Abstract
Since the COVID-19 emergence as a global pandemic in March 2020, more than 5 million SARS-CoV-2-related deaths have been globally documented. As the pandemic progressed, it became clear that, although the infection is mainly characterized as a respiratory disease, it also affects other organs and systems, including the thyroid gland. Indeed, emerging evidence suggests that SARS-CoV-2 can act as a trigger for various thyroid disorders, for example, subacute thyroiditis (SAT), Grave’s disease, and non-thyroidal illness syndrome. The entry of SARS-CoV-2 into the host cells is mainly mediated by the ACE2-receptor, making organs and systems with high expression of this receptor, such as the thyroid gland, highly vulnerable to COVID-19. Accumulating data propose that SAT may be an underestimated manifestation of COVID-19 infection. Importantly, if SAT remains unrecognized, it may trigger or aggravate potential other complications of the disease, for example, respiratory insufficiency and cardiovascular complications, and thus negatively influence prognosis. Moreover, recent case reports, case series, and systematic reviews highlight SAT as a potential side effect of the vaccination against SARS-CoV-2. The present review aims to raise awareness of SARS-CoV-2-associated- and post-vaccination subacute thyroiditis, to discuss recent evidence regarding its pathophysiology, and to present useful information for this special form of SAT related to daily clinical practice.
Similar content being viewed by others
Introduction
The novel coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome virus 2 (SARS-CoV-2) was characterized as a pandemic on March 11, 2020, by the World Health Organization, when 118,000 confirmed cases were diagnosed in 114 different countries [1]. As on April 2021, the number of confirmed cases had exceeded 35 million worldwide, with more than 5 million fatalities making it the most lethal and most rapidly spreading pandemic since the Spanish influenza of 1918 [2, 3]. Despite that the respiratory system represents the main system affected by the virus. This infection can progress to acute respiratory distress syndrome and multiorgan failure; the virus shows a marked tropism for various organs and systems, leading to extrapulmonary manifestations comprising central and peripheral neurological disorders, coagulation disturbances, renal failure, liver abnormalities, cardiac dysfunction including heart failure and arrhythmias, and rhabdomyolysis [4]. Indeed, ACE 2 and transmembrane protease serine 2 (TMPRSS 2), which are variably expressed in human organs and tissues, essentially facilitate the internalization of SARS-CoV-2 into host cells. As we meanwhile know, ACE2 and TMPRSS2 serve as the key molecular complex to enter the host cells and are highly expressed in the small intestine, the kidney, the heart, the brain, and the skin [1]. In addition, the endocrine system demonstrates high ACE2 and TMPRSS2 expression levels, including the reproductive tract, testicle, pancreas, parathyroids, and thyroid gland, making the mentioned glands susceptible to the SARS-CoV-2 infection (Fig. 1) [5].
Simplified schematic representation of the main pathophysiological mechanisms of thyroid injury due to COVID-19 infection. SARS-CoV-2 can damage the thyroid gland in a direct and indirect way. Direct toxicity ACE2 and TMPRSS2 on the surface of thyroid follicular cells serve as an entrance gate for the internalization of the virus into the host cells. The same possibly applies to the integrin αvβ3, leading to thyroid gland damage. Additionally, it is suggested that the virus can affect the hypothalamus and the pituitary resulting in HPA-axis dysfunction and, thus, thyroid abnormalities. Indirect toxicity: SARS-CoV-2-induced pulmonary and systemic inflammation and innate immune system activation could potentially damage the thyroid gland in an indirect way. Finally, corticosteroids, which are widely used in the management of COVID-19 patients, inhibit pituitary thyrotrope cells and TRH-release. ACE2 angiotensin-converting enzyme 2; COVID-19 Coronavirus disease 2019; HPA-Axis hypothalamic–pituitary–adrenal axis; SARS-CoV-2 severe acute respiratory syndrome coronavirus 2; TMPRSS2 transmembrane serine protease 2; TRH thyrotropin-releasing hormone
During the last three years, several studies have been published highlighting the effect of COVID-19 infection on the thyroid gland [5]. Since 2020, some of these studies have been listed in COVID-19-associated SAT, whereas since 2021, SAT has been demonstrated as a complication that can potentially follow SARS-CoV-2 vaccination [6]. Given the increasing incidence of SAT during and post COVID-19 infection and the mass vaccination of the population against SARS-CoV-2, the present review aims to sensitize clinicians to these new clinical entities of SAT, fill the gap regarding its pathophysiology by presenting recent research evidence and quote useful clinical approaches regarding diagnosis and management of SAT in the COVID-19 area.
