Abstract
Background
Pediatric tuberculosis (TB), human immunodeficiency virus (HIV), and TB-HIV co-infection are health problems with evidence-based diagnostic and treatment algorithms that can reduce morbidity and mortality. Implementation and operational barriers affect adherence to guidelines in many resource-constrained settings, negatively affecting patient outcomes. This study aimed to assess performance in the pediatric HIV and TB care cascades in Mozambique.
Methods
A retrospective analysis of routine PEPFAR site-level HIV and TB data from 2012 to 2016 was performed. Patients 0–14 years of age were included. Descriptive statistics were used to report trends in TB and HIV indicators. Linear regression was done to assess associations of site-level variables with performance in the pediatric TB and HIV care cascades using 2016 data.
Results
Routine HIV testing and cotrimoxazole initiation for co-infected children in the TB program were nearly optimal at 99% and 96% in 2016, respectively. Antiretroviral therapy (ART) initiation was lower at 87%, but steadily improved from 2012 to 2016. From the HIV program, TB screening at the last consultation rose steadily over the study period, reaching 82% in 2016. The percentage of newly enrolled children who received either TB treatment or isoniazid preventive treatment (IPT) also steadily improved in all provinces, but in 2016 was only at 42% nationally. Larger volume sites were significantly more likely to complete the pediatric HIV and TB care cascades in 2016 (p value range 0.05 to < 0.001).
Conclusions
Mozambique has made significant strides in improving the pediatric care cascades for children with TB and HIV, but there were missed opportunities for TB diagnosis and prevention, with IPT utilization being particularly problematic. Strengthened TB/HIV programming that continues to focus on pediatric ART scale-up while improving delivery of TB preventive therapy, either with IPT or newer rifapentine-based regimens for age-eligible children, is needed.
Similar content being viewed by others
Background
Recent epidemiologic studies estimate that 2.1 million children are living with human immunodeficiency virus (HIV) globally [1]. As of 2016, approximately 108,000 children were living with HIV (CLHIV) in Mozambique, with an estimated 75,953, or 70%, on antiretroviral treatment (ART) [2]. The World Health Organization (WHO) estimated pediatric tuberculosis (TB) incidence in 2016 was 1.0 million cases globally, with 22,000 new pediatric cases in Mozambique [3]. In 2017, the Mozambique Ministry of Health (MoH) registered 11,198 pediatric TB cases (children 0–14 years of age), which represents a 51% case detection rate based on WHO epidemiologic estimates of overall childhood TB burden. Additionally, the MoH reported a 40% HIV-infection rate among registered adult and pediatric TB patients [4].
From these data, it is evident children in Mozambique account for a significant proportion of the global pediatric HIV and TB burden, and there are sizable gaps between the reported numbers of children receiving care and the estimates of those in need. Given the high rates of HIV-TB co-infection, well-integrated care programs for these diseases are critical to ensure that new cases are detected and that children receive the full package of available preventive and therapeutic evidence-based interventions [5,6,7]. This begins with routine screening, and both WHO and Mozambique national guidelines recommend active case-finding through provider-initiated testing and counseling (PITC) and/or routine opt-out testing for HIV in all children with TB, as well as routine symptom-based screening for TB during all pediatric HIV consultations [8,9,10,11,12].
For pediatric TB patients newly diagnosed with HIV, the evidence-based cascade of care includes starting cotrimoxazole preventive therapy (CPT) and timely initiation of ART (usually after two weeks of TB treatment) with regimens compatible with rifampicin-based TB therapy. These time-sensitive interventions are part of both WHO and national guidelines [10, 11, 13].
For children living with HIV, once active TB has been ruled out through routine screening, the risk of developing future disease can be reduced with TB preventive therapy (TPT). Accordingly, WHO and Mozambique national guidelines recommend isoniazid (INH) preventive therapy (IPT) in CLHIV over 12 months of age without active TB and newly enrolled in ART independent of contact history, and more targeted use in infants under 12 months of age without active TB but with a known contact [9, 12].
