Abstract
The clinical data of a patient with Epstein-barr virus (EBV) associated with cholangiocarcinoma was reported in this paper: a case of a 36-year-old female presented with abdominal pain and systemic skin yellowing combined with skin itching. Laboratory studies showed increase in alanine aminotransferase 242 U/L, aspartate aminotransferase 404 U/L, r-glutamyltransferase 1516 U/L, total bilirubin 308.2 µmol/L and CA199 (101.0 U/ml). AFP (4.5 ng/ml) was normal. CT revealed multiple space-occupying lesions in the liver. PET-CT revealed liver malignant tumor and lymph node metastasis. Liver puncture pathology revealed infiltrative growth of significant heterocyst nests in the liver tissue, which was morphologically consistent with malignant tumors, considering poorly differentiated carcinoma. Pathology suggestion: combining liver puncture with morphology, immunohistochemistry, and EBV in situ hybridization results, it was consistent with EB virus-associated poorly differentiated carcinoma, therefore, consider EBV infection-associated poorly differentiated cholangiocarcinoma (CCA) (LELC morphology). The patient underwent liver transplantation in Hangzhou Shulan Hospital on June 8, 2021 successfully. After surgery, the patient orally took tacrolimus for anti-rejection, entecavir for antiviral therapy, gemcitabine 1.2 g + cis-platinum 30 mg for chemotherapy. After following up for more than 5 months post liver transplantation, the condition of the patient deteriorated. The patient subsequently died. Based on the case of our patient and the review of existing literature, when the patient's serum CA199 increased, AFP did not change significantly, and there was no previous history of hepatitis B. CT revealed a low-density mass in the liver, ring enhancement in the arterial phase, and heterogeneous enhancement of the tumor in the delayed phase. Ring enhancement of the liver lesion mass was observed on MRI. Consider the might possibility of hepatic CCA. When patients showed recurrent tonsillitis at an early age, EBV virus infection should be vigilant and oropharyngeal tissue should persist, diagnosis of EBV-associated liver cancer should be considered. In particular, EBV infection-related liver cancer is relatively rare, the clinician should improve the recognition of the disease to strive for early diagnosis and therapy.
Similar content being viewed by others
Background
Primary liver malignancies including hepatocellular carcinoma (HCC) is the most common type of liver cancer and cholangiocarcinoma. Primary liver cancers are a major cause of mortality worldwide and the third leading cause of cancer-related deaths globally [1]. For chemotherapy and radiation therapy are generally invalid, hepatic resection and liver transplantation are the standard of treatment for liver cancers [2]. However, literatures on the Epstein–Barr virus (EBV) cholangiocarcinoma have rarely been reported.
In 1964, Epstein-Barr first discovered human B lymphocytic herpesvirus with herpesvirus particles in malignant lymphocytoma tissues of African children, and established a lymphoblastoid cell line that can be transmitted in biopsies. It is named Epstein-Barr virus (EBV) because of its different characteristics from other members of the known human herpesvirus family [3]. At present, it is known that EBV infection is not only closely related to nasopharyngeal carcinoma, Burkitt's lymphoma, Hodgkin's disease, and human immunodeficiency virus, but also related to the occurrence and development of some foregut-derived organs such as stomach, parotid gland, lung, and thymic carcinoma [4]. Is the development of tumors in the biliary tract, as a foregut-derived organ, associated with EBV infection? EBV has a high infection rate in the population and can remain latent in the human body for life after infection. It can sometimes cause lytic death of infected cells and may also lead to malignant transformation of infected host cells and finally tumorigenesis [5]. Wang Xuemin et al concluded that there is latent infection of EBv in some cholangiocarcinoma cells, especially poorly differentiated cancer cells, suggesting that there are some correlation between EBV infection and the occurrence and development of the cholangiocarcinoma [6].
Undifferentiated carcinomas possessing dense lymphoplasmacytoid stroma are usually classified as lymphoepithelioid carcinoma (LELC) [7]. Among them, nasopharyngeal carcinoma (NPC) is the most common LELC tumor. LELC can also originate from tissues such as salivary glands, stomach, lung, and most of which are associated with EBV [8]. Pathologically, because Lymphoepithelioma-like cholangiocarcinoma (LELCC) is a rare primary adenocarcinoma, LELCC is considered to be an intrahepatic cholangiocarcinoma variant, with only 16 relevant references and 62.5% of cases associated with EBV [9,10,11,12,13,14,15,16,17,18]. The following two aspects must be met for its pathological diagnosis: the presence of EBV in glandular tissue, and no abnormal phenotype in lymphoid tissue [19]. Its etiology may be associated with DNA demethylation in tumor tissue [20, 21]. Fukayama M et al reported that many EBV-associated tumor tissues showed DNA demethylation [22, 23]. Some scholars believed that LELC-type cholangiocarcinoma had a better prognosis than conventional type of cholangiocarcinoma [14]. While some scholars believed that gastric and pulmonary LELC tumors had a better prognosis [24, 25]. However, Iezzoni et al concluded that organ types and existence/inexistence of EBV infection had no significance for assessing the prognosis of LELC tumors [8].
