Abstract
Background
Enhancing the quality of life of people with a lower limb amputation is critical in prosthetic development and rehabilitation. Yet, no overview is available concerning the impact of passive, quasi-passive and active ankle–foot prostheses on quality of life.
Objective
To systematically review the therapeutic benefits of performing daily activities with passive, quasi-passive and active ankle–foot prostheses in people with a lower limb amputation.
Methods
We searched the Pubmed, Web of Science, Scopus and Pedro databases, and backward citations until November 3, 2021. Only English-written randomised controlled trials, cross-sectional, cross-over and cohort studies were included when the population comprised individuals with a unilateral transfemoral or transtibial amputation, wearing passive, quasi-passive or active ankle–foot prostheses. The intervention and outcome measures had to include any aspect of quality of life assessed while performing daily activities. We synthesised the participants’ characteristics, type of prosthesis, intervention, outcome and main results, and conducted risk of bias assessment using the Cochrane risk of bias tool. This study is registered on PROSPERO, number CRD42021290189.
Results
We identified 4281 records and included 34 studies in total. Results indicate that quasi-passive and active prostheses are favoured over passive prostheses based on biomechanical, physiological, performance and subjective measures in the short-term. All studies had a moderate or high risk of bias.
Conclusion
Compared to passive ankle–foot prostheses, quasi-passive and active prostheses significantly enhance the quality of life. Future research should investigate the long-term therapeutic benefits of prosthetics devices.
Similar content being viewed by others
Introduction
Lower limb loss is detrimental for physical function and psychosocial health, harming an individual’s quality of life [1, 2]. After lower limb loss, assistive devices are a fundamental part of rehabilitation with the aim to restore daily activities and improve quality of life [3,4,5]. A prosthesis is generally favoured among assistive devices as it enables one to carry out daily activities as naturally as possible [4, 6, 7]. It additionally helps to enhance self-esteem as it ensures that people diverge as little as possible from the physical appearance of able-bodied individuals [8]. Conversely, prostheses may cause falls and secondary injuries, including low back pain and osteoarthritis of the healthy knee and hip, entailing high medical costs and diminishing quality of life [9,10,11,12,13].
Lower limb prostheses also complicate the performance of daily activities. This performance is affected by several factors, including the type of prosthesis, prosthetic embodiment, the level and cause of the amputation, degree of mobility and presence of comorbidities [14, 15]. These factors complicate tasks such as positioning the foot in space, walking horizontally, going up and down ramps and stairs, crossing obstacles, walking on slippery floors and transitioning between activities [16,17,18]. For instance, it has been well-established that walking with a lower limb prosthesis results in aberrations in gait kinetic and spatiotemporal parameters compared to able-bodied walking [19]. These aberrations can be attributed to the loss of sensory feedback and the inability of the prosthetic device to mimic the normal muscular function [19, 20]. As a result, bilateral proximal muscle compensations, increased metabolic cost and secondary injuries (e.g. low back pain, arthritis of the sound knee, bilateral hip osteoarthritis, reduced hip bone density of the amputated limb and muscle atrophy) occur [21,22,23,24,25,26]. Furthermore, people with a lower limb amputation concomitantly show increased structural and functional changes occurring in the brain after an amputation and exhibit a decrease in static and dynamic balance. These unfavourable changes culminate in an increased risk of falling, which leads to reduced quality of life [9, 10, 27, 28]. Besides the physical and biomechanical consequences, the psychosocial impact is equally important and keeps fluctuating throughout the years following amputation [29]. For example, an individual’s functional status has a strong positive influence on overall satisfaction and thus on the quality of life, while the emotional state (i.e., depression and anxiety), body image disturbances, and high pain levels have a negative influence [29, 30]. All these adaptations emphasise the necessity for both short- and long-term research into the effect of ankle–foot prosthetic technological innovations on quality of life.
The current evolution in prosthetic development is shifting from developing passive prostheses to quasi-passive and active prostheses in order to minimise prosthetic related adverse events affecting quality of life [31,32,33,34,35,36]. This critical aspect of lower limb prosthetic development and rehabilitation might be achieved by restoring the quality of life by increasing mobility, improving psycho-sociological negative implications following amputation, and alleviating gait compensations during daily activities as well as better mimicking able-bodied motions [3, 15, 37, 38].
Therapeutic benefits for people with lower limb amputation might thus arise from technological innovations that could improve their quality of life [31,32,33,34,35,36]. Nevertheless, quality of life is an inherently intricate concept, and there seems to be no consensus on a single definition constituting quality of life [39]. There is, however, agreement on its multidimensionality and subjectivity, covering health (i.e., physical, social, mental and emotional functioning) and individuals’ perceptions such as pain, relationships and life satisfaction [39, 40]. Differences in quality of life can be investigated through objective (e.g. performance, biomechanical, physiological) and subjective measurements (e.g. psychosocial) in this population [41,42,43]. Though, no insight is available concerning the impact of passive, quasi-passive and active ankle–foot prostheses on the different dimensions of quality of life. Therefore, the purpose of this study was to systematically review the therapeutic benefits of performing daily activities with passive, quasi-passive and active ankle–foot prostheses in people with a unilateral lower limb amputation.
Methods
Search strategy
The review protocol has been registered in Prospero under CRD42021290189. This systematic review has been reported in compliance with the PRISMA 2020 statement, the PRESS guideline and the PERSiST consensus statement [44,45,46]. A systematic search strategy through four electronic databases (i.e., PubMed, Web of Science, Scopus, and Pedro) was conducted using the PICO acronym (population, intervention, comparison, outcome) on November 3, 2021, followed by a backward reference search. We have not sought and browsed additional data from study registers or other online sources.