In Mozambique and other high-burden settings, well-integrated clinical management of children with HIV/TB co-infection following these guidelines continues to be problematic. Studies of HIV and TB co-infected children found high loss-to-follow-up rates among patients in both the HIV and TB care settings [14, 15]. There is also evidence demonstrating lower quality of HIV care (including proper TB screening, treatment, and prevention) is associated with lower retention and higher mortality [16]. TPT scale-up and treatment completion continues to be a challenge in most countries with a significant pediatric HIV epidemic [17]. And successful linkage of patients between the TB and HIV sectors faces persistent operational barriers [18,19,20].
As such, the overall aim of this study was to evaluate Mozambique pediatric TB-HIV national program results, identify strengths and weaknesses concerning adherence to national TB and HIV guidelines, and propose approaches that could be implemented to improve national program performance and pediatric outcomes.
Methods
Setting and data source
The President’s Plan for Emergency AIDS Relief (PEPFAR) supports the Mozambique MoH’s HIV and TB programs. The Centers for Disease Control and Prevention (CDC) and the United States Agency for International Development (USAID) provide PEPFAR funding to clinical partners who report routine data from both the HIV and TB programs. The frequency and breadth of data collected by the PEPFAR partners are greater than that collected routinely by the MoH, which often does not include age disaggregations. This study used PEPFAR aggregate data that were collected from both electronic patient tracking systems (ePTS) and paper-based patient registries at health care facilities.
Design
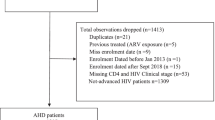
A retrospective analysis of site-level, aggregate patient TB/HIV indicators for patients 0–14 years of age was conducted with data from 2012 to 2016. Due to differences in clinical partner data collection approaches during the time period of the study which affected full reporting of indicators of interest, only data from CDC-supported sites using ePTS and USAID-supported sites using paper-based registries were included. Health centers in the TB sector without at least one child co-infected with HIV were excluded, and from the HIV sector, sites without at least one child on ART were excluded.
Analysis
The TB sector indicators included in the analysis were percentage of children tested for HIV, percentage of co-infected children who initiated CPT, and percentage of co-infected children who initiated ART. Indicators from the HIV sector included the percentage of children who were screened for TB at their last clinical consultation, the number of children treated for TB, and the percentage of new enrollees who received IPT or TB treatment. Trends in these indicators over the study period were reported as frequencies. A more detailed analysis of the most recent 2016 data was done to evaluate the performance of sector-specific care cascades relative to site-level independent/explanatory variables. These variables include province, district type (rural vs. urban according to standard MoH definitions), pediatric ART patient volume (converted into a categorical variable based on quartiles), and whether a site was a new or established pediatric ART site (established sites had at least one pediatric ART patient enrolled as of 2014, new sites enrolled their first pediatric ART patient in 2015 or 2016). The distribution of patients and sites according to these independent variables was analyzed with descriptive statistics including aggregate numbers of patients and sites with associated frequencies and a range for the lowest and highest site-level results.
The percentage of co-infected children with TB who initiated ART, and the percentage of newly enrolled CLHIV who received either TB treatment or IPT were chosen as the primary dependent outcomes of the TB and HIV care cascades, respectively, for tests of association with the site-level independent variables of interest. Data on initiation of IPT and TB treatment were analyzed; however, data about completion of treatment was not available. Generalized linear models with the logit link function and the binomial family were used to estimate the impact of each independent variable since both of our primary outcomes were bounded (0–100%). Separate models were constructed for each of the independent variables (unadjusted models) and adjusted models with all independent variables in the same model, with regression coefficients with 95% confidence intervals and p values reported. All models were adjusted for clustering within provinces to obtain robust standard errors using the vce(cluster) option in Stata. All analyses were performed in Stata version 14.0.a.
Ethical considerations
Use of routine, anonymized data for this study was approved by the Mozambican Ethics Committee and the Center for Global Health Science Office at the Centers for Disease Control and Prevention. Informed consent was not required.
Results
A total of 312 TB sites reporting 2350 co-infected children, and 718 HIV sites reporting 22,898 children newly enrolled in care (patients who commenced ART care for the first time), were included in the study. The majority of patients in both the TB and HIV cascade analysis were from rural (54.9% and 68.6%, respectively), high volume (83.4% and 68.3%, respectively), and established sites (92.3% and 86.9%, respectively). The distribution of patients and sites is presented in Table 1.