An unusual case of cholangiocarcinoma with a lymphoepithelioma-like appearance associated with EBV infection with poor prognosis was reported. Although previous studies have reported the EBV cholangiocarcinoma pathologic features, few studies have revealed the clinic features, laboratory tests, imaging characteristics and clinical course and outcomes. This study aims to highlight the clinical and imaging characteristic, pathologic features, the treatment as well as the outcome of the patient. Furthermore, a review of the literature was conducted in the present study to improve the recognition of the disease, and finally to strive for early diagnosis and therapy.
Case presentation
A 36-year-old female patient was admitted to the Department of Hepatobiliary Surgery, Affiliated Hangzhou First People's Hospital, Zhejiang University School of Medicine on April 28, 2021 with complaints of middle and upper abdominal pain and discomfort for more than 1 month combined with systemic skin yellowing with skin itching for 2 weeks. One month ago, the patient had middle and upper abdominal pain and discomfort without obvious inducement, which was intolerable. She visited Zhongshan Hospital, Fudan University. CA199:101.0 U/ml, AFP: 4.5 ng/ml. Abdominal CT showed multiple space-occupying lesions in the liver, PET-CT showed multiple MTs, hilar lymph node metastasis in the liver, and cervical lymphadenitis. Liver mass puncture was performed, On April 7, 2021, pathology report showed: consider poorly differentiated carcinoma, and it is recommended to consider primary poorly differentiated carcinoma of the liver after clinical exclusion of metastasis. Immunohistochemistry: Hepa (partially weak+), ARG-1 (−), CK7 (−), CK19 (+), CK20 (−), CDX2 (bits of weak +), p63 (−), p40 (−), SATB2 (weak+), Ki-37 (80% positive), Syn (−), CgA (−), CD56 (−), GATA3 (weak+), PAX8 (−), TTF-1 (−), NapsinA (−), a-Inhibin (−), S-100 (−), SF1 (+), ER (−), PR (−), CK {pan} (+), CK8 (+), SALL4 (individual weak +), CD30 (−), PAX-5 (−), SMA (−), Des (weak +), HMB-45 (−), AFP (−), LCA (lymphocyte +), OCT-4 (−), PLAP (−), CD34 (−). The patient did not receive further treatment. Two weeks ago, the patient developed gradually aggravated abdominal pain, yellow sclera and yellowish skin all over the body, with skin itching. The patient visited to our department for further treatment, and was admitted to the outpatient department for liver malignant tumor. The patient had a history of diabetes for 1 year and was regularly treated with 1 tablet of metformin (Tid) and 1 tablet of acarbose (Tid) orally. Physical examination on admission: right upper quadrant tenderness +, no rebound tenderness, no enclosed mass, negative Murphy's sign, and negative shifting dullness.
