Abstract
Background
The present study examined the quality of life and its relationship with socio-demographic characteristics among eye patients.
Methods
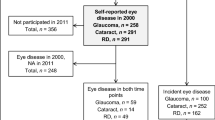
A cross-sectional survey was administered from January 2022 to April 2022. Data were collected from participants with eye diseases (N = 617) in the Herat province of Afghanistan.
Results
Of the 617 participants, 63.4% had poor physical quality of life and 14.9% had poor mental quality of life. Multiple regression analysis indicated that poor physical quality of life was significantly associated with being above 54 years old (adjusted odds ratio [AOR] = 1.15, p = .0048), being female (AOR = 3.58. p < 0.01), being illiterate (AOR = 3.31, p = 0.01), being unemployed (AOR = 1.93, p = 0.04), and experiencing a traumatic event during the past month (AOR = 2.06, p = 0.02). Poor mental quality of life was associated with occupational status (being unemployed) (AOR = 3.62, p = 0.05), and experiencing a traumatic event in the past month (AOR = 3.49, p < 0.01).
Conclusion
The present study provides a novel contribution to the field eye diseases and quality of life especially in relation to Afghanistan where there has been very little research in this area. The results indicate that public health authorities in Afghanistan should implement policies to improve mental and physical aspects of quality of life of patients with eye diseases as well as formulating strategies to help improve it.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
According to the World Health Organization (WHO), the world faces numerous challenges, including disparities in the availability and quality of ophthalmic services for prevention, treatment, and rehabilitation [1]. Eye problems include a wide range of disorders and diseases including refractive errors, age-related macular degeneration, cataracts, diabetic retinopathy, glaucoma, amblyopia, and strabismus [2] . The WHO reports that 2.2 billion individuals worldwide suffer from vision impairment [1]. A study concerning the impact of blindness and moderate and severe vision impairment on the global economy reports an estimate of a 30.2% employment reduction among employees with vision loss. Moreover, the global annual cost of this reduction in employment is estimated to be $410.7 billion (US) [3].
According to the Lancet Global Health Commission on Global Eye Health, it is estimated that there will be 895 million individuals worldwide with vision impairment by 2050, of whom 61 million will be blind, due to population aging, growth, and urbanization. Therefore, interventions in ophthalmic healthcare, which are known to be the most economical in the entire healthcare system, are necessary to be prioritized through equitable and inclusive services [4]. Vision impairment significantly lowers the quality of life among adults by lowering productivity and workforce participation rates, while increasing anxiety and depression levels [5]. Quality of life is a term that refers to the well-being of a population or an individual in terms of both positive and negative aspects of their existence during a specific period [6]. A significant indicator of how eye health affects individuals’ everyday lives, general well-being, and visual function is quality of life, such that vision impairment and eye illness have been linked to higher rates of mortality and lower quality of life [7].
Several studies underscore the impact of vision impairment on quality of life across different demographics. A large-scale study in Germany (n = 11,941) highlighted that evaluating both eyes is crucial, as relying solely on the better-seeing eye may underestimate the effect on vision-related quality of life [8]. In Northwest Ethiopia, 49.2% of patients with vision impairment (n = 484) reported low quality of life, associated with factors such as being aged over 75 years, rural residence, severe visual impairment, and prolonged history of visual impairment [9]. Enoch et al. found in a survey (n = 250) that sight ranked highest among senses, with participants preferring 4.6 years of perfect health over 10 years with total blindness [10]. Gender disparities exist in ocular diseases, with conditions like dry eye syndrome and cataracts disproportionately affecting women [11]. Children with strabismus also exhibit poorer quality of life compared to those with normal sight [12]. According to a study conducted in schools for the blind in Northeast India, 85.5% of the children (n = 515) experienced a low quality of life [13]. Emerging adults (18–25 years) experiencing vision problems (n = 172) reported significantly poorer quality of life in daily activities, work, and study compared to peers without chronic diseases [14]. Among older adults in Tehran (n = 566), vision-related quality of life correlated significantly with physical and socio-cultural factors, and access to ophthalmic services [15].