Search string
Table 1 provides the search string used across all databases combining the intended population, intervention, and outcome through the Boolean operator “AND”. The search string has been created by one author (EL) and reviewed by two authors (BT & KDP). We limited the search hits to journal articles written in English published later than 2000. The timeframe was chosen as research into the development and evaluation of lower-limb prostheses only started to advance rapidly in the twenty-first century with the introduction of quasi-passive and active ankle–foot prostheses [47,48,49].
Selection criteria
Randomised controlled trials, cross-sectional, cross-over or cohort studies were included. Subjects had to be individuals with a unilateral transfemoral or a transtibial amputation, wearing passive, quasi-passive or active ankle–foot prostheses. We excluded studies on children, and adults with upper limb amputation, bilateral, foot or trans articular knee amputation. The intervention and outcome measures had to include any aspect of quality of life assessed while performing daily activities. Since we aimed at reviewing differences between passive, quasi-passive and active prostheses, we chose to include only articles comparing different ankle–foot prostheses.
Eligibility assessment
Studies collected through the electronic databases for duplicate removal and eligibility were imported into Rayyan (https://rayyan.qcri.org) [50]. Duplicates were removed using Rayyan’s duplicate identification software, and the remaining duplicates were removed manually. Two authors (EL & MAD) performed a two-stage eligibility assessment. Disagreements were resolved upon consensus and a third author (AM) was contacted if a consensus could not be reached. First, screening was conducted on title and abstract for language, study design, population, intervention, and outcome. Subsequently, the remaining eligible articles were screened on full text following the same criteria.
Data extraction
The author’s name, year of publication, study design, participants’ characteristics (i.e., number of participants, level of amputation, reason of amputation, gender, age, weight, height, time since amputation), type of prosthesis, intervention, outcome and main results were extracted from the included studies and tabulated by one author (EL).
Risk of bias assessment
Risk of bias assessment was performed by two reviewers (MAD & AM) using the “The Cochrane 2.0 risk of bias tool” for crossover studies [51]. Disagreement was resolved by consensus between the two author and a third author (EL) if consensus could not be reached. “The Cochrane 2.0 risk of bias tool” consists of eighteen questions to assess the randomization process (n = 5), the deviation from intended interventions (n = 5), the missing outcome data (n = 3), the measurement of the outcome (n = 2) and selection of the reported results (n = 3). Four possible answers could be given to each question: ‘yes’, ‘no’, ‘no information’ and ‘not applicable’. The risk of bias was determined by following the decision tree as indicated in the assessment tool and resulted in a low, moderate or a high risk of bias [51]. Overall low risk of bias across domains was indicated if the study was judged to have a low risk of bias over all of the individual domains. If the study raised some concern in at least one domain but did not present a high risk of bias in any domain, it resulted in an overall moderate risk of bias. If one of the domains had a high risk of bias, by default this resulted in an overall high risk of bias for all domains [51].
Results
Study selection
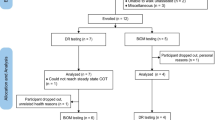
The search yielded 1352 records through PubMed, 1177 through Web of Science, 1656 through Scopus and 97 through Pedro. After screening, 34 studies remained and were included in this systematic review. The results of the selection process are illustrated in Fig. 1.
Study design and quality assessment
Seventeen studies had a cross-sectional study design [52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68], and 17 had a cross-over design [69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85]. Cross-sectional studies implemented a within-study design. This made them identical to those with a crossover design except for the order in which the devices were evaluated. Therefore, we reported the risk of bias using the same tool for all studies.
The risk of bias assessment revealed an overall high risk of bias. When we investigated the questions on which the scores were weak, we observed shortcomings in describing the randomization process and reporting deviation from the intended intervention resulting in a high risk of bias. Additionally, we identified minor issues in reporting outcome measurements, entailing a moderate risk of bias. At last, we rated bias due to missing data or reporting a selection of the results as low. Figure 2 details the individual risk of bias per study, and Fig. 3 visualizes the overall risk of bias.
Study characteristics
Table 2 presents a summary of the study characteristics. Comparison between passive ankle–foot prostheses was most frequently conducted (47%, n = 16) [54, 59,60,61,62,63,64, 68,69,70,71, 73, 80, 81, 84, 85]. Within this category, 14 articles included people with a transtibial amputation, 3 included people with a transfemoral amputation (88% [54, 61,62,63,64, 68,69,70,71, 73, 80, 81, 84, 85] and 19% [59, 60, 73], respectively), and the mean sample size totalled 13. Ten articles compared quasi-passive with passive prostheses (29%, n = 10) [53, 66, 67, 72, 74,75,76, 82, 83, 86]. All articles included people with a transtibial amputation (100%, n = 10 [53, 66, 67, 72, 74,75,76, 82, 83, 86]), and only three included people with a transfemoral amputation (30%, n = 3 [74,75,76]). The mean sample size equalled 9. The remaining studies compared active with passive prostheses in people with a transtibial amputation (24%, n = 8) with a mean sample size of 9 [52, 55,56,57,58, 65, 77, 79].
The prosthetic evaluation was mainly conducted through level walking tasks. Within the cluster of studies comparing passive prostheses, level walking tasks amounted to 63% (n = 10) [54, 61,62,63,64, 68, 73, 81, 84, 85]. Among those comparing passive to quasi-passive ankle–foot devices, the number equalled 30% (n = 3) [72, 82, 86]. For those comparing active to passive devices, level walking was assessed in 63% (n = 5) [52, 55,56,57, 79]. Less frequent tasks included treadmill level walking (19%, n = 3 [60, 71, 80]; 30%, n = 3 [74,75,76] and 13%, n = 1 [77], respectively), slope walking (6%, n = 1 [63]; 40%, n = 4 [66, 67, 72, 83] and 25%, n = 2 [55, 65], respectively) and treadmill slope walking (6%, n = 1 [71]; 10%, n = 1 [53] and 0%, n = 0, respectively). Tasks that were only performed to a limited extent were, within studies comparing passive prostheses, standing tasks (13%, n = 2) [69, 70], completing a walking circuit (6%, n = 1) [59] and climbing stairs (6%, n = 1) [63]. Within studies comparing active with passive prostheses, these were walking over rocks and performing clinical tests assessing agility and mobility (13%, n = 1 [58] and 13%, n = 1 [57], respectively).
