Abstract
Background
Human Immunodeficiency Virus (HIV) infection remains a public health concern in many countries. The increased life expectancy in the post-Antiretroviral Therapy (ART) era has led to an increased risk of cardiovascular disease and death among Persons Living with HIV (PLHIV). Hypertension remains a significant risk factor for cardiovascular disease among PLHIV. Some studies have suggested associations between hypertension among PLHIV and HIV-related health factors.
Objective
To determine the prevalence of hypertension among PLHIV on antiretroviral medications and examine its association with HIV-related health factors.
Methods
A cross-sectional study was conducted among attendants at an adult HIV clinic. 362 study participants were selected by systematic sampling. Data on hypertension diagnosis, HIV-related health factors, sociodemographic and other traditional cardiovascular risk factors were collected using a standardized questionnaire and patient chart review. Multivariate logistic regression model was used to determine the association between hypertension and HIV-related factors, adjusting for other risk factors for hypertension.
Results
The mean age of participants was 47.9 years and majority of participants were female (77.1%). 42% of study participants had been on antiretroviral medications for > 10 years. The prevalence of hypertension was 17.4%. Age > 50 years was associated with higher odds of hypertension (aOR: 3.75, 95%CI 1.68, 8.55, p-value: 0.002). BMI in overweight and obese categories, and a history of comorbid medical conditions (diabetes, hyperlipidemia) were also associated with higher odds of hypertension (aOR: 3. 76, 95%CI 1.44, 9.81, p-value: 0.007), (aOR: 3.17, 95%CI 1.21, 8.32, p-value: 0.019) and (aOR: 14.25, 95%CI 7.41, 27.41, p-value: < 0.001) respectively. No HIV-related health factors were associated with hypertension.
Conclusion
Hypertension was a common condition among PLHIV on antiretroviral medications. No HIV-related health factors were associated with hypertension. Traditional risk factors associated with hypertension were increased age > 50 years, increased BMI, and a history of comorbid medical conditions.
Similar content being viewed by others
Background
HIV continues to pose a significant public health challenge worldwide, with more than 37 million individuals living with the virus [1]. Although antiretroviral medications have markedly reduced mortality rates, a cure for HIV remains elusive [2]. Nevertheless, the incidence of cardiovascular disease-related mortality has notably risen among People Living with HIV (PLHIV) [3, 4]. Hypertension, a well-established risk factor for cardiovascular disease and mortality [5,6,7], is emerging as a growing concern among this population [3, 8]. Sub-Saharan African countries, which bear the highest global burden of both HIV and hypertension, are particularly affected [1, 9].
The prevalence of hypertension among PLHIV has surged, largely attributable to increased life expectancy resulting from expanded access to antiretroviral medications [10, 11]. A study conducted in Kenya estimated the prevalence of hypertension among PLHIV on antiretroviral therapy to range from 6 to 50% [12]. Similarly, investigations in Burundi and Zambia reported prevalence rates of 17.4% and 18.4%, respectively [13, 14].
Various mechanisms have been proposed to explain the heightened risk of hypertension in HIV-infected individuals, including microbial translocation, chronic inflammation, immune reconstitution, lipodystrophy, adipocytokines, neuroendocrine responses, and HIV-related renal disease [15,16,17,18,19,20]. Epidemiological factors contributing to the increased prevalence of hypertension among PLHIV are manifold. The improved survival of PLHIV receiving antiretroviral therapy is associated with a heightened risk of developing traditional hypertension risk factors, such as advancing age, lifestyle-related risk factors, and comorbid medical conditions [13, 21, 22].
Certain HIV-related health factors have also been linked to hypertension among PLHIV. Some studies have suggested that the use of specific antiretroviral medications, notably those in the protease inhibitors (PIs) and integrase strand transfer inhibitors (INSTI) classes, may increase the incidence of metabolic syndrome and weight gain, thereby elevating the risk of hypertension [12, 14, 23, 24]. Furthermore, a study conducted in Ethiopia identified associations between hypertension among PLHIV and the duration of HIV infection and the duration of antiretroviral medication use [22]. While certain studies have suggested a connection between CD4 count and hypertension, others have not found a significant association [3, 7, 25].
