Abstract
Background
CD4 cells are a type of white blood cells that plays a significant role in protecting humans from infectious diseases. Lack of information on associated factors on CD4 cell count reduction is an obstacle for improvement of cells in HIV positive adults. Therefore, the main objective of this study was to investigate baseline factors that could affect initial CD4 cell count change after highly active antiretroviral therapy had been given to adult patients in North West Ethiopia.
Methods
A retrospective cross-sectional study was conducted among 792 HIV positive adult patients who already started antiretroviral therapy for 1 month of therapy. A Chi square test of association was used to assess of predictor covariates on the variable of interest. Data was secondary source and modeled using generalized linear models, especially Quasi-Poisson regression.
Results
The patients’ CD4 cell count changed within a month ranged from 0 to 109 cells/mm3 with a mean of 15.9 cells/mm3 and standard deviation 18.44 cells/mm3. The first month CD4 cell count change was significantly affected by poor adherence to highly active antiretroviral therapy (aRR = 0.506, P value = 2e−16), fair adherence (aRR = 0.592, P value = 0.0120), initial CD4 cell count (aRR = 1.0212, P value = 1.54e−15), low household income (aRR = 0.63, P value = 0.671e−14), middle income (aRR = 0.74, P value = 0.629e−12), patients without cell phone (aRR = 0.67, P value = 0.615e−16), WHO stage 2 (aRR = 0.91, P value = 0.0078), WHO stage 3 (aRR = 0.91, P value = 0.0058), WHO stage 4 (0876, P value = 0.0214), age (aRR = 0.987, P value = 0.000) and weight (aRR = 1.0216, P value = 3.98e−14).
Conclusions
Adherence to antiretroviral therapy, initial CD4 cell count, household income, WHO stages, age, weight and owner of cell phone played a major role for the variation of CD4 cell count in our data. Hence, we recommend a close follow-up of patients to adhere the prescribed medication for achievements of CD4 cell count change progression.
Similar content being viewed by others
Background
Globally, about 330,000 children were infected with HIV in 2011, and 90% of these infections occurred in Sub-Saharan Africa mainly through mother to child transmission [1]. About 38.1 million people were infected by HIV virus in the world at the end of 2014 and about 25.3 million people died with AIDs related illness [2]. In 2014, about 39.9 million people were living with HIV and the global prevalence rate was 0.8% [3]. In 2009 alone, an estimated 1.3 million adults and children died because of HIV/AIDs in Sub-Saharan African [4]. Most of the people living with HIV/AIDS in Africa are between age 15 and 49, which is the prime age of working [5]. Furthermore, the International Labor Organization (ILO) indicated that in 2005 an estimated number of 2 million workers were unable to work in Africa due to HIV/AIDs illness; and this figure was doubled in 2015 [6]. During the period, around 25.8 million people were living with HIV virus in Sub-Saharan Africa, accounting for 67.7% of the global total [6]. The impact of HIV/AIDs in Africa, on the workforce, increases expenditure on the one hand and decreases productivity on the other [6]. In Ethiopia, about 730,000 people were living with HIV and among these 23,000 died due to AIDs. An estimated prevalence among pregnant women was 1.2%, and one of every 3 children born to these women got infected with HIV [7]. In Amhara Region, all HIV prevalence was estimated to be 1.6% [8] and the prevalence among women attending prenatal clinics from 1999 to 2000 was more than 18% [9]. Therefore, the Amhara region is among the regions that require special attention to HIV- related problems such as recovery of CD4 cell count to highly active antiretroviral therapy (HAART) [10].
Although the current HIV/AIDs surveillance estimates indicate some encouraging signs that the epidemic is stabilizing, the observed changes are not sufficient enough to be compared to the desired goals of response against the epidemic [11]. Availability of information about factors that affect CD4 cell count in the study area at initial stage of treatment is important for HIV patients to have long life period [12]. Information on the rate of initial HAART regimen change and its predictor in Ethiopia is scarce [13, 14]. There is a limited data regarding factors that predict initial CD4 cell count change to HAART medication in the study area [14]. In particular, there are no studies that examine how patient-related factors relate to each other (interact) and their subsequent influence on initial CD4 cell count change [15]. The purpose of this study is thus to identify whether or not specific clinical and socio-demographic factors present at the baseline influence first month CD4 cell count change among HIV positive adults in Amhara region (North west Ethiopia) [16]. Therefore, the present study emphasizes the role of covariates (predictors) that are thought to affect the parameters of the conditional distribution of events, given the covariates. The knowledge and understanding of such factors is important given the increasing number of patients enrolled in HAART [16]. This improvement helps to reduce dropout patients from the treatment. The results of this research can further be used to shape communication and counseling prior to treatment initiation.