Therapeutic benefits
All studies investigated the short-term effects of performing daily activities with prosthetic ankle–foot devices, and none of the studies examined long-term effects. The mean familiarisation time amounted to 11 days (range: no familiarisation–6 weeks). Biomechanical outcome measures were most frequently gathered. Within the cluster of studies comparing passive prostheses, the number of biomechanical measures amounted to 81% (n = 13) [59, 61, 62, 64, 68,69,70,71, 73, 80, 81, 84]. Among these, 11 found results favouring the newly tested passive prosthesis [59, 61, 62, 64, 68, 69, 71, 73, 81, 84]. Within the studies comparing passive with quasi-passive prostheses, the number of biomechanical measures was 60% (n = 6), and all reported positive results favouring the quasi-passive device [66, 67, 72, 76, 82, 83]. Within the studies comparing active with passive prostheses, 88% (n = 7) [52, 55,56,57,58, 65, 79] reported biomechanical outcome measures, all found positive effects in favour of the active device, and 1 article also found a negative effect [55].
Within studies comparing passive prostheses, comparing passive with quasi-passive prostheses, and comparing active with passive prostheses, physiological outcome measures (25%, n = 4 [54, 60, 64, 80]; 40%, n = 4 [53, 75, 76, 82] and 25%, n = 2 [55, 77] respectively) and performance outcomes were less frequently investigated (69%, n = 11 [54, 59,60,61, 63, 64, 68, 73, 80, 81, 85]; 33%, n = 3 [75, 76, 86] and 63%, n = 5 respectively [56,57,58, 65, 77]). Within the cluster of studies comparing passive prostheses, four studies reported physiological benefits [50, 52, 55, 58], and eight studies reported benefits on the performance of the novel passive prosthesis [54, 59, 61, 63, 64, 73, 80, 81]. Among the studies comparing passive with quasi-passive prostheses, one study reported positive physiological effects for the quasi-passive prosthesis [53], one reported negative physiological effects [74], and one found favourable results on performance regarding the quasi-passive prosthesis [75]. Within the studies comparing active with passive prostheses, 1 study reported a physiological benefit [55], and two reported a benefit on performance with the active prosthesis [57, 58]. Lastly, subjective outcome measures were scarce (31%, n = 5 [54, 59, 63, 70, 84]; 30%, n = 3 [53, 74, 86] and 25%, n = 2 [56, 57] respectively). Three studies favoured the novel passive prosthesis within the cluster of studies comparing passive prostheses [54, 63, 70]. Among the studies comparing passive with quasi-passive prostheses, one found positive results [53], and mixed results for the quasi-passive device [74]. One study favoured the active device within the studies comparing active with passive prostheses [57].
Discussion
The purpose of this study was to systematically review the therapeutic benefits of performing daily activities with passive, quasi-passive and active ankle–foot prostheses in people with a unilateral lower limb amputation. Remarkably, no studies investigated the long-term therapeutic benefits.
Figure 4 captures the short-term therapeutic benefits of passive, quasi-passive and active prostheses. This figure shows the domains in which benefits were found. It was not possible to provide such an overview at the outcome measure level due to high heterogeneity. Overall, the numerous outcome measures per study yielded positive results on biomechanical, physiological, performance-related or subjective outcomes for the more advanced prostheses, implying therapeutic benefits for the individuals walking with them, though all studies also identified no or unfavourable effects. The technological innovations contribute to improving the quality of life in the short-term when people with lower limb amputation switch the conventional passive cushion foot for a more advanced prosthesis (i.e. the passive energy-storing release feet, the surface-adaptive quasi-passive feet, the active feet generating an external force through an actuator). However, comparisons between active prostheses and quasi-passive devices have not yet been conducted.
Short-term therapeutic benefits of passive, quasi-passive and active ankle–foot prostheses in people with a unilateral transtibial and transfemoral amputation. The arrows indicate the effect of switching from one type of prosthesis to another. For example, switching from passive non-ESR to quasi-passive prostheses entails positive effects on biomechanics, performance and RPE. ESR: energy-storing and release; RPE: rating of perceived exertion; ?: currently unknown, to be investigated; *effect based on studies only including people with a transtibial amputation
Among the included studies, quality of life has been evaluated using biomechanical, physiological, performance-related or subjective measures. The biomechanical and physiological dimensions of quality of life have been assessed during level and slope walking in 94% of the included studies, while only 29% included the subjective dimension. In general, gait efficiency and efficacy improved in parallel with technological advances, though gait asymmetries remained [52,53,54,55,56,57,58,59,60,61,62, 64,65,66,67,68,69,70,71,72,73, 75,76,77, 79,80,81,82,83,84]. Further in-depth discussion of these parameters is not feasible due to the heterogeneity in outcome measure among the biomechanical and physiological parameters (Table 2). Nevertheless, it is the ultimate goal of prosthetic development to strive towards the most efficient gait patterns by seeking complete gait symmetry and matching the gait patterns as closely as possible to those of able-bodied individuals [37]. Furthermore, the limited data on the subjective dimension of quality of life revealed that the perceived effort and satisfaction increased in line with the advancement of the devices. The limited use of subjective measures can be attributed to the prohibitive cost of most active and quasi-passive devices for a subset of individuals. This factor might introduce a confounding variable in the data affecting subjective feedback. Conversely, these paywalls will not affect the biomechanical or physiological data. Nevertheless, subjective measures (e.g. perceived effort, satisfaction, feedback on the noise of motors in active prostheses) should be more prominent in prosthetic evaluations, as they are crucial to assessing the quality of life [87].
