Abstract
Background
The efficacy and safety of oncolytic virotherapies in the treatment of advanced melanoma still remains controversal. It is necessary to conduct quantitative evaluation on the basis of preclinical trial reports.
Methods
Publicly available databases (PubMed, Embase, Medline, Web of Science and Cochrane Library.) and register (Clinicaltrials.gov) were searched to collect treatment outcomes of oncolytic virotherapies (including herpes simplex virus type 1 (HSV), coxsackievirus A21 (CVA21), adenovirus, poxvirus and reovirus) for advanced/unresectable melanoma. Comparisons of treatment response, adverse events (AEs) and survival analyses for different virotherapies were performed by R software based on the extracted data from eligible studies.
Results
Finally, thirty-four eligible studies were analysed and HSV virotherapy had the highest average complete response (CR, 24.8%) and HSV had a slightly higher average overall response rate (ORR) than CVA21 (43.8% vs 42.6%). In the pooled results of comparing talimogene laherparepve (T-VEC) with or without GM-CSF/ICIs (immune checkpoint inhibitors) to GM-CSF/ICIs monotherapy suggested virotherapy was more efficient in subgroups CR (RR = 1.80, 95% CI [1.30; 2.51], P < 0.01), ORR (RR = 1.17, 95% CI [1.02; 1.34], P < 0.05), and DCR (RR = 1.27, 95% CI [1.15; 1.40], P < 0.01). In patients treated with T-VEC+ICIs, 2-year overall survival (12.1 ± 6.9 months) and progression-free survival (9.9 ± 6.9) were significantly longer than those treated with T-VEC alone. Furthermore, we found that AEs occurred frequently in virotherapy but decreased in a large cohort of enrolled patients, some of which, such as abdominal distension/pain, injection site pain and pruritus, were found to be positively associated with disease progression in patients treated with T-VEC monotherapy.
Conclusion
Given the relative safety and tolerability of oncolytic viruses, and the lack of reports of dose-limiting-dependent toxicities, more patients treated with T-VEC with or without ICIs should be added to future assessment analyses. There is still a long way to go before it can be used as a first-line therapy for patients with advanced or unresectable melanoma.
Similar content being viewed by others
Introduction
Patients with advanced melanoma had a poor prognosis with surgery and chemotherapy, until immune checkpoint inhibitors (ICIs) made breakthroughs in tumor regression and long-term durable cancer control [1,2,3]. However, occurrence of immune-related adverse events and a cold tumor microenvironment result in poor response and drug resistance over time [4]. Therefore, the induction of “cold tumors” into “hot tumors” has become the target of the next generation of antitumour therapy [5, 6]. Oncolytic viruses (OVs), which stimulate host antitumour immunity by preferentially replicating in tumor cells and forming a hot tumor environment, are a highly favorable tumor therapy strategy for patients with poor response to ICIs [7, 8]. Since virotherapy with talimogene laherparepvec (T-VEC) was approved for use in the United States and Europe, it has been explored in preclinical treatment studies for advanced/unresectable melanoma for nearly a decade [9,10,11]. Numerous clinical trials in advanced melanoma have evaluated the efficacy of T-VEC and other novel OVs (e.g. reovirus, poxvirus, etc.) in combination with immunosuppressants, including ipilimumab, nivolumab, and pembrolizumab [12,13,14]. There have been several reviews on the efficacy evaluation of virotherapy for advanced or metastatic melanoma [15,16,17], however, the quantitative evaluation of different oncolytic virotherapies has not been reported. Therefore, on the basis of data on treatment response, adverse events and survival, this study conducted a systematic meta-analysis to evaluate the efficacy and safety of different OVs and to promote our understanding of virotherapies in advanced melanoma.
Materials and methods
Searching strategies
We searched the following databases from January 1, 2000 to December 31, 2022: PubMed, Embase, Medline, Web of Science, Cochrane Library and online Clinicaltrials.gov. The keywords used in the search included “oncolytic virus”, “advanced/metastatic/unresectable melanoma”, “adverse event”, “overall survival”, “talimogene laherparepvec”, “herpesvirus”, “reovirus”, “coxsackievirus”, “poxvirus” and “adenovirus”. For example, the search formulas were ((oncolytic virus [Title/Abstract]) OR (talimogene laherparepvec) OR (poxvirus) OR (herpesvirus) OR (reovirus) OR (coxsackievirus)) AND ((advance melanoma [Title/Abstract]) OR (metastatic melanoma)), ((virotherapy [Title/Abstract]) AND (melanoma [Title/Abstract])) AND ((adverse event [Title/Abstract]) OR (overall survival [Title/Abstract])).
Inclusion and exclusion criteria
Inclusion criteria: (a) The recruited patients have unresectable, advanced or metastatic melanoma; (b) The virotherapies are limited to human herpes simplex virus type 1 (HSV), coxsackievirus A21 (CVA21), reovirus, adenovirus and poxvirus; (c) The treatment responses were assessed by the response evaluation criteria for solid tumors (RECIST), including complete response (CR), partial response (PR), stable disease (SD), progressive disease (PD) and adverse events (AEs) (optional); (d) The study types are limited to clinical trials, retrospective or randomized control trials (RCTs); (e) The study design described detailed treatment procedures.
Exclusion criteria: (a) Patients suffer from active cerebral, bone, or any more than 3 visceral metastases; (b) The recruited patients had an early stage (I-II) of the disease; (c) The recruited patients were younger than 18 years of age; (d) Data and results have been reported in previous studies; (e) Clinical trials are ongoing, and the results there are not yet available; (f) Animal studies and in vitro studies.
