Abstract
Objective
This study investigated prevalence trends and identified the associated factors of HIV, syphilis and hepatitis C virus (HCV) among pregnant women in the Guangxi Zhuang Autonomous Region (Guangxi), Southwest China.
Methods
Serial cross-sectional surveys were performed annually among pregnant women in Guangxi from 2009 to 2018. Blood specimens were collected to test the prevalence of HIV, syphilis and HCV. Cochran–Armitage analysis was used to assess the trends of HIV, syphilis and HCV prevalence, as well as the sociodemographic and behavioural data. In this study, we used zero-inflated negative binomial (ZINB) regression models to identify factors associated with HIV, syphilis and HCV infection.
Results
A total of 23,879 pregnant women were included in the study. The prevalence of HIV, syphilis and HCV was 0.24%, 0.85% and 0.19%, respectively. There was a decrease in HIV prevalence from 0.54% to 0.10%, a decrease in HCV prevalence from 0.40% to 0.05% and a decrease in syphilis prevalence from 1.53% to 0.30%. The findings based on the ZINB model revealed that pregnant women who had a history of STI had significantly increased risks of HIV (OR 6.63; 95% CI 1.33–32.90) and syphilis (OR 9.06; 95% CI 3.85–21.30) infection, while pregnant women who were unmarried/widowed/divorced were more likely to have HIV (OR 2.81; 95% CI 1.20–6.54) and HCV (OR 58.12; 95% CI, 3.14–1076.99) infection. Furthermore, pregnant women whose husband had a history of STI (OR 5.62; 95% CI 1.24–25.38) or drug use (OR 7.36; 95% CI 1.25–43.43) showed an increased risk of HIV infection.
Conclusions
There was a relatively low prevalence of HIV, syphilis and HCV among pregnant women. Although decreasing trends in HIV, syphilis and HCV infections were observed, effort is needed to promote STI testing in both premarital medical check-ups and antenatal care, especially targeting couples with a history of STI or drug use.
Similar content being viewed by others
Introduction
Sexually transmitted infections (STI) continue to be a public health concern, especially in developing countries [1,2,3]. Studies have demonstrated that human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS), syphilis and hepatitis C virus (HCV) are the most commonly reported STI in pregnant women [4]; their main routes of transmission are sexual exposure and vertical transmission [2]. Physiological changes in pregnant women may increase the susceptibility to STI [5, 6] and result in devastating health consequences [6,7,8] and adverse pregnancy outcomes [9].
In 2019, about 1.7 million people became newly infected with HIV worldwide, of which 48% were females; also, there were 1.8 million children (0–14 years) living with HIV in 2019 [10]. Most women and children infected with HIV came from developing countries [10]. Globally, there were 6.3 million new cases of syphilis, representing a prevalence of 0.69% among pregnant women, with approximately 355,000 adverse pregnancy outcomes caused by mother-to-child transmission (MTCT) in 2016 [11]. Estimates of the World Health Organisation (WHO) state that approximately 71 million people have chronic HCV infection worldwide [12] and those who are chronically infected will develop cirrhosis or liver cancer. However, the epidemiology of HCV during pregnancy is still poorly documented. The scope of HIV, syphilis, or HCV infection among pregnant women needs to be better understood for resources to be allocated and to improve the quality of life of infants exposed to and/or infected with these viruses.
Although the prevalence of HIV [13, 14], syphilis [15, 16] and HCV [17, 18] among pregnant women has been shown in a few observational studies, there has been no comprehensive and up-to-date study on the epidemiology of these three STI in an area severely affected by HIV/AIDS. To date, studies about these infections are limited and mainly concentrated on the detection [13] or treatment of these infections, pregnancy outcomes [19] and associated factors [20]. Despite several studies reporting that the lack of formal education, inadequate access to healthcare and poverty increase the risk of spreading infectious diseases, mainly in low- and middle-income countries [2, 21], limited information regarding behavioural characteristics of the spread of infectious diseases is available among pregnant women from Southwest China. Identifying the risk factors related to HIV, syphilis and HCV infection among pregnant women could be beneficial for guiding policy formulation and initiating effective targeted preventive interventions in the population. The most cost-effective method to prevent MTCT of STI is routine testing for STI. There are barriers to preventing STI transmission due to a lack of awareness of the risk factors for STI and the extent of the problem. Thus, this study aimed to estimate the prevalence of HIV, syphilis and HCV among pregnant women and identify factors associated with these infections in Guangxi, Southwest China.