Due to its biomechanical focus, the prosthetic evaluation primarily targets aberrated movement patterns that can be remedied in the short term by a prosthesis [4, 6, 7]. However, movement patterns are orchestrated by the intertwining between biomechanical factors and the human brain [27, 88]. This entails that the brain plays a vital role in the organization and performance of human gait [88]. Magnetic resonance imaging revealed that amputation causes thinning of the premotor cortex and visual-motor area combined with a decrease in white matter integrity in the premotor area contralateral to the amputation and at a bilateral connection between both premotor cortices [27]. These changes interfere with movement planning or coordinating eye movements in relation to limbs and lead to decreased perception–action coupling [27]. Additionally, amputation causes changes in limb representation in the primary motor cortex and somatosensory cortex, and causes decreased connectivity between many brain areas, including the primary motor cortex, primary somatosensory cortex, basal ganglia, thalamus and cerebellum [27]. These changes in connectivity translate towards reduced motor control and balance and potentially lead to falls [9, 10, 27]. Remarkably, only a single study examining the effect on brain functioning across prosthetic ankle–foot prostheses has been included in this review [75]. De Pauw et al. [75] explored whether motor-related cortical potentials differed between passive and quasi-passive prostheses during daily activities using electro-encephalography but did not detect any difference between both devices. The absence of an effect is not unexpected, considering neuroplasticity is a time-consuming process, and sufficient familiarisation time was not provided [89,90,91,92,93,94]. Unravelling neuroplasticity in relation to the type of prosthesis may provide a new understanding of the effects of prostheses to improve the quality of life in people with a lower limb amputation.
A conceivable approach to account for the brain’s influence is through dual tasks, conditional on adequate familiarisation [95]. Dual tasks involve the concurrent performance of two tasks and are regarded as a measurement of cognitive-motor capacity as they require executive function and attentional demand [95]. Their performance usually results in decreased mobility and deteriorated gait patterns leading to increment falls [96, 97]. Out of the included articles in this review, only 1 investigated the difference between passive and quasi-passive prostheses during the performance of a dual-task during treadmill walking [75]. They found that only in individuals with a transfemoral amputation attention demands (reaction times and accuracy) increased during walking with the quasi-passive prosthesis compared to the current prosthesis and able-bodied individuals [75]. Lack of familiarization time to habituate to the new prosthetic device may have influenced these results. As discussed earlier, the negative implications of performing dual-tasks are attributable to cognitive demands associated with prosthetic use, balance and gait disturbances, and brain adaptations [9, 10, 27, 95]. Combined with the fact that dual-tasks represent daily activities, the recommendation is to include dual-task paradigms in the evaluation process of prostheses [95].
The design, development and evaluation of prosthetic devices is an iterative process requiring high cross-disciplinary collaboration between multiple research branches. This review reveals that the current emphasis in prosthetic evaluation has been placed on comparing ankle–foot prostheses without long-term evaluation. Since none of the included studies investigated the long-term benefits of comparing different ankle–foot prostheses, we, for example, cannot make any substantiated statements about the association between the onset of secondary injuries and the use of different types of prostheses solely based on studies conducted at a single point in time. Furthermore, it should be emphasized that the included studies mainly involved people with a transtibial amputation. In contrast, only six of the included studies included people with a transfemoral amputation, limiting the results’ generalisability within the prosthetic population [59, 60, 73,74,75,76]. Also, the majority of the studies (94%) are based upon biomechanical and physiological findings during the performance of walking tasks, except for 2, which used performance and subjective measures [63, 86]. Another concern relates to the overall high risk of bias. The high risk of bias can be attributed to the lack of randomisation, the inability to blind participants to the prosthetic condition and the lack of reporting protocol deviations. Specifically, the lack of randomisation and inability to blind participants are essentially inherent to prosthetic research. Taken all of the aforementioned elements into account, heterogeneity of the outcome measures combined with small sample sizes, limited familiarisation time, and the high risk of bias of the included studies do not allow robust conclusions to be made. Therefore, the recommendation is to perform adequate sampled studies with a limited number of outcome measures and ample familiarisation time evaluating a prosthetic device during daily activities. Secondly, the recommendation is shifting the emphasis towards the psychosocial dimension of quality of life through questionnaires finding a suitable poise between objective and subjective measures to obtain a thorough insight into the benefits of prosthetic devices. A recent review provides an overview of psychometric properties of functional, ambulatory, and quality of life instruments to be used in people with a lower limb amputation [43]. At last, we advise conducting prospective studies assessing the benefits of passive, quasi-passive and active prostheses in the longer term similar to those already conducted comparing prosthetic knees or those investigating quality of life after an amputation without comparing prosthetic devices [14, 30, 98,99,100,101].
Conclusion
This review evaluated the differences in the quality of life between passive, quasi-passive and active prostheses for people with a lower limb amputation using biomechanical, physiological, performance and subjective measures. Compared to passive ankle–foot prostheses, quasi-passive and active prostheses improve quality of life. Although short-term therapeutic benefits have been established favouring more advanced prostheses, outcome measures’ discrepancies prevail, the brain’s influence on prosthetic functioning is insufficiently studied, and the long-term benefits remain unknown. Investigating these aspects may improve the quality of life of people with a lower limb amputation.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
Sinha R, van den Heuvel WJ, Arokiasamy P. Factors affecting quality of life in lower limb amputees. Prosthet Orthot Int. 2011;35(1):90–6.
