Abstract
Background
Human papillomavirus (HPV) infection is the leading cause of genital diseases. It can cause a series of cervical lesions. The distribution of HPV genotypes indicates that the increased prevalence of high-risk HPV (HR-HPV) is positively correlated with the severity of cervical lesions. In addition, persistent HR-HPV infection is associated with the risk of cervical cancer. Considering the latest approval of homemade HPV vaccine in China and the prevalence of HPV distribution, this is of great significance for guiding HPV vaccination work.
Objective
Our study’s purpose was to examine trends of cervical HPV infection rate in each 5-year age group from 2011 to 2019.
Methods
Retrospective analysis of human papillomavirus prevalence rate of 59,541 women from 2011 to 2019 in the District Zhoupu of Shanghai City in China. HPV genotype testing is performed using a commercial kit designed to detect 15 high-risk HPV genotypes and 6 low-risk HPV genotypes. Trends were examined for each 5-year age group.
Results
In the District Zhoupu of Shanghai City in China, the prevalence rate of cervical HPV increased significantly among women aged 15–34 years. The most prevalent HR-HPV genotypes were 52, 16, 58, 53, 39, and 51.
Conclusion
Cervical HPV prevalence rate is very high in younger women in suburb Shanghai. Due to significant differences in infection rates between specific age groups and HPV subtypes, timely intervention is required for these vulnerable populations.
Similar content being viewed by others
Introduction
Cervical cancer is the fourth most common cancer among women worldwide and the fourth leading cause of cancer-related deaths [1]. Persistent human papillomavirus (HPV) infection, especially high-risk HPV (HR-HPV) infection, is the main cause of precancerous lesions and cervical cancer [2, 3], and is closely related to cervical and reproductive tract cancers [4]. However, the prevalence of HPV infection remains at a high level in China. In China alone, it is estimated that 98,900 cervical cancer cases, accounting for approximately 20% of total new cases globally, and nearly 30,500 cervical cancer deaths occur each year [5].
A meta-analysis made by Li et al. showed that the overall infection rate of HR-HPV in mainland Chinese women was 19.0% [6] and the national overall prevalence of HPV infection was 15.54% [7]. Some studies have investigated the HPV infection rate and the genotype distribution of Shanghai China in Minhang district [8], female [9] and male [10] patients in the Songjiang district. Our study’s purpose was to examine trends in HPV prevalence from 2011 to 2019 in the District Zhoupu of Shanghai City in China, among each 5- year age group, comparing prevalence rates.
Methods
Data source
We extracted 59,541 women data on HPV prevalence in China at Shanghai Zhoupu Hospital from 2011 to 2019. The data is in the form of 5-year age groups. As a regional medical center, Shanghai Zhoupu Hospital provides medical and health services for about 500,000 people in nearby districts and towns.
Ethics statement
This study was approved by the Institutional Medical Ethics Review Board of Zhoupu Hospital in Shanghai City. The participant received informed consent. For participants under the age of 18, the parents signed a consent form. Confidentiality was ensured during the data collection process at Zhoupu Hospital. Data is analyzed anonymously.
HPV genotyping
By using Human papillomavirus (HPV) typing test kits (PCR + membrane hybridization) analysis, HPV genotyping was performed on the collected specimens. This assay has been approved by the Chinese FDA (Certification Number (2014): 3402188).
PCR membrane hybridization was used to detect 21 HPV genotypes (6,11,16,18,31,33,35,39,42,43,44,45,51,52,56,58,59,66,68 and 81) by reverse dot hybridization and envelope specific probe membrane hybridization. Sample collection and DNA extraction were the same as PCR fluorescence method. The PCR mix, Taq enzyme and DNA template were mixed in proportion with the typing test kit provided by China Chaozhou Hybribio biochemistry Co., Ltd. (Stock code: 300639.SZ). Amplification parameters were: 95 °C 9 min, 40 cycles (95 °C 20s, 55 °C 30s, 72 °C 30s), 72 °C 5 min. All outcomes were used in the hybridization process. After color rendering, the positive test results were clear blue and purple dots. According to the distribution of HPV types in membrane strips, the positive points were determined. Negative and positive control were set up in the whole process. Internal quality control and external quality assessment was taken in the experiment and the results met the requirements.