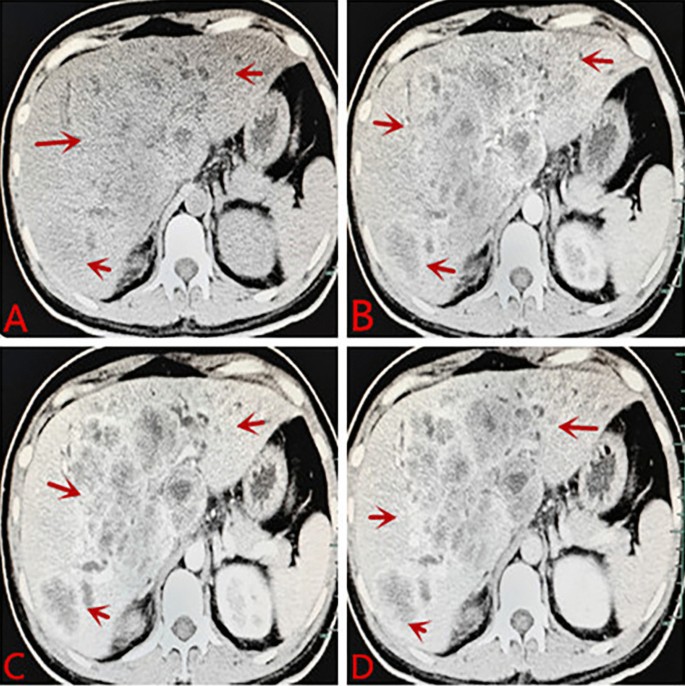
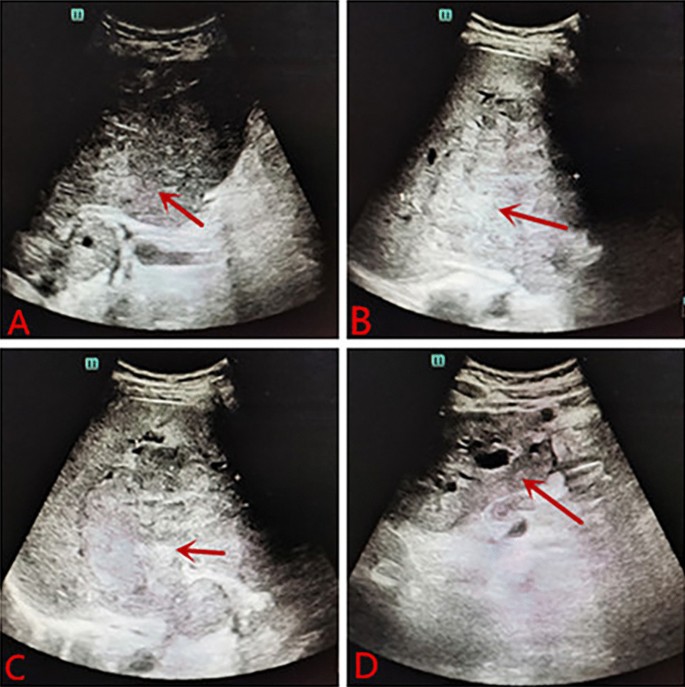
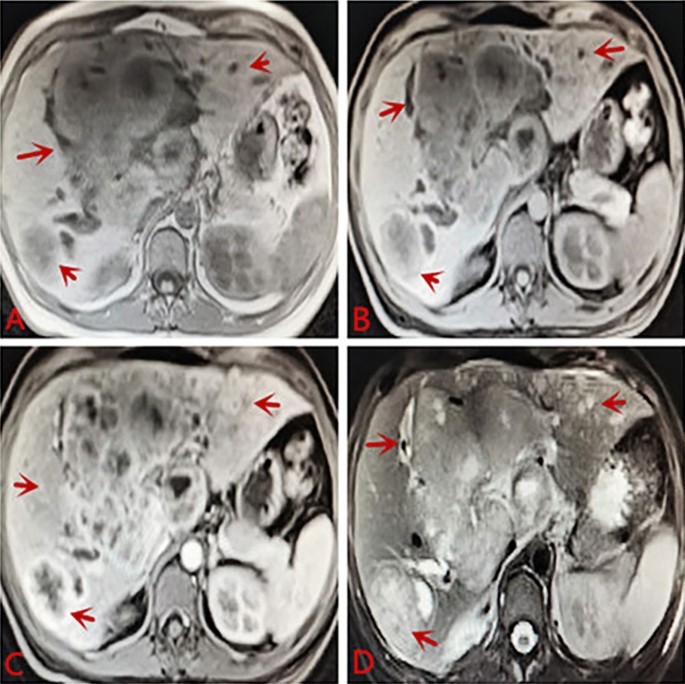
Laboratory tests after admission: liver function: alanine aminotransferase 242 U/L, aspartate aminotransferase 404 U/L, r-glutamyltransferase 1516 U/L, total protein 63.4 g/L, albumin 27.6 g/L, globulin 35.8 g/L, total bilirubin 308.2 µmol/L, conjugated bilirubin 224.9 µmol/L, indirect bilirubin 83.3 µmol/L, lactate dehydrogenase 3433 U/L, C-reactive protein 23.5 mg/L, and HbA1c glycosylated hemoglobin 6.4%. Blood coagulation routine: prothrombin time 15.1 s, international normalized ratio 1.42, D-dimer 350.0 µg/L. Blood routine: WBC: 12.7 * 109/L, NEU: 81.9%, hemoglobin: 89 g/L, RBC: 3.48 * 1012/L, PLT: 593 * 109/L. Chest CT: pulmonary nodules, exudation in both lower lobes, bilateral pleural reactions, a small amount of right pleural effusion. Contrast-enhanced CT of the abdomen: diffuse mass-like and nodular slightly hypodense lesions, some of which were fused, with significant ring enhancement in the arterial phase, continuous ring enhancement in the venous and delayed phases, and local wall thinning and irritability in the right and left branches of the portal vein. The hepatobiliary ducts were dilated, and the gallbladder wall was thickened and edematous. Malignant tumors were considered, with a high possibility of hepatocellular carcinoma or cholangiocarcinoma, with local invasion of the right and left branches of the portal vein, hilar lymphadenopathy, and a small amount of ascites (see Fig. 1). Abdominal ultrasound: multiple hypoechoic masses in liver, possibility of liver cancer, irritable gallbladder wall, hypoechoic nodules in front of the pancreas, considering enlarged lymph nodes (see Fig. 2). Contrast-enhanced MR of the liver: diffuse nodular mass shadows in the liver, and contrast-enhanced scans showed mild enhancement of nodular mass shadows and ring-like enhancement changes. Consider malignant tumor combine with intrahepatic multiple metastases, the left branch of the portal vein was not clearly displayed, consider possible involvement; the right branch of the portal vein was suspect been locally invaded, the hepatic vein and the bile duct in the hilar area were not clearly displayed, the bile duct at the upper level was slightly dilated, the left upper quadrant was turbid, with the possibility of local nodules (see Fig. 3).