SARS-CoV-2-associated subacute thyroiditis
Pathophysiology
The exact pathophysiology of COVID-19-associated SAT has not been completely deciphered (Fig. 1). However, as mentioned above, direct molecular analysis of surgical samples of thyroid tissues has demonstrated the expression of ACE2 and TMPRSS2 on the thyroid follicular cells making the thyroid gland susceptible to the development of injury during COVID-19 infection either via direct viral toxicity or via an indirect way due to immune-mediated injury or activation of the hypothalamo-pituitary axis by inflammatory cascades [7]. Moreover, another hypothesis regarding the internalization of SARS-CoV-2 into host cells focuses on the role of integrin ανβ3, which recognizes and binds Arg-Gly-Asp (RGD) and Lys-Gly-Asp (KGD), molecular motifs, which are localized in the ACE2 and the spike protein of SARS-CoV-2. Thus, it is hypothesized that integrin ανβ3 may serve as an alternative entrance gate for COVID-19 into host cells [8]. Matters appear to be further complicated by the fact that increased thyroxine concentrations—commonly seen in SAT—induce enhanced expression of integrins, potentially facilitating the entry of the virus into the host cells [1]. Moreover, as it is known, the initial stage of the disease—with its flu-like manifestations and possible transition to pneumonia—is followed by the second stage, characterized by pulmonary and systemic inflammation. Indeed, this phase of the disease commonly coexists with innate immune activation and excessive release of pro-inflammatory cytokines, for example, tumor necrosis factor α, interleukin (IL) 1β, IL-6, and adaptive T-cell-mediated immune responses [7].
Finally, it should be mentioned that genetic predisposition—especially regarding various haplotypes of human leukocyte antigen (HLA)—seems to play a pivotal role in the pathogenesis of SAT [9] via stimulation of aberrant human leukocyte antigen DR isotype expression and the activation of toll-like receptors [10]. The first correlation of SAT with HLA and specifically with HLA-B35 was carried out by Nyulassy almost 50 years ago [11], a native that was verified in a multitude of publications in the years that followed [9]. In the meantime, it is well documented that 70% of patients with SAT are carriers of HLA-B35, while for the remaining 30%, the genetic background is not determined [12]. This observation raises the question if patients who are negative for HLA-B35 have another unknown genetic predisposition. Indeed, further studies have shown that other HLA haplotypes, for example, HLA-B67, HLA-B15/62, HLA-Bw35, and HLA-Drw8, could be additionally implicated in the pathogenesis of SAT [13]. Lastly, a recent, large healthy Polish cohort of Stasiak et al. (2020) highlighted that HLA-B*18:01 and HLA-DRB1*01 represent independent SAT risk alleles and that carriers of HLA-B*35 and HLA-C*04:01 are genetically susceptible to its development [9].