Data collection
Three staff members (CY.W, NX.L and L.Y) were independently involved in data extraction and rectification, including database retrieval, duplicate examination and treatment endpoint recording. Subsequently, full-text publications and registers were reviewed against eligibility criteria and differences were resolved by discussion and mutual consent with the two investigators (CY.W and NX.L). For eligible studies, the following were extracted independently by two researchers (NX.L and L.Y) using the same format table: name of first author, year of publication, age (mean/range) of enrolled patients, phase of clinical trial, treatment arms of study, viral family of OV, and administration of study drug. Survival data of enrolled patients could not be obtained directly from the original studies. Therefore, we used the Engauge Digitizer tool (version 12.1, https://github.com/markummitchell/engauge-digitizer) to digitize the overall survival (OS) and progression-free survival (PFS) curves provided in the publications. All curves were then redrawn and compared in the OS or PFS composite graphs.
Quality assessment
The quality assessment of RCTs was evaluated by two researchers (NX.L and Y.L) using the Cochrane Collaboration's tool [18], including seven items. Each item consists of three risk levels: low, high and unclear. Other studies were evaluated with 8 items of the scale of methodological index for non-randomized studies [19]. Details of the quality assessment results were attached to the Additional file 3.
Statistical analysis
All statistical analyses were conducted by R software (version 4.1.3, Copyright (C) 2022 The R Foundation for Statistical Computing). The combination method for single-sample proportions follows the guidance in the R package meta (version 5.2.0) described by Balduzzi [20]. The overall response rate (ORR) and disease control rate (DCR) were calculated based on the events of CR, PR and SD: ORR = CR+PR and DCR = ORR+SD. The relationship between treatment response and AEs was calculated by the Pearson correlation test. In single-arm studies, Freeman-Tukey Double arcsine transformation was used to polled an overall inverse-variance (IV). In binary data of some multi-arm studies, the IV method was used to combine and compare the estimated effect sizes. The risk ratio (RR) and P value less than 0.05 were used as the criteria of significance.
Results
Basic information of included studies
According to the flow diagram of databases and registers retrieval and screening described in PRISMA(2020) [21] (Additional file 1: Fig. S1). Finally, 21 clinical trials (Table 1) (4 of which did not provide publications [22,23,24,25]) and 10 other studies [13, 14, 26,27,28,29,30,31,32,33] were included in this analysis. Clinical trials of NCT02263508 [34, 35], NCT00769704 [36, 37] and NCT01740297 [38, 39] reported conclusions twice with different sample sizes until completion. Six of these clinical trials [40,41,42,43,44,45] did not post results on ClinicalTrials.org at the time of completion of this study (Table 1). A total of 2,710 patient records were used to assess the efficacy and safety of virotherapies.
Efficacy
Changes in response to virotherapies
Correlation test results showed that there were no significant changes in CR, PR, SD, PD, ORR, DCR or DRR from 2003 to 2022 (Fig. 1A). Meanwhile, their R values were all less than 0.3. Interestingly, the mean DCR values for virotherapies CVA21 and HSV were the same (62.2%), and the ORR of HSV was slightly greater than that of CVA21 (43.8% vs 42.6%) (Fig. 1B). Among the five kinds of oncolytic viruses, HSV had the highest mean CR (24.8%). For the endpoint of PD, the mean value of virotherapy for poxvirus was the highest (47.4%), followed by adenovirus (31.5%). In addition, the Wilcoxon-test was performed for difference in CR+PR (Fig. 1C) according to the phase and virotherapy of clinical trials. Significant results were found in phase II versus Ib (P = 0.031), HSV versus reovirus (P = 0.0036) and HSV versus poxvirus (P = 0.011). However, no significant difference was found when the same test method was performed for CR+PR+SD.
The comparison of therapeutic efficacy with oncolytic virotherapy in the treatment of advance melanoma in recent decades. A Changes of treatment response over time 2000 to 2022. The size of dots was weighted by the number of events. The local regression fitting line with 95% confidence region was drawn according to the changes of time (x) and ratio (y). B Comparison of the average treatment response in different oncolytic virotherapy. C Wilcoxon-test of changes in ORR grouped by clinical trials phase (left) and oncolytic virotherapy (right). (HSV Herpes simplex virus, CVA21 Coxsackievirus A21, CR Complete response, PR Partial response, SD Stable disease, PD Progressive disease, DCR Disease control rate, DRR Durable response rate, ORR Overall/objective response rate, AE Adverse effect, DCR = CR+PR+SD, ORR = CR+PR. Notes in Fig. 2B: Due to multiple studies have different observations and events. The sum of the proportions in a single pie chart does not equal to 100%.)
In the fixed model of different virotherapies (Additional file 2: Table S1), the ORR of HSV (IV = 0.18, 95% CI [0.16; 0.19]) and CVA21 (IV = 0.19, 95% CI [0.10; 0.30]) were nearly 3-, 9-, and 18-fold that of adenovirus (IV = 0.06; 95% CI [0.00; 0.22]), poxvirus (IV = 0.02; 95% CI [0.00; 0.14]) and reovirus (IV = 0.01; 95% CI [0.00; 0.04]), respectively.