The results of a cohort study on glaucoma patients (n = 1728) and their socioeconomic status found that when the development of visual impairment occurred before being diagnosed with glaucoma, patients with lower income experienced higher visual impairment in comparison to patients with higher income [16]. Another study evaluated the effect of socioeconomic status on vision-related quality of life among open-angle glaucoma patients (n = 186). The results showed patients with a college degree or above had a better quality of life than patients with lower educational attainment [17].
A Delphi study recruiting eye experts from 118 countries (n = 470) including the South Asia region, ranked 16 grand challenges in global eye health from highest priority to least. These 16 challenges were categorized into four sections. The challenges reported from highest to lowest priority were (i) detection and treatment of conditions, (ii) health services and policy, (iii) access and equality, and (iv) human resource capacity [18]. In the Asia–Pacific region, the most common ophthalmic healthcare service challenges have been found to be a large and rapidly aging population, a wide spectrum of eye diseases, and imbalanced distribution of resources [19].
In a study conducted in Kabul, Afghanistan among adults aged 50 years and above (n = 3751), it was found that severe vision impairment had a prevalence of 2.2%, while moderate and mild vision impairments had a prevalence of 6.9% and 8.7% respectively. Cataracts were identified as the leading cause of blindness, severe vision impairment, and moderate vision impairment. Additionally, uncorrected refractive error emerged as the primary contributor to mild vision impairment [20]. Another study conducted in the Nangarhar province of Afghanistan (n = 1281) reported that the most common causes of blindness and vision impairment were cataracts, uncorrected refractive error, glaucoma, age-related macular degeneration, and diabetic retinopathy [21]. The findings of a cross-sectional study in Herat (Afghanistan) (n = 509) indicated that younger adults had low awareness of common eye diseases. However, participants over the age of 35 years reported higher odds of awareness regarding eye diseases [22]. Overall, the World Health Organization estimates that there are 400,000 blind and 1.5 million visually impaired individuals in Afghanistan [23].
Eye care in Afghanistan encounters several critical challenges. There is a shortage of trained health professionals to diagnose and treat eye conditions [40]. While eye care services are available through primary care channels, access remains hindered by economic constraints and societal restrictions, particularly affecting women's access to these services [41]. Lastly, Afghanistan grapples with low health literacy, influenced by cultural and religious factors that impact health-seeking behaviors and awareness about eye health [42].
Despite the available studies, there is still a paucity of data regarding the impact of eye diseases on the quality of life of individuals in Afghanistan. Therefore, the objective of the present study was to assess the association between socio-demographic variables with physical and mental aspects of quality of life among individuals with eye diseases in Herat, Afghanistan.
2 Methods
2.1 Design
A cross-sectional study was conducted among patients visiting the governmental and private eye clinics in Herat province of Afghanistan between January 10, 2022 and April 15 2022. Data from 617 participants were collected from patients visiting an ophthalmologist. The data were collected by means of print-based self-reported surveys (with the questions asked by an interviewer rather than self-completion due to the high rate of illiteracy). The study utilized convenience sampling from patients visiting a private and a governmental eye clinic who agreed to participate in the study. The inclusion criteria for enrollment in this study included: (i) being diagnosed with an eye condition; (ii) demonstrating proficiency in understanding the Dari language; and (iii) providing informed consent, either in written or verbal form, from adults aged 18 years or older, and from parents or guardians on behalf of adolescents under 18 years of age.
2.2 Measures
The survey used in the present study comprised two sections (socio-economic questions, and quality of life questions). The first section contained questions regarding age, gender (male, female), marital status (single, married, widow/divorced), residency (urban, rural), educational level (illiterate, primary school, secondary school, high school, university), monthly income (less than $50, $50–$100, $100–$200, $200–$300, more than $300), occupational status (employed, unemployed), social media user (yes/no), wore glasses (yes/no), and traumatic event occurring during the past month (yes/no).
The 12-item Short-Form Survey (SF-12v2) was used to assess the quality of life of participants. Although the SF-12 actually assesses the impact of health on an individual's everyday life, according to the SF-12v2 manual and other studies [24], the instrument can be used to assess quality of life. The scale comprises two general components (physical component score [PCS] and the mental component score [MCS]), and eight subcomponents (physical functioning [PF], role-physical [RP], bodily pain [BP], general health [GH], energy/fatigue [VT], social functioning [SF], role-emotional [RE)], and mental health [MH]). Items in the scale (e.g., “During the past week, how much of the time has your physical health or emotional problems interfered with your social activities [like visiting with friends, relatives, etc.]?”) are rated from 1 to 6 with scores ranging from 6 to 20 for the physical component score and 6 to 28 for the mental component score. Higher score indicates better quality of life in that component. A threshold of less than 50% was designated to indicate poor quality of life, whereas a score exceeding 50% was considered indicative of fair quality of life. In the present study, the Cronbach’s alpha was 0.88.