TB program trends
Our descriptive analysis at a national level indicates that 99% of TB patients (all ages, pediatric disaggregation not available from the study time period) were tested for HIV in 2016, up from 90% in 2012. CPT for co-infected children improved from 92% in 2014, 95% in 2015, and 96% in 2016. Initiation of ART for newly identified HIV co-infected children also showed steady improvement, from 81% in 2014, 86% in 2015, and 87% in 2016.
HIV program trends
Nationally, the percentage of HIV-infected children enrolled in care (includes newly enrolled and those already in care) and screened for TB at their last clinical consultation rose steadily from 2012 to 2016 (38% to 82%). The percentage of children diagnosed and treated for TB during the same time period did not rise correspondingly (2.6% to 1.3%), (Fig. 1). The number of newly enrolled HIV-infected children who received either IPT or TB treatment also trended positively in all provinces over the same time period, but remained well below target for 2016 at 42% nationally (37.7% received IPT and 4.3% received TB treatment) (Fig. 2).
TB program sub-analysis
Using the percentage of co-infected children on ART as the end-point indicator for the TB sector care cascade, performance by province, care setting of urban and rural, patient volume, and site experience were analyzed. The results are detailed in Table 2. In unadjusted regression analysis, urban sites (p = 0.001) and those in the higher volume quartiles (p value range 0.043– < 0.001)) were significantly more likely to have co-infected children on ART, while in the adjusted analysis, only higher volume sites retained significance (p value range 0.015– < 0.001), with urban sites having near significant results (p = 0.05), (Table 3).
HIV program sub-analysis
Performance of percentage of newly enrolled HIV-infected children who received either IPT or TB treatment by province, setting, volume, and site experience are detailed in Table 4. In unadjusted regression analysis, volume quartile 2 was the only site-level variable significantly associated with IPT or TB treatment in newly enrolled children (p = 0.001), while in the adjusted analysis, sites in volume quartiles 1 and 3 had significant results (p = < 0.001 and 0.043, respectively) (Table 5).
Discussion
TB program
This review of Mozambique national program data revealed that performance in the HIV care cascade from the TB program is strong, with positive trends and near-optimal performance in HIV testing (99.4%) and CPT initiation (95.7%) for co-infected children in 2016. ART initiation for co-infected children was lower (87.2%), but also improved from 2014 results of 81.0%. This indicator is limited in that co-infected children need to complete at least two weeks of TB treatment before initiating ART, so ART initiations in children enrolled near the end of a reporting period will be missed. That said, a result of 87.2% of pediatric TB patients newly identified as HIV + who started ART represents strong program performance and compares favorably with a 2015 global adult and pediatric rate of 78%, particularly since ART coverage rates for adults tend to be higher than for children [3].
In regression analysis controlled for provincial clustering, higher volume sites were significantly more likely to initiate co-infected children on ART. This is encouraging in that larger sites care for more of the overall number of affected children nationally, but, based on the results of this study, it is recommended that the MoH and supporting partners develop strategies to increase training and support to smaller sites to improve treatment outcomes.
HIV program
Results from the HIV program are less encouraging and provide evidence of missed opportunities to reduce TB-related morbidity and mortality in HIV-infected children. Intensified case-finding, as measured by documented TB screen at the last HIV consultation, was 82.2% in 2016. This indicator is measured by a simple yes/no tick box on the standardized national pediatric ART patient record/mastercard (a clinical and monitoring tool for patients on ART) and it is impossible to assess whether these represent thorough TB screens.
One way to assess the quality and efficacy of TB screening is to monitor if the increased frequency of screening leads to increased diagnosis and treatment. In this review, the percentage of CLHIV in care who were diagnosed and treated for TB decreased from 2.6% in 2012 to 1.3% in 2016. It is possible that during the time of the study improved TB control activities, expansion of pediatric ART and IPT, and improved adult HIV and TB care could have resulted in decreased TB disease in CLHIV. As such, it is not possible to conclude that the reported TB screening in HIV-infected children was not high quality, but the findings do raise that possibility.