Statistical analysis
All HPV data from 2011 to 2019 were entered into an Excel spreadsheet and then analyzed on the R platform (www.r-project.org) (v3.2.0) and R packages, and the overall and type-specific prevalence of HPV were calculated. All genotypes from single and multiple infections were computed individually. These data were also stratified by age(< 20 years, 20–24 years, 25–29 years,30–34 years, 35–39 years,40–44 years, 45–49 years, 50–54 years, 55–59 years, 60–64 years, 65–69 years,70–74 years, 75–79, years 80–84 years, ≥85 years). The HPV prevalence rate was estimated by a proportion and summarized as a percentage. The secular trends for HPV subtypes and for HPV infection rates of different ages were calculated using student t-test. p < 0.05 was considered statistically significant.
Results
Characteristics of the study participants
In this study, a total of 59,541 women from Shanghai Zhoupu Hospital, underwent outpatient gynecological examinations and met the participation criteria. The ages of the participants were between 15 and 94 years. The mean age was 37.49. Among the 59,541 subjects, 10,670 women were positive for HPV infection, with a total HPV infection rate of 17.92% (10,670 / 59,541) and a HR-HPV positive rate of 15.56% (9263 / 59,541). Therefore, 86.81% of the infections were caused by HR-HPV.
The six most prevalent HR-HPV genotypes were HPV 52, 16, 58, 53, 39, and 51; however, the top three LR-HPV genotypes were HPV 81,6 and 11. (Table 1).
Trends of different HPV subtype infection rates
Among these 21 HPV subtypes examined, HPV 52, 16, and 58 were also most commonly seen in women both with single-type and multiple-type HPV infections (Table 1). Here, HPV subtype infection rate is calculated as the ratio of the number of HPV subtype infections to the total number of participants in this study (N = 59,541).
We investigated the temporal trend of HPV subtype infection. From 2011 to 2019, HPV16, 52, and 58 infection rates were higher. Except for HPV43, there are significant differences in secular trends for most HPV subtypes from 2011 to 2019 (P < 0.05, Table 2).
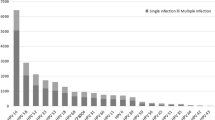
Trends of single-type and multiple-type HPV infection rates
Single HPV genotype infection was found to be the most common pattern (72.32%, 7717/10,670). The multiple genotype infection rate was 27.68% (2953/10,670). Single-type infection (72.32%) was more common than multiple-type infection (27.68%). And the most mixed infection included 9 genotypes(Table 3).
Secular trends of the number of HPV single-type infection and multiple-type infection were also calculated. We found that the HPV numbers of single-type infection and some of multiple-type (2–5,7) infection rates among women showed significant differences from 2011 to 2019 (all P < 0.05, Table 4).
Trend analysis stratified by 5-year age groups from 2011 to 2019
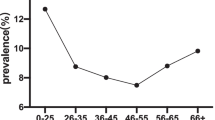
For women aged < 55 years, the highest prevalence numbers occurred in 2017, and the prevalence rate decreased from then. Prevalence number of HPV was significantly higher in women aged 25–34 years in Fig. 1a, in contrast to women older than 65 years in Fig. 1c.
Secular trends of HPV infection rates of different ages were also calculated. We found that HPV positive rates among women aged < 80 years also showed significant differences from 2011 to 2019 (all P < 0.05, Table 5).
Discussion
Our study analyzed HPV prevalence trends of Zhoupu district in Shanghai city from 2011 to 2019. While the overall trend demonstrated there was an increase in prevalence rate, women aged < 55 years in 2017 experienced the highest infection numbers, and a decline in HPV infection rate from 2018 to 2019. Zhoupu district is located in the suburb of Pudong New Area, Shanghai City of China. According to the analysis report of Pudong’s population development in 2017 issued by the development and Reform Commission of Pudong New Area Government in Shanghai, there is a significant increase in the population development situation. So, the number of patients seeking medical treatment in the Zhoupu area also increases. The main reasons may be as follows: first, with the implementation of the two-children policy, the number and proportion of the two children have increased steadily; second, a large number of floating populations have gathered in the suburbs; third, the population ageing has deepened.
Single-type HPV infection and some of multiple-type (2–5,7) infection rates among women showed significant differences. HPV prevalence trends stratified by 5-year age groups demonstrated that HPV positive rates among women aged < 80 years also showed significant differences.
In the 59,541 outpatient women, the overall prevalence of HPV was 17.92% and the HR-HPV prevalence was 15.56%. Compared with similar studies in China, the prevalence in our study was higher than that in Xinjiang (14.02%) [11], Urumqi (16.74%) [12], Zhejiang (17.6%) [13], and Nanjing KingMed Diagnostics (17.7%) [14], but lower than that in Meizhou (18.34%) [15], Wuhan (18.6%) [13], Beijing (20.16%) [4], Guangdong (21.06%) [16] Shandong (28.4%) [17], and three cities (Xuzhou, Nanjing and Suzhou) of Jiangsu Province (26.92%) [18]. Different HPV prevalence rates may be a combination of different economic levels, cultural diversity, geographic locations, and survey periods.