A Plane CT scan indicates less regular shape of liver, diffuse mass-like and nodular slightly hypodense lesions, some of which were fused. B Contrast-enhanced CT: significant ring enhancement in the arterial phase. C, D Continuous ring enhancement in the venous and delayed phases, local wall thinning and irritability in the right and left branches of the portal vein. Consider malignant tumors, a high possibility of hepatocellular carcinoma or cholangiocarcinoma, with local invasion of the right and left branches of the portal vein, hilar lymphadenopathy, and a small amount of ascites
A Plain MRI scan: increased liver volume with multiple nodules and mass shadows inside, showing slightly long T1 and slightly long T2 signals, liquefaction necrosis changes were observed in the center of the lesion, and some lesions appeared to be fused. B–D Contrast-enhanced scans showed mild enhancement of nodular mass shadows and ring-like enhancement changes. Consider malignant tumor combine with intrahepatic multiple metastases. The left branch of the portal vein was not clearly displayed, consider possible involvement. The right branch of the portal vein was suspect been locally invaded, the hepatic vein and the bile duct in the hilar area were not clearly displayed, the bile duct at the upper level was slightly dilated, the left upper quadrant was turbid, consider the possibility of local nodules
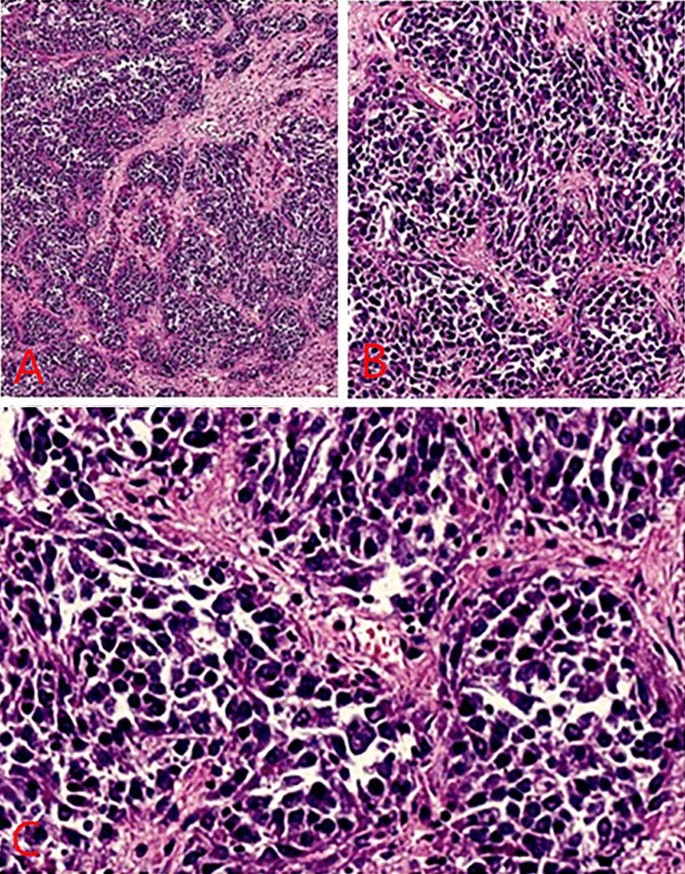
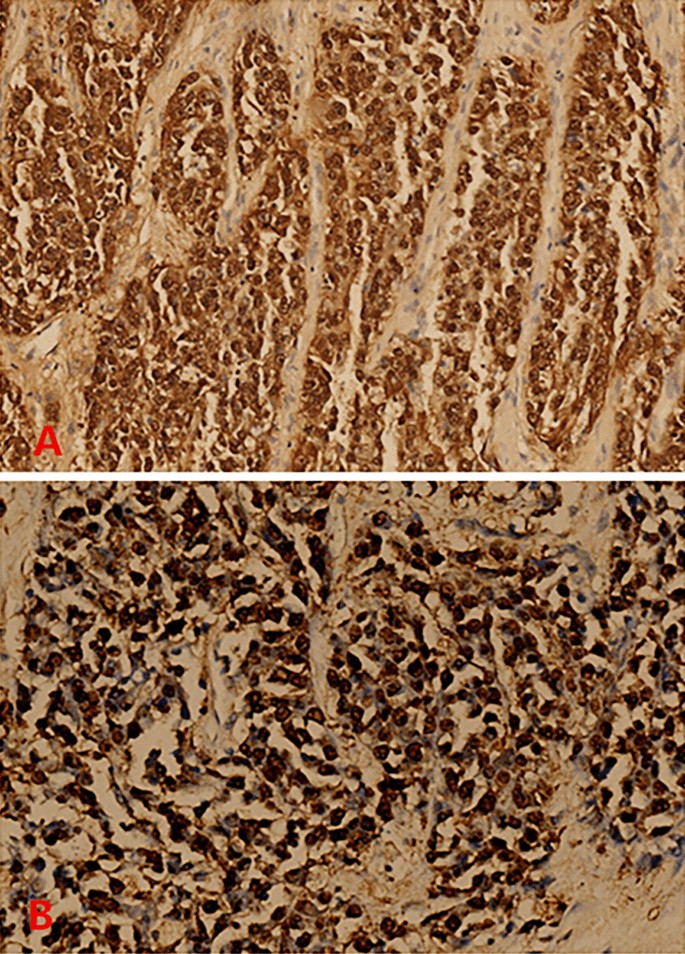
The patient was given ademetionine 1000 mg Qd for choleresis treatment, vitamin K1iInjection 30 mg Qd for thromboprophylaxis, cefoperazone sodium and sulbactam sodium injection 2g Q8h for anti-infection. Transfusion of type O RH positive suspended red blood cells was given to repair anemia and coagulation abnormalities. On May 1, 2021, ultrasound-guided biliary drainage was performed for jaundice reduction treatment, and the right bile duct PTCD conditions were immature. After surgery, the PTCD drainage tube was patent, and the icteric skin and sclera gradually improved. Liver puncture pathology revealed infiltrative growth of significant heterocyst nests in the liver tissue, which was morphologically consistent with malignant tumors, and poorly differentiated carcinoma was considered. Pathology suggestion: combining liver puncture with morphology, immunohistochemistry, and EBV in situ hybridization results, it was consistent with EB virus-associated poorly differentiated carcinoma (See Fig. 4). Consider EBV infection-associated poorly differentiated cholangiocarcinoma (LELC morphology). Immunohistochemical results: CK7 foci (+), CK18 (weak + - +), CK19 (weak + - +), CK20 (−), CDX2 (weak + - +), AFP (−), Hepar1 (−), Arg-1 (−), GATA-3 (−), Vim (-), P40 a little (+), CD117 (−), CerbB2 (−), Ki-67 (+) 80%-90%, EBV in situ hybridization: tumor cells EBER (+) (Fig. 5).
A Lymphoepithelioma-like carcinomas (staining, H&E; magnification, × 40). B High-power view of the same portion (staining, H&E; magnification, × 100). C Further high-power view revealed infiltrative growth of significant heterocyst nests in the liver tissue, which was morphologically consistent with malignant tumors, consider poorly differentiated carcinoma. (staining, H&E; magnification, × 200)