Methods
Study design and participants
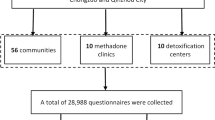
The consecutive cross-sectional study was conducted among pregnant women attending antenatal care between April 2009 and September 2018 in Guangxi, Southwest China. All eligible pregnant women aged from 15 to 49 years-old who self-reported for the first antenatal visit were included after providing informed consent. The following sociodemographic and behavioural data were collected during individual interviews using a standardised questionnaire: age, ethnicity, marital status, education, awareness of HIV-related knowledge, gravidity, parity, multiple sexual partners, history of out-migrating for work and history of STI and drug use (her or her husband) (Additional file 1). HIV/AIDS-related knowledge was assessed using eight basic questions regarding HIV transmission routes, treatment and preventive measures. Those who had a cumulative score of 6 or above were considered as having accurate HIV/AIDS-related knowledge [22, 23].
STI detection
About 5 ml of peripheral blood was collected from each participant by trained physicians for serological testing. Briefly, blood specimens were tested for antibodies against HIV, syphilis and HCV. HIV antibody testing was performed according to standardized operating procedures based on the manufacturer’s instructions. Any specimen that screened positive by enzyme-linked immunosorbent assay (ELISA) (Wantai Biological Pharmaceutical Co., Beijing, China) was confirmed by western blot (WB) assay (HIV Blot 2.2 WB; Genelabs Diagnostic, Singapore). For syphilis, rapid plasma regain (RPR) (Rongsheng Biotechnical Company, Shanghai, China) was used as a screening test and positive samples were confirmed by Treponema pallidum particle agglutination (TPPA, Serodia; Fujirebio, Fuji, Japan). Subjects with positive results for both RPR and TPPA were considered to have a current syphilis infection. HCV antibody testing was performed using an IgG-based ELISA (Wantai Biological Pharmaceutical Co., Beijing, China).
Statistical analysis
All data were double entered into EpiData version 3.1 software for Windows (Odense, Denmark) and then transferred to SPSS version 22.0 software (Chicago, IL, USA) and R version 4.2.0 for statistical analysis. The frequencies and percentages for qualitative variables were calculated by year of survey (2009–2018). Cochran–Armitage trend analysis was used to assess the trends of HIV, syphilis and HCV prevalence and risk behaviours.
The zero-inflated negative binomial (ZINB) regression models [24, 25] were used to identify the risk factors associated with three binary outcome variables: HIV, syphilis and HCV infection. As the three STI infections were most commonly 0 and the standard deviation was larger than the mean, the analysis was performed using the pscl package (version 1.5.5) in R. The ZINB regression model can account for the over-dispersion of count data, handle issues related to the presence of many zero values and improve the overall explanatory power by accounting for zero values [26] (Additional file 2: Table S1). Some covariates with few counts were excluded from the ZINB regression model. Crude odds ratios (cOR) from univariate logistic regression models, adjusted odds ratios (aOR) from the ZINB regression model and their respective 95% confidence intervals (95% CI) were presented in a table. The reported p-values are two-tailed and deemed statistically significant when p < 0.05.
Results
Characteristics of participants
A total of 23,879 pregnant women with a mean age of 27.89 ± 5.59 years were recruited to the study. As shown in Table 1, most of the participants were younger than 35 years-old (88.27%). The percentage of married women was much higher (91.81%) than the percentage of single/widowed/divorced women (8.19%). Over half of the participants were non-Han ethnic Chinese (62.32%) and received < 9 years of education (71.48%). Approximately three fifths of pregnant women self-reported being in their second gravidity or more and two fifths of participants self-reported having given birth at least once.