Analysis of HPV prevalence indicates that the most common HR-HPV genotypes in outpatient women are HPV 52,16,58,53 and 39. These are the same common genotypes as Meizhou [15]. This is similar to other studies conducted in China. HPV 16,58, 52, 53, and 39 were the dominant subtypes in Jiangsu [14]. HPV 52,16 and 58 had a higher prevalence in Beijing [4]. HPV 52, 16, 58, CP8304, and 53 were the dominant subtypes among gynecological outpatients among women in Guangdong, China 2008 to 2017 [16]. The most common HR-HPV group included HPV types 16, 31, 33, 35, 52, and 58 in Zhejiang and Wuhan [13]. HPV 16, 52, 58, 51, and 56 were the five most common HR-HPV genotypes in Shandong [17]. The most prevalent genotypes were HPV 16, 52,58,53 and 31 in Xinjiang [11]. From the analysis of 303 China-specific articles, the top 4 common HPV types were detected HPV 16, 18, 58, 52 in descending order of frequency [7]. The top 5 subtypes with the highest infection rates were 16, 52, 58, 53, and 18 in a systematic review of the epidemiology of HR-HPV infections in mainland Chinese women from January 2000 to June 2018 [6]. Among all these studies above, HPV 52, 16 and 58 were the most common subtypes found, so vaccines against HPV 52, 16 and 58 should be developed for Chinese women.
Our research shows that HPV prevalence of women in Zhoupu District of Shanghai is age-related and single-type was more common than multiple-type HPV infection. The same is true in the rest of China, such as Guangdong and Beijing [4, 16]. Single-type was more common; however, multiple-type HPV infections are more dangerous than single-type infections. The HPV infection reached a peak in women aged 25–29 years. Perhaps because women in this age group are more sexually active and have more than one sexual partner, so HPV infection rates are higher than in other age groups. Our study may provide valuable data to inform cervical cancer screening and HPV vaccination programs for women in Shanghai.
Our research has an important policy implication: it is necessary to vaccinate Chinese women nationwide, especially young women, against HPV infection. Injecting HPV vaccine can induce a durable anti-HPV response and prevent HPV infection. At present, China has 2- and 4-valent HPV vaccines, and 9-valent vaccines in some regions (since May 2018). However, the proportion of women who are willing to take the initiative to receive the HPV vaccine is still very low, and various measures are urgently needed to increase the vaccination rate in China.
Our research focuses on the prevalence of HPV in different HPV-subtype-related and age-related groups, which allowed us to identify trends in differences in 2011–2019. However, our study also has some limitations. Although Zhoupu Hospital is the largest public hospital in the local area, it is located in the suburbs. These areas have large population mobility and relatively poor data quality.
In the future, we plan to examine the relationship between the mortality rate of cervical cancer and the HPV prevalence in Shanghai Zhoupu district. And we will compare it with the two databases from the World Health Organization Cancer Mortality Database (International Agency for Research on Cancer, Lyon, France) and China Health Statistical Yearbooks, like what Min did [5].
Conclusions
In conclusion, we conducted a population-based study on the prevalence of HPV-subtype-related and age-related groups in the Zhoupu area of Shanghai. The cervical HPV prevalence rate is very high in younger women aged 25–34 years in suburb Shanghai city. The prevention of HPV-related diseases is challenging. There are significant differences in infection rates between specific age groups and HPV subtypes, and this finding will provide guidance for future vaccination programs and improve their accuracy.
Availability of data and materials
The data were collected from Zhoupu Hospital in Shanghai City. We are grateful for their generous help. The data can be freely shared. The materials were purchased from Hybribio Biotechnology Limited Corp.
Abbreviations
- HPV:
-
Human papillomavirus
- (HR-HPV):
-
High-risk HPV
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Walboomers JMM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJF, Peto J, Meijer CJLM, Muñoz N. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12–9.
Baseman JG, Koutsky LA. The epidemiology of human papillomavirus infections. J Clin Virol. 2005;32:16–24.
Ma L, Lei J, Ma L, Cong X, Wang N, Yang H, Liu Q, Yu Y, Cao Y. Characteristics of women infected with human papillomavirus in a tertiary hospital in Beijing China, 2014–2018. BMC Infect Dis. 2019;19:670.
Wei M, Zhou W, Bi Y, Wang H, Liu Y, Zhang Z-J. Rising mortality rate of cervical Cancer in younger women in urban China. J Gen Intern Med. 2019;34:281–4.