A Immunohistochemical results: CK7 foci (+), CK18 (weak + - +), CK19 (weak + - +), CK20 (−), CDX2 (weak + - +), AFP (−), Hepar1 (−), Arg-1 (−), GATA-3 (−), Vim (−), P40 a little (+), CD117 (−), CerbB2 (−), Ki-67 (+) 80–90%, EBV in situ hybridization: tumor cells EBER (+). Combining liver puncture with morphology, immunohistochemistry, and EBV in situ hybridization results, it was consistent with EB virus-associated poorly differentiated carcinoma (magnification, × 100). B Consider EBV infection-associated poorly differentiated cholangiocarcinoma (LELC morphology) magnification, × 200)
The Department of Infectious Diseases was invited for consultation, and the patient's pathology suggested EBV-related tumor. Upon inquiry of medical history, the patient often had fever from an early age, accompanied with tonsillitis and pus moss. The fever could be controlled after the use of antipyretics. The tonsils had been removed in 2015. In summary, EBV infection could be diagnosed. The patient was given intravenous drip of phosphopotassium sodium chloride injection (tolerable) 3g Q12h for antiviral symptomatic treatment. He was transferred to Shulan Hospital for liver transplantation. The patient underwent liver transplantation in Hangzhou Shulan Hospital on June 8, 2021, and the operation was successful. The pathology revealed EBV-related poorly differentiated cholangiocarcinoma. Regional lymph nodes: (groups 7, 8 and 9) 7/8 lymph node cancer metastases. After surgery, the patient orally took tacrolimus for anti-rejection, entecavir for antiviral therapy, gemcitabine 1.2 g combined with cis-platinum 30 mg for chemotherapy. With followed up for more than 5 months after liver transplantation, and the condition of the patient deteriorated. The patient is in critical condition currently, and the patient's family had given up treatment. The patient subsequently died. See Table 1 for patient condition and treatment process, and abbreviations
Discussion
Cholangiocarcinoma (CCA) is a malignant tumor arising from the biliary epithelium and its surrounding glands and is relatively rare, however, EB virus-associated CCA is even rarer and its prognosis is extremely poor. For special types of CCA, if the diagnosis is made early, early surgical treatment or combination with systemic chemotherapy and other regimens may delay the development of the disease and prolong survival. WAKIZAKA K et al believed that the laboratory and imaging features of CCA were: elevated serum CA199, insignificant elevation of AFP, no previous history of hepatitis B, a low-density mass in the liver by CT, ring enhancement in the arterial phase, and heterogeneous enhancement of the tumor in the delayed phase. Ring enhancement of the liver lesion mass was observed on MRI [26]. In this case, the patient's clinical symptom was abdominal pain, and the laboratory test results revealed CA199:101.0 U/mL and AFP: 4.5 ng/mL. There was no history of hepatitis B. Contrast-enhanced CT of the abdomen revealed diffuse mass-like and nodular slightly hypodense lesions with significant ring enhancement in the arterial phase and continuous ring enhancement in the venous and delayed phases, showing typical imaging findings of intrahepatic cholangiocarcinoma, which was consistent with previous references. MRI examination of the liver can be used to assess the infiltration of the tumor along the extension of the biliary tract. Contrast-enhanced MRI of the liver in this patient revealed mild enhancement of diffuse nodular mass shadows and ring-like enhancement changes on contrast-enhanced scans. It conforms to previous references.