Clinical, laboratory, and radiologic findings
In the vast majority of cases, SAT is a self-limited inflammatory disease that—although not exclusively—is caused by viral infections [14]. It is presumed to occur either simultaneously with SARS-CoV-2 infection due to direct viral toxicity or to represent a post-viral complication of COVID-19 infection, frequently within 6–8 weeks [6]. Similar to SAT caused by other viruses, COVID-19-associated SAT shows a predilection for middle age female patients [15]. Patients with SARS-CoV-2-induced SAT present classical signs and symptoms caused by thyroid inflammation, including neck tenderness and pain, and symptoms associated with the underlying hyperthyroidism (e.g., fever, palpitations, anxiety, agitation, tremor, heat intolerance, insomnia, weight loss, and excessive perspiration) [15]. However, compared to SAT induced by other infections, some studies have highlighted a stronger intensity of neck pain, a higher incidence of fever, and a higher probability of hypothyroidism at three months of the disease onset [6]. Until March 2022—and two years after the first described case of COVID-19-associated SAT [2, 6]—only 81 cases of SAT related to SARS-CoV-2 infection had been published. This observation raises the suspicion that the described low incidence rate may have been underestimated when the high expression of ACE2 and TMPRSS2 in the thyroid gland is taken into account. Indeed, as mentioned above, neck tenderness and pain constitute the main findings and diagnostic criteria of painful SAT [15]. However, in patients with COVID-19 infection, there is a significant possibility that these signs and symptoms may be either masked by the respiratory symptoms of the disease or modified by therapeutic interventions (e.g., by dexamethasone- and heparin application), leading to atypical forms of SAT and, as such, easily escaping physicians’ attention. Indeed, despite the initial skepticism about corticosteroid administration, almost half of the patients with COVID-19 have been treated with some type of corticosteroid [16]. Moreover, SAT and COVID-19 often present common symptoms (e.g., fever, asthenia, and neck pain), which can lead to misinterpretation of the contemporary presence of thyroiditis [16].
A further diagnostic pitfall in the context of corticosteroid administration is the fact that even low doses of corticosteroid administration can affect TSH levels in humans due to their direct inhibitory effect on pituitary thyrotrope cells and inhibition of the hypothalamic release of TRH. Furthermore, acute glucocorticoid administration results in a decrease in circulating T3 to T4, indicating that these agents hinder the conversion of T4 to T3 [16]. Additionally, in critically ill patients with COVID-19 admitted to high-intensity care units, low levels of TSH and free T3 have been demonstrated in the study of Muller et al. [17]. Moreover, regarding the clinical findings for this specific patients population, the authors described an atypical subtle form of SAT characterized by lymphopenia and not leucocytosis, formulating the hypothesis that the presence of lymphopenia inhibits the pathognomic infiltration of giant cells and, consequently, the appearance of classic symptoms of the disease.
Despite the fact that SAT is mainly a clinical diagnosis, laboratory and ultrasound findings can support its diagnosis further, particularly in atypical manifestations of the disease. Typically, laboratory findings include thyroid function disturbances and elevated inflammatory markers, whereas thyroid ultrasound frequently reveals a voluminous and inhomogenous thyroid gland [6].
Therapeutic management
Although, to date, no causal treatment for SAT exists, corticosteroids appear to be effective in controlling symptoms even within the first 24 h. In order to avoid the detrimental effects of long-term steroid use, some authors recommend the combined use of steroids/celecoxib. In the case of patients with mild to moderate disease severity, starting with a low dose of prednisolone is encouraged, whereas, for more severe cases, it seems that higher doses cannot be avoided [18].
Subacute thyroiditis following vaccination against SARS-CoV-2
Similar to infections, vaccination can potentially induce immunologic reactions resulting in autoimmune diseases. The pathophysiological mechanisms are complex and include molecular mimicry, polyclonal activation, epitope spreading, and presentation of cryptic antigenic components [19]. In this context, the development of subacute thyroiditis after vaccination is well established and has been previously described as a consequence of influenza [20], hepatitis B [21], and human papillomavirus vaccinations [22].
Although no curative treatment against SARS-CoV-2 currently exists, various types of vaccines have been developed [3, 23], whose safety and efficacy have been adequately tested in a significant number of clinical studies [19]. Regardless, however, of the provable safety of the vaccines, several types of post-vaccination side effects have been highlighted. The most frequently observed side effect refers to mild reactions, including pain and swelling at the injection site, fever, headaches, chills, muscle/joint aches, and tiredness [24]. However, rare complications, such as thyroid diseases, including SAT, may also occur [19].