Methods
Study materials and setting
The data for this study consisted of secondary data, records of social, demographic and clinical characteristics of 792 adult HIV patients recorded after 1 month of therapy by HIV care providers. A Chi square test of association was used to assess predictors of the response variable. The study was cross-sectional, targeted for 6036 HIV/AIDS patients who visited Felege-Hiwot Referral and Teaching Hospital and Health Research center in Bahir Dar, Ethiopia, under the follow-up of ART from September 2005 to August 2012.
Inclusion criteria
Adult patients, whose ages were 15+ years, with a CD4 cell count below 200 cells/mm3 or patients with World Health Organization (WHO) stage IV of HIV disease regardless of CD4 cell count, enrolled at Felege-Hiwot Referral and Teaching Hospital were included under this study.
Sample size and sampling technique
Out of the targeted HIV/AIDS patients, 792 were selected using stratified random sampling technique considering their residence area as strata using 95% level of confidence and 5% marginal error.
Data collection tools and procedures
The available information was first observed and discussed with health care service providers at ART section from the hospital. Data was extracted using data extraction format developed by the investigators in consultation with health service providers. All relevant information was collected by health care service providers after theoretical and practical orientations. Charts of patients were retrieved using the patients’ registration card number which was found in the electronic database system.
Data quality
The quality of the data was controlled by data controllers from the ART section as well as the regional health research center who had intensive ART training from the Ministry of Health for these and other purposes. Data collectors got introductions about definitions of variables in the questionnaires. The data extraction tools and variables included in the analysis were pre-tested for consistency of understanding, review of tools and completeness of data items on 45 random charts. Based on the pilot data result, the necessary amendments were made on the final data extraction format. The retrieval process was closely monitored by the principal investigator throughout the data collection period. Both predictor and response variables were checked regularly for completeness of information. Any problem traced was immediately communicated to data collectors for giving corrections.
Variable of interest
The variable of interest for this study was CD4 cell count change per mm3. The response variable was count data.
Independent variable
The potential predictor variables for this study were age in years, weight in kg, baseline CD4 cell count, gender (male, female), educational status (no education, primary, secondary and tertiary), disease disclosure (disclosed their disease to family members, closed the disease to family members), residential area (rural, urban), WHO stages (stage 1, stage 2, stage 3 and stage 4), adherence to HAART (poor, fair and good), level of income (low, middle and high), marital status (living with partner, living without partner), and owner of cell phone (with cell phone, without cell phone).
The standard model for count data is Poisson distribution. It is, therefore, useful at the outset to review some fundamental properties and characterize results of the Poisson distribution. If the discrete random variable Y has Poisson distribution with intensity or rate parameter μ, μ > 0 and t is the exposure defined as the length of time which the event recorded, then Y has the density [17]
where \(E\left( y \right)\, = \,var\left( y \right)\, = \,\mu t\). If the time period equals to unity, then its density given in (1) equals
Equality of mean and variance of Poisson distribution is referred to as the equi-dispersion property of Poisson which is mostly violated in real life data [18].
In generalized linear models, the method of maximum likelihood estimation is usually used to estimate the parameters in the given model [19]. To define likelihood, we have to specify the form of distribution of observation; while to define quasi-likelihood function, we need to specify only the mean–variance relationship and then apply quasi-likelihood for parameter estimation [20]. The important motivation of Poisson distribution from estimation point of view depends on mean–variance relation [20]. In over-dispersed Poisson model, an extra parameter is included which estimates how much larger the variance is than the mean [21]. This parameter estimate is then, used to correct the effects of the larger variance on the P values [22]. In the over-dispersed distribution, one alternative approach to fit extra dispersion parameter which accounts for that extra variance is a Quasi-Poisson model. It has two parameters, namely mean, μ and over-dispersion parameter θ such that variance is a linear function of mean [23]. Hence for random variable y that follows Quasi-Poisson distribution, we have
for \(\emptyset \, > \,1\), we have over-dispersion relative to Poisson. Applying iteratively re-weighted least squares in the more general case involves working with weights say \(W^{*} \, = \,\frac{\mu }{ \emptyset }\). This implies that when variance is proportional to mean (not necessarily equal to mean), Poisson estimator is maximum Quasi-Poisson likelihood estimator and the model is said to Quasi-Poisson regression model [21]. The quasi-likelihood function \({\text{K}}(y_{i} ,\,\mu_{i} )\) for each independent observation, \(y_{i}\) is defined as
where V is some known function and suppose the expectation, \(\mu_{i}\) is some function of parameters β i . Another alternative for modeling over-dispersion is a negative binomial regression model [24] with two parameters and having a form of the Poisson distribution in which the distribution’s parameter itself is considered as random variable. The first two moments of negative binomial regression model are [24].