EBV is a herpes virus and a widespread DNA virus. After individuals are infected with EBV at an early age, the virus often persists in oropharyngeal tissue, cervical epithelium and lymphocytes. Malignant tumors associated with EBV infection mainly include nasopharyngeal carcinoma, lymphoma and gastric cancer [27]. However, whether there is an association between EBV infection and hepatocellular carcinoma development has rarely been reported. Randbawa PS et al have reported the presence of EBV in the recipient liver of liver transplantation. EBER-1 is the RNA encoded by EBV during the latent infection period. The authors used in situ hybridization to detect EBER-1 in liver cancer tissues, suggesting that EBV invasion also occurs in the liver. Since EBER-1 is not found in the liver tissues, including cirrhotic tissues and atypical hyperplastic hepatocytes, it is considered that EBV infection occurs after hepatocyte carcinogenesis [28]. Howe JG et al believed that EBV in HCC cells could promote cell proliferation, and EBER-1 positive cases were seen in poorly differentiated hepatocellular carcinoma, but dysplasia hepatocytes were negative, so it was concluded that EBER-1 promoted the progression of HCC, and HCC associated with EBV infection might be expanded from an EBV-infected cell clone [29]. Domestic scholars have reported that with the progression of HBV-related liver diseases (including hepatitis B, hepatitis B cirrhosis and liver cancer), the positive rate of EB virus antibody is significantly increased, and EB virus antibody positive patients have a poor prognosis and a high mortality rate [30]. Xuemin Wang et al., some Chinese scholars, has reported that EBV infection has certain correlation with the occurrence and development of CCA. It is believed that the positive expression rate of LMP-1 is related to the differentiation degree of CCA cells. The lower the differentiation degree, the higher the positive expression rate. It is speculated that poorly differentiated carcinoma allows EBV amplification in poorly differentiated carcinoma of the bile duct. The expanded EBV can endow the growth advantage of the tumor and promote the proliferation of cancer cells, resulting in the invasion and development of the tumor [6]. Pathological findings in this case suggested that EBV infection-associated poorly differentiated cholangiocarcinoma (LELCs) was poorly differentiated hepatocellular carcinoma, and the patient often had fever, tonsillitis, and pus moss at an early age. The tonsils were removed in 2015. In summary, it could be diagnosed as EBV infection. The prognosis of this patient was poor, and the condition of this patient was consistent with previous reports in the literature.
In this case, although the pathology suggested EBV infection-associated poorly differentiated cholangiocarcinoma (LELC), the pathological section of the patient showed less lymphocyte infiltration in the tumor background, and the tumor cells showed diffuse and consistent expression of EBER. Hsu et al have reported the pathology of the first patient with undifferentiated LELC, and it may be difficult to diagnose CCA complicated by LELC type due to the heterogeneity of tumor components [7]. Labgaa I et al believed that LELC was usually associated with EBV infection, studied showed that, in 28 cases of lymphoepithelioma-like CCA patients, 92% were Asian, and the 5-year survival of patients with lymphoepithelioma-like CCA was longer than that of patients with simple CCA (100% vs. 13.2%) [31]. Austin Lin et al have reported that two patients with intrahepatic CCA of LELC (African descent), could not undergo surgery due to tumor progression, and had a poor prognosis [32]. In this case, the patient was young, and although liver transplantation, systemic chemotherapy and other tumors were performed, the progression was rapid and the prognosis was still poor. It is consistent with the report of Austin Lin et al.
