Abstract
Objectives
Accelerated atherosclerosis in older HIV-infected patients has been attributed to persistent immune activation and high burden cytomegalovirus (CMV), as demonstrated in transplant recipients and the general population. Here we assess CMV and inflammatory markers linked with vascular health in young adult patients treated in Indonesia.
Study design
HIV-infected adults (n = 32) were examined when they began antiretroviral therapy (ART) with < 200 CD4 T-cells/µl (V0) and after 60 months (V60). Age-matched healthy controls (HC, n = 32) were assessed once.
Methods
Flow Mediated Dilatation (FMD) was assessed by ultrasound on brachial arteries at V60 and in HC. Plasma markers of immune activation and endothelial activation, and CMV antibodies (lysate, gB, IE-1) were assessed in all samples. Results were assessed using bivariate (non-parametric) and multivariable analyses.
Results
Levels of inflammatory biomarkers and CMV antibodies declined on ART, but the antibodies remained higher than in HC. FMD values were similar in patients and HC at V60. In HIV patients, levels of CMV lysate antibody correlated inversely (r = − 0.37) with FMD. The optimal model predicting lower FMD values (adjusted R2 = 0.214, p = 0.012) included CMV lysate antibodies and chondroitin sulphate. In HC, levels of sTNFR correlated inversely with FMD (r = − 0.41) and remained as a risk factor in the optimal multivariable model, with CMV glycoprotein-B (gB) antibody predicting a healthier FMD (adjusted R2 = 0.248, p = 0.013).
Conclusions
Higher levels CMV antibodies optimally predict vascular health measured by FMD in HIV patients. However in healthy controls, sTNFR marks risk and CMV gB antibody may be protective.
Similar content being viewed by others
Introduction
The wide availability of antiretroviral therapy (ART) has changed the profile of HIV disease from a life-threatening illness to one characterised by accelerated age-associated comorbidities, such as cardiovascular disease (CVD) [1]. However the relative contributions of traditional risk factors and HIV disease to vascular pathologies remains unclear, and there have been few studies in resource constrained or Asian populations. Without overt coronary heart disease, one can assess plaque and endothelial dysfunction through plasma biomarkers and non-invasive examinations. Meta-analyses establish increased risk of CVD in HIV-infected individuals based on carotid intima-media thickness (cIMT) and flow-mediated dilatation (FMD) [2], but the authors noted that many co-factors remain to be investigated. FMD assesses earlier stages of endothelium-dependent vasodilator function and has been validated as a surrogate of endothelial function of the coronary circulation, as it associates with prevalent and incident cardiovascular diseases [3]. FMD was independently predicted by high levels of antibodies reactive with cytomegalovirus (CMV) in renal transplant recipients [4]. CMV is addressed here in Indonesian HIV patients (the JakCCANDO study) with a very high CMV burden [5, 6]. In this population, changes to cIMT and cardiac parameters were small in the first year on ART [5].
CMV is a β-herpesvirus and replicates in endothelial cells, fibroblast and monocytes. Chronic infections can up-regulate leucocyte adhesion molecules (e.g. VCAM-1 and ICAM-1) and pro-inflammatory cytokines [7]. Recent meta-analyses establish links between CMV burden (assessed by seropositivity or levels of CMV-reactive antibodies) and CVD in the general population [8]. Hsue et al. [9] reported correlations between T-cell responses to CMV and increased cIMT in HIV patients in the US, and Knudsen et al. [10] described a direct association between levels of CMV-reactive antibodies and cIMT in Danish patients stable on ART. In our cohort, periodontitis and levels of CMV antibodies were independent predictors of raised cIMT after 5 years on ART [11].
Fewer studies have used FMD to assess HIV patients, although Parrinello et al. [12] reported an association between CMV antibodies and arterial stiffness in HIV-infected women. Andrade et al. [13] showed that FMD was significantly lower in Brazilian HIV patients, with a reduction on ART to values below healthy controls. CMV was not considered, and some groups have found no effect of HIV disease on FMD [14]. Here measures of the burden of CMV were evaluated alongside with markers of traditional markers of cardiovascular risk as determinants of FMD after 5 years on ART. We included Body Mass Index (BMI), but note that HIV patients with > 200 CD4 T-cells/µl are often overweight, while many patients with < 200 CD4 T-cells/µl are underweight [15, 16]. Levels of markers of inflammation (sTNFR-2, IL-6), endothelial activation (ICAM-1, VCAM-1) and coagulation (D-dimers) are higher in ART-naive HIV patients than in healthy controls, and may associate with accelerated atherosclerosis [17]. Chondroitin sulphate also plays a role in the modification and accumulation of lipids, especially low-density lipoprotein, and so may be pro-atherogenic in the general population with a role in early atherosclerotic lesions [18]. Patients undergoing endarterectomy to treat atherosclerotic plaque had higher plasma chondroitin sulphate levels than healthy controls [19]. We assess demographic parameters (age, gender, BMI), CD4 T-cell counts, biomarkers of inflammation and endothelial dysfunction (CRP, ICAM-1, sTNFR-1), chondroitin sulphate and CMV antibodies recognising Immediate Early (IE-1), lysate and glycoprotein B (gB) antigens.