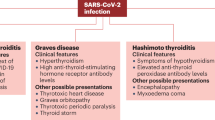
There is mounting evidence from case reports, case series, and retrospective, prospective, and longitudinal studies indicating that SAT is a rare adverse effect that has been observed after vaccination with different types of SARS-CoV-2 vaccines (Table 1, Fig. 2) [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. Even though post-vaccination SAT represents an uncommon complication, given the intensity of vaccinations against COVID-19—until March 2022, a total of almost 11 billion vaccine doses had been globally administered [3]—physicians should be aware of this side effect, which should not influence immunization strategies in any case.
Pathophysiology
As previously mentioned, the pathogenesis of vaccine-induced-SAT is mediated by various pathophysiological mechanisms, for example, molecular mimicry, polyclonal and bystanding activation, epitope spreading, and presentation of cryptic antigen determinants [19]. However, the main pathogenetic mechanisms include molecular mimicry between thyroid components (e.g., thyroid peroxidase peptide sequences) and vaccine antigens—particularly the spike protein—and immune system hyperstimulation [6].
The vast majority of vaccines against COVID-19 encode the S protein of the virus, leading to the production of antibodies, which could potentially play a role in initiating autoimmunity via molecular mimicry mechanisms [35]. Moreover, accumulating data indicate that if the vaccine contains antigenic epitopes, which are structurally similar to autoantigens, then the immune reaction to the vaccination antigen can extend to host cells’ antigens, especially in genetically susceptible individuals [73, 74]. Concerning thyroid tissue antigens, recent research highlights that thyroid peroxidase sequences share structural similarities with SARS-CoV-2-related proteins [35], potently contributing to a cross-reactive immune reaction between the spike protein of the virus and the thyroid antigens [73, 74].
The second major hypothesis regarding the pathophysiology of post-vaccination SAT refers to an autoimmune/autoinflammatory syndrome induced by adjuvants, that is, the ASIA syndrome, according to which the vaccination against SARS-CoV-2 can trigger an autoimmune thyroid response [6]. Indeed, it has been proposed that vaccine adjuvants, used to enhance the immunogenicity of the vaccine, are potential triggers of adverse immune reactions [75]. However, this last hypothesis requires further and in-depth investigation as a number of studies failed to show a causal relationship between vaccine adjuvants and autoimmune pathologic entities [19].
Additionally, it should be mentioned that vaccine-related S protein may directly interact with thyroid cells expressing ACE2 and thus result in thyroid dysfunction [19]. Finally, vaccine-associated enhanced viscosity-status may lead to a pathological release of thyroid hormones from the thyroid, especially in patients with abnormal coagulation status [76].
Diagnosis and differential diagnosis
Post-vaccination SAT literally refers to a painful thyroid inflammation following vaccination [77]. Consistent with previous studies of SAT of other etiologies [78], recent systematic reviews demonstrate a clear gender preference, with middle-aged women being more affected than men, with a gender ratio of about 2.57:1 [79]. The patient’s age at presentation ranges from 26 to 73 years old [79], while the timeline between vaccination and onset of SAT symptoms lies between a few hours to a few weeks (12 h to 60 days) [77].
Similarly to classic forms of SAT, the most frequently reported signs and symptoms of post-vaccination SAT include anterior neck pain, commonly radiating to the jaw and the ear, neck swelling, headaches, nausea, concentration difficulties, fever, asthenia, fatigue, emotional lability, and signs of thyrotoxicosis (e.g., palpitations, hypertension, weight loss, hyper-defecation, anxiety, and sweating) [79]. It should be noted, however, that in some patients, symptoms caused by post-vaccination SAT may have been underestimated and falsely identified as common vaccination side effects leading to an overlook of the diagnosis of SAT induced by the SARS-CoV-2 vaccine.
Regarding the biochemical characteristics of patients with post-vaccination SAT, thyroid function tests are almost universally consistent with thyrotoxicosis (i.e., suppressed TSH and elevated free T4), with some patients additionally revealing enhanced levels of free T3. Antithyroid antibodies are typically negative, while inflammation markers, such as erythrocyte sedimentation rate (ESR) and C-reactive protein, are typically elevated [51, 79].