In the pooled IV of the fixed model of HSV (T-VEC) and HSV+(T-VEC+ICIs) (Additional file 2: Table S2), the ORR of HSV (IV = 0.36, 95% CI [0.34; 0.39]) was lower than that of HSV+(IV = 0.43, 95% CI [0.39; 0.47]), while the CR of HSV (IV = 0.19, 95% CI [0.17; 0.21]) was higher than that of HSV+(IV = 0.15, 95% CI [0.12; 0.18]). There were no significant differences among the paired treatment response groups.
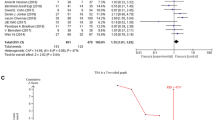
In the pooled IV of fixed model results from five studies [24, 34, 36,37,38], the two arms compared T-VEC with or without GM-CSF/ICIs to GM-CSF/ICIs monotherapy, suggesting that virotherapy is more efficient in the subgroups CR (RR = 1.80, 95% CI [1.30; 2.51], P < 0.01), ORR (RR = 1.17, 95% CI [1.02; 1.34], P < 0.05), DCR (RR = 1.27, 95% CI [1.15; 1.40], P < 0.01) and DRR (RR = 5.48, 95% CI [2.13; 14.05], P < 0.01) (Additional file 1: Fig. S2, Additional file 2: Table S3).
Survival
As shown in Fig. 2, in the combined Kaplan–Meier curves of OS or PFS, virotherapy with HSV showed the best therapeutic results. The mean OS at 1-year of HSV, CVA21, reovirus and adenovirus were 6.8 ± 3.6, 6.9 ± 3.4, 6.3 ± 4.0 and 4.8 ± 3.6 months, respectively. The corresponding mean proportions were 88.4 ± 9.2, 88.2 ± 8.0, 61.5 ± 26.7 and 65.1 ± 23.2. The mean OS at 2-year of HSV, CVA21, reovirus and adenovirus were 11.7 ± 6.8, 10.8 ± 6.2, 9.6 ± 6.4 and 9.2 ± 7.4 months, respectively. The corresponding mean proportions of them were 81.6 ± 14.2, 79.4 ± 14.4, 50.3 ± 29.7 and 55.2 ± 25.1, respectively. There was a significant difference (P < 0.001) in the results of the Wilcoxon-test between every two groups of them (top-right of Fig. 2A).
The combined Kaplan–Meier curves of OS or PFS plots. A, B. The comparison results of combined OS A and PFS B curves of different oncolytic virotherapies in included studies. C, D. The comparison results of HSV(T-VEC) and HSV + (T-VEC+ICIs) in OS C and PFS D, respectively. The Wilcoxon-test comparison results of 2-year median times were placed in the upper-right corner of each graph
The mean PFS at 1-year of HSV, CVA21 and reovirus were 5.6 ± 3.5, 6.0 ± 3.9 and 3.9 ± 3.4 months, respectively. The corresponding mean proportions of them were 69.8 ± 17.8, 58.5 ± 21.6 and 54.5 ± 28.1, respectively. The mean PFS at 2-year of HSV, CVA21 and reovirus were 9.9 ± 6.9, 9.6 ± 6.2 and 6.1 ± 6.1 months, respectively. The corresponding mean proportions of them were 62.3 ± 18.8, 43.5 ± 28.1 and 47.7 ± 30.5, respectively. There was a significant difference (P < 0.001) in the results of the Wilcoxon-test between every two groups of them (top-right of Fig. 2B).
In studies treated with T-VEC + ICIs (Fig. 2C, HSV +), the mean OS at 1-year was 6.9 ± 3.7 months and was not significantly longer than the 6.8 ± 3.6 months with T-VEC alone (P = 0.11). The mean OS at 2-year was 12.1 ± 6.9 months and was significantly longer than the 11.5 ± 6.8 months with T-VEC alone (P < 0.001). Similarly, there was no significant difference in PFS between HSV+ and HSV at 1-year (P = 0.09), while there was a significant difference in PFS at 2-year (P = 0.006) (Fig. 2D).
Safety
In addition to the difference in efficacy of different virotherapies, AEs are one of the major factors leading to treatment ineffectiveness. Although AEs frequently occur in virotherapy, their incidence is reduced in a large cohort of enrolled patients (Fig. 3A, R = − 0.32, P < 0.001). The heatmap in Fig. 3B shows the most common AE frequencies for each virotherapy. The top six most common AEs were fatigue, chills, nausea, diarrhoea, headache and myalgia. All types of AEs were detailed in supplementary Figure S3 (Additional file 1). For the top six AEs in the T-VEC group compared with the control group (Additional file 1: Fig. S4, Additional file 2: Table S4), the RR of fatigue was 1.44 (95% CI [1.24; 1.66], P < 0.01), the RR of chills was 5.78 (95% CI [4.06; 8.23], P < 0.01), the RR of nausea was 1.59 (95% CI [1.30; 1.94], P < 0.01), the RR of headache was 1.57 (95% CI [1.22; 2.02], P < 0.01) and the RR of myalgia was 2.48 (95% CI [1.62; 3.81], P < 0.01). As shown in Fig. 3C, most AEs occurred in general disorders, gastrointestinal disorders, and musculoskeletal and connective tissue disorders.