Because the rarity of special types of CCA cases, there is no uniform regimen for the treatment of this type of disease, and the prognosis varies among treatment regimens. O'Connor et al concluded that special types of CCA should be actively treated through surgery and chemotherapy [33]. Nakhoul et al. believed that antiviral therapy was required for the treatment of hepatic EBV-associated tumors, and the commonly used antiviral drugs were ganciclovir and acyclovir [4]. Austin Lin et al believed that FOLFOX chemotherapy regimen could be given to patients who could not undergo surgical treatment [32]. Labgaa et al. believed that (PDL-1) inhibitors was available for nasopharyngeal carcinoma treatment, so they were also effective for patients with EB virus-associated LELCCCA. In this case, the patient's treatment regimen was: liver transplantation, entecavir for antiviral therapy, gemcitabine 1.2 g combined with cis-platinum 30 mg for chemotherapy. After more than 5 months of follow-up after liver transplantation, the patient died with deteriorated condition. Combined with the clinical data of this patient, EBV infection-related CCA has a poor prognosis and a high mortality rate.
Conclusion
In summary, when the patient's serum CA199 increased, AFP did not change significantly, and there was no previous history of hepatitis B. CT revealed a low-density mass in the liver, ring enhancement in the arterial phase, and heterogeneous enhancement of the tumor in the delayed phase. Ring enhancement of the liver lesion mass was observed on MRI. The possibility of hepatic CCA should be considered. When patients have recurrent tonsillitis at an early age, EBV virus infection should be vigilant and oropharyngeal tissue should persist, EBV in liver cancer cells has a role in promoting cell proliferation, and the prognosis is often poor. For patients with suspected CCA, EB virus immunohistochemical detection is recommended during liver biopsy for early detection and treatment. Antiviral treatment can be combined with antiviral surgery, as well as chemotherapy when necessary. The mechanism of infection of CCA by EBV is unknown. Considering the small number of cases, this conclusion needs to be confirmed by further studies.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- PET:
-
Positron emission tomography
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- CA 19-9:
-
Carbohydrate antigen 19-9
- MRI:
-
Magnetic resonance imaging
- LELC:
-
Lymphoepithelioma-like carcinomas
- LELCC:
-
Lymphoepithelioma-like cholangiocarcinoma
- HCC:
-
Hepatocellular carcinoma
- EBV:
-
Epstein–Barr virus
- CCA:
-
Cholangiocarcinoma
References
Forner A, Reig M, Bruix J. Hepatocellular carcinoma. The Lancet. 2018;391(10127):1301–14.
Kirstein MM, Wirth TC. Multimodale therapie des hepatozellularen karzinoms. Sci Der Internist. 2020;61(2):164–9.
Lezzqni JC, Gaffey MJ, Weise LM. The role of Epstein-barr virus in lymphoepithelioma-like carcinomas. Am J Clin Pethol. 1995;1103(11):308–15.
Young LS, Rickinson AB. Epstein-Barr virus: 40 years on. Nat Rev Cancer. 2004;4:757–68.
Ortiz MR, Garijo G, Adrados M, et al. Epstein-Barr virus associated cholangiocarcinoma with lymphoepithelioma-like component. Int J Surg Pathol. 2000;8:347–51.
Wang X, Dou K, Youchi F. Expression of latent membrane protein-1 of EBV in cholangiocarcinoma. Med J Chin People’s Armed Police Forces. 2022;11:78–80.
Hsu HC, Chen CC, Huang GT. Clonal Epstein-Barr virus associated cholangiocarcinoma with lymphoepithelioma-like component. Hum Pathol. 1996;27:848–50.
Iezzoni JC, Gaffey MJ, Weiss LW. The role of Epstein-Barr virus in lymphoepithelioma-like carcinomas. Am J Clin Pathol. 1994;103:308–15.
Henderson-Jackson E, Nasir NA, Hakam A, Nasir A, Coppola D. Primary mixed lymphoepithelioma-like carcinoma and intrahepatic cholangiocarcinoma: a case report and review of literature. Int J Clin Exp Pathol. 2010;3:736–41.
Adachi S, Morimoto O, Kobayashi T. Lymphoepithelioma-like cholangiocarcinoma not associated with EBV. Pathol Int. 2008;58:69–74.
Chen TC, Ng KF, Kuo T. Intrahepatic cholangiocarcinoma with lymphoepithelioma-like component. Mod Pathol. 2001;14:527–32.
Hur YH, Kim HH, Koh YS, Seoung JS, Cho CK. Lymphoepithelioma- like cholangiocarcinoma not associated with Epstein-Barr virus. ANZ J Surg. 2011;81:652–3.
Huang Y, Tsung JS, Lin CW, Cheng TY. Intrahepatic cholangiocarcinoma with lymphoepithelioma-like carcinoma component. Ann Clin Lab Sci. 2004;34:476–80.