Trends of HIV, syphilis and HCV prevalence
As shown in Table 2 and Fig. 1, the overall HIV, syphilis and HCV prevalence among participants was 0.24%, 0.85% and 0.19%, respectively. There was a significant decrease in the overall HIV, syphilis and HCV prevalence among pregnant women during the study period. The prevalence of HIV reduced from 0.54% to 0.00% during 2009–2018, with a cOR of 0.76 (95% CI 0.67–0.85). The seropositive rate of syphilis increased from 2009 to 2012, with the highest prevalence of 1.53% in 2012, and then fell sharply to 0.3% in 2018 with a cOR of 0.91 (95% CI 0.86–0.97). The prevalence of HCV showed a relatively low level, ranging from 0.40% in 2009 to 0.03% in 2014, with a cOR of 0.83 (95% CI 0.73–0.94).
HIV/STI-related knowledge and behaviours
This study found that the awareness of HIV-related knowledge was maintained at a high level and increased from 2009 to 2018 (cOR = 1.17, 95% CI 1.15–1.19). During the study period, the percentage of participants who reported a history of STI and drug use decreased (cOR = 0.76, 95% CI 0.71–0.82; cOR = 0.70, 95% CI 0.59–0.84). Concurrently, the percentage of participants who reported their husbands having a history of STI and drug use also decreased (cOR = 0.76, 95% CI 0.72–0.80; cOR = 0.90, 95% CI 0.83–0.98). However, the percentage of participants who reported having multiple sexual partners remained at a low level (0.51%) and did not show a significant decrease (cOR = 0.93, 95% CI 0.87–1.00). Also, the percentages of multi-gravidae and multi-parity gradually increased (cOR = 1.15, 95% CI 1.14–1.16; cOR = 1.17, 95% CI 1.15–1.18) (Table 3).
Factors associated with three STIs in zero-inflated negative binomial regression
Tables 4, 5 and 6 show factors associated with a negative binomial count model for HIV, syphilis and HCV infections. HIV infection increased among pregnant women who were unmarried/widowed/divorced (aOR = 2.81, 95% CI 1.20–6.54), who had a history of STI (aOR = 6.63, 95% CI 1.33–32.90) and whose husband had a history of STI (aOR = 5.62, 95% CI 1.24–25.38) or drug use (aOR = 7.36, 95% CI 1.25–43.43). However, being ethnic Han was found to be associated with a reduced risk of HIV infection (aOR = 0.16, 95% CI 0.04–0.72) (Table 4). The probability of having a syphilis infection was higher in the group of pregnant women aged more than 35 years-old compared with those aged below 35 years-old (1.54% vs. 0.75%) (Table 5). ZINB regression analysis identified that pregnant women who aged more than 35 years-old were more likely to be at risk of being infected with syphilis (aOR = 1.64, 95% CI 1.00–2.70). The risk of contracting syphilis was also found to be much higher in pregnant women who were ethnic Han (aOR = 3.44, 95% CI 1.40–8.42) and whose husband had a history of STI (aOR = 9.06, 95% CI 3.85–21.30) (Table 5). Only pregnant women who were unmarried/widowed/divorced (aOR = 58.12, 95% CI 3.14–1076.99) increased the risk of having HCV infection in ZINB regression analysis (Table 6).
Discussion
In this work, we first reported the province-wide prevalence of STI among pregnant women in Southwest China. As far as we know, this study has the largest sample size and longest period, which included 10 years of sentinel surveillance data and provided the trends of three STI among pregnant women from 2009 to 2018 in Guangxi, one of the regions that is strongly affected by HIV infection in Southwest China [27]. The findings of this work are of significance to understanding the STI epidemic and evaluating the strategies of STI prevention and control.
Within this study, the prevalence of HIV, syphilis, HCV and co-infection among pregnant women was less than 1% and there was a decreasing trend of STI, with a small fluctuation in the prevalence of syphilis over time. We found that the decreasing HIV prevalence among pregnant women was consistent with other studies based in China [13, 14, 18]. The HIV prevalence reported in this study was lower than that reported in other countries, such as Cameroon (5.70% in 2017) [28], Ethiopia (4.1% in 2011–2014) [29] and Angola (3.0% in 2017) [30]. Simultaneously, the prevalence of syphilis and HCV was also comparatively lower than reported in other studies [28,29,30,31,32], which was higher than 1% for both.