Incidence and frequency of (serious) adverse events of virotherapies. A, D. Trends in the incidence of common A or serious D adverse events. The size of dots was weighted by the square root of number of events. The local regression fitting line with 95% confidence region in the main scatter plot was drawn according to the changes of incidence (x) and total recruitment (y), while in the subplot (upper-right) was drawn according to the changes of incidence (x) and total events (y). B, E. Distribution of frequently common (B) or serious (E) adverse events in the five kinds of virotherapies. The complete distribution results were attached to supplementary figures S3 and S6, respectively. C, F. Weighted ratios of common (C) or serious (F) adverse events in different organ-system
However, there was no significant difference between the T-VEC and control groups in serious adverse events (SAEs), such as anaemia, pyrexia, sepsis, dyspnoea, pneumonia and abdominal distension/pain (Additional file 1: Figure S5, Additional file 2: Table S4). In addition, the incidence of SAEs decreased dramatically as the number of enrolled patients increased (Fig. 3D, R = − 0.75, P < 0.01). The heatmap in Fig. 3E shows the most common SAE frequencies for each virotherapy. Most SAEs occurred in neoplasms, general disorders, and infections and infestations (Fig. 3F). All types of SAEs were detailed in supplementary Figure S6 (Additional file 1).
Efficacy and safety
The association between efficacy and safety of T-VEC monotherapy or T-VEC+ICIs was showed in Fig. 4A. In T-VEC monotherapy, abdominal distension/pain, injection site pain and pruritus were significantly positively correlated with PD, and decreased appetite was significantly positively correlated with ORR. In T-VEC+ICIs therapy, chill was significantly positively correlated with CR but negatively correlated with DCR.
Association between treatment responses and adverse events (AEs). A. Correlation test between treatment responses and 30 common AEs for treatments T-VEC and T-VEC+ICIs. B. Correlation test between treatment responses and organ-system classification of AEs for treatments T-VEC and T-VEC+ICIs. The positive and negative correlation coefficients are represented by red and blue saturated colors, respectively. The size of the square responds to the strength of correlation between 0 and 1. (DRR Durable response rate, SD Stable disease. CR Complete response, PR Partial response, PD Progression disease, DCR Disease control rate, ORR Overall response rate, ICIs Immune checkpoint inhibitors. * < 0.05, ** < 0.01, *** < 0.001)
In the organ-system classification of AEs treated with T-VEC (Fig. 4B), blood and lymphatic system disorders, skin and subcutaneous tissue disorders were significantly negatively correlated with CR and ORR. Gastrointestinal disorders, general disorders, infections and infestations, nervous system disorders, vascular disorders, ear and labyrinth disorders, and investigations were significantly positively correlated with PD. In treatment with T-VEC+ICIs, respiratory, thoracic and mediastinal disorders, musculoskeletal and connective tissue disorders, and nervous system disorders were significantly positively correlated with SD but were significantly negatively correlated with PR. General disorders were significantly positively correlated with CR and negatively correlated with DCR.
Discussion
In this study, 34 studies including 2,710 records were used for the first time to evaluate the efficacy and safety of five oncolytic viruses in the treatment of advanced melanoma. Patients treated with HSV and CVA21 showed similar high efficacy in terms of DCR and ORR, while other virotherapies showed poorer outcomes. Compared with other virotherapies, HSV treatment significantly extended OS and PFS. In particular, patients treated with T-VEC+ICIs had significantly longer OS and PFS than those treated with T-VEC monotherapy. Therefore, encoding the blockade function of ICIs into OVs will be more effective than combination therapy, which has achieved significant efficacy in preclinical models [51, 52].
Cancer therapy has entered a new era since the discovery of the oncolytic potential of viruses such as T-VEC, a human herpes simplex virus type 1, which is modified to selectively replicate and secrete human granulocyte–macrophage colony-stimulating factor (GM-CSF) in tumor cells, resulting in activation of the immune response and killing of the infected target [53]. This property limits antitumour effects within the tumor microenvironment and avoids ineffective treatment due to drug resistance to ICIs and the restrictiveness of gene mutations [2, 54]. For example, in an open-label, multicentre study of patients with BRAF mutated metastatic melanoma treated with vemurafenib, only 90 (3.3%) patients endured CR, and 829 (30.6%) patients endured PR [55]. While in a randomized study of advanced melanoma patients treated with T-VEC, patients with mutant BRAF occurred CR in 5 (10.9%) and PR in 9 (19.6%) patients, and patients with wild-type BRAF occurred CR in 5 (11.1%) and PR in 9 (20.0%) patients [36]. In another phase II, open-label, multicentre study of T-VEC in patients with stage IIIB-IVM1c melanoma, the ORR of mutant BRAF was 10 (25%) patients, and that of wild-type BRAF was 20 (29%) patients [9].
Treatment response is a double-edged sword. To some extent, a high treatment response corresponds to more AEs, especially high-dose-dependent AEs, which may lead to cancer treatment termination and failure. In this study, treatment-related AEs such as nausea, fatigue and myalgia were more common in patients treated with T-VEC (+ ICIs) than GM-CSF/ICIs. In the randomized phase III trial OPTiM [36] included in this study, the ORR of T-VEC monotherapy (31.5%) was higher than that of GM-CSF (6.4%) alone, and AEs occurred in 11.3% of patients treated with T-VEC and 4.7% of patients treated with GM-CSF. In another randomized, double-blind phase III trial, MASTERKEY-265 [35], the ORR of combination therapy T-VEC+ pembrolizumab (48.6%) was higher than that of placebo+pembrolizumab (41.3%). Meanwhile, the incidence of grade > 3 treatment-related AEs was 20.3% and 15.7%, respectively, and the incidence of fatal AEs was 13.1% and 12.2%, respectively. Furthermore, no dose-limiting toxicity of T-VEC has been reported in advanced melanoma. The safety and tolerability of T-VEC make it a good treatment option for patients with advanced or unresectable melanoma and those unable to tolerate other treatment toxicities.