Ultrasonographic findings of the disease, when available, include a voluminous, hypoechoic thyroid gland with heterogeneous echo-structure and suppressed vascularization, similar to SAT of other etiologies [77].
A differential diagnosis is of decisive importance for the prognosis of the patients and should include alternative causes of thyrotoxicosis and thyroiditis, such as SARS-CoV-2-associated SAT, as well as causes related to other infectious, for example, Epstein-Barr, cytomegalovirus, influenza, measles, rubella, and mumps [80].
Conclusions
Nowadays, SARS-CoV-2-associated SAT is considered a rare complication of ongoing COVID-19 infection or a post-viral immune manifestation of the disease. However, accumulating research evidence indicates a high rate of undiagnosed cases of SARS-CoV-2- associated SAT, especially during the acute phase of the disease. Moreover, during the last few years, a variety of studies have indicated SAT as a potential rare side effect of vaccination. However, given the greatest mass vaccination in world history, it is estimated that the number of post-vaccination SAT will undoubtedly increase. High clinical suspicion leading to its early recognition significantly contributes to the improvement of patients’ prognosis. Currently, several issues in reference to the pathophysiology, the clinical presentations, and the specific therapeutic approaches of both SARS-CoV-2-associated- and post-vaccination SAT still remain open. Further research is also needed for the clarification of questions related to the optimization of therapeutic implications and the improvement of prognosis for both pathologic entities.
Availability of data and materials
Not applicable.
References
Lisco G, et al. Thyroid and COVID-19: a review on pathophysiological, clinical and organizational aspects. J Endocrinol Investig. 2021;44(9):1801–14.
Duntas LH, Jonklaas J. COVID-19 and thyroid diseases: a bidirectional impact. J Endocr Soc 2021;5(8): p. bvab076.
Organization WH. WHO COVID-19 dashboard. 2022.
Khatri A, Charlap E, Kim A. Subacute thyroiditis from COVID-19 infection: a case report and review of literature. Eur Thyroid J. 2021;9(6):324–8.
Rossetti CL, et al. COVID-19 and thyroid function: What do we know so far? Front Endocrinol (Lausanne). 2022;13:1041676.
Popescu M, et al. The new entity of subacute thyroiditis amid the COVID-19 pandemic: from infection to vaccine. Diagnostics (Basel) 2022;12(4).
Chen W, et al. Potential interaction between SARS-CoV-2 and thyroid: a review. Endocrinology, 2021;162(3).
Ross RS. Integrating integrins: A new way to increase our COVID-19 armamentarium? JACC Basic Transl Sci. 2021;6(1):9–11.
Stasiak M, et al. Subacute thyroiditis is associated with HLA-B*18:01, -DRB1*01 and -C*04:01-the significance of the new molecular background. J Clin Med 2020;9(2).
Scappaticcio L, et al. Impact of COVID-19 on the thyroid gland: an update. Rev Endocr Metab Disord. 2021;22(4):803–15.
Nyulassy S, Hnilica P, Stefanovic J. The HL-A system and subacute thyroiditis A preliminary report. Tissue Antigens. 1975;6(2):105–6.
Nyulassy S, et al. Subacute (de Quervain’s) thyroiditis: association with HLA-Bw35 antigen and abnormalities of the complement system, immunoglobulins and other serum proteins. J Clin Endocrinol Metab. 1977;45(2):270–4.
Stasiak M, et al. The risk of recurrence of subacute thyroiditis is HLA-dependent. Int J Mol Sci 2019;20(5).
Trimboli P, et al. COVID-19-associated subacute thyroiditis: evidence-based data from a systematic review. Front Endocrinol (Lausanne). 2021;12: 707726.
Christensen J, et al. Risk factors, treatment and outcomes of subacute thyroiditis secondary to COVID-19: a systematic review. Intern Med J. 2022;52(4):522–9.
Croce L, et al. The cytokine storm and thyroid hormone changes in COVID-19. J Endocrinol Investig. 2021;44(5):891–904.
Muller I, et al. SARS-CoV-2-related atypical thyroiditis. Lancet Diabetes Endocrinol. 2020;8(9):739–41.