Several reasons could explain the decreasing trend of STI prevalence among pregnant women in this study. One of the reasons could be that China released the National Implementation Guidelines on the Integrated Prevention of MTCT (iPMTCT) of HIV, syphilis and hepatitis B virus (HBV) programme in 2011. Numbers of comprehensive projects targeting women, combining free premarital medical check-ups and the treatment of STI, were provided in various regions of China during the study period. These effective and profitable programmes might have reduced the burden of STI among pregnant women. As shown in the study results, the increasing awareness of HIV-related knowledge and education, along with the decreasing proportion of pregnant women with a history of STI and drug use, could support this explanation. Another potential reason is the change in the main transmission route of HIV from injected drug use (IDU) to sexual transmission [33]. Moreover, it is possible that the low mobility of this population decreased the potential for spreading infections beyond provincial and national borders.
Our results showed that pregnant women who were unmarried/widowed/divorced were 2.8 times more likely to be infected with HIV than those who were married or cohabiting. A similar study also reported that people engaged in a marital relationship were less exposed to HIV infection [34], probably because individuals are more likely to have multiple sexual partners either before marriage or after divorce or separation [35]. Also, multiple sexual partnerships were independently associated with HIV infection [7]. This study also indicated that pregnant women whose husband had a history of drug use had a positive association with HIV infection. This result can be explained by the fact that some men living in the study site (Guangxi, China) who were infected with HIV via drug use transmitted it to their wife 10 years ago by risky sexual behaviours (e.g., unprotected sex) [36], although the main mode of HIV transmission has shifted from intravenous drug use to sexual transmission [37]. Due to Guangxi being situated along a major heroin trafficking route linking Guangxi with Yunnan and Vietnam, and its close proximity to the world’s major heroin-producing area, known as the Golden Triangle [38], routine HIV screening and treatment for this population are also critical. Policies enhancing HIV management, adherence support and prevention services tailored to their needs, as well as harm reduction services, should be more widely adopted to control the transmission of HIV in this population [39]. With women of reproductive age, identifying the route of HIV infection and transmission is important, but more than half of women did not know all three methods of MTCT (e.g., during pregnancy, during delivery and through breastfeeding) [40]. These results emphasized that it is necessary to promote the awareness of HIV related knowledge, enhance HIV testing in both premarital medical check-ups and antenatal care and promote mother-to-child blocking therapy among HIV-infected pregnant women.
This study showed a higher syphilis prevalence among pregnant women aged ≥ 35 years compared to those aged < 35 years. Women in the higher age groups had more sexual experience and a progressively increasing exposure duration to sexual activity could result in the higher risk of syphilis infection [1, 35]. Previous research has indicated that syphilis could also facilitate HIV transmission by compromising the skin barrier, activating immune cells and increasing viral load [41, 42]. Untreated maternal syphilis during pregnancy can result in a variety of adverse outcomes in both pregnancies and infants [2, 9]; therefore, it is crucial to improve the ability to carry out timely interventions to reduce the spread of syphilis infection. There are several recommendations that we can make. Firstly, early identification, integrated antenatal screening and disease surveillance, as well as early medical treatment of syphilis infection among pregnant women, should be widely implemented. Secondly, syphilis screening is required at the first prenatal care examination and should be repeated at delivery. Thirdly, the local health department should conduct patient-level case management for pregnant women infected with syphilis. Case management involves ensuring necessary treatment and follow-up testing during pregnancy.
In this study, pregnant women and husbands who had a history of STI contributed to HIV infection and pregnant women who had a history of STI contributed to syphilis infection. Nevertheless, the early stages of these infections among pregnant women and their husbands may present with minimal or no symptoms, so they may remain undiagnosed and untreated. Untreated STI among pregnant women could represent a serious risk for survival and may increase the risk of HIV, syphilis and HCV transmission to their infants. Untreated male partners are a critical source of maternal reinfection [43], so it is crucial to provide additional age- and risk-based screening for STI during pregnancy, including regular STI testing in pregnant women as well as their sexual partners.
The present study has several limitations. Firstly, this study relied on self-reported data. As such, the underreporting of behaviours such as multiple sexual partners and drug use due to social stigma, desirability and discrimination may have occurred. Secondly, the low number of positive cases may have limited the ability to identify other relevant risk factors in the study. Thirdly, our study was based on consecutive cross-sectional surveys, which limited the ability to examine causal relationships. Hence, further research is needed to address these limitations.