Another way to assess the quality of TB screening in this population is to consider the proportion of CLHIV newly enrolled on ART that was started on either IPT or TB treatment. The MoH does not have a formal goal for this indicator, but a reasonable benchmark would be 60% (55% IPT, 5% TB treatment) based on current trends in new enrollees and IPT age-based eligibility criteria. In this review, only 42.0% of newly enrolled children received either treatment in 2016, representing an over three-fold increase from 2012 results of 11.7%, and a positive trend despite the overall poor result. The major shortfall was with IPT, with only 37.7% of newly enrolled CLHIV receiving this preventive treatment.
Healthcare worker training that addresses known common misperceptions about the risk of INH toxicity, developing INH resistance while on IPT, and IPT efficacy and durability is recommended [21,22,23,24,25,26,27,28]. This training should also include content on how to address patients concerns about pill burden, adherence, and stigma and improving overall IPT treatment literacy [22, 29,30,31]. And Mozambique should consider fully aligning its TB screening algorithm with WHO recommendations that just use poor weight gain or loss, current cough, and fever to determine IPT eligibility [12].
Since the time period of this study, evidence has emerged that a three-month, once-weekly regimen of isoniazid and rifapentine (3HP) and a one-month regimen of daily isoniazid and rifapentine (1HP) have preventive efficacy similar to that of six months of isoniazid monotherapy while having superior outcomes in terms of adverse events and treatment completion [32, 33]. WHO has included 3HP and 1HP as alternative regimens for the treatment of latent TB in patients ≥ 2 years of age in recent guidelines (there is insufficient data to recommend rifapentine in children < 2 years at this time), and their adoption in Mozambique could undoubtedly help address some of the patient and healthcare worker barriers to IPT. However, the introduction of 3HP and 1HP will not resolve persistent challenges related to ruling out active TB in children, medical training gaps, and TB/HIV program integration.
Limitations and strengths
This study has several limitations. The foremost is that the study used routine programmatic data that are intrinsically prone to error. However, PEPFAR performs routine data quality assessments and requires logic checks before partners can finalize and submit results. Despite the inclusion of pediatric HIV and TB indicators that are not available in the standard MoH reporting system, there were a limited number of site-level independent variables available for use in the regression analysis. Finally, there is an inherent bias towards larger established sites, as CDC clinical partners prioritized these health facilities for ePTS deployment. Larger sites did have better results in the TB care cascade and there may be an overestimation of aggregate national performance as a result. However, the sites included in the study accounted for the large majority of the children in care nationally, and thus the findings and recommendations should be more widely applicable.
Conclusions
Pediatric TB, HIV, and TB-HIV co-infection are health problems with evidence-based diagnosis and treatment guidelines and well-defined cascades of care that should be followed in order to improve health outcomes among this already vulnerable population. The challenges facing children with these diseases in developing countries are less biomedical, in terms of defining what care should be delivered, but rather more operational, in terms of how to implement these recommendations in resource-constrained and overburdened healthcare systems.
This study demonstrates that Mozambique has made significant strides in improving the pediatric care cascades for children with TB and HIV. HIV case finding along with initiation of CPT and ART for co-infected children is systematically strong and trending positively. Results from the HIV sector, however, show significant missed opportunities for TB diagnosis and prevention, with IPT utilization being particularly problematic. While the site-level analysis did not reveal significant predictors of improved performance aside from higher patient volume, further province and district-level sub-analysis could help identify implementation best practices that could be adopted elsewhere.
Integrated TB/HIV programming that continues to focus on pediatric ART scale-up, while strengthening TPT can reduce morbidity and mortality in HIV-infected Mozambican children and opportunities for improved collaboration have been identified.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Antiretroviral therapy
- CDC:
-
Centers for Disease Control and Prevention
- CLHIV:
-
Children living with HIV
- CPT:
-
Cotrimoxazole preventive therapy
- ePTS:
-
Electronic patient tracking system
- HIV:
-
Human immune deficiency virus
- IPT:
-
Isoniazid preventive therapy
- MoH:
-
Mozambique Ministry of Health
- PEPFAR:
-
President’s Emergency Plan for AIDS Relief
- TB:
-
Tuberculosis
- TPT:
-
Tuberculosis preventive therapy
- TST:
-
Tuberculin skin test
- USAID:
-
United States Agency for International Development
- WHO:
-
World Health Organization
References
Data AIDS. Geneva: UNAIDS; 2016.