2.3 Data analysis
IBM SPSS version 26 was used for data entry and data analysis. The frequency option was used to obtain the frequencies and percentages of the socio-economic variables. To evaluate the relationship between categorical variables, chi-square tests were used. A p-value of equal or less than 0.05 was considered significant in the present study. Multinomial logistic regression analysis was used to examine independent socio-demographics with quality of life.
2.4 Ethics
Ethical approval for the present study was obtained from the Afghanistan Center for Epidemiological Studies—Ethical Committee (ref: #21.021). During the initial contact with the participants, a description of the study was presented to them. Informed consent was obtained from all the participants in the present study. Participants were aware that they could withdraw at any point in time from the study. All methods were carried out in accordance with relevant ethical guidelines and regulations.
3 Results
A total of 617 eye patients participated in the present study with an age range of 18 to 100 years. The mean age of the participants was 44.42 years. More than two-thirds of the participants were female (68.1%). Almost three-quarters of the participants were married (72.0%). More than half of the participants were living in urban areas (58.8%) (Table 1).
The quality of life of almost two-thirds of the participants was poor on the physical component score (63.4%). One-seventh of the participants had poor quality of life on the mental component score (14.9%). The physical functioning component of quality of life among almost two-thirds of the participants was poor (60.1%) (Table 2).
The quality of life on the physical component score (PCS) among half of the participants aged 30–42 years was poor (49.6%). The quality of life on the PCS was poor among over three-quarters of the participants who were illiterate (78.7%) (Table 3).
The mental component score (MCS) of quality of life among one-fifth of the participants aged above 54 years old was poor (20.4%). The MCS of quality of life was poor among almost one-third of the participants who were widow/divorced (28.9%). The mental component of quality of life among one-quarter of the participants with a monthly income of less than $50 was poor (25.0%) (Table 4).
Multiple logistic regression was performed to identify predictors of the physical component score of quality of life comprising the following variables: age group, gender, job marital status, residency, education level, occupational status, using social media, wearing glasses, and traumatic event occurring during the past month. The analysis indicated that poor physical quality of life among participants was significantly associated with being above 54 years old (adjusted odds ratio [AOR] = 5.73, p = 0.0048), being female (AOR = 3.58. p < 0.01), being illiterate (AOR = 3.31, p = 0.01), being unemployed (AOR = 1.93, p = 0.04), and experiencing a traumatic event during the past month (AOR = 2.06, p = 0.02) (Table 5).
Multiple logistic regression was also performed to identify predictors of the mental component score of quality of life comprising the following variables: age group, gender, job marital status, residency, education level, occupational status, social media user, wearing glasses, and traumatic event occurring during the past month. The analysis indicated that poor mental quality of life among participants was associated with occupational status (being unemployed) (AOR = 3.62, p = 0.05), and experiencing a traumatic event in the past month (AOR = 3.49, p < 0.01) (Table 6).
4 Discussion
According to the findings of the present study, sociodemographic factors such as age group, gender, marital status, education level, monthly income, occupational status, being a social media user, and a traumatic event occurring in the past month were all significantly associated with both physical and mental components of quality of life among patients with eye disease, while residency was only associated with the physical component of the quality of life.
More specifically, there was a significant association between age and both physical and mental components of quality of life among patients with eye diseases (i.e., being aged above 54 years). This concurs with research conducted in Northwest Ethiopia which found that individuals older than 75 years of age reported a lower quality of life compared to younger participants [9].
Additionally, the present study’s findings find corroborate with previous studies in Afghanistan. For instance, a study carried out in the Nangarhar province found that as age increased, instances of visual impairment and blindness tended to be higher, despite the absence of a significant increase in low vision cases [21]. This age-associated trend is particularly evident among older adults. Age-related issues such as decreased mobility and challenges in managing daily tasks can significantly impact individual’s quality of life [25]. For individuals experiencing visual impairment due to eye diseases, these age-associated challenges can be exacerbated, leading to further declines in quality of life.