This is the first study to determine the prevalence of HIV, HCV and syphilis and the risk factors among pregnant women with a large sample size in the cross-border region of Guangxi Province, China. Despite the above-mentioned limitations, the prevalence estimated in this long-term consecutive study was derived from data of sentinel surveillance and might be close to the true prevalence of these three STI among pregnant women in this border area. Nevertheless, further studies on behavioural risk factors that influence the emergence and spread of STI in pregnant women need to be carried out in Guangxi.
Conclusions
This study has presented the relatively low HIV, syphilis and HCV prevalence with decreasing trends among pregnant women over a 10-year study in Southwest China. Decreasing HIV/STI-related behaviours such as drug use and having a history of STI infection have been reported. Factors such as being older than 35 years, unmarried/widowed/divorced, having a history of STI and having a history of drug use were the main risk factors for STI infection. The results highlighted the fact that integrated interventions involving screening STI before marriage, diagnostic testing and timely treatments should be implemented and help to further reduce new infections in this group, also avoiding vertical transmission.
Availability of data and materials
The datasets used or analysed in the study are available from the corresponding author on reasonable request.
Abbreviations
- STI:
-
Sexually transmitted infections
- HIV:
-
Human immunodeficiency virus
- AIDS:
-
Acquired immune deficiency syndrome
- HCV:
-
Hepatitis C virus
- MTCT:
-
Mother-to-child transmission
- WHO:
-
World Health Organisation
- ELISA:
-
Enzyme-linked immunosorbent assay
- WB:
-
Western blot
- RPR:
-
Rapid plasma regain
- TPPA:
-
Treponema pallidum particle agglutination
- cOR:
-
Crude odds ratios
- aOR:
-
Adjusted odds ratios
- CI:
-
Confidence intervals
- CDC:
-
Centre for Disease Control and Prevention
- ZINB:
-
Zero-inflated negative binomial
References
Niama R, Loukabou Bongolo N, Bayonne Kombo E, et al. Syphilis and HIV infections among pregnant women attending antenatal clinics in Republic of Congo. Pan Afr Med J. 2017;28:8.
Sebastião C, Neto Z, Jandondo D, et al. HIV, hepatitis B virus, hepatitis C virus, and syphilis among pregnant women attending antenatal care in Luanda, Angola: seroprevalence and risk factors. J Med Virol. 2020;92(12):3265–70.
Hogben M, Leichliter J. Social determinants and sexually transmitted disease disparities. Sex Transm Dis. 2008;35:S13-18.
Ormaeche M, Whittembury A, Pun M, et al. Hepatitis B virus, syphilis, and HIV seroprevalence in pregnant women and their male partners from six indigenous populations of the Peruvian Amazon Basin, 2007–2008. Int J Infect Dis. 2012;16(10):e724–30.
Williams C, Harrison L, Llata E, et al. Sexually transmitted diseases among pregnant women: 5 states, United States, 2009–2011. Matern Child Health J. 2018;22(4):538–45.
Mofenson LM. Risk of HIV acquisition during pregnancy and postpartum: a call for action. J Infect Dis. 2018;218(1):1–4.
Machekano R, Tiam A, Kassaye S, et al. HIV incidence among pregnant and postpartum women in a high prevalence setting. PLoS ONE. 2018;13(12): e0209782.
Thomson KA, Hughes J, Baeten JM, et al. Increased risk of HIV acquisition among women throughout pregnancy and during the postpartum period: a prospective per-coital-act analysis among women with HIV-infected partners. J Infect Dis. 2018;218(1):16–25.
Liao TS, Hashmi A, Lazaroff J, et al. Effect of policy change to require laboratory reporting with pregnancy indicated for syphilis and hepatitis B virus infection, New York City, January 2013–June 2018. Public Health Rep. 2020;135(1_suppl):182S-188S.
Global HIV & AIDS statistics—2020 fact sheet. https://www.unaids.org/en/resources/fact-sheet.
Korenromp E, Rowley J, Alonso M, et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes-Estimates for 2016 and progress since 2012. PLoS ONE. 2019;14(2): e0211720.
World Health Organization, Hepatitis C. https://www.who.int/news-room/fact-sheets/detail/hepatitis-c.
Qiao YP, Wang AL, Wang XY, et al. Status on maternal testing and detection of HIV infection among pregnant women in Liangshan Yi Autonomous Prefecture, Sichuan province, 2008–2016. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(4):552–6.