Materials and methods
Subjects
JakCCANDO was a comprehensive survey of clinical and immunological responses in 75 HIV-infected patients who began ART with < 200 CD4 T-cells/µl in the HIV outpatient clinic of a tertiary hospital (Cipto Mangunkusumo Hospital, Jakarta, Indonesia) [5, 6, 11]. Here we describe a subset of 32 patients who attended a 5-year follow up (Visit60). Losses to follow up were attributed to increased access to clinics nearer their homes, changed phone numbers or home addresses, refusal to participate further and HIV-related death. Patients who returned and the 43 lost from the cohort were similar in all standard demographic parameters including age (32 ± 7.1 vs 32 ± 6.2 years, p = 0.63) and CD4 T-cell counts at V12 (304 ± 157 vs 332 ± 183 cells/µl, p = 0.26). Thirty-two healthy controls (HC) were assessed around the V60 timepoint, and matched the patient group by age and gender (see Table 1). The Health Research Ethics Committee Faculty of Medicine Universitas Indonesia & Cipto Mangunkusumo Hospital approved the study (no:133/UN2.FI/ETIK/2018) [5, 6].
Carotid intima-media thickness (cIMT)
Carotid Doppler ultrasonography was assessed using an Esaote echocardiography machine and a LA522E probe (Genova, Italy) [4]. The cIMT measurements were performed by a single operator (BK) on greyscale 2D pictures, at sites with no focal lesions.
Flow Mediated Dilatation (FMD)
Flow-mediated vasodilation was assessed in the brachial artery by ultrasonography (Esaote, probe LA522E) at V60. Participants were asked to abstain from exercise, caffeine, smoking or smoke exposure (≥ 12 h), vitamin supplementation (> 3 days), non-steroidal anti-inflammatory agents (1 day) and aspirins (3 days) and food (12 h). The measurements were performed on both arms with the patient in a supine position after 10–20 min rest. The brachial artery was scanned longitudinally above the antecubital crease using linear multi-frequency 5–12 MHz transducer B-mode. The diameter of the artery was measured on the interface between the media and adventitia of the anterior and posterior wall as a baseline. Gain settings were optimised to identify the lumen and the vessel wall interfaces and held constant. Hyperemia was induced by inflation of a pneumatic cuff on the proximal forearm to 200–250 mm Hg for 5 min. Arterial diameters were measured by one investigator (MS) 30–60 s before and after deflation of the cuff. Flow-mediated vasodilation was defined as 100 × [(post-hyperemia diameter − basal diameter)/basal diameter]. FMD values recorded in the right and left arms were correlated (HIV+: r = 0.49, p = 0.006; HC: r = 0.34, p = 0.059).
Soluble TNFR, CRP, ICAM-1 and chondroitin sulphate
Plasma samples were aliquoted and stored at -80C. Soluble (s)TNFR-1, CRP and ICAM-1 were measured by ELISA using commercial antibody pairs (R&D Systems, Minneapolis, MN). Samples were serially diluted from 1:3000 for CRP, 1:100 for ICAM-1 and 1:10 for sTNFR [6]. Chondroitin sulphate was measured using a commercial ELISA kit (MyBioSource, San Diego, CA) with samples diluted 1:10.
CMV Immediate Early (IE)-1, lysate and glycoprotein B (gB) antibodies
CMV-reactive IgG was quantified by ELISA. Parallel plates were coated with a lysate of human fibroblasts infected with CMV AD169, recombinant IE-1 (produced in Escherichia coli, Miltenyi Biotech; Cologne, Germany) and recombinant gB (kindly provided by Sanofi Pasteur; Lyon, France). Plasma samples were serially diluted from 1:10,000 (CMV lysate and gB) or 1:500 (IE-1). The binding was detected using goat anti-human IgG-horseradish peroxidase followed by tetramethylbenzidine substrate (Sigma Aldrich; Castle Hill, Australia). Antibodies were assessed relative to standard plasma pool assigned a value of 1000 arbitrary units (AU) [5, 6]. The method provides accurate quantitation in the high range.