Prolonging (progression-free) survival is the primary goal of treatment for patients with advanced melanoma. In current study, T-VEC with or without ICIs had a significantly longer OS at 2-year than other types of OVs, and T-VEC+ICIs was superior to T-VEC alone. This superior outcome was also observed in 2-year PFS for T-VEC+ICIs compared to other OVs, but there was no significant superiority to T-VEC alone at 1-year. Interestingly, in two randomized phase III trials, OPTiM [36] and MASTERKEY-265 [35], no significant difference in OS/PFS was found in T-VEC versus GM-CSF and T-VEC+pembrolizumab versus placebo+pembrolizumab. In the OS of the OPTiM study, T-VEC was found to be superior to GM-CSF only after the removal of 18 patients who had not received allocated therapy, and patients treated with T-VEC as first-line therapy were superior to those treated with T-VEC as second-line therapy. In the staging subsets, T-VEC was superior to GM-CSF in patients with IIIB-IVM1a but not in patients with IVMIb/c.
Although virotherapy appears to be more effective in treating advanced melanoma, there are still some factors that need to be considered before a leap in efficacy can be made. Differences in viral injection volume and the time to peak may result in a delay in the initial response, making it difficult to distinguish false responses from true responses and to decide whether to continue treatment [56]. Furthermore, there is evidence that truly responsive tumors have a “mimicry” of presence with persistent pigmentation, which is in fact an inflammatory infiltrate enriched in melanophages, with no viable tumor cells remaining [57]. This will result in melanoma-specific markers and tissue staining that make it difficult to distinguish between true and false tumor tissue, adversely affecting the manipulation and injection of technicians and affecting viral transmission and optimal tumor perfusion [58]. The host's ability to defend against the virus and the presence of antibodies that neutralize the virus are potential mechanisms of resistance and a robust immune response elicited by the virus that may clear the virus, thereby limiting the activity of virotherapy [59].
The limitation of this study is that injection methods (such as intratumoral and intravenous) may contribute to the heterogeneity in efficacy assessment. The lack of data on patients who withdrew or changed treatment due to AEs may have influenced the results of this study. More studies of other rarely used virotherapies (such as CVA21) need to be included in future updated assessments.
Conclusion
Considering the relative safety and tolerability of OVs and the absence of reports of dose-limiting-dependent toxicities, more patients treated with T-VEC with or without ICIs should be added to future assessment analyses. There is still a long way to go before it can be used as a first-line therapy for patients with advanced or unresectable melanoma.
Availability of data and materials
The data sets that support the conclusions of this article are included within the article and the included publications and registered trials.
Abbreviations
- HSV:
-
Herpes simplex virus
- CVA21:
-
Coxsackievirus A21
- CR:
-
Complete response
- PR:
-
Partial response
- SD:
-
Stable disease
- PD:
-
Progressive disease
- DCR:
-
Disease control rate
- DRR:
-
Durable response rate
- ORR:
-
Overall/objective response rate
- AE:
-
Adverse effect
- DCR:
-
CR+PR+SD
- ORR:
-
CR+PR
- T-VEC:
-
Talimogene laherparepvec
- GM-CSF:
-
Granulocyte macrophage colony-stimulating factor
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- AE:
-
Adverse events
- PFU:
-
Plaque forming units
References
Galluzzi L, Humeau J, Buqué A, Zitvogel L, Kroemer G. Immunostimulation with chemotherapy in the era of immune checkpoint inhibitors. Nat Rev Clin Oncol. 2020;17:725–41. https://doi.org/10.1038/s41571-020-0413-z.
Carlino MS, Larkin J, Long GV. Immune checkpoint inhibitors in melanoma. The Lancet. 2021;398:1002–14. https://doi.org/10.1016/S0140-6736(21)01206-X.
Bagchi S, Yuan R, Engleman EG. Immune checkpoint inhibitors for the treatment of cancer: clinical impact and mechanisms of response and resistance. Annu Rev Pathol. 2021;16:223–49. https://doi.org/10.1146/annurev-pathol-042020-042741.
Duan Q, Zhang H, Zheng J, Zhang L. Turning cold into hot: firing up the tumor microenvironment. Trends Cancer. 2020;6:605–18. https://doi.org/10.1016/j.trecan.2020.02.022.
Dummer R, Ascierto PA, Gogas HJ, Arance A, Mandala M, Liszkay G, et al. Encorafenib plus binimetinib versus vemurafenib or encorafenib in patients with BRAF -mutant melanoma (COLUMBUS): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2018;19:603–15. https://doi.org/10.1016/S1470-2045(18)30142-6.
Long GV, Dummer R, Hamid O, Gajewski TF, Caglevic C, Dalle S, et al. Epacadostat plus pembrolizumab versus placebo plus pembrolizumab in patients with unresectable or metastatic melanoma (ECHO-301/KEYNOTE-252): a phase 3, randomised, double-blind study. Lancet Oncol. 2019;20:1083–97. https://doi.org/10.1016/S1470-2045(19)30274-8.
Ylösmäki E, Cerullo V. Design and application of oncolytic viruses for cancer immunotherapy. Curr Opin Biotech. 2020;65:25–36. https://doi.org/10.1016/j.copbio.2019.11.016.