Yu MR, Yang KX, Xu YB, et al. Analysis on HIV/AIDS surveillance among pregnant women in Taizhou City from 2014 to 2018. Chin J Dis Control Prec. 2019;23(12):1535–8.
Qin QH, Xie XH, Zhang H, et al. Monitoring and analysis on maternal HIV, syphilis and hepatitis B serologic testing in Guangxi, 2011–2016. Chin J Health Educ. 2018;34(1):10–3.
Hu H, Zhang SY, Qiu JM. Analysis of treatment status of syphilis pregnant women and associated factors in Nanchang, Jiangxi province from 2015–2018. Chin J AIDS STD. 2020;26(4):411–5.
Li J, Yang ZR, Jin MH, et al. Analysis of maternal health of AIDS sentinel surveillance in Huzhou during 2016–2019. Chin J AIDS STD. 2021;27(1):86–8.
Song LJ, Luo HB, Zhang ZY, et al. Analysis of AIDS sentinel surveillance among pregnant women in Yunnan from 2010 to 2018. Chin J AIDS STD. 2020;26(12):1342–1344+1358.
Wan Z, Zhang H, Xu H, et al. Maternal syphilis treatment and pregnancy outcomes: a retrospective study in Jiangxi Province, China. BMC Pregnancy Childbirth. 2020;20(1):648.
Albert AYK, Elwood C, Wagner EC, et al. Investigation of factors associated with spontaneous preterm birth in pregnant women living with HIV. AIDS. 2020;34(5):719–27.
Barnighausen T, Hosegood V, Timaeus IM, et al. The socioeconomic determinants of HIV incidence: evidence from a longitudinal, population-based study in rural South Africa. AIDS. 2007;21(Suppl 7):S29–38.
Wang L, Tang WM, Wang L, et al. The HIV, syphilis, and HCV epidemics among female sex workers in china: results from a serial cross-sectional study between 2008 and 2012. Clin Infect Dis. 2014;59(1):E1–9.
tPsRoC. The State Council AIDS Working Committee Office: China HIV/AIDS monitoring and evaluation framework (trial). Beijing: Beijing medical publishing house; 2007.
Zero-inflated negative binomial regression | R data analysis examples. https://stats.oarc.ucla.edu/r/dae/zinb/.
Hailu Amare H, Lindtjørn B. Helminth infections among rural schoolchildren in Southern Ethiopia: a cross-sectional multilevel and zero-inflated regression model. Plos Neglect Trop D. 2020;14(12): e0008002.
Zaninotto P, Falaschetti E. Comparison of methods for modelling a count outcome with excess zeros: application to activities of daily living (ADL-s). J Epidemiol Community Health. 2011;65(3):205–10.
Hu X, Liang B, Zhou C, et al. HIV late presentation and advanced HIV disease among patients with newly diagnosed HIV/AIDS in Southwestern China: a large-scale cross-sectional study. AIDS Res Ther. 2019;16(1):6.
Kengne-Nde C, de Dieu AJ, Loni-Ekali G, et al. Highlighting a population-based re-emergence of syphilis infection and assessing associated risk factors among pregnant women in Cameroon: evidence from the 2009, 2012 and 2017 national sentinel surveillance surveys of HIV and syphilis. PLoS ONE. 2020;15(11): e0241999.
Kassa D, Gebremichael G, Tilahun T, et al. Prevalence of sexually transmitted infections (HIV, hepatitis B virus, herpes simplex virus type 2, and syphilis) in pregnant women in Ethiopia: trends over 10 years (2005–2014). Int J Infect Dis. 2019;79:50–7.
Oliveira D, Martins MDR, Castro R, et al. Seropositivity rate and sociodemographic factors associated to HIV, HBV, HCV and syphilis among parturients from Irene Neto Maternity of Lubango city, Angola. Sex Transm Infect. 2020;96(8):587–9.
Biadgo B, Hassen A, Getaneh M, et al. Syphilis and human immunodeficiency virus infections among pregnant women attending antenatal care clinic of Gondar family guidance association, Northwest Ethiopia: implication for prevention of mother to child transmission. Reprod Health. 2019;16(1):27.