Given the substantial burden of both HIV and hypertension in Sub-Saharan Africa, there is a pressing need for further research examining the interplay between these two conditions in this region. Consequently, our study aims to determine the prevalence of hypertension among PLHIV at the Infectious Disease Unit of the Korle-Bu Teaching Hospital in Ghana, while also exploring its association with some HIV-related health factors.
Materials and methods
Study design and data collection
This was a facility-based analytic cross-sectional study among attendants of the adult HIV clinic at Korle Bu Teaching Hospital between June and August 2020. The study was limited to PLHIV aged 18 years and above who had been on antiretroviral treatment for at least 6 months. A standardized questionnaire was used for data collection on hypertension diagnosis, sociodemographic and health factors of study participants. In addition, participant health information such as confirmation of hypertension diagnosis, BMI, and comorbid medical conditions as well as HIV-related health factors including duration of HIV diagnosis, duration on antiretrovirals, HIV-typing, ART regimen, and viral load within the past year was extracted from participants’ medical records.
Self-adherence to medications was ascertained for all participants. The study protocol (KBTH-IRB/00047/2020) was reviewed and approved by the Korle Bu Teaching Hospital Institutional Review Board on 27th May 2020.
Dependent and explanatory variables
The dependent variable of interest was a diagnosis of hypertension. This was derived from participants' responses of ‘Yes’ or ‘No’ to a history of hypertension. Diagnosis was confirmed with a review of participants’ medical records.
HIV-related health factors
Health-related factors examined in this study were HIV type, HIV viral load, duration of HIV diagnosis, duration of ART treatment, ART regimen, ART adherence rate, and comorbidities. These were obtained from patients using the questionnaire and review of patient health records.
ART adherence rate was assessed by a standardized 30 day recall of medications using the Brief Adherence Rating Scale (BARS) and pill count. History of comorbid medical conditions (diabetes and hyperlipidemia), smoking history and BMI were also derived from medical record reviews.
Sociodemographic factors
Data were collected on sociodemographic factors such as age, education, sex, marital status, using a standardized questionnaire.
Statistical analyses
Descriptive statistics were first produced for each variable. Following this, univariate tests were performed to examine the association between hypertension and HIV-related health factors, socio-demographic factors and some traditional risk factors of hypertension.
Multiple logistic regression was then utilized to examine the association between hypertension and HIV-related health factors adjusting for sociodemographic and other predictor variables. All analyses were done with STATA (version 16). Statistical tests were 2-sided, and the significance level was set at 0.05.
Results
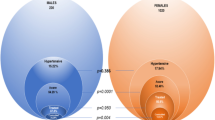
Mean age was 47.9 years and majority of participants were female (77.1%). 42% of study participants had been on antiretroviral medications for > 10 years. The prevalence of hypertension was 17.4% (63/362). Univariate analysis showed no difference in HIV-related health factors between participants who had hypertension and those without hypertension.
Age, history of comorbid medical conditions (diabetes, hyperlipidemia), BMI category were statistically associated with hypertension. Table 1 summarizes the results of univariate tests.
Results of the multivariate logistic regression showed that adjusted for socio-demographic factors and traditional risk factors for hypertension, no HIV-related health factor was associated with hypertension. Table 2 provides a summary of results of the multivariate logistic regression.
Discussion
From our study, we observed a prevalence of hypertension among People Living with HIV (PLHIV) at 17.4%. This prevalence aligns closely with findings from studies conducted in Burundi and Zambia [13, 14]. Slightly lower prevalence rates were reported from studies conducted in Ethiopia (14%) and Tanzania (8%) [26, 27]. Conversely, Dzudie et al. reported a higher rate of 23.9% in Cameroon [28], and a separate study from Nigeria found a prevalence rate of 24.9% [29]. Other studies reported hypertension prevalence rates among PLHIV to be 27% and 53% in Uganda and South Africa, respectively [30, 31]. Within the general population of Ghana, hypertension prevalence has been reported to range between 13% and 27.3% [32, 33]. These findings suggest that the prevalence of hypertension among PLHIV in Ghana is in line with that observed in PLHIV populations in other Sub-Saharan African nations, and the general population in Ghana. A systematic review study estimated the global prevalence of hypertension among PLHIV to be approximately 25.2%, with studies from the USA and Malaysia reporting higher prevalence rates compared to our study’s results [34,35,36].