Ray I, et al. Management of subacute thyroiditis—a systematic review of current treatment protocols. Int J Gen Med. 2022;15:6425–39.
Olivieri B, Betterle C, Zanoni G. Vaccinations and autoimmune diseases. Vaccines (Basel) 2021;9(8).
Hernan Martinez J, et al. Subacute thyroiditis and dyserythropoesis after influenza vaccination suggesting immune dysregulation. Bol Asoc Med P R 2011;103(2):48–52.
Toft J, Larsen S, Toft H. Subacute thyroiditis after hepatitis B vaccination. Endocr J. 1998;45(1):135.
Pellegrino P, et al. The epidemiological profile of ASIA syndrome after HPV vaccination: an evaluation based on the Vaccine Adverse Event Reporting Systems. Immunol Res. 2015;61(1–2):90–6.
Shiravi AA, et al. Cardiovascular complications of SARS-CoV-2 vaccines: an overview. Cardiol Ther. 2022;11(1):13–21.
Polack FP, et al. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine. N Engl J Med. 2020;383(27):2603–15.
Flores Rebollar A. Subacute thyroiditis after anti-SARS-CoV-2 (Ad5-nCoV) vaccine. Enferm Infecc Microbiol Clin (Engl Ed). 2022;40(8):459–60.
Murashita M, et al. Subacute thyroiditis associated with thyrotoxic periodic paralysis after COVID-19 vaccination: a case report. Endocrinol Diabetes Metab Case Rep 2022;2022.
Sozen M, et al. COVID-19 mRNA vaccine may trigger subacute thyroiditis. Hum Vaccin Immunother. 2021;17(12):5120–5.
Khan F, Brassill MJ. Subacute thyroiditis post-Pfizer-BioNTech mRNA vaccination for COVID-19. Endocrinol Diabetes Metab Case Rep 2021;2021.
Saha A, Chittimoju S, Trivedi N. Thyroiditis after mRNA vaccination for COVID-19. Case Rep Endocrinol. 2022;2022:7604295.
Jhon M, et al. Subacute thyroiditis after receiving the mRNA COVID-19 vaccine (Moderna): the first case report and literature review in Korea. J Korean Med Sci. 2022;37(6): e39.
Oyibo SO. Subacute thyroiditis after receiving the adenovirus-vectored vaccine for coronavirus disease (COVID-19). Cureus. 2021;13(6): e16045.
Raashid S, et al. Subacute thyroiditis after receiving inactivated virus vaccine for COVID-19. J Community Hosp Intern Med Perspect. 2022;12(2):14–7.
Gonzalez Lopez J, Martin Nino I, Arana Molina C. Subacute thyroiditis after SARS-CoV-2 vaccination: report of two clinical cases. Med Clin (Engl Ed) 2022;158(12):e13–e14.
Sahin Tekin M, Saylisoy S, Yorulmaz G. Subacute thyroiditis following COVID-19 vaccination in a 67-year-old male patient: a case report. Hum Vaccin Immunother 2021;17(11):4090–4092.
Iremli BG, Sendur SN, Unluturk U. Three cases of subacute thyroiditis following SARS-CoV-2 vaccine: postvaccination ASIA syndrome. J Clin Endocrinol Metab. 2021;106(9):2600–5.
Adelmeyer J, et al. Two case reports of subacute thyroiditis after receiving vaccine for COVID-19. Case Rep Endocrinol. 2022;2022:3180004.
Vu TB, et al. Subacute thyroiditis after receiving the vaccine for COVID-19: a case report and literature review. Clin Exp Vaccine Res. 2022;11(2):226–9.
Ie K, et al. Subacute thyroiditis developing within 2 days of vaccination against COVID-19 with BNT162b2 mRNA. Eur J Case Rep Intern Med. 2023;10(1): 003735.
Bahcecioglu AB, et al. Subacute thyroiditis during the COVID-19 pandemic: a prospective study. J Endocrinol Investig. 2022;45(4):865–74.
Chatzi S, et al. Subacute thyroiditis after SARS-CoV-2 vaccination: a report of two sisters and summary of the literature. Hormones (Athens). 2022;21(1):177–9.