To further explore these relationships and to identify predictors of mental and physical component scores of quality of life, logistic regression analyses were carried out. Despite the noticeable age-related trends, no statistically significant association was found between the participants' age and their mental quality of life. However, individuals over 54 years of age were significantly more likely to report worse physical quality of life. One possible explanation for this disparity between physical and mental quality of life could be the differential resilience of mental and physical health to aging and illness. Whereas physical health might deteriorate more rapidly with age and disease progression, mental health may be bolstered by factors such as adaptive coping strategies, social support, and life experience. Further research is needed to clarify the reasons for these differences and to develop effective strategies that consider the varying needs of different age groups within this patient population.
Another finding was the significant relationship between monthly income and the quality of life among patients with eye diseases. Descriptive data suggested that higher income was generally associated with a higher quality of both physical and mental life. It is important to note that replication studies are needed to confirm the significance of this observed pattern. This finding concurs with the results from a study conducted in Nangarhar, Afghanistan, which reported an association between self-reported poor economic status and vision impairment [21]. A reasonable explanation for this could be the financial problems encountered when managing eye diseases. A lower income may curtail access to necessary healthcare services, medications, and other therapeutic resources, possibly leading to less efficient management of eye diseases and, subsequently, a decline in quality of life. Conversely, those with a higher income may have access to better healthcare resources enabling them to manage their health conditions more effectively, therefore maintaining a relatively higher quality of life. Further research is needed to examine whether this finding occurs across countries that have free access to healthcare (e.g., UK). However, it should be noted that that income was not a significant predictor in the regression model.
The present study also found several other factors significantly associated with the mental and physical quality of life among patients with eye diseases. Being female, being divorced/widowed, being illiterate, being unemployed, not using social media, and having experienced a traumatic event within the past month were found to be associated with both physical and mental quality of life. However, residency (i.e., living in a rural area) was only associated solely with poor physical quality of life, suggesting living conditions impact more negatively on physical well-being than mental wellbeing.
Multiple logistic regression analysis was carried out to further examine these associations. Unemployment and experiencing a traumatic event in the past month both emerged as significant predictors for lower mental and physical quality of life among participants. Being female was a significant predictor of poor physical (but not mental) quality of life.
It's notable that other studies have similarly associated gender, occupational status, and recent traumatic experiences to quality of life. For instance, a cross-sectional web-based registry study reported gender differences in quality of life among individuals with eye diseases, with females often reporting lower quality of life scores than males [26]. This disparity might be driven by a combination of biological differences, gender-specific health concerns, and social factors such as gender roles and expectations. In contrast, the results of a study on quality of life among patients with a very specific form of eye disease (i.e., anterior uveitis) reported no significant association between gender and quality of life [27]. Further exploration of different eye diseases is required to reconcile these differing outcomes.
The findings of the present study showed participants who were using social media reported better quality of life than those who were not using it. Although some studies have highlighted that using social media is associated with poor quality of life, such studies refer to problematic social media use [28]. Indeed, studies examining non-problematic social media use have shown that using social media can have a positive impact on quality of life among its users [30, 31]. The positive impact of social media on individuals' quality of life can be attributed to a variety of factors. This can be due to the benefits of social media uses such as connection and social support, which foster a sense of belonging and provide emotional sustenance. Additionally, social media platforms offer opportunities for networking, enabling individuals to forge professional relationships and explore career possibilities. Furthermore, social media serves as a medium for creativity and self-expression, allowing users to showcase their talents and receive feedback from a global audience. Lastly, social media platforms can be a source of inspiration and motivation, exposing individuals to diverse ideas and success stories. Collectively, these benefits contribute to an enhanced quality of life for many social media users [29, 30].