In our analysis, factors significantly associated with hypertension in our sample population included age 50 years and above, Body Mass Index (BMI) falling within the overweight and obese categories, and a history of comorbid medical conditions such as diabetes and hyperlipidemia. These risk factors have long been established as traditional associations with hypertension and cardiovascular disease [37,38,39,40,41]. A hypertension awareness and screening study conducted in Ghana also identified increasing age and elevated BMI as significant factors associated with hypertension in the general population [36].
Of note is the finding that factors such as the duration of HIV diagnosis, HIV type, viral load, duration on antiretroviral treatment, antiretroviral adherence rate, and antiretroviral regimen were not significantly associated with hypertension in our study. Similar findings have been reported in several studies investigating the association between hypertension and these HIV-related health factors [13, 42]. In contrast, some studies have reported associations between hypertension and antiretroviral medication regimens based on Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) and Protease Inhibitors (PIs) [14, 43]. Given the concerns surrounding incident hypertension attributed to antiretroviral medications among PLHIV, this finding carries important implications for clinicians, policymakers, and other stakeholders involved in HIV control programs in Ghana. However, it is important to acknowledge that our study's cross-sectional design leaves room for residual confounding, and findings may differ in studies employing alternative designs, such as cohort studies or randomized control studies(RCTs). As such, this finding does not negate the need for ongoing monitoring of PLHIV on antiretroviral medications and the implementation of hypertension screening protocols in facilities providing care to PLHIV.
In light of these findings, it is imperative to consider the adoption and implementation of integrated chronic disease management models, as demonstrated in Uganda and South Africa, which have yielded positive results in the diagnosis and management of hypertension among PLHIV [44, 45]. Sensitization of care providers responsible for PLHIV to the increasing burden of hypertension and other cardiovascular disease risk factors is also crucial in reducing cardiovascular disease-related mortality.
Limitations
Our study has some limitations. Firstly, this was a single-site study with a cross-sectional design which lacks the ability to establish causality. The study was limited to the HIV clinic attendants who were on antiretroviral treatments, and findings may not be the same among PLHIV who are not clinic attendants or are not on antiretroviral treatment. The comorbid medical conditions used as part of the study were diabetes and dyslipidemia. This fails to consider other medical conditions that are associated with hypertension.
Conclusion
Hypertension remains highly prevalent among PLHIV although no HIV-related health factor was associated with hypertension in this study. Hypertension was however associated with some traditional risk factors for hypertension. Given the significant prevalence of hypertension among PLHIV, there is a need for an integrative disease management approach in managing both diseases. Further studies among PLHIV on antiretroviral medication using a prospective cohort study design is needed to further study the association between hypertension and HIV-related health factors.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- HIV:
-
Human Immunodeficiency Virus
- PLHIV:
-
Persons living with HIV
- CVD:
-
Cardiovascular disease
- ART:
-
Antiretroviral therapy
References
World Health Organization (WHO). HIV/AIDS Fact sheet. Accessed 10 July 2022.
Cummins NW, Badley AD. Can HIV be cured and should we Try? Mayo Clin Proc. 2015;90(6):705–9. https://doi.org/10.1016/j.mayocp.2015.03.008.
Fahme SA, Bloomfield GS, Peck R. Hypertension in HIV-infected adults: novel pathophysiologic mechanisms. Hypertension. 2018;72:44–55. https://doi.org/10.1161/HYPERTENSIONAHA.118.10893.
Feinstein MJ, Bahiru E, Achenbach C, et al. Patterns of cardiovascular mortality for HIV-infected adults in the United States: 1999 to 2013. Am J Cardiol. 2016;117:214–20.
Nüesch R, Wang Q, Elzi L, Bernasconi E, Weber R, Cavassini M, Vernazza P, Thurnheer MC, Calmy A, Battegay M, Bucher HC. Risk of cardiovascular events and blood pressure control in hypertensive HIV-infected patients: Swiss HIV Cohort Study (SHCS). J Acquir Immune Defic Syndr. 2013;62(396):404. https://doi.org/10.1097/QAI.0b013e3182847cd0.