Li K, Li Q, Song L, Wang D, Yin R. The distribution and prevalence of human papillomavirus in women in mainland China. Cancer. 2019;125:1030–7.
Zhou H-L, Zhang W, Zhang C-J, Wang S-M, Duan Y-C, Wang J-X, Yang H, Wang X-Y. Prevalence and distribution of human papillomavirus genotypes in Chinese women between 1991 and 2016: A systematic review. J Infect. 2018;76:522–8.
Wu J, Li X, Liu X, Gao Z. Human papillomavirus genotype prevalence in the women of Shanghai, China and its association with the severity of cervical neoplasia. Int J Clin Exp Pathol. 2018;11:4614–21.
Zhang C, Zhang C, Huang J, Wu Z, Mei X, Shi W. Prevalence and genotype distribution of human papillomavirus among females in the suburb of Shanghai, China. J Med Virol. 2018;90:157–64.
Zhang C, Zhang C, Huang J, Shi W. The genotype of human papillomavirus and associated factors among high risk males in Shanghai, China: a molecular epidemiology study. Med Sci Monitor. 2018;24:912–8.
Wang J, Tang D, Wang K, Wang J, Zhang Z, Chen Y, Zhang X, Ma C. HPV genotype prevalence and distribution during 2009-2018 in Xinjiang, China: baseline surveys prior to mass HPV vaccination. BMC Womens Health. 2019;19:90.
Yao L, Yuan M, Yuan J, Zhou P, Mei L, Cheng J. Analysis of cervical human papillomavirus infection in 2300 women in Urumqi, China. Medicine. 2018;97:e13206.
Wang Y, Meng Y, Li W, Zhang X, Deng Z, Hu M, Shen P, Xu S, Fu C, Jiang W, et al. Prevalence and characteristics of hrHPV infection among 414,540 women: a multicenter study in central and eastern China. J Cancer. 2019;10:1902–8.
Ge Y, Zhong S, Ren M, Ge Y, Mao Y, Cao P. Prevalence of human papillomavirus infection of 65,613 women in East China. BMC Public Health. 2019;19:178.
Liu S, Gu X, Weng R, Liu J, Zhong Z. Positivity and prevalence of human papillomavirus among a large population of women in southeastern China. J Int Med Res. 2019;47:6171–81.
Luo G, Sun X, Li M, Liu T, Hu G, He Y, Mao L, Yan L, Xie L, Zou H, Luo X. Cervical human papillomavirus among women in Guangdong, China 2008-2017: Implication for screening and vaccination. J Med Virol. 2019;91:1856–65.
Jiang L, Tian X, Peng D, Zhang L, Xie F, Bi C, Wang R, Wang J, Qi D. HPV prevalence and genotype distribution among women in Shandong Province, China: Analysis of 94,489 HPV genotyping results from Shandong's largest independent pathology laboratory. PLoS One. 2019;14:e0210311.
Zhang C, Cheng W, Liu Q, Guan Q, Zhang Q. Distribution of human papillomavirus infection: a population-based study of cervical samples from Jiangsu Province. Virol J. 2019;16:67.
Acknowledgements
We thank Hybribio Biotechnology Limited Corp for the partial support of this study. We express our gratitude to those who contributed to the publication of the article. We are grateful to those authors who made available the details of the data from their published articles.
Funding
This project was supported by the Medical Leaders Training Program of Health Bureau of Shanghai Pudong in China (No. PWRq2016–15), Health Bureau of Shanghai in China (No.201740291), National Key R&D Program of China (2018YFB1307700), Collaborative Education Project of Industry University Cooperation (No. 201902004006), the National Natural Science Foundation of China (NSFC, No.81803581), the Program for Professor of Special Appointment (Eastern Scholar) at Shanghai Institutions of Higher Learning-2018, and Collaborative Innovation Key Project SPCI-18-18-003 by SUMHS.
Author information
Authors and Affiliations
Contributions
HPL and PL designed and supervised the research. PQL, LYL, and HPL acquisition of data. HR, LPS and PL analyzed and interpreted the data. HPL and PL prepared the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Medical Ethics Review Board of Zhoupu Hospital in Shanghai City.
Consent for publication
Not applicable. This manuscript does not contain any individual person’s data in any form (including individual details, images or videos.
Competing interests
We declare that we have no financial and personal relationships with other people or organizations that can inappropriately influence our work. The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, H., Li, P., Huang, L. et al. Prevalence characteristics of cervical human papillomavirus (HPV) infection in the Zhoupu District, Shanghai City, China. Virol J 17, 84 (2020). https://doi.org/10.1186/s12985-020-01352-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-020-01352-8