The present study also found that illiterate participants were more likely to report having a have poor quality of life. This concurs with other studies which have also reported a similar relationship [30, 32, 33]. Being illiterate often means that opportunities in life (e.g., career advancement) are limited, which is associated with poorer income. These consequences are associated with poorer life quality. Regarding occupational status, the World Health Organization (WHO) recognizes unemployment and job insecurity as social determinants of health [34]. Studies have shown that unemployed individuals often exhibit a poorer quality of life than their employed counterparts [35]. The low quality of life of unemployed individuals might be related to factors such as a lack of perceived meaningfulness in life for some, and financial dissatisfaction. [36]
Although there are no previous studies examining the association between traumatic experiences and quality of life among patients with eye diseases in Afghanistan, the present study’s findings align with prior research that explores the impact of trauma on quality of life. Extant research suggests that trauma can directly reduce quality of life or indirectly influence it through the mediation of mental distress [37]. Additionally, there is evidence to suggest that post-traumatic stress disorder (PTSD) symptoms are associated with a poor quality of life [38]. However, it is important to note that these studies are not specific to eye disease patients and may not fully capture the unique circumstances and challenges faced by this particular population. Therefore, the present study contributes to the understanding of this relationship in the context of patients with eye diseases in Afghanistan and highlights the need for further research to better address their specific needs and experiences.
The results of the present study highlight a potentially complex interplay of sociodemographic factors impacting the quality of life among patients with eye diseases. The findings contribute to this growing body of knowledge, offering further insight into the determinants of quality of life in this patient population. However, more comprehensive studies are needed to delineate these relationships and discern the underlying mechanisms.
There are some limitations that need to be taken into account when interpreting the present study’s findings. First, the study comprised self-report data which can lead to biased responses. Second, the study design was cross-sectional which limits the long-term assessment of specific factors such as experience of a traumatic life event, as well as being unable to determine the causality between the study variables. Third, the study was only carried out in one area of Afghanistan so the findings may not generalize to other areas of Afghanistan (or other countries). Fourth, the sample had a gender imbalance (with two-thirds being female) which also biases the findings and affects generalizability. Also, the traumatic event among participants were assessed using only one variable which could increase the chance of bias. Another limitation of this study is not recording the type of eye disease and time since eye disease, and medical and mental comorbidity. These variables can influence the quality of life of patients and can increase the chance of bias.
5 Conclusion
Further studies are needed to understand how sociodemographic factors are associated with the quality of life of patients with specific eye diseases. The present study provides a novel contribution to the field of eye diseases and quality of life especially in relation to Afghanistan where there has been very little previous research in this area. No previous study has used the approach of identifying both mental and physical components of quality of life among Afghan patients with eye diseases. The results indicate that public health authorities in Afghanistan should implement policies to improve mental and physical aspects of quality of life of patients with eye diseases as well as formulating strategies to help improve it.
Data availability
The datasets collected and/or analyzed during the present study are available from the corresponding author upon reasonable request.
References
World Health Organization. World Report on vision. https://www.who.int/publications/i/item/9789241516570.
Centers for Disease Control and Prevention. Common eye disorders and diseases. 2022. https://www.cdc.gov/visionhealth/basics/ced/index.html.
Marques AP, Ramke J, Cairns J, Butt T, Zhang JH, Muirhead D, et al. Global economic productivity losses from vision impairment and blindness. EClinicalMedicine. 2021;35: 100852.
Burton MJ, Ramke J, Marques AP, Bourne RR, Congdon N, Jones I, et al. The Lancet Global Health Commission on global eye health: vision beyond 2020. Lancet Glob Health. 2021;9(4):e489-551.
World Health Organization Vision Impairment and blindness. https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment.
Teoli D, Bhardwaj A. Quality of life. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. http://www.ncbi.nlm.nih.gov/books/NBK536962/. Accessed 16 Jan 2023.
Assi L, Rosman L, Chamseddine F, Ibrahim P, Sabbagh H, Congdon N, et al. Eye health and quality of life: an umbrella review protocol. BMJ Open. 2020;10(8): e037648.
Nickels S, Schuster AK, Elflein H, Wolfram C, Schulz A, Münzel T, et al. Vision-related quality of life considering both eyes: results from the German population-based Gutenberg Health Study (GHS). Health Qual Life Outcomes. 2019;17(1):1–8.
Yibekal BT, Alemu DS, Anbesse DH, Alemayehu AM, Alimaw YA. Vision-related quality of life among adult patients with visual impairment at University of Gondar, Northwest Ethiopia. J Ophthalmol. 2020;23(2020): e9056097.