Onen NF, Overton ET, Seyfried W, Stumm ER, Snell M, Mondy K, Tebas P. Aging and HIV infection: a comparison between older HIV-infected persons and the general population. HIV Clin Trials. 2010;11:100–9. https://doi.org/10.1310/hct1102-100.
Peck RN, Shedafa R, Kalluvya S, Downs JA, Todd J, Suthanthiran M, Fitzgerald DW, Kataraihya JB. Hypertension, kidney disease, HIVand antiretroviral therapy among Tanzanian adults: a cross-sectional study. BMC Med. 2014;12:125. https://doi.org/10.1186/s12916-014-0125-2.
Gazzaruso C, Bruno R, Garzaniti A, Giordanetti S, Fratino P, Sacchi P, Filice G. Hypertension among HIV patients: prevalence and relationships to insulin resistance and metabolic syndrome. J Hypertens. 2003;21:1377–82. https://doi.org/10.1097/01.hjh.0000059071.43904.dc.
Ferdinand KC. Uncontrolled hypertension in sub-Saharan Africa: Now is the time to address a looming crisis. J Clin Hypertens. 2020;22(11):2111–3. https://doi.org/10.1111/jch.14046.
Zoest RA, Wit FW, Kooij KW, van der Valk M, Schouten J, Kootstra NA, Wiersinga WJ, Prins M, van den Born BJ, Reiss P. Higher prevalence of hypertension in HIV-1-infected patients on combination antiretroviral therapy is associated with changes in body composition and prior stavudine exposure. Clin Infect Dis. 2016;63(205):213. https://doi.org/10.1093/cid/ciw285.
Xu Y, Chen X, Wang K. Global prevalence of hypertension among people living with HIV: a systematic review and meta-analysis. J Am Soc Hypertens. 2017;11:530–40. https://doi.org/10.1016/j.jash.2017.06.004.
Dillon DG, Gurdasani D, Riha J, et al. african partnership for chronic disease research (APCDR). association of HIV and ART with cardiometabolic traits in sub-Saharan Africa: a systematic review and meta-analysis. Int J Epidemiol. 2013;42:1754–71. https://doi.org/10.1093/ije/dyt198.
Harimenshi D, Niyongabo T, Preux PM, Aboyans V, Desormais I. Hypertension and associated factors in HIV-infected patients receiving antiretroviral treatment in Burundi: a cross-sectional study. Sci Rep. 2022;12(1):20509. https://doi.org/10.1038/s41598-022-24997-7.
Musekwa R, Hamooya BM, Koethe JR, Nzala S, Masenga SK. Prevalence and correlates of hypertension in HIV-positive adults from the Livingstone Central Hospital, Zambia. Pan Afr Med J. 2021;12(39):237. https://doi.org/10.11604/pamj.2021.39.237.29718.
Blodget E, Shen C, Aldrovandi G, Rollie A, Gupta SK, Stein JH, Dubé MP. Relationship between microbial translocation and endothelial function in HIV infected patients. PLoS One. 2012;7:e42624. https://doi.org/10.1371/journal.pone.0042624.
Crane HM, Van Rompaey SE, Kitahata MM. Antiretroviral medications associated with elevated blood pressure among patients receiving highly active antiretroviral therapy. AIDS. 2006;20:1019–26. https://doi.org/10.1097/01.aids.0000222074.45372.00.
Bautista LE, Vera LM, Arenas IA, Gamarra G. Independent association between inflammatory markers (C-reactive protein, interleukin-6, and TNF-alpha) and essential hypertension. J Hum Hypertens. 2005;19:149–54. https://doi.org/10.1038/sj.jhh.1001785.
Freitas P, Carvalho D, Santos AC, Madureira AJ, Xerinda S, Martinez E, Pereira J, Sarmento A, Medina JL. Central/Peripheral fat mass ratio is associated with increased risk of hypertension in HIV-infected patients. J Clin Hypertens (Greenwich). 2012;14:593–600. https://doi.org/10.1111/j.1751-7176.2012.00671.x.
Wang J, Wang H, Luo W, Guo C, Wang J, Chen YE, Chang L, Eitzman DT. Leptin-induced endothelial dysfunction is mediated by sympathetic nervous system activity. J Am Heart Assoc. 2013;2: e000299. https://doi.org/10.1161/JAHA.113.000299.