Statistical analyses
HC and HIV-infected patients were compared using non-parametric Mann–Whitney tests, whilst paired Wilcoxon tests were used to assess changes over time in patients. Natural log transformations (Ln) were used to approximate normal distributions where required and Pearson’s texts were used to identify bivariate associations between FMD (left arm) and patient characteristics, biomarkers and CMV antibodies. Multiple linear regression models were then initiated using all factors that achieved p ≤ 0.25 in the Pearson’s tests. Models were optimised by sequential elimination to identify factors that independently predict FMD. Regression analyses were performed in Stata SE 15.1 (StataCorp LP; College Station, TX). P-values < 0.05 are reported as significantly different.
Results
HIV patients maintained on ART for 5 years retain elevated responses to CMV
Smoking histories and age were similar in patients and HC. Patients’ CD4 T-cell counts and BMI increased on ART. Plasma biomarkers parameters generally decreased from V0 to V12 and V60, but were similar to HC at V60. Levels of antibodies reactive with CMV lysate and CMV gB remained elevated relative to HC (Table 1). Patients began ART with slightly higher cIMT values than HC, but FMD values were not significantly different from HC at V60.
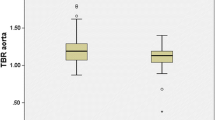
CMV lysate antibodies optimally predict FMD in HIV patients, whereas sTNFR predicts FMD in HC
Levels of CMV lysate antibody recorded at V60 showed a moderate inverse correlation with FMD at V60 in HIV-infected patients (p = 0.035, Table 2A, Fig. 1), linking robust response to CMV with poor vascular health. We found no other significant correlations between FMD and levels of any biomarkers assessed at V0 or V60, but a weak correlation was noted with levels of chondroitin sulphate at V60 (p = 0.110) so this was carried forward into multivariable analysis predicting FMD. Both remained significant in the optimal model (adjusted R2 = 0.214, p = 0.012). Data recorded at V0 did not provide a significant multivariable model predicting FMD at V60 (data not shown).
For HC, plasma levels of sTNFR correlated inversely with FMD (p = 0.021; Table 2A) with weak inverse correlations with BMI (p = 0.074), chondroitin sulphate (p = 0.101), CRP (p = 0.247) and ICAM-1(p = 0.146) and not CMV lysate antibody (Fig. 1). We noted a weak direct association with CMV gB antibody (p = 0.247). These factors were included in our initial models. In the optimal model (Table 2B, adjusted R2 = 0.248, p = 0.013), sTNFR was most clearly associated with risk, but inclusion of chondroitin sulphate improved the model. In contrast, gB antibody appeared weakly protective.
Discussion
Endothelial dysfunction is an early event in the development of atherosclerotic lesions and was assessed here after 5 years on ART using FMD of the brachial artery. FMD did not reveal endothelial damage attributable to HIV disease in our cohort. Previous studies have reported low or normal FMD values in patients on ART [2, 13, 14]. Most studies did not assess CMV but an association between FMD and CMV reactive antibodies was described in a largely middle aged male cohort based in California and stable on ART [20].
Here levels of CMV-reactive antibodies were extremely high in all patients ever tested in our clinic, being assayed from a starting dilution of 1:10,000. Levels decreased over 5 years of ART, but remained higher than in HC. Accordingly, in Australian patients commencing ART with < 210 CD4 T-cells/µL, levels of CMV antibody increased during the first year and remain elevated after 10 years [21]. The rise on ART suggests that levels of CMV-reactive antibody recorded before ART underestimate the high burden of CMV present at that time. The high CMV burden in JakCCANDO patients is evident from our finding that 50% of the cohort began ART with CMV DNA detectable with a simple in-house RT-PCR assay. This associated with low CD4/CD8 ratios and a depletion of naive T-cells and accumulation of memory T-cells, which may be a more stable metrics of the burden of CMV 7. Two patients retained CMV DNA detectable with this assay at V60 (in preparation).
Our key finding is that levels of CMV reactive antibodies on ART correlated inversely with FMD, as they do in renal transplant recipients [4]. The absence of associations between FMD and inflammatory biomarkers fits the observed decrease in these markers on ART to levels similar to healthy controls. The data suggest that CMV has a specific role in the pathogenesis of endothelial dysfunction that is not attributable to enhanced immune activation. It is probably relevant that levels of CMV reactive antibodies remain higher in patients than controls at V60, implying a higher viral burden.