Amtmann D, Morgan SJ, Kim J, Hafner BJ. Health-related profiles of people with lower limb loss. Arch Phys Med Rehabil. 2015;96(8):1474–83.
Kovač I, Kauzlaric N, Živkovic O, Muzic V, Abramovic M, Vuletic Z, et al. Rehabilitation of lower limb amputees. Period Biol. 2015;117(1):147–59.
Geertzen J, van der Linde H, Rosenbrand K, Conradi M, Deckers J, Koning J, et al. Dutch evidence-based guidelines for amputation and prosthetics of the lower extremity: rehabilitation process and prosthetics. Part 2. Prosthet Orthot Int. 2015;39(5):361–71.
O’Keeffe B, Rout S. Prosthetic rehabilitation in the lower limb. Indian J Plast Surg. 2019;52(1):134–43.
Crowe CS, Impastato KA, Donaghy AC, Earl C, Friedly JL, Keys KA. Prosthetic and orthotic options for lower extremity amputation and reconstruction. Plast Aesthet Res. 2019;6:4.
Vetrayan J, Abd Ghafar NB, Paulraj SJPV, Murad MS. Occupational performance role and satisfaction among lower limb amputees with different adaptive devices usage. Procedia Soc Behav Sci. 2016;222:432–41.
Demirdel S, Ülger Ö. Body image disturbance, psychosocial adjustment and quality of life in adolescents with amputation. Disabil Health J. 2021;14(3): 101068.
Steinberg N, Gottlieb A, Siev-Ner I, Plotnik M. Fall incidence and associated risk factors among people with a lower limb amputation during various stages of recovery—a systematic review. Disabil Rehabil. 2019;41(15):1778–87.
Rodrigues FB, Andrade AO, Vieira MF. Effects of inclined surfaces on gait variability and stability in unilateral lower limb amputees. Med Biol Eng Comput. 2019;57(11):2337–46.
McDonald CL, Westcott-McCoy S, Weaver MR, Haagsma J, Kartin D. Global prevalence of traumatic non-fatal limb amputation. Prosthet Orthot Int. 2020;45(2):105–14.
Chihuri ST, Youdan GA Jr, Wong CK. Quantifying the risk of falls and injuries for amputees beyond annual fall rates—a longitudinal cohort analysis based on person-step exposure over time. Prevent Med Rep. 2021;24: 101626.
Hartholt KA, van Beeck EF, Polinder S, van der Velde N, van Lieshout EM, Panneman MJ, et al. Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma. 2011;71(3):748–53.
Pran L, Baijoo S, Harnanan D, Slim H, Maharaj R, Naraynsingh V. Quality of life experienced by major lower extremity amputees. Cureus. 2021;13(8): e17440.
Davie-Smith F, Coulter E, Kennon B, Wyke S, Paul L. Factors influencing quality of life following lower limb amputation for peripheral arterial occlusive disease: a systematic review of the literature. Prosthet Orthot Int. 2017;41(6):537–47.
Batten H, Lamont R, Kuys S, McPhail S, Mandrusiak A. What are the barriers and enablers that people with a lower limb amputation experience when walking in the community? Disabil Rehabil. 2020;42(24):3481–7.
Fogelberg DJ, Allyn KJ, Smersh M, Maitland ME. What people want in a prosthetic foot: a focus group study. J Prosthet Orthot. 2016;28(4):145–51.
McDonald CL, Cheever SM, Morgan SJ, Hafner BJ. Prosthetic limb user experiences with crossover feet: a pilot focus group study to explore outcomes that matter. J Prosthet Orthot. 2019;31(2):121–32.
Varrecchia T, Serrao M, Rinaldi M, Ranavolo A, Conforto S, De Marchis C, et al. Common and specific gait patterns in people with varying anatomical levels of lower limb amputation and different prosthetic components. Hum Mov Sci. 2019;66:9–21.
Petrini FM, Bumbasirevic M, Valle G, Ilic V, Mijović P, Čvančara P, et al. Sensory feedback restoration in leg amputees improves walking speed, metabolic cost and phantom pain. Nat Med. 2019;25(9):1356–63.
Esquenazi A. Gait analysis in lower-limb amputation and prosthetic rehabilitation. Phys Med Rehabil Clin N Am. 2014;25(1):153–67.
Wentink EC, Prinsen EC, Rietman JS, Veltink PH. Comparison of muscle activity patterns of transfemoral amputees and control subjects during walking. J Neuroeng Rehabil. 2013;10:87.
Weinert-Aplin RA, Twiste M, Jarvis HL, Bennett AN, Baker RJ. Medial–lateral centre of mass displacement and base of support are equally good predictors of metabolic cost in amputee walking. Gait Posture. 2017;51:41–6.
Gailey R, Allen K, Castles J, Kucharik J, Roeder M. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 2008;45(1):15–29.
Highsmith MJ, Goff LM, Lewandowski AL, Farrokhi S, Hendershot BD, Hill OT, et al. Low back pain in persons with lower extremity amputation: a systematic review of the literature. Spine J. 2019;19(3):552–63.
Probsting E, Blumentritt S, Kannenberg A. Changes in the locomotor system as a consequence of amputation of a lower limb. Z Orthop Unfall. 2017;155(1):77–91.
Molina-Rueda F, Navarro-Fernández C, Cuesta-Gómez A, Alguacil-Diego IM, Molero-Sánchez A, Carratalá-Tejada M. Neuroplasticity modifications following a lower-limb amputation: a systematic review. PM&R. 2019;11(12):1326–34.