Ascher SB, Scherzer R, Peralta CA, Tien PC, Grunfeld C, Estrella MM, Abraham A, Gustafson DR, Nowicki M, Sharma A, Cohen MH, Butch AW, Young MA, Bennett MR, Shlipak MG. Association of kidney function and early kidney injury with incident hypertension in HIV-infected women. Hypertension. 2017;69:304–13. https://doi.org/10.1161/HYPERTENSIONAHA.116.08258.
Todowede OO, Sartorius B, Magula N, Schutte AE. Association of predicted 10 years cardiovascular mortality risk with duration of HIV infection and antiretroviral therapy among HIV-infected individuals in Durban. South Africa Diabetol Metab Syndr. 2019;11:105. https://doi.org/10.1186/s13098-019-0502-2.
Fiseha T, Belete AG, Dereje H, Dires A. Hypertension in HIV-infected patients receiving antiretroviral therapy in Northeast Ethiopia. Int J Hypertens. 2019;23(2019):4103604. https://doi.org/10.1155/2019/4103604.
Pangmekeh PJ, Awolu MM, Gustave S, Gladys T, Cumber SN. Association between highly active antiretroviral therapy (HAART) and hypertension in persons living with HIV/AIDS at the Bamenda regional hospital. Cameroon Pan Afr Med J. 2019;33:87.
Eckard AR, McComsey GA. Weight gain and integrase inhibitors. Curr Opin Infect Dis. 2020;33(1):10–9.
Dimala CA, Kadia BM, Kemah BL, Tindong M, Choukem SP. Association between CD4 cell count and blood pressure and its variation with body mass index categories in HIV-infected patients. Int J Hypertens. 2018;2018(22):1691474. https://doi.org/10.1155/2018/1691474.
Gebrie A. Hypertension among people living with human immunodeficiency virus receiving care at referral hospitals of Northwest Ethiopia: a cross-sectional study. PLoS ONE. 2020;15(8): e0238114. https://doi.org/10.1371/journal.pone.023811.
Mosha NR, Mahande M, Juma A, Mboya I, Peck R, Urassa M, Michael D, Todd J. Prevalence, awareness and factors associated with hypertension in North West Tanzania. Glob Health Action. 2017;10(1):1321279.
Dzudie A, Hoover D, Kim H-Y, Ajeh R, Adedimeji A, Shi Q, et al. Hypertension among people living with HIV/AIDS in Cameroon: a cross-sectional analysis from Central Africa international epidemiology databases to evaluate AIDS. PLoS ONE. 2021;16(7): e0253742. https://doi.org/10.1371/journal.pone.0253742.
Jackson IL, Lawrence SM, Igwe CN, Ukwe CV, Okonta MJ. Prevalence and control of hypertension among people living with HIV receiving care at a Nigerian hospital. Pan Afr Med J. 2022;21(41):153. https://doi.org/10.11604/pamj.2022.41.153.21809.
Migisha R, Ario AR, Kadobera D, et al. High blood pressure and associated factors among HIV-infected young persons aged 13 to 25 years at selected health facilities in Rwenzori region, western Uganda, September–October 2021. Clin Hypertens. 2023;29:6. https://doi.org/10.1186/s40885-022-00230-5.
Tsuro U, Oladimeji KE, Pulido-Estrada G-A, Apalata TR. Risk Factors attributable to hypertension among hiv-infected patients on antiretroviral therapy in selected Rural Districts of the Eastern Cape Province, South Africa. Int J Environ Res Public Health. 2022;19(18):11196. https://doi.org/10.3390/ijerph191811196.
Sanuade OA, Boatemaa S, Kushitor MK. Hypertension prevalence, awareness, treatment and control in Ghanaian population: evidence from the Ghana demographic and health survey. PLoS ONE. 2018;13:1–18.
Tannor EK, Nyarko OO, Adu-Boakye Y, Owusu Konadu S, Opoku G, Ankobea-Kokroe F, Opare Addo M, Amuzu EX, Ansah GJ, Appiah-Boateng K, Ansong D. Burden of hypertension in Ghana—analysis of awareness and screening campaign in the Ashanti Region of Ghana. JRSM Cardiovasc Dis. 2022;28(11):20480040221075520. https://doi.org/10.1177/20480040221075521.PMID:35111304;PMCID:PMC8801650.