Tian Y, Xie D, Yang L. Engineering strategies to enhance oncolytic viruses in cancer immunotherapy. Signal Transduct Target Ther. 2022;7:117. https://doi.org/10.1038/s41392-022-00951-x.
Malvehy J, Samoylenko I, Schadendorf D, Gutzmer R, Grob J, Sacco JJ, et al. Talimogene laherparepvec upregulates immune-cell populations in non-injected lesions: findings from a phase II, multicenter, open-label study in patients with stage IIIB–IVM1c melanoma. J Immunother Cancer. 2021;9:e1621. https://doi.org/10.1136/jitc-2020-001621.
Dummer R, Gyorki DE, Hyngstrom J, Berger AC, Conry R, Demidov L, et al. Neoadjuvant talimogene laherparepvec plus surgery versus surgery alone for resectable stage IIIB–IVM1a melanoma: a randomized, open-label, phase 2 trial. NAT MED. 2021;27:1789–96. https://doi.org/10.1038/s41591-021-01510-7.
Andtbacka RHI, Amatruda T, Nemunaitis J, Zager JS, Walker J, Chesney JA, et al. Biodistribution, shedding, and transmissibility of the oncolytic virus talimogene laherparepvec in patients with melanoma. EBioMedicine. 2019;47:89–97. https://doi.org/10.1016/j.ebiom.2019.07.066.
Shoushtari AN, Olszanski AJ, Nyakas M, Hornyak TJ, Wolchok JD, Levitsky V, et al. Pilot study of ONCOS-102 and pembrolizumab: remodeling of the tumor microenvironment and clinical outcomes in anti–PD-1–resistant advanced melanoma. Clin Cancer Res. 2022. https://doi.org/10.1158/1078-0432.CCR-22-2046.
Mahalingam D, Fountzilas C, Moseley J, Noronha N, Tran H, Chakrabarty R, et al. A phase II study of REOLYSIN® (pelareorep) in combination with carboplatin and paclitaxel for patients with advanced malignant melanoma. Cancer Chemoth Pharm. 2017;79:697–703. https://doi.org/10.1007/s00280-017-3260-6.
Hwang T, Moon A, Burke J, Ribas A, Stephenson J, Breitbach CJ, et al. A mechanistic proof-of-concept clinical trial with JX-594, a targeted multi-mechanistic oncolytic poxvirus, in patients with metastatic melanoma. Mol Ther. 2011;19:1913–22. https://doi.org/10.1038/mt.2011.132.
Trager MH, Geskin LJ, Saenger YM. Oncolytic viruses for the treatment of metastatic melanoma. Curr Treat Option On. 2020;21:26. https://doi.org/10.1007/s11864-020-0718-2.
Bayan CY, Lopez AT, Gartrell RD, Komatsubara KM, Bogardus M, Rao N, et al. The role of oncolytic viruses in the treatment of melanoma. Curr Oncol Rep. 2018;20:80. https://doi.org/10.1007/s11912-018-0729-3.
LaRocca CJ, Warner SG. Oncolytic viruses and checkpoint inhibitors: combination therapy in clinical trials. Clin Transl Med. 2018;7:35. https://doi.org/10.1186/s40169-018-0214-5.
Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–6. https://doi.org/10.1046/j.1445-2197.2003.02748.x.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evidence Based Mental Health. 2019;22:153–60. https://doi.org/10.1136/ebmental-2019-300117.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178–89. https://doi.org/10.1016/j.jclinepi.2021.03.001.
Neoadjuvant trial of nivolumab in combination with HF10 oncolytic viral therapy in resectable stage IIIB, IIIC, IVM1a Melanoma. (2022). https://clinicaltrials.gov/ct2/show/NCT03259425.
A study of talimogene laherparepvec in stage IIIc and stage IV malignant melanoma. (2015). https://clinicaltrials.gov/ct2/show/NCT00289016.
An extended use study of safety and efficacy of talimogene laherparepvec in melanoma. (2015). https://clinicaltrials.gov/ct2/show/NCT01368276.
Viral therapy in treating patients with metastatic melanoma. (2014). https://clinicaltrials.gov/ct2/show/NCT00651157.
Ressler JM, Karasek M, Koch L, Silmbrod R, Mangana J, Latifyan S, et al. Real-life use of talimogene laherparepvec (T-VEC) in melanoma patients in centers in Austria Switzerland and Germany. J Immunother Cancer. 2021;9:e1701. https://doi.org/10.1136/jitc-2020-001701.
Franke V, Berger DMS, Klop WMC, Hiel B, Wiel BA, Meulen S, et al. High response rates for T-VEC in early metastatic melanoma (stage IIIB/C-IVM1a). Int J Cancer. 2019;145:974–8. https://doi.org/10.1002/ijc.32172.
Louie RJ, Perez MC, Jajja MR, Sun J, Collichio F, Delman KA, et al. Real-world outcomes of talimogene laherparepvec therapy: a multi-institutional experience. J Am Coll Surg. 2019;228:644–9. https://doi.org/10.1016/j.jamcollsurg.2018.12.027.
Sun L, Funchain P, Song JM, Rayman P, Tannenbaum C, Ko J, et al. Talimogene laherparepvec combined with anti-PD-1 based immunotherapy for unresectable stage III-IV melanoma: a case series. J Immunother Cancer. 2018;6:36. https://doi.org/10.1186/s40425-018-0337-7.