Barnett CT, Vanicek N, Polman RC. Temporal adaptations in generic and population-specific quality of life and falls efficacy in men with recent lower-limb amputations. J Rehabil Res Dev. 2013;50(3):437–48.
Akyol Y, Tander B, Goktepe AS, Safaz I, Kuru O, Tan AK. Quality of life in patients with lower limb amputation: does it affect post-amputation pain, functional status, emotional status and perception of body image? J Musculoskelet Pain. 2013;21(4):334–40.
Wurdeman SR, Stevens PM, Campbell JH. Mobility analysis of AmpuTees (MAAT I): quality of life and satisfaction are strongly related to mobility for patients with a lower limb prosthesis. Prosthet Orthot Int. 2018;42(5):498–503.
Lechler K, Frossard B, Whelan L, Langlois D, Müller R, Kristjansson K. Motorized biomechatronic upper and lower limb prostheses-clinically relevant outcomes. PM&R. 2018;10(9 Suppl 2):S207–19.
Versluys R, Beyl P, Van Damme M, Desomer A, Van Ham R, Lefeber D. Prosthetic feet: state-of-the-art review and the importance of mimicking human ankle–foot biomechanics. Disabil Rehabil Assist Technol. 2009;4(2):65–75.
Cherelle P, Mathijssen G, Wang QN, Vanderborght B, Lefeber D. Advances in propulsive bionic feet and their actuation principles. Adv Mech Eng. 2014;6: 984046.
Windrich M, Grimmer M, Christ O, Rinderknecht S, Beckerle P. Active lower limb prosthetics: a systematic review of design issues and solutions. Biomed Eng Online. 2016;15(3):140.
Au SK, Weber J, Herr H. Powered ankle–foot prosthesis improves walking metabolic economy. IEEE Trans Rob. 2009;25(1):51–66.
Winter DA, Sienko SE. Biomechanics of below-knee amputee gait. J Biomech. 1988;21(5):361–7.
Laferrier JZ, Gailey R. Advances in lower-limb prosthetic technology. Phys Med Rehabil Clin N Am. 2010;21(1):87–110.
Asano M, Rushton P, Miller WC, Deathe BA. Predictors of quality of life among individuals who have a lower limb amputation. Prosthet Orthot Int. 2008;32(2):231–43.
Post MWM. Definitions of quality of life: what has happened and how to move on. Top Spinal Cord Inj Rehabil. 2014;20(3):167–80.
Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645–9.
Gallagher P, Desmond D. Measuring quality of life in prosthetic practice: benefits and challenges. Prosthet Orthot Int. 2007;31(2):167–76.
Chadwell A, Diment L, Micó-Amigo M, Morgado Ramírez DZ, Dickinson A, Granat M, et al. Technology for monitoring everyday prosthesis use: a systematic review. J Neuroeng Rehabil. 2020;17(1):93.
Balk EM, Gazula A, Markozannes G, Kimmel HJ, Saldanha IJ, Trikalinos TA, et al. Psychometric properties of functional, ambulatory, and quality of life instruments in lower limb amputees: a systematic review. Arch Phys Med Rehabil. 2019;100(12):2354–70.
Ardern CL, Büttner F, Andrade R, Weir A, Ashe MC, Holden S, et al. Implementing the 27 PRISMA 2020 statement items for systematic reviews in the sport and exercise medicine, musculoskeletal rehabilitation and sports science fields: the PERSiST (implementing Prisma in Exercise, Rehabilitation, Sport medicine and SporTs science) guidance. Br J Sports Med. 2021;56(4):175–95.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Bertos GA, Papadopoulos EG. Lower-limb prosthetics. In: Handbook of biomechatronics. London: Academic Press; 2018. p. 241.
Chumacero E, Masud AA, Isik D, Shen CL, Chyu MC. Advances in powered ankle–foot prostheses. Crit Rev Biomed Eng. 2018;46(2):93–108.
Harvey ZT, Potter BK, Vandersea J, Wolf E. Prosthetic advances. J Surg Orthop Adv. 2012;21(1):58.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):1–10.
Higgins J, Sterne J, Savović J, Page M, Hróbjartsson A, Boutron I, et al. Revised tool for assessing risk of bias in randomized trials. In: Chandler J, McKenzie J, Boutron I, Welch V, editors. Cochrane methods. Cochrane database of systematic reviews. 2016(10 Suppl 1).
D’Andrea S, Wilhelm N, Silverman AK, Grabowski AM. Does use of a powered ankle–foot prosthesis restore whole-body angular momentum during walking at different speeds? Clin Orthop Relat Res. 2014;472(10):3044–54.
Darter BJ, Wilken JM. Energetic consequences of using a prosthesis with adaptive ankle motion during slope walking in persons with a transtibial amputation. Prosthet Orthot Int. 2014;38(1):5–11.
Delussu AS, Paradisi F, Brunelli S, Pellegrini R, Zenardi D, Traballesi M. Comparison between SACH foot and a new multiaxial prosthetic foot during walking in hypomobile transtibial amputees: physiological responses and functional assessment. Eur J Phys Rehabil Med. 2016;52(3):304–9.
Esposito ER, Whitehead JMA, Wilken JM. Step-to-step transition work during level and inclined walking using passive and powered ankle–foot prostheses. Prosthet Orthot Int. 2016;40(3):311–9.
Esposito ER, Wilken JM. Biomechanical risk factors for knee osteoarthritis when using passive and powered ankle–foot prostheses. Clin Biomech. 2014;29(10):1186–92.
Ferris AE, Aldridge JM, Rábago CA, Wilken JM. Evaluation of a powered ankle–foot prosthetic system during walking. Arch Phys Med Rehabil. 2012;93(11):1911–8.