Xu Y, Chen X, Wang K. Global prevalence of hypertension among people living with HIV: a systematic review and meta-analysis. J Am Soc Hypertens. 2017;11(8):530–40. https://doi.org/10.1016/j.jash.2017.06.004.
Hejazi N, Huang MS, Lin KG, Choong LC. Hypertension among HIV-infected adults receiving highly active antiretroviral therapy (HAART) in Malaysia. Glob J Health Sci. 2013;6(2):58–71. https://doi.org/10.5539/gjhs.v6n2p58.PMID:24576366;PMCID:PMC4825229.
Myerson M, Poltavskiy E, Armstrong EJ, Kim S, Sharp V, Bang H. Prevalence, treatment, and control of dyslipidemia and hypertension in 4278 HIV outpatients. J Acquir Immune Defic Syndr. 2014;66(4):370–7. https://doi.org/10.1097/QAI.0000000000000168.
Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294(4):466–72. https://doi.org/10.1001/jama.294.4.466.
Oliveros E, Patel H, Kyung S, et al. Hypertension in older adults: assessment, management, and challenges. Clin Cardiol. 2020;43:99–107. https://doi.org/10.1002/clc.23303.
Qiao W, Zhang X, Kan B, Vuong AM, Xue S, Zhang Y, Li B, Zhao Q, Guo D, Shen X, Yang S. Hypertension, BMI, and cardiovascular and cerebrovascular diseases. Open Med (Wars). 2021;16(1):149–55. https://doi.org/10.1515/med-2021-0014.PMID:33585690;PMCID:PMC7862997.
Tsimihodimos V, Gonzalez-Villalpando C, Meigs JB, Ferrannini E. Hypertension and diabetes mellitus: coprediction and time trajectories. Hypertension. 2018;71:422–8.
Halperin RO, Sesso HD, Ma J, Buring JE, Stampfer MJ, Gaziano JM. Dyslipidemia and the risk of incident hypertension in men. Hypertension. 2006;47:45–50.
Medina-Torne S, Ganesan A, Barahona I, Crum-Cianflone NF. Hypertension is common among HIV-infected persons, but not associated with HAART. J Int Assoc Phys AIDS Care. 2012;11(1):20–5. https://doi.org/10.1177/1545109711418361.
Zanuzzi MG, Cattaneo MJ, López SM, Pérez Maure MLÁ, Romero CA. Hipertensión y síndrome metabólico en pacientes con virus de la inmunodeficiencia-humana Hypertension and metabolic syndrome in HIV infected patients. Medicina (B Aires). 2020;80(5):453–61.
Muddu M, Tusubira AK, Sharma SK, Akiteng AR, Ssinabulya I, Schwartz JI. Integrated hypertension and HIV care cascades in an HIV treatment program in eastern uganda: a retrospective cohort study. JAIDS J Acquir Immune Defic Syndr. 2019;81:552–61.
Ameh S. Evaluation of an integrated HIV and hypertension management model in rural South Africa: a mixed methods approach. Glob Health Action. 2020;13:1750216.
Acknowledgements
The authors would like to acknowledge all the staff of the Infectious Disease Unit of the Korle Bu Teaching Hospital who helped with this study. They also want to acknowledge all the patients who agreed to participate in this study for being gracious and willing to take part in the study.
Funding
The authors received no funding for this study.
Author information
Authors and Affiliations
Contributions
MKID—Study design, drafting of article, data analysis, review and revisions, final approval; MAEB, RR, OO—review and revisions, final approval; KPB—study conceptualization and design, drafting of article, review and revisions, final approval.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Korle Bu Teaching Hospital Institutional Review Board (IRB) reviewed and approved the study protocol on 27th May, 2020. (Protocol Number KBTH-IRB /00047/2020). All study methods were carried out in accordance with relevant guidelines and regulations including the Declaration of Helsinki. Informed consent was obtained from all study subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Denu, M.K.I., Revoori, R., Buadu, M.A.E. et al. Hypertension among persons living with HIV/AIDS and its association with HIV-related health factors. AIDS Res Ther 21, 5 (2024). https://doi.org/10.1186/s12981-023-00576-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-023-00576-2