Perez MC, Miura JT, Naqvi SMH, Kim Y, Holstein A, Lee D, et al. Talimogene laherparepvec (TVEC) for the treatment of advanced melanoma: a single-institution experience. Ann Surg Oncol. 2018;25:3960–5. https://doi.org/10.1245/s10434-018-6803-0.
Kaufman HL, Amatruda T, Reid T, Gonzalez R, Glaspy J, Whitman E, et al. Systemic versus local responses in melanoma patients treated with talimogene laherparepvec from a multi-institutional phase II study. J Immunother Cancer. 2016;4:12. https://doi.org/10.1186/s40425-016-0116-2.
Bramante S, Kaufmann JK, Veckman V, Liikanen I, Nettelbeck DM, Hemminki O, et al. Treatment of melanoma with a serotype 5/3 chimeric oncolytic adenovirus coding for GM-CSF: results in vitro, in rodents and in humans. Int J Cancer. 2015;137:1775–83. https://doi.org/10.1002/ijc.29536.
Senzer NN, Kaufman HL, Amatruda T, Nemunaitis M, Reid T, Daniels G, et al. Phase II clinical trial of a granulocyte-macrophage colony-stimulating factor-encoding, second-generation oncolytic herpesvirus in patients with unresectable metastatic melanoma. J Clin Oncol. 2009;27:5763–71. https://doi.org/10.1200/JCO.2009.24.3675.
Ribas A, Dummer R, Puzanov I, VanderWalde A, Andtbacka RHI, Michielin O, et al. Oncolytic virotherapy promotes intratumoral T cell infiltration and improves anti-PD-1 immunotherapy. Cell. 2017;170:1109–19. https://doi.org/10.1016/j.cell.2017.08.027.
Chesney JA, Ribas A, Long GV, Kirkwood JM, Dummer R, Puzanov I, et al. Randomized, double-blind, placebo-controlled, global phase III trial of talimogene laherparepvec combined with pembrolizumab for advanced melanoma. J Clin Oncol. 2022. https://doi.org/10.1200/JCO.22.00343.
Andtbacka RHI, Collichio F, Harrington KJ, Middleton MR, Downey G, Ӧhrling K, et al. Final analyses of OPTiM: a randomized phase III trial of talimogene laherparepvec versus granulocyte-macrophage colony-stimulating factor in unresectable stage III–IV melanoma. J Immunother Cancer. 2019;7:145. https://doi.org/10.1186/s40425-019-0623-z.
Andtbacka RHI, Agarwala SS, Ollila DW, Hallmeyer S, Milhem M, Amatruda T, et al. Cutaneous head and neck melanoma in OPTiM, a randomized phase 3 trial of talimogene laherparepvec versus granulocyte-macrophage colony-stimulating factor for the treatment of unresected stage IIIB/IIIC/IV melanoma. Head Neck. 2016;38:1752–8. https://doi.org/10.1002/hed.24522.
Chesney J, Puzanov I, Collichio F, Singh P, Milhem MM, Glaspy J, et al. Randomized, open-label phase II study evaluating the efficacy and safety of talimogene laherparepvec in combination with ipilimumab versus ipilimumab alone in patients with advanced unresectable Melanoma. J Clin Oncol. 2018;36:1658–67. https://doi.org/10.1200/JCO.2017.73.7379.
Puzanov I, Milhem MM, Minor D, Hamid O, Li A, Chen L, et al. Talimogene laherparepvec in combination with Ipilimumab in previously untreated, unresectable stage IIIB-IV melanoma. J Clin Oncol. 2016;34:2619–26. https://doi.org/10.1200/JCO.2016.67.1529.
Schwarze JK, Tijtgat J, Awada G, Cras L, Vasaturo A, Bagnall C, et al. Intratumoral administration of CD1c (BDCA-1)+ and CD141 (BDCA-3)+ myeloid dendritic cells in combination with talimogene laherparepvec in immune checkpoint blockade refractory advanced melanoma patients: a phase I clinical trial. J IMMUNOTHER CANCER. 2022;10:e5141. https://doi.org/10.1136/jitc-2022-005141.
Stahlie EHA, Franke V, Zuur CL, Klop WMC, van der Hiel B, Van de Wiel BA, et al. T-VEC for stage IIIB-IVM1a melanoma achieves high rates of complete and durable responses and is associated with tumor load: a clinical prediction model. Cancer Immunol Immunother. 2021;70:2291–300. https://doi.org/10.1007/s00262-020-02839-7.
García M, Moreno R, Gil-Martin M, Cascallò M, de Olza MO, Cuadra C, et al. A phase 1 trial of oncolytic adenovirus ICOVIR-5 administered intravenously to cutaneous and uveal melanoma patients. Hum Gene Ther. 2019;30:352–64. https://doi.org/10.1089/hum.2018.107.
Curti B, Richards J, Faries M, Andtbacka RHI, Grose M, Karpathy R, et al. The MITCI (phase 1b) study: a novel immunotherapy combination of coxsackievirus A21 and ipilimumab in patients with advanced melanoma. ANN ONCOL. 2016;27:i360. https://doi.org/10.1093/annonc/mdw378.06.
Galanis E, Markovic SN, Suman VJ, Nuovo GJ, Vile RG, Kottke TJ, et al. Phase II trial of intravenous administration of reolysin® (reovirus serotype-3-dearing strain) in patients with metastatic melanoma. Mol Ther. 2012;20:1998–2003. https://doi.org/10.1038/mt.2012.146.