Gates DH, Aldridge JM, Wilken JM. Kinematic comparison of walking on uneven ground using powered and unpowered prostheses. Clin Biomech. 2013;28(4):467–72.
Graham LE, Datta D, Heller B, Howitt J. A comparative study of conventional and energy-storing prosthetic feet in high-functioning transfemoral amputees. Arch Phys Med Rehabil. 2007;88(6):801–6.
Graham LE, Datta D, Heller B, Howitt J. A comparative study of oxygen consumption for conventional and energy-storing prosthetic feet in transfemoral amputees. Clin Rehabil. 2008;22(10):896–901.
Heitzmann DWW, Salami F, De Asha AR, Block J, Putz C, Wolf SI, et al. Benefits of an increased prosthetic ankle range of motion for individuals with a trans-tibial amputation walking with a new prosthetic foot. Gait Posture. 2018;64:174–80.
Houdijk H, Wezenberg D, Hak L, Cutti AG. Energy storing and return prosthetic feet improve step length symmetry while preserving margins of stability in persons with transtibial amputation. J Neuroeng Rehabil. 2018;15:76.
Paradisi F, Delussu AS, Brunelli S, Iosa M, Pellegrini R, Zenardi D, et al. The conventional non-articulated SACH or a multiaxial prosthetic foot for hypomobile transtibial amputees? A clinical comparison on mobility, balance, and quality of life. Sci World J. 2015;2015: 261801.
Prakash A, Kumar R, Kumari P. Designing and evaluation of new dynamic prosthetic foot on transtibial amputees in a low resource setup. Int J Health Allied Sci. 2020;9(4):332–6.
Rábago CA, Aldridge Whitehead J, Wilken JM. Evaluation of a powered ankle–foot prosthesis during slope ascent gait. PLoS ONE. 2016;11(12): e0166815.
Riveras M, Ravera E, Ewins D, Shaheen AF, Catalfamo-Formento P. Minimum toe clearance and tripping probability in people with unilateral transtibial amputation walking on ramps with different prosthetic designs. Gait Posture. 2020;81:41–8.
Schmalz T, Altenburg B, Ernst M, Bellmann M, Rosenbaum D. Lower limb amputee gait characteristics on a specifically designed test ramp: preliminary results of a biomechanical comparison of two prosthetic foot concepts. Gait Posture. 2019;68:161–7.
Wezenberg D, Cutti AG, Bruno A, Houdijk H. Differentiation between solid-ankle cushioned heel and energy storage and return prosthetic foot based on step-to-step transition cost. J Rehabil Res Dev. 2014;51(10):1579–90.
Arifin N, Abu Osman NA, Ali S, Gholizadeh H, Wan Abas WAB. Postural stability characteristics of transtibial amputees wearing different prosthetic foot types when standing on various support surfaces. Sci World J. 2014. https://doi.org/10.1155/2014/856279.
Arifin N, Abu Osman NA, Ali S, Wan Abas WAB. The effects of prosthetic foot type and visual alteration on postural steadiness in below-knee amputees. BioMedical Eng Online. 2014;13(1):1–10.
Childers WL, Takahashi KZ. Increasing prosthetic foot energy return affects whole-body mechanics during walking on level ground and slopes. Sci Rep. 2018;8(1):5354.
Davot J, Thomas-Pohl M, Villa C, Bonnet X, Lapeyre E, Bascou J, et al. Experimental characterization of the moment-angle curve during level and slope locomotion of transtibial amputee: which parameters can be extracted to quantify the adaptations of microprocessor prosthetic ankle? Proc Inst Mech Eng H J Eng Med. 2021;235(7):762–9.
De Asha AR, Munjal R, Kulkarni J, Buckley JG. Impact on the biomechanics of overground gait of using an ‘Echelon’ hydraulic ankle–foot device in unilateral trans-tibial and trans-femoral amputees. Clin Biomech. 2014;29(7):728–34.
De Pauw K, Cherelle P, Roelands B, Lefeber D, Meeusen R. The efficacy of the ankle mimicking prosthetic foot prototype 4.0 during walking: physiological determinants. Prosthet Orthot Int. 2018;42(5):504–10.
De Pauw K, Cherelle P, Tassignon B, Van Cutsem J, Roelands B, et al. Cognitive performance and brain dynamics during walking with a novel bionic foot: a pilot study. PLoS ONE. 2019;14(4): e0214711.
De Pauw K, Serrien B, Baeyens JP, Cherelle P, De Bock S, Ghillebert J, et al. Prosthetic gait of unilateral lower-limb amputees with current and novel prostheses: a pilot study. Clin Biomech. 2020;71:59–67.
Gardinier ES, Kelly BM, Wensman J, Gates DH. A controlled clinical trial of a clinically-tuned powered ankle prosthesis in people with transtibial amputation. Clin Rehabil. 2018;32(3):319–29.
Gorjan DGK, De Pauw K, Marusic U. Removal of movement-induced EEG artifacts: current state of the art and guidelines. J Neural Eng. 2022. https://doi.org/10.1088/1741-2552/ac542c.
Grabowski AM, D’Andrea S. Effects of a powered ankle–foot prosthesis on kinetic loading of the unaffected leg during level-ground walking. J Neuroeng Rehabil. 2013;10:49.
Hsu MJ, Nielsen DH, Lin-Chan SJ, Shurr D. The effects of prosthetic foot design on physiologic measurements, self-selected walking velocity, and physical activity in people with transtibial amputation. Arch Phys Med Rehabil. 2006;87(1):123–9.
Johnson L, De Asha AR, Munjal R, Kulkarni J, Buckley JG. Toe clearance when walking in people with unilateral transtibial amputation: effects of passive hydraulic ankle. J Rehabil Res Dev. 2014;51(3):429–37.