Frangos S, et al. Subacute thyroiditis after the third dose of the COVID-19 mRNA vaccine. Case report Hell J Nucl Med. 2022;25(2):210–2.
Casey C, Higgins T. Subacute thyroiditis post viral vector vaccine for COVID-19. Endocrinol Diabetes Metab Case Rep 2022;2022.
Kishimoto M, Ishikawa T, Odawara M. Subacute thyroiditis with liver dysfunction following coronavirus disease 2019 (COVID-19) vaccination: report of two cases and a literature review. Endocr J. 2022;69(8):947–57.
Zhao Y, Zhao B, Liang YB. Successful treatment of subacute thyroiditis after recombinant COVID-19 vaccination using traditional chinese medicine: a case report. Cureus. 2022;14(10): e30716.
Borges Canha M, et al. Subacute thyroiditis after severe acute respiratory syndrome coronavirus 2 Vaxzevria vaccination in a patient with thyroid autoimmunity. Cureus. 2022;14(2): e22353.
Pujol A, et al. Thyroid as a target of adjuvant autoimmunity/inflammatory syndrome due to mRNA-based SARS-CoV2 vaccination: from Graves’ disease to silent thyroiditis. J Endocrinol Invest. 2022;45(4):875–82.
Saygili ES, Karakilic E. Subacute thyroiditis after inactive SARS-CoV-2 vaccine. BMJ Case Rep 2021;14(10).
Bres F, et al. Three cases of thyroiditis after COVID-19 RNA-vaccine. Ann Endocrinol (Paris). 2022;83(4):262–4.
Pandya M, et al. Thyroiditis after COVID-19 mRNA vaccine: a case series. AACE Clin Case Rep. 2022;8(3):116–8.
Siolos A, Gartzonika K, Tigas S. Thyroiditis following vaccination against COVID-19: Report of two cases and review of the literature. Metabol Open. 2021;12: 100136.
PlaPeris B, et al. Thyrotoxicosis following SARS-COV-2 vaccination: a case series and discussion. J Endocrinol Investig. 2022;45(5):1071–7.
Alkis N, Baysal M. Subacute thyroiditis after SARS-CoV-2 BNT162b2 vaccine in a multiple myeloma patient. SAGE Open Med Case Rep 2022;10:2050313X221091392.
Teti C, et al. Subacute thyroiditis after SARS-CoV2 vaccine: possible relapse after boosting. J Endocrinol Invest. 2022;45(10):2019–20.
Patel KR, Cunnane ME, Deschler DG. SARS-CoV-2 vaccine-induced subacute thyroiditis. Am J Otolaryngol. 2022;43(1): 103211.
Bornemann C, Woyk K, Bouter C. Case report: two cases of subacute thyroiditis following SARS-CoV-2 vaccination. Front Med (Lausanne). 2021;8: 737142.
Ratnayake GM, Dworakowska D, Grossman AB. Can COVID-19 immunisation cause subacute thyroiditis? Clin Endocrinol (Oxf). 2022;97(1):140–1.
Das L, Bhadada SK, Sood A. Post-COVID-vaccine autoimmune/inflammatory syndrome in response to adjuvants (ASIA syndrome) manifesting as subacute thyroiditis. J Endocrinol Invest. 2022;45(2):465–7.
Jeeyavudeen MS, et al. COVID-19 vaccine-associated subacute thyroiditis: an unusual suspect for de Quervain's thyroiditis. BMJ Case Rep 2021;14(11).
Plaza-Enriquez L, et al. A case report of subacute thyroiditis following mRNA COVID-19 vaccine. Case Rep Endocrinol. 2021;2021:8952048.
Vasileiou V, et al. Recurring subacute thyroiditis after SARS-CoV-2 mRNA vaccine: a case report. Case Rep Womens Health. 2022;33: e00378.
Bostan H, et al. Evaluation of the diagnostic features and clinical course of COVID-19 vaccine-associated subacute thyroiditis. Hormones (Athens). 2022;21(3):447–55.