Enoch J, McDonald L, Jones L, Jones PR, Crabb DP. Evaluating whether sight is the most valued sense. JAMA Ophthalmol. 2019;137(11):1317–20.
Korpole NR, Kurada P, Korpole MR. Gender difference in ocular diseases, risk factors and management with specific reference to role of sex steroid hormones. J Mid-Life Health. 2022;13(1):20.
Silva N, Castro C, Caiado F, Maia S, Miranda V, Parreira R, et al. Evaluation of functional vision and eye-related quality of life in children with strabismus. Clin Ophthalmol. 2022;16:803.
Magdalene D, Bhattacharjee H, Deshmukh S, Mohapatra SD, Ali A, Paidi RR, et al. Assessment of quality of life, mental health and ocular morbidity in children from schools for the blind in North-East India. Indian J Ophthalmol. 2021;69(8):2040.
Elsman EB, van Rens GH, van Nispen RM. Quality of life and participation of young adults with a visual impairment aged 18–25 years: comparison with population norms. Acta Ophthalmol. 2019;97(2):165–72.
Bigdeli S, Arab M, Hadian M, Tajvar M. Vision-related quality of life of older people in Tehran and their access and utilization of eye care services. Iran J Public Health. 2022;51(8):1857–65.
Sung H, Shin HH, Baek Y, Kim GA, Koh JS, Park EC, et al. The association between socioeconomic status and visual impairments among primary glaucoma: the results from Nationwide Korean National Health Insurance Cohort from 2004 to 2013. BMC Ophthalmol. 2017;17(1):1–9.
Kuo YS, Liu CJ, Cheng HC, Chen MJ, Chen WT, Ko YC. Impact of socioeconomic status on vision-related quality of life in primary open-angle glaucoma. Eye. 2017;31(10):1480–7.
Ramke J, Evans JR, Habtamu E, Mwangi N, Silva JC, Swenor BK, Congdon N, et al. Grand challenges in global eye health: a global prioritisation process using Delphi method. Lancet Healthy Longevity. 2022;3(1):e31-41.
Yusufu M, Bukhari J, Yu X, Lin TP, Lam DS, Wang N. Challenges in eye care in the Asia-Pacific region. Asia-Pac J Ophthalmol. 2021;10(5):423–9.
Sapkota Y, Alizoi N, Siddiqi AM, Naseem M, Salaam AS, ur Rehman A, et al. Rapid assessment of prevalence of blindness and cataract surgery in Kabul province Afghanistan. BMJ Open Ophthalmol. 2021;6(1): e000790.
Abdianwall MH, Doğan BG. Prevalence of visual impairment and related factors in Nangarhar Province of Afghanistan: a cross sectional study. Int J Ophthalmol. 2018;11(12):1968.
Hosaini F, Padhi BK, Mohanty P, Razaqi N, Neyazi M, Noorzad E, et al. Sociodemographic factors associated with knowledge of common eye diseases: a cross-sectional study in Afghanistan. medRxiv; 2022. https://doi.org/10.1101/2022.09.19.22280069.
World Health Organization. Eye care. https://www.emro.who.int/afg/programmes/eye-care.html.
Huo T, Guo Y, Shenkman E, Muller K. Assessing the reliability of the short form 12 (SF-12) health survey in adults with mental health conditions: a report from the wellness incentive and navigation (WIN) study. Health Qual Life Outcomes. 2018;16(1):1–8.
Netuveli G, Wiggins RD, Hildon Z, Montgomery SM, Blane D. Quality of life at older ages: evidence from the English longitudinal study of aging (wave 1). J Epidemiol Community Health. 2006;60(4):357–63.
Kandel H, Nguyen V, Piermarocchi S, Ceklic L, Teo K, Arnalich-Montiel F, et al. Quality of life impact of eye diseases: a Save Sight Registries study. Clin Exp Ophthalmol. 2022;50(4):386–97.
Liang Z, Zhang T, Lin T, Liu L, Wang B, Fu AZ, et al. Health-related quality of life among rural men and women with hypertension: assessment by the EQ-5D-5L in Jiangsu, China. Qual Life Res. 2019;15(28):2069–80.