Segal AD, Zelik KE, Klute GK, Morgenroth DC, Hahn ME, Orendurff MS, et al. The effects of a controlled energy storage and return prototype prosthetic foot on transtibial amputee ambulation. Hum Mov Sci. 2012;31(4):918–31.
Struchkov V, Buckley JG. Biomechanics of ramp descent in unilateral trans-tibial amputees: comparison of a microprocessor controlled foot with conventional ankle–foot mechanisms. Clin Biomech. 2016;32:164–70.
Underwood HA, Tokuno CD, Eng JJ. A comparison of two prosthetic feet on the multi-joint and multi-plane kinetic gait compensations in individuals with a unilateral trans-tibial amputation. Clin Biomech. 2004;19(6):609–16.
Yang JR, Yang HS, Ahn DH, Ahn DY, Sim WS, Yang HE. Differences in gait patterns of unilateral transtibial amputees with two types of energy storing prosthetic feet. Ann Rehabil Med. 2018;42(4):609–16.
Gailey RS, Gaunaurd I, Agrawal V, Finnieston A, O’Toole C, Tolchin R. Application of self-report and performance-based outcome measures to determine functional differences between four categories of prosthetic feet. J Rehabil Res Dev. 2012;49(4):597–612.
Fanciullacci C, McKinney Z, Monaco V, Milandri G, Davalli A, Sacchetti R, et al. Survey of transfemoral amputee experience and priorities for the user-centered design of powered robotic transfemoral prostheses. J Neuroeng Rehabil. 2021;18(1):168.
Wittenberg E, Thompson J, Nam CS, Franz JR. Neuroimaging of human balance control: a systematic review. Front Hum Neurosci. 2017;11:170.
Bruno V, Ronga I, Fossataro C, Galigani M, Sacco K, Garbarini F. Long-term limb immobilization modulates inhibition-related electrophysiological brain activity. Neuroimage. 2020;218: 116911.
Burianová H, Sowman PF, Marstaller L, Rich AN, Williams MA, Savage G, et al. Adaptive motor imagery: a multimodal study of immobilization-induced brain plasticity. Cereb Cortex. 2016;26(3):1072–80.
Garbarini F, Cecchetti L, Bruno V, Mastropasqua A, Fossataro C, Massazza G, et al. To move or not to move? Functional role of ventral premotor cortex in motor monitoring during limb immobilization. Cereb Cortex. 2019;29(1):273–82.
Koppelmans V, Bloomberg JJ, De Dios YE, Wood SJ, Reuter-Lorenz PA, Kofman IS, et al. Brain plasticity and sensorimotor deterioration as a function of 70 days head down tilt bed rest. PLoS ONE. 2017;12(8): e0182236.
Opie GM, Evans A, Ridding MC, Semmler JG. Short-term immobilization influences use-dependent cortical plasticity and fine motor performance. Neuroscience. 2016;330:247–56.
Wanamaker AB, Andridge RR, Chaudhari AM. When to biomechanically examine a lower-limb amputee: a systematic review of accommodation times. Prosthet Orthot Int. 2017;41(5):431–45.
Omana H, Madou E, Montero-Odasso M, Payne MW, Viana R, Hunter SW. The effect of dual-task testing on the balance and gait of people with lower limb amputations: a systematic review. PM&R. 2021. https://doi.org/10.1002/pmrj.12702.
Hunter SW, Frengopoulos C, Holmes J, Viana R, Payne MWC. Dual-task related gait changes in individuals with trans-tibial lower extremity amputation. Gait Posture. 2018;61:403–7.
Morgan SJ, Hafner BJ, Kartin D, Kelly VE. Dual-task standing and walking in people with lower limb amputation: a structured review. Prosthet Orthot Int. 2018;42(6):652–66.
Burçak B, Kesikburun B, Köseoğlu BF, Öken Ö, Doğan A. Quality of life, body image, and mobility in lower-limb amputees using high-tech prostheses: a pragmatic trial. Ann Phys Rehabil Med. 2021;64(1): 101405.
Sarroca N, Valero J, Deus J, Casanova J, Luesma MJ, Lahoz M. Quality of life, body image and self-esteem in patients with unilateral transtibial amputations. Sci Rep. 2021;11(1):12559.
Silva ADM, Furtado G, Dos Santos IP, da Silva CB, Caldas LR, Bernardes KO, et al. Functional capacity of elderly with lower-limb amputation after prosthesis rehabilitation: a longitudinal study. Disabil Rehabil Assist Technol. 2021;16(5):556–60.
Jayaraman C, Mummidisetty CK, Albert MV, Lipschutz R, Hoppe-Ludwig S, Mathur G, et al. Using a microprocessor knee (C-Leg) with appropriate foot transitioned individuals with dysvascular transfemoral amputations to higher performance levels: a longitudinal randomized clinical trial. J Neuroeng Rehabil. 2021;18(1):88.
Acknowledgements
Not applicable.
Funding
This study is funded by the Innoviris project Talaris (BRGRD40: R&D project 2019: The Talaris project) and is part of the SRP17 Exercise and the Brain in Health & Disease: The Added Value of Human-Centered Robotics.
Author information
Authors and Affiliations
Contributions
EL drafted the work. EL, BT, CC, PC, KDP and RM contributed substantially to the conceptualisation of the work. EL, BT and KDP contributed substantially to the design of the work. EL, MAD, AM and BT contributed substantially to the acquisition of the work. EL and BT contributed substantially to the data analysis and data interpretation of the work. All authors revised the work critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lathouwers, E., Díaz, M.A., Maricot, A. et al. Therapeutic benefits of lower limb prostheses: a systematic review. J NeuroEngineering Rehabil 20, 4 (2023). https://doi.org/10.1186/s12984-023-01128-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12984-023-01128-5