Pi L, et al. Case Report: Subacute thyroiditis after receiving inactivated SARS-CoV-2 vaccine (BBIBP-CorV). Front Med (Lausanne). 2022;9: 918721.
Wijenayake UN, et al. A case report of subacute thyroiditis after inactivated SARS-CoV-2 vaccine. SAGE Open Med Case Rep 2022;10:2050313X221140243.
Yorulmaz G, Sahin Tekin M. SARS-CoV-2 vaccine-associated subacute thyroiditis. J Endocrinol Investig 2022;45(7):1341–1347.
Pipitone G, et al. Vaccine-induced subacute thyroiditis (De Quervain’s) after mRNA vaccine against SARS-CoV-2: a case report and systematic review. Infect Dis Rep. 2022;14(1):142–54.
Huang Y, et al. Case report: subacute thyroiditis after receiving SARS-CoV-2 vaccine, maybe not only adjuvants. Front Med (Lausanne). 2022;9: 856572.
Stasiak M, Zawadzka-Starczewska K, Lewinski A. Significance of HLA haplotypes in two patients with subacute thyroiditis triggered by mRNA-based COVID-19 vaccine. Vaccines (Basel) 2022;10(2).
Topaloglu O, et al. Differences in clinical aspects between subacute thyroiditis associated with COVID-19 vaccines and classical subacute thyroiditis. Horm Metab Res. 2022;54(6):380–8.
Soltanpoor P, Norouzi G. Subacute thyroiditis following COVID-19 vaccination. Clin Case Rep. 2021;9(10): e04812.
Reisi-Vanani V, et al. Role of the immune system and possible mechanisms in COVID-19 vaccine-induced thyroiditis: Case report and literature review. J Clin Transl Endocrinol Case Rep. 2022;26: 100138.
Sigstad E, Groholt KK Westerheim O. Subacute thyroiditis after vaccination against SARS-CoV-2. Tidsskr Nor Laegeforen 2021;141(2021–14).
Oguz SH, et al. SARS-CoV-2 vaccine-induced thyroiditis: safety of revaccinations and clinical follow-up. J Clin Endocrinol Metab. 2022;107(5):e1823–34.
Vojdani A, Kharrazian D. Potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases. Clin Immunol. 2020;217: 108480.
Vojdani A, Vojdani E, Kharrazian D. Reaction of human monoclonal antibodies to SARS-CoV-2 proteins with tissue antigens: implications for autoimmune diseases. Front Immunol. 2020;11: 617089.
Watad A, et al. Autoimmune/inflammatory syndrome induced by adjuvants and thyroid autoimmunity. Front Endocrinol (Lausanne). 2016;7:150.
Joob B, Wiwanitkit V. Expected viscosity after COVID-19 vaccination, hyperviscosity and previous COVID-19. Clin Appl Thromb Hemost. 2021;27:10760296211020832.
Caironi V, Pitoia F, Trimboli P. Thyroid inconveniences with vaccination against SARS-CoV-2: the size of the matter a systematic review. Front Endocrinol (Lausanne). 2022;13: 900964.
Fatourechi V, et al. Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study. J Clin Endocrinol Metab. 2003;88(5):2100–5.
Jafarzadeh A, et al. Thyroid dysfunction following vaccination with COVID-19 vaccines: a basic review of the preliminary evidence. J Endocrinol Investig. 2022;45(10):1835–63.
Kyriacou A, Ioakim S, Syed AA. COVID-19 vaccination and a severe pain in the neck. Eur J Intern Med. 2021;94:95–6.
Acknowledgements
Figures created with BioRender.com.
Funding
Publication costs for this article were funded by the authors’ institutions.
Author information
Authors and Affiliations
Contributions
The study was designed by MZ and AE. MZ searched the articles and drafted the manuscript, to which AE contributed and revised. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ziaka, M., Exadaktylos, A. Insights into SARS-CoV-2-associated subacute thyroiditis: from infection to vaccine. Virol J 20, 132 (2023). https://doi.org/10.1186/s12985-023-02103-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-023-02103-1