FMD associated inversely with levels of sTNFR in healthy controls, with a weak protective effect of gB antibodies. gB also marked protection in our search for biomarkers that predict FMD measured in Australian renal transplant recipients after an interval of three years [22]. The association is plausible because CMV gB is considered a protective antigen based on its critical role in mediating viral-host cell fusion and thus viral entry. Phase II clinical trials of a monomeric recombinant trimeric CMV gB protein demonstrated efficacy in reducing viremia in solid organ transplantation recipients [23]. A corollary of our finding is that CMV itself is a negative influence in the HC, but is kept in check by a robust immune response marked by gB antibodies.
Chondroitin sulphate was included as a wild-card but was retained in the optimal multivariable models as it associated weakly with unhealthy FMD values in both patients and controls. This is accordance with the literature based on the general population [18, 19]. One can postulate a role in arterial stiffness but further studies should include assessments of other anionic polysaccharides. For example heparan sulfate interacts with HIV at a step prior to CD4 recognition, increasing infectivity by pre-concentrating the virion particles at the cell surface [24]. We have also demonstrated a role for heparan sulphate in murine CMV infection using cells pre-treated with heparinase [25]. However the present dataset shows no correlations between levels of chondroitin sulphate and CD4 T-cell counts (V0; r = -0.05: V60: r = 0.10) or levels of CMV lysate antibody (V0; r = 0.23: V60: r = − 0.05) and levels of chondroitin sulphate are similar in CMV DNA positive and negative patients when assessed at V0, V12 or V60 (p > 0.10). Further studies are needed, but this provides no evidence to link chondroitin sulphate with the burden of HIV or CMV.
We recognise the limitations of our study. The cohort is small and we did not assess plasma lipids or host genotypes. Moreover we did not assess FMD before ART, or assess CMV DNA at regular intervals to detect bursts of CMV replication. Nonetheless we show for the first time that higher levels CMV antibodies optimally predict vascular health measured by FMD in Indonesian HIV patients after 5 years on ART—individuals with a very high burden of CMV. The effect of CMV on FMD in patients was distinct from healthy controls.
Availability of data and materials
Data and relevant materials are available on request.
Abbreviations
- BMI:
-
Body mass index
- cIMT:
-
Carotid intima-media thickness
- CMV:
-
Cytomegalovirus
- FMD:
-
Flow Mediated Dilatation
- CRP:
-
C reactive protein
- ICAM-1:
-
Intercellular adhesion molecule-1
- sTNFR:
-
Soluble tumour necrosis factor receptor
- gB:
-
Glycoprotein B
- IE-1:
-
Immediate Early-1
References
Zanni MV, Schouten J, Grinspoon SK, Reiss P. Risk of coronary heart disease in patients with HIV infection. Nat Rev Cardiol. 2014;11:728–41.
Sun D, Wu Y, Yuan Y, Wang Y, Liu W, Yang J. Is the atherosclerotic process accentuated under conditions of HIV infection, antiretroviral therapy, and protease inhibitor exposure? Meta-analysis of the markers of arterial structure and function. Atherosclerosis. 2015;242:109–16.
Alley H, Owens CD, Gasper WJ, Grenon SM. Ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery in clinical research. J Vis Exp. 2014. https://doi.org/10.3791/52070.
Lee S, Brook E, Affandi J, et al. A high burden of cytomegalovirus marks poor vascular health in transplant recipients more clearly than in the general population. Clin Transl Immunology. 2019;8:e1043.
Karim B, Wijaya IP, Rahmaniyah R, et al. Factors affecting affect cardiovascular health in Indonesian HIV patients beginning ART. AIDS Res Ther. 2017;14(1):52.
Ariyanto IA, Estiasari R, Waters S, et al. Active and persistent cytomegalovirus infections affect T Cells in young adult HIV patients commencing antiretroviral therapy. Viral Immunol. 2018;31:472–9.
Waters S, Brook E, Lee S, Estiasari R, Ariyanto I, Price P. HIV patients, healthy aging and transplant recipients can reveal the hidden footprints of CMV. Clin Immunol. 2018;187:107–12.
Wang H, Peng G, Bai J, et al. Cytomegalovirus infection and relative risk of cardiovascular disease (ischemic heart disease, stroke, and cardiovascular death): a meta-analysis of prospective studies up to 2016. J Am Heart Assoc. 2017;6(7):e005025.
Hsue PY, Hunt PW, Sinclair E, et al. Increased carotid intima-media thickness in HIV patients is associated with increased cytomegalovirus-specific T-cell responses. AIDS. 2006;20:2275–83.
Knudsen A, Kristoffersen US, Panum I, Hansen YB, Skottrup PD, Hasbak P, Kjaer A, Lebech AM. Coronary artery calcium and intima-media thickness are associated with level of cytomegalovirus immunoglobulin G in HIV-infected patients. HIV Med. 2019;20:60–2.