Relatório Anual 2016; Relatório Anual das Actividades Relacionadas ao HIV/SIDA. Maputo, Mozambique: Ministério da Saúde, Moçambique; 2016.
Global Tuberculosis Report. Geneva. Switzerland: World Health Organization; 2017.
Relatorio de Actividades Desenvolvidas durante o Ano de 2017 (TB). Maputo, Mozambique: Ministério da Saúde, Moçambique; 2017.
Swaminathan S. Tuberculosis in HIV-infected children. Paediatr Respir Rev. 2004;5(3):225–30.
Marais BJ, Schaaf HS. Childhood tuberculosis: an emerging and previously neglected problem. Infect Dis Clin North Am. 2010;24(3):727–49.
Feja K, Saiman L. Tuberculosis in children. Clin Chest Med. 2005;26(2):295–312.
de Tuberculose M, Moçambique I. Maputo. Mozambique: Ministério da Saúde, Moçambique; 2013.
Guia de Tratamento Antiretroviral e Infecções Oportunistas no Adulto, Adolescente, Grávida e Criança. Maputo, Mozambique: Ministério da Saúde, Moçambique; 2014.
Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. Geneva: World Health Organization; 2013.
Guidance for national tuberculosis programmes on the management of tuberculosis in children. Geneva: World Health Organization; 2014.
Latent tuberculosis infection. updated and consolidated guidelines for programmatic management. Geneva: World Health Organization; 2018.
Crook AM, Turkova A, Musiime V, Bwakura-Dangarembizi M, Bakeera-Kitaka S, Nahirya-Ntege P, et al. Tuberculosis incidence is high in HIV-infected African children but is reduced by co-trimoxazole and time on antiretroviral therapy. BMC Med. 2016;14:50.
Enane LA, Lowenthal ED, Arscott-Mills T, Matlhare M, Smallcomb LS, Kgwaadira B, et al. Loss to follow-up among adolescents with tuberculosis in Gaborone, Botswana. Int J Tuber Lung Dis. 2016;20(10):1320–5.
Buck WC, Olson D, Kabue MM, Ahmed S, Nchama LK, Munthali A, et al. Risk factors for mortality in Malawian children with human immunodeficiency virus and tuberculosis co-infection. Int J Tuber Lung Dis. 2013;17(11):1389–95.
Ojikutu B, Higgins-Biddle M, Greeson D, Phelps BR, Amzel A, Okechukwu E, et al. The association between quality of HIV care, loss to follow-up and mortality in pediatric and adolescent patients receiving antiretroviral therapy in Nigeria. PLoS ONE. 2014;9(7):e100039.
Davies MA, Gibb D, Turkova A. Survival of HIV-1 vertically infected children. Curr Opin HIV AIDS. 2016;11(5):455–64.
Diese M, Shrestha L, Pradhan B, Singh D, Raaijmakers H, Kisesa A, et al. Bottlenecks and opportunities for delivering integrated pediatric HIV services in Nepal. Curr Opin HIV AIDS. 2016;11(Suppl 1):S21–9.
Ahmed S, Kim MH, Sugandhi N, Phelps BR, Sabelli R, Diallo MO, et al. Beyond early infant diagnosis: case finding strategies for identification of HIV-infected infants and children. AIDS (London, England). 2013;27(Suppl 2):S235–45.
Phelps BR, Ahmed S, Amzel A, Diallo MO, Jacobs T, Kellerman SE, et al. Linkage, initiation and retention of children in the antiretroviral therapy cascade: an overview. AIDS (London, England). 2013;27(Suppl 2):S207–13.
Date AA, Vitoria M, Granich R, Banda M, Fox MY, Gilks C. Implementation of co-trimoxazole prophylaxis and isoniazid preventive therapy for people living with HIV. Bull World Health Organ. 2010;88(4):253–9.
Lester R, Hamilton R, Charalambous S, Dwadwa T, Chandler C, Churchyard GJ, et al. Barriers to implementation of isoniazid preventive therapy in HIV clinics: a qualitative study. AIDS (London, England). 2010;24(Suppl 5):S45–8.