Kaufman HL. Targeting the local tumor microenvironment with vaccinia virus expressing B7.1 for the treatment of melanoma. J Clin Invest. 2005;115:1903–12. https://doi.org/10.1172/JCI24624.
Cui C, Wang X, Lian B, Ji Q, Zhou L, Chi Z, et al. OrienX010, an oncolytic virus, in patients with unresectable stage IIIC–IV melanoma: a phase Ib study. J Immunother Cancer. 2022;10:e4307. https://doi.org/10.1136/jitc-2021-004307.
Andtbacka RHI, Curti B, Daniels GA, Hallmeyer S, Whitman ED, Lutzky J, et al. Clinical responses of oncolytic coxsackievirus A21 (V937) in patients with unresectable melanoma. J Clin Oncol. 2021;39:3829–38. https://doi.org/10.1200/JCO.20.03246.
Andtbacka RHI, Kaufman HL, Collichio F, Amatruda T, Senzer N, Chesney J, et al. Talimogene laherparepvec improves durable response rate in patients with advanced melanoma. J Clin Oncol. 2015;33:2780–8. https://doi.org/10.1200/JCO.2014.58.3377.
Andtbacka RHI, Ross M, Puzanov I, Milhem M, Collichio F, Delman KA, et al. Patterns of clinical response with talimogene laherparepvec (T-VEC) in patients with melanoma treated in the OPTiM phase III clinical trial. Ann Surg Oncol. 2016;23:4169–77. https://doi.org/10.1245/s10434-016-5286-0.
Zajac P, Oertli D, Marti W, Adamina M, Bolli M, Guller U, et al. Phase I/II clinical trial of a nonreplicative vaccinia virus expressing multiple HLA-A0201-restricted tumor-associated epitopes and costimulatory molecules in metastatic melanoma patients. Hum Gene Ther. 2003;14:1497–510. https://doi.org/10.1089/104303403322495016.
Hardcastle J, Mills L, Malo CS, Jin F, Kurokawa C, Geekiyanage H, et al. Immunovirotherapy with measles virus strains in combination with anti–PD-1 antibody blockade enhances antitumor activity in glioblastoma treatment. Neuro Oncol. 2017;19:w179. https://doi.org/10.1093/neuonc/now179.
Passaro C, Alayo Q, DeLaura I, McNulty J, Grauwet K, Ito H, et al. Arming an oncolytic herpes simplex virus type 1 with a single-chain fragment variable antibody against PD-1 for experimental glioblastoma therapy. Clin Cancer Res. 2019;25:290–9. https://doi.org/10.1158/1078-0432.CCR-18-2311.
Bommareddy PK, Patel A, Hossain S, Kaufman HL. Talimogene laherparepvec (T-VEC) and other oncolytic viruses for the treatment of melanoma. Am J Clin Dermatol. 2017;18:1–15. https://doi.org/10.1007/s40257-016-0238-9.
Morad G, Helmink BA, Sharma P, Wargo JA. Hallmarks of response, resistance, and toxicity to immune checkpoint blockade. Cell. 2021;184:5309–37. https://doi.org/10.1016/j.cell.2021.09.020.
Larkin J, Del Vecchio M, Ascierto PA, Krajsova I, Schachter J, Neyns B, et al. Vemurafenib in patients with BRAFV600 mutated metastatic melanoma: an open-label, multicentre, safety study. Lancet Oncol. 2014;15:436–44. https://doi.org/10.1016/S1470-2045(14)70051-8.
Breitbach CJ, Lichty BD, Bell JC. Oncolytic viruses: therapeutics with an identity crisis. EBioMedicine. 2016;9:31–6. https://doi.org/10.1016/j.ebiom.2016.06.046.
Park SY, Green AR, Hadi R, Doolittle-Amieva C, Gardner J, Moshiri AS. Tumoral melanosis mimicking residual melanoma in the setting of talimogene laherparepvec treatment. J Immunother Cancer. 2022;10:e5257. https://doi.org/10.1136/jitc-2022-005257.
Audrey-Bayan C, Trager MH, Gartrell-Corrado RD, Rizk EM, Pradhan J, Silverman AM, et al. Distinguishing melanophages from tumor in melanoma patients treated with talimogene laherparepvec. Melanoma Res. 2020;30:410–5. https://doi.org/10.1097/CMR.0000000000000661.
Kaufman HL, Kohlhapp FJ, Zloza A. Oncolytic viruses: a new class of immunotherapy drugs. Nat Rev Drug Discov. 2015;14:642–62. https://doi.org/10.1038/nrd4663.
Acknowledgements
None.
Funding
This work is supported by National Natural Science Foundation of China (Grant Num. 81801381), and Qingdao Medical and Health Outstanding Young Talent Training Project:2020–2023. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
CY.W and Y.L contributed to the conception, interpretation and drafting of the study. NX.L and L.Y searched the database and extracted data with help from CY.W. NX.L and Y.L contributed to the quality assessment of included studies. NX.L and L.Y performed the statistical design and analysis, and prepared the tables and figures. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors declare no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Figures S1-S6.
Additional file 2.
Supplementary Tables S1-S4.
Additional file 3.
Quality assessment results of included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, C., Lu, N., Yan, L. et al. The efficacy and safety assessment of oncolytic virotherapies in the treatment of advanced melanoma: a systematic review and meta-analysis. Virol J 20, 252 (2023). https://doi.org/10.1186/s12985-023-02220-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-023-02220-x