Wulandari EAT, Wijaya IP, Karim B, et al. Periodontitis and cytomegalovirus associate with atherosclerosis among HIV patients after 5 years on ART. JAIDS. 2020;85:195–200.
Parrinello CM, Sinclair E, Landay AL, et al. Cytomegalovirus immunoglobulin G antibody is associated with subclinical carotid artery disease among HIV-infected women. J Infect Dis. 2012;205:1788–96.
Andrade ACO, Ladeia AM, Netto EM, et al. Cross-Sectional study of endothelial function in HIV-Infected patients in Brazil. AIDS Res Hum Retrovir. 2008;24:27–33.
Dysangco A, Liu Z, Stein JH, Dubé MP, Gupta SK. HIV infection, antiretroviral therapy, and measures of endothelial function, inflammation, metabolism, and oxidative stress. PLoS ONE. 2017;12(8):e0183511.
Mariz Cde A, Albuquerque Mde F, Ximenes RA, et al. Body mass index in individuals with HIV infection and factors associated with thinness and overweight/obesity. Cad Saúde Pública. 2011;27:1997–2008.
Crum-Cianflone NF, Roediger M, Eberly LE, et al. Impact of weight on immune cell counts among HIV-infected persons. Clin Vaccine Immunol. 2011;18:940–6.
Hileman CO, Carman TL, Longenecker CT, et al. Rate and predictors of carotid artery intima media thickness progression in antiretroviral-naive HIV-infected and uninfected adults: a 48-week matched prospective cohort study. Antivir Ther. 2013;18:921–9.
Theocharis AD, Tsolakis I, Tzanakakis GN, Karamanos NK. Chondroitin Sulfate as a key molecule in the development of atherosclerosis and cancer progression. Adv Pharm. 2006;53:281–95.
Zinellu E, Lepedda AJ, Cigliano A, et al. Association between human plasma chondroitin sulfate Isomers and carotid atherosclerotic plaques. Biochem Res Int. 2012;2012:1–6.
Sinha A, Ma Y, Scherzer R, Hur S, Li D, Ganz P, Deeks SG, Hsue PY. Role of T-cell dysfunction, inflammation, and coagulation in microvascular disease in HIV. J Am Heart Assoc. 2016;5(12):e004243.
Brunt SJ, Cysique LA, Lee S, Burrows S, Brew BJ, Price P. Short communication: do cytomegalovirus antibody levels associate with age-related syndromes in HIV patients stable on antiretroviral therapy? AIDS Res Hum Retrovir. 2016;32:567–72.
Affandi JS, Lee S, Chih HJ, et al. Cytomegalovirus burden improves a predictive model identifying measures of vascular risk in renal transplant recipients and healthy adults. J Med Virol. 2020. https://doi.org/10.1002/jmv.25697.
Griffiths PD, Stanton A, McCarrell E, et al. Cytomegalovirus glycoprotein-B vaccine with MF59 adjuvant in transplant recipients: a phase 2 randomised placebo-controlled trial. Lancet. 2011;377:1256–63.
Connell BJ, Lortat-Jacob H. Human immunodeficiency virus and heparan sulfate: from attachment to entry inhibition. Front Immunol. 2013;4:385.
Price P, Allcock RJ, Coombe DR, Shellam GR, McCluskey J. MHC proteins and heparan sulphate proteoglycans regulate murine cytomegalovirus infection. Immunol Cell Biol. 1995;73:308–15.
Acknowledgements
We thank the patients and controls who participated in this study, and Ms Faizah and staff of the HIV clinic who managed examination schedules. We thank Agung Karyawinara and Patrick Indradjaja who prepared the Esaote machine and healthy control schedules, and Larasinta Aulia Hartawan for collecting the data.
Funding
No funding was received for this project.
Author information
Authors and Affiliations
Contributions
IPW co-ordinated the project and facilitated the cardiovascular screening, BK and MSA carried out the cardiovascular screening, IA performed the laboratory analyses, AM performed the statistical analyses, EY, KH and IA provided intellectual and institutional support for the project, SL optimised the laboratory assays and PP designed the project and managed the preparation of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is specified in materials and methods.
Consent for publication
All authors have provided consent.
Competing interests
No authors have competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wijaya, I.P., Karim, B., Azizi, M.S. et al. Cytomegalovirus may influence vascular endothelial health in Indonesian HIV-infected patients after 5 years on ART. AIDS Res Ther 18, 83 (2021). https://doi.org/10.1186/s12981-021-00410-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-021-00410-7