Jeng YM, Chen CL, Hsu HC. Lymphoepithelioma-like cholangiocarcinoma: an Epstein-Barr virus-associated tumor. Am J Surg Pathol. 2001;25:516–20.
Lee W. Intrahepatic lymphoepithelioma-like cholangiocarcinoma not associated with Epstein-Barr virus: a case report. Case Rep Oncol. 2011;4:68–73.
Szekely E. Lymphoepithelioma-like cholangiocarcinoma (LELC) not associated with Epstein-Barr virus. Am J Surg Pathol. 2001;25:1464–6.
Kim YB, Park YN, Han JY, Hong KC, Hwang TS. Biliary lymphoepithelioma-like carcinoma not associated with Epstein-Barr virus. Arch Pathol Lab Med. 1999;123:441–3.
Vortmeyer AO, Kingma DW, Fenton RG, Curti BD, Jaffe ES, Duray PH. Hepatobiliary lymphoepithelioma-like carcinoma associated with Epstein-Barr virus. Am J Clin Pathol. 1998;109:90–5.
Chan AWH, Tong JHM, Sung MYM, Lai PBS, To K-F. Epstein-Barr virus-associated lymphoepithelioma-like cholangiocarcinoma: a rare variant of intrahepatic cholangiocarcinoma with favourable outcome. Histopathology. 2014;65(5):674–83.
Iizasa H, Nanbo A, Nishikawa J, Jinushi M, Yoshiyama H. Epstein-Barr virus (EBV)-associated gastric carcinoma. Viruses. 2012;4:3420–39.
Lo KW, Chung GT, To KF. Deciphering the molecular genetic basis of NPC through molecular, cytogenetic, and epigenetic approaches. Semin Cancer Biol. 2012;22:79–86.
Fukayama M. Epstein-Barr virus and gastric carcinoma. Pathol Int. 2010;60:337–50.
Kwong J, Lo KW, Chow LS, et al. Epigenetic silencing of cellular retinol-binding proteins in nasopharyngeal carcinoma. Neoplasia. 2005;7:67–74.
Matusnou H, Konishi F, Hori H, et al. Characteristics of Epstein-Barr-virus-associated gastric carcinoma with lymphoid stroma in Japan. Cancer. 1996;77:1998–2004.
Chen FF, Yan JJ, Lai WW, et al. Epstein-Barr virus-associated non-small lung carcinoma: Undifferentiated ‘lymphoepitheliomalike’ carcinoma as a distinct entity with better prognosis. Cancer. 1998;82:2334–42.
Wakizaka K, Yokoo H, Kamiyama T, et al. Clinical and pathological features of combined hepatocellular- cholangiocarcinoma compared with other liver cancers. J Gastroenterol Hepatol. 2019;34(6):1074–80.
Nakhoul H, Lin Z, Wang X, et al. High-throughput sequence analysis of peripheral T-cell lymphomas indicates subtype-specific viral gene expression patterns and immune cell microenvironments. mSphere. 2019;4(4):e00248-19.
Randbawa PS, Jaffe R, Demetris AJ, et al. Expression of Epstein-Barr virus-encoded small RNA (by the EBER-1 gene) in liver specimens from transplant recipients with post-transplantation lymphoproliteratlve disease. N Engl J Med. 1992;327:1710.
Howe JG, Steitp JA. Location of Epstein-Barr virus-encoded small RNAs by in situ hybridization. Proc Natl Acad Sci USA. 1986;83:9006.
An H, Zhou X. Clinical study on the relationship between EBV infection and liver diseases infected by HBV. Zhong Xi Yi Jie He Gan Bing J. 2005;15(3):144.
Labgaa I, Stueck A, Ward SC. Lymphoepithelioma-like carcinoma in liver. Am J Pathol. 2017;187:1438–44.
Lin A, Alpert L, Hart J, et al. Lymphoepithelioma-like carcinomas: a rare variant of cholangiocarcinoma. Hepatology. 2020;72(1):353–5.
O’Connor K, Walsh JC, Schaeffer DF. Combined hepatocellular-cholangiocarcinoma (cHCC-CC): a distinct entity. Ann Hepatol. 2014;13(3):317–22.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
XZ and NW: conceptualization, methodology, formal analysis, investigation, writing—review and editing original draft. These authors contributed equally to this work. WW: validation, investigation. YL: investigation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors. Our hospital does not need ethics approval number when publishing a case report. The study obtained written informed consent from the patient. The patient details have been de-identifed.
Consent for publication
All authors have reviewed and agreed to publish.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, X., Wang, N., Wei, W. et al. Epstein-Barr virus infection-associated cholangiocarcinoma: a report of one case and the review of literature. Virol J 19, 133 (2022). https://doi.org/10.1186/s12985-022-01862-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-022-01862-7