Frempong MT, Ntiamoah P, Annani-Akollor ME, et al. Hepatitis B and C infections in HIV-1 and non-HIV infected pregnant women in the Brong-Ahafo Region, Ghana. PLoS ONE. 2019;14(7): e0219922.
Chen H, Luo L, Pan SW, et al. HIV epidemiology and prevention in southwestern China: trends from 1996–2017. Curr HIV Res. 2019;17(2):85–93.
Anoubissi JD, Gabriel EL, Kengne Nde C, et al. Factors associated with risk of HIV-infection among pregnant women in Cameroon: evidence from the 2016 national sentinel surveillance survey of HIV and syphilis. PLoS ONE. 2019;14(4): e0208963.
Mohamed B, Mahfouz M. Factors associated with HIV/AIDS in Sudan. BioMed Res Int. 2013;2013: 971203.
Qiao YC, Xu Y, Jiang DX, et al. Epidemiological analyses of regional and age differences of HIV/AIDS prevalence in China, 2004–2016. Int J Infect Dis. 2019;81:215–20.
Ge XM, Yang WM, Zhu QY, et al. Epidemiological characteristics of HIV/AIDS in Guangxi Zhuang Autonomous Region, 2010–2017. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40(3):315–21.
Beyrer C, Razak MH, Lisam K, et al. Overland heroin trafficking routes and HIV-1 spread in south and south-east Asia. AIDS. 2000;14(1):75–83.
Han WM, Jiamsakul A, Salleh NAM, et al. HIV treatment outcomes among people who acquired HIV via injecting drug use in the Asia-Pacific region: a longitudinal cohort study. J Int Aids Soc. 2021;24(5): e25736.
Vo Hoang L, Nguyen Si Anh H, Tran Minh H, et al. Trends and changes in the knowledge of mother-to-child transmission means of HIV among Vietnamese women aged 15–49 years and its associated factors: findings from the multiple indicator cluster surveys, 2000–2014. AIDS Care. 2020;32(4):445–51.
Buchacz K, Patel P, Taylor M, et al. Syphilis increases HIV viral load and decreases CD4 cell counts in HIV-infected patients with new syphilis infections. AIDS. 2004;18(15):2075–9.
Reynolds S, Risbud A, Shepherd M, et al. High rates of syphilis among STI patients are contributing to the spread of HIV-1 in India. Sex Transm Infect. 2006;82(2):121–6.
Qin J, Feng T, Yang T, et al. Risk factors for congenital syphilis and adverse pregnancy outcomes in offspring of women with syphilis in Shenzhen, China: a prospective nested case-control study. Sex Transm Dis. 2014;41(1):13–23.
Acknowledgements
The authors thank the staff of the Centre for Disease Control and Prevention of Chongzuo and Qinzhou for supporting and facilitating the study activities. We also thank the study participants for their time and trust.
Funding
The study was supported by the National Natural Science Foundation of China (Grant No. 82060610), National Key Science and Technology Project of China (Grant No. 2018ZX10101002-001-006), Guangxi Scientific and Technological Key Project (Gui Ke AB18050022), and Guangxi Scientific and Technological Key Project (Gui Ke AB19245038).
Author information
Authors and Affiliations
Contributions
SZ and YO conceived the study, organised the data collection, and finalised the manuscript. QW, ZW, and YY performed HIV, syphilis, and HCV tests and wrote the original draft of the manuscript. HL, FZ, and CQ coordinated the study and data analysis. ZL, RH, and AN interpreted the results and reviewed the final manuscript. Xianyan Tang and Dee Yu was in charge of investigation and manuscript development. DL, HL, and BL designed the study and participated in the funding acquisition. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Guangxi Centre for Disease Control and Prevention’s (CDC) institutional ethics review board (GXIRB2014-0041). Written informed consent was obtained from the participants.
Consent for publication
Not applicable.
Competing interests
The authors declared no competing interests with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Maternal quantitative questionnaires.
Additional file 2: Table S1.
Model fitness for three STI among pregnant women in southwest China, 2009–2018.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhong, S., Ou, Y., Zhang, F. et al. Prevalence trends and risk factors associated with HIV, syphilis, and hepatitis C virus among pregnant women in Southwest China, 2009–2018. AIDS Res Ther 19, 31 (2022). https://doi.org/10.1186/s12981-022-00450-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-022-00450-7