Akolo C, Bada F, Okpokoro E, Nwanne O, Iziduh S, Usoroh E, et al. Debunking the myths perpetuating low implementation of isoniazid preventive therapy amongst human immunodeficiency virus-infected persons. World J Virol. 2015;4(2):105–12.
Chehab JC, Vilakazi-Nhlapo K, Vranken P, Peters A, Klausner JD. Survey of isoniazid preventive therapy in South Africa, 2011. Int J Tuber Lung Dis. 2012;16(7):903–7.
Wood R, Bekker LG. Isoniazid preventive therapy for tuberculosis in South Africa: an assessment of the local evidence base. SAMJ South Afr Med J. 2014;104(3):174–7.
Pathmanathan I, Ahmedov S, Pevzner E, Anyalechi G, Modi S, Kirking H, et al. TB preventive therapy for people living with HIV: key considerations for scale-up in resource-limited settings. Int J Tuber Lung Dis. 2018;22(6):596–605.
Getahun H, Granich R, Sculier D, Gunneberg C, Blanc L, Nunn P, et al. Implementation of isoniazid preventive therapy for people living with HIV worldwide: barriers and solutions. AIDS (London, England). 2010;24(Suppl 5):S57-65.
Ait-Khaled N, Alarcon E, Bissell K, Boillot F, Caminero JA, Chiang CY, et al. Isoniazid preventive therapy for people living with HIV: public health challenges and implementation issues. Int J Tuber Lung Dis. 2009;13(8):927–35.
Costenaro P, Massavon W, Lundin R, Nabachwa SM, Fregonese F, Morelli E, et al. Implementation and Operational Research: Implementation of the WHO 2011 Recommendations for Isoniazid Preventive Therapy (IPT) in Children Living With HIV/AIDS: A Ugandan Experience. J Acq Immun Defic Syndr. 2016;71(1):e1-8.
Masini EO, Sitienei J, Weyeinga H. Outcomes of isoniazid prophylaxis among HIV-infected children attending routine HIV care in Kenya. Public health action. 2013;3(3):204–8.
Takarinda KC, Choto RC, Harries AD, Mutasa-Apollo T, Chakanyuka-Musanhu C. Routine implementation of isoniazid preventive therapy in HIV-infected patients in seven pilot sites in Zimbabwe. Public Health Action. 2017;7(1):55–60.
Hamada Y, Ford N, Schenkel K, Getahun H. Three-month weekly rifapentine plus isoniazid for tuberculosis preventive treatment: a systematic review. Int J Tuberc Lung Dis. 2018;22(12):1422–8.
Swindells S, Ramchandani R, Gupta A, Benson CA, Leon-Cruz J, Mwelase N, et al. One month of Rifapentine plus isoniazid to prevent HIV-related tuberculosis. N Engl J Med. 2019;380(11):1001–11.
Acknowledgements
This research has been supported by the President's Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC) and the United States Agency for International Development. The PEPFAR data set used for this project represents the combined work of a considerable number of people including the clinical workforce of the Mozambique MoH, various PEPFAR-funded clinical partners, and CDC and USAID technical and strategic information staff. Dr. Greg Thomas-Reilly and Ms. Claire Duddy from the London School of Hygiene and Tropical Medicine made valuable contributions to the study design, and literature review, respectively.
Disclaimer
The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC), the United States Agency for International Development (USAID), or the Mozambique Ministry of Health.
Funding
There was no specific funding for this study.
Author information
Authors and Affiliations
Contributions
WCB conceived the study and had primary responsibility for manuscript drafting and study coordination. HN and MS had primary responsibility for data analysis and contributed to manuscript drafting and revision. FF and CX assisted with data analysis and contributed to manuscript revision. LB, JC, MID, MG, and PK provided input into study design and contributed to manuscript revision. BJ, CM, and BS contributed to manuscript revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Use of routine, anonymized data for this study was approved by the Mozambican Ethics Committee and the Center for Global Health Science Office at the Centers for Disease Control and Prevention. Informed consent was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Buck, W.C., Nguyen, H., Siapka, M. et al. Integrated TB and HIV care for Mozambican children: temporal trends, site-level determinants of performance, and recommendations for improved TB preventive treatment. AIDS Res Ther 18, 3 (2021). https://doi.org/10.1186/s12981-020-00325-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-020-00325-9