Geirdal AØ, Ruffolo M, Leung J, Thygesen H, Price D, Bonsaksen T, et al. Mental health, quality of life, wellbeing, loneliness and use of social media in a time of social distancing during the COVID-19 outbreak. A cross-country comparative study. J Mental Health. 2021;30(2):148–55.
Chen HT, Li X. The contribution of mobile social media to social capital and psychological well-being: examining the role of communicative use, friending and self-disclosure. Comput Hum Behav. 2017;1(75):958–65.
Cotten SR, Schuster AM, Seifert A. Social media use and well-being among older adults. Curr Opin Psychol. 2022;1(45): 101293.
Zhao Y, Zhang X, Wang J, Zhang K, Ordonez de Pablos P. How do features of social media influence knowledge sharing? An ambient awareness perspective. J Knowl Manag. 2020;24(2):439–62.
Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health. Accessed 24 May 2023.
Merchant JA, Kelly KM, Burmeister LF, Lozier MJ, Amendola A, Lind DP, et al. Employment status matters: a statewide survey of quality-of-life, prevention behaviors, and absenteeism and presenteeism. J Occup Environ Med. 2014;56(7):686–98.
Polizzi CP, Aksen DE, Lynn SJ. Quality of life, emotion regulation, and dissociation: evaluating unique relations in an undergraduate sample and probable PTSD subsample. Psychol Trauma Theory Res Pract Policy. 2022;14:107–15.
Hult M, Pietilä AM, Saaranen T. The factors predicting quality of life among unemployed adults: a model based on salutogenic approach. Soc Indic Res. 2020;152:1197–211.
Hogewind B, Ciggaar I. No significant gender difference in vision-related quality of life of anterior uveitis patients. Austin J Clin Ophthalmol. 2018;5(2).
Karimy M, Parvizi F, Rouhani MR, Griffiths MD, Armoon B, Fattah ML. The association between internet addiction, sleep quality, and health-related quality of life among Iranian medical students. J Addict Dis. 2020;38(3):317–25.
Araya M, Chotai J, Komproe IH, de Jong JTVM. Effect of trauma on quality of life as mediated by mental distress and moderated by coping and social support among post-conflict displaced Ethiopians. Qual Life Res. 2007;16(6):915–27.
Neyazi A, Hosaini F, Razaqi N, Ahmadi M, Padhi BK, Neyazi M, Noorzad E, Rahmani A, Griffiths MD. The physical and mental aspects of quality of life among patients with eye diseases: a cross-sectional survey study in Afghanistan. Research Square. https://doi.org/10.21203/rs.3.rs-3094767/v1.
HealthNet TPO. Eye care in Afghanistan. https://www.healthnettpo.org/en/project/eye-care-afghanistan.
Reliefweb. Persistent Barriers to Access Healthcare in Afghanistan: The Ripple Effects of a Protracted Crisis and a Staggering Economic Situation. https://reliefweb.int/report/afghanistan/persistent-barriers-access-healthcare-afghanistan-ripple-effects-protracted-crisis-and-staggering-economic-situation.
Harsch S, Jawid A, Jawid M, Bittlingmayer U. Health literacy, the role of beliefs and barriers in Afghanistan. A quantitative study: Stefanie Harsch. Eur J Public Health. 2017;27(suppl3):186–228.
Acknowledgements
We would like to express our sincere gratitude to all the participants who enrolled in the present study.
This article’s preprint has already been published in Research Square [39].
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
A.N. and F.H. designed the study. N.R., M.N., H.A., R.M.T., E.N., and A.R. contributed in data collection of this study. A.N. and B.K.P analyzed the data. A.N., M.A., M.N., H.A., R.M.T., and F.H. prepared the draft of the manuscript. A.N., F.H., and M.D.G. critically reviewed, rewrote, edited, and finalized the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethical approval from the Ethical Committee of the Afghanistan Center for Epidemiological Studies (ref: #21.021). Prior to involving participants, a comprehensive explanation of the study was provided. Consent was obtained from all participants, who were informed of their right to withdraw from the study at any time. All procedures adhered to pertinent ethical guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Neyazi, A., Hosaini, F., Razaqi, N. et al. The physical and mental aspects of quality of life among patients with eye diseases: a cross-sectional survey study in Afghanistan. Discov Public Health 21, 49 (2024). https://doi.org/10.1186/s12982-024-00169-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12982-024-00169-y