ, Jones IM. Membrane binding proteins of coronaviruses. Future Virol. 2019;14:275–86.
Yoshimoto FK. The proteins of severe Acute Respiratory Syndrome Coronavirus-2 (SARS CoV-2 or n-COV19), the cause of COVID-19. Protein J. 2020;39:198–216.
Yanglin Q, Kai X. (2020) Functional studies of the coronavirus nonstructural proteins. STEMedicine 1.
Santerre M, Arjona SP, Allen CNS, Shcherbik N, Sawaya BE. Why do SARS-CoV-2 NSPs rush to the ER? Journal of Neurology; 2020.
Benvenuto D, Angeletti S, Giovanetti M, Bianchi M, Pascarella S, Cauda R, Ciccozzi M, Cassone A. Evolutionary analysis of SARS-CoV-2: how mutation of non-structural protein 6 (NSP6) could affect viral autophagy. J Infect. 2020;81:e24–7.
Shojaei S, Suresh M, Klionsky DJ, Labouta HI, Ghavami S. Autophagy and SARS-CoV-2 infection: a possible smart targeting of the autophagy pathway. Virulence. 2020;11:805–10.
Romano M, Ruggiero A, Squeglia F, Maga G, Berisio R. A structural view of SARS-CoV-2 RNA replication Machinery: RNA synthesis, proofreading and final Capping. Cells. 2020;9:1267.
Kirchdoerfer RN, Ward AB. Structure of the SARS-CoV nsp12 polymerase bound to nsp7 and nsp8 co-factors. Nat Commun. 2019;10:2342.
Peng Q, Peng R, Yuan B, Zhao J, Wang M, Wang X, Wang Q, Sun Y, Fan Z, Qi J, Gao GF, Shi Y. Structural and biochemical characterization of the nsp12-nsp7-nsp8 core polymerase complex from SARS-CoV-2. Cell Rep. 2020;31:107774.
Konkolova E, Klima M, Nencka R, Boura E. Structural analysis of the putative SARS-CoV-2 primase complex. J Struct Biol. 2020;211:107548–107548.
Littler DR, Gully BS, Colson RN, Rossjohn J. (2020) Crystal structure of the SARS-CoV-2 non-structural protein 9, Nsp9. bioRxiv:2020.2003.2028.013920.
Lin S, Chen H, Ye F, Chen Z, Yang F, Zheng Y, Cao Y, Qiao J, Yang S, Lu G. Crystal structure of SARS-CoV-2 nsp10/nsp16 2′-O-methylase and its implication on antiviral drug design. Signal Transduct Target Therapy. 2020;5:131.
Rosas-Lemus M, Minasov G, Shuvalova L, Inniss NL, Kiryukhina O, Wiersum G, Kim Y, Jedrzejczak R, Enders M, Jaroszewski L, Godzik A, Joachimiak A, Satchell KJF. (2020) The crystal structure of nsp10-nsp16 heterodimer from SARS-CoV-2 in complex with S-adenosylmethionine. bioRxiv:2020.2004.2017.047498.
Gadhave K, Kumar P, Kumar A, Bhardwaj T, Garg N, Giri R. (2020) NSP 11 of SARS-CoV-2 is an intrinsically disordered protein. bioRxiv:2020.2010.2007.330068.
Jia Z, Yan L, Ren Z, Wu L, Wang J, Guo J, Zheng L, Ming Z, Zhang L, Lou Z, Rao Z. Delicate structural coordination of the severe Acute Respiratory Syndrome coronavirus Nsp13 upon ATP hydrolysis. Nucleic Acids Res. 2019;47:6538–50.
Jang K-J, Jeong S, Kang DY, Sp N, Yang YM, Kim D-E. A high ATP concentration enhances the cooperative translocation of the SARS coronavirus helicase nsP13 in the unwinding of duplex RNA. Sci Rep. 2020;10:4481.
Shu T, Huang M, Wu D, Ren Y, Zhang X, Han Y, Mu J, Wang R, Qiu Y, Zhang DY, Zhou X. SARS-Coronavirus-2 Nsp13 possesses NTPase and RNA helicase activities that can be inhibited by Bismuth Salts. Virol Sin. 2020;35:321–9.
White MA, Lin W, Cheng X. Discovery of COVID-19 inhibitors targeting the SARS-CoV-2 Nsp13 helicase. J Phys Chem Lett. 2020;11:9144–51.
Yuen C-K, Lam J-Y, Wong W-M, Mak L-F, Wang X, Chu H, Cai J-P, Jin D-Y, To KK-W, Chan JF-W, Yuen K-Y, Kok K-H. SARS-CoV-2 nsp13, nsp14, nsp15 and orf6 function as potent interferon antagonists. Emerg Microbes Infections. 2020;9:1418–28.
Ogando NS, Zevenhoven-Dobbe JC, van der Meer Y, Bredenbeek PJ, Posthuma CC, Snijder EJ. The enzymatic activity of the nsp14 exoribonuclease is critical for replication of MERS-CoV and SARS-CoV-2. J Virol. 2020;94:e01246–01220.
Hackbart M, Deng X, Baker SC. Coronavirus endoribonuclease targets viral polyuridine sequences to evade activating host sensors. Proc Natl Acad Sci U S A. 2020;117:8094–103.
Kim Y, Jedrzejczak R, Maltseva NI, Wilamowski M, Endres M, Godzik A, Michalska K, Joachimiak A. Crystal structure of Nsp15 endoribonuclease NendoU from SARS-CoV-2. Protein Science: Publication Protein Soc. 2020;29:1596–605.
Senanayake SL. Overcoming nonstructural protein 15-nidoviral uridylate-specific endoribonuclease (nsp15/NendoU) activity of SARS-CoV-2. Future Drug Discovery. 2020;2:FDD42.
Baric RS. Emergence of a highly fit SARS-CoV-2 variant. N Engl J Med. 2020;383:2684–6.
Davies NG, Jarvis CI, Edmunds WJ, Jewell NP, Diaz-Ordaz K, Keogh RH. (2021) Increased hazard of death in community-tested cases of SARS-CoV-2 Variant of Concern 202012/01. medRxiv.
Nonaka CKV, Franco MM, Gräf T, de Lorenzo Barcia CA, de Ávila Mendonça RN, de Sousa KAF, Neiva LMC, Fosenca V, Mendes AVA, de Aguiar RS, Giovanetti M, de Freitas Souza BS. (2021) Genomic evidence of SARS-CoV-2 Reinfection Involving E484K Spike Mutation, Brazil. Emerg Infect Dis 27.
Funding
Not applicable.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
H.A.M.H.; S.M.F.; and S.S. performed the literature search, prepared the figures, and wrote the first draft. H.A.M.H.; A.A.T.; A.A.W.; A.M.E.; M.A.; M.E.A.H.; M.A.B.A.; A.M.A.M.; A.S.; M.A.E; M.M.A.; S.M.F.; and S.S. wrote the manuscript. All authors have read and agreed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals. For consent to participate, it is not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hussein, H.A.M., Thabet, A.A., Wardany, A.A. et al. SARS-CoV-2 outbreak: role of viral proteins and genomic diversity in virus infection and COVID-19 progression. Virol J 21, 75 (2024). https://doi.org/10.1186/s12985-024-02342-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-024-02342-w