If θ = 0, there will be no unobserved heterogeneity which results in Poisson variance (Poison model is a special case of negative binomial when θ = 0); and if θ > 0, variance will be greater than mean and becomes over-dispersed [17]. Using weighted least squares; these models have a little difference with weight-mean relation as shown below [20]:
provided all other elements are zero. The mean-weight relation that exists in model Eq. (6) provides us with full comparison between Quasi-Poisson and negative binomial models where Quasi-Poisson weights are directly proportional to the mean and have concave relation to the mean of negative binomial [20].
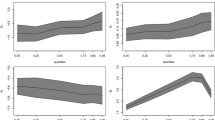
Therefore, the two models, Quasi-Poisson and negative binomial regression models; are to be considered as potential candidates for fitting over-dispersed data. Different scholars such as Ver Hoef [20], Gardner [23], Power [25] and Potts [26] gave different decisions and comments at different times about the models appropriate to over-dispersed data. Therefore, we compared the two models using the following two approaches; comparing the values of log-likelihood, AIC and BIC to assess goodness-of-fit based on our data for the two models as shown in Table 2 [27]; and using mean–variance and mean-weight relation and finding the cut-off- point (boundary value) where the two curves cross each other as shown in Eqs. (3), (5), (6) and (refer Fig. 1). To do this, one can equate the two mean–variance relation equations of the two models (3) and (5) after predicting over-dispersed parameters for the two models separately. Then, one can find the mean value that makes the two graphs cross each other. We consider this value as cut-off point or boundary value. If the mean of response variable (CD4 cell count for our case) is less than the cut-off point, we have to consider negative binomial; while if the mean of the variable of interest is greater than the cut-off point, we need to consider a Quasi-Poisson model [20] (refer to Fig. 1).
Data analysis
The variables under study were summarized using descriptive statistics such as median for continuous variable and proportions for categorical variables. The data was also analyzed using generalized linear models using Quasi-Poisson regression model. The mean–variance relation, information criteria and the value of Chi square divided by its degree of freedom were used to select the model that fits the data appropriately. Change of deviance was used to measure the extent to which the fit of the model was improved when extra variables were added to the model. The main effects and combination of two ways interaction were fitted, provided that attention was given to hierarchical principle of model fitting. The mean–variance relations for negative binomial and Quasi-Poisson were solved simultaneously to get the value (cut-off points) where the two curves meet each other. The mean of response variable and cut-off points were compared to each other for the two models to select the one which had smaller variation for response variable. The model selected for analysis was the one with smallest information criteria and smallest dispersion parameter and its goodness-of-fit was assessed using Hosmer–Lemeshow goodness-of-fit statistic [28]. Influential observations were identified using cook’s distance against observations [29]. Finally, the linear predictor and its square on the response variable were important for checking appropriateness of link function for the selected model [28]. Data analysis was conducted using SPSS version 21 and R version 3.2.3.
Results
In Table 1, out of the sample of 792 patients, 40.9% were from rural areas while 59.1% were residing in urban areas; 50.6% were female and 49.4% were male and 44.8% were living with their partners and 55.2% were living without partners. About 47.3% of them disclosed their disease to family members and the rest did not. Of these patients, 46.1% owned cell phone. Lastly 25.5, 44.3 and 30.2% of the patients had good, fair and poor adherence, respectively.
After 1 month of treatment, the change in CD4 cell count ranged from 0 to 109 cells/mm3 with mean 15.9, standard deviation 18. 44 and median 7 cell/mm3 (see Fig. 2). Figure 2 also shows that 17.55% of the patients had 4 CD4 cells/mm3 and only 0.63% had 109 CD4 cells/mm3, and the distribution indicated that variance is about 21 times the mean and this is an indicator of over-dispersed distribution. Using Pearson’s Chi square statistic, deviance divided by degree of freedom, the over-dispersion parameter for Quasi Poisson was \(\hat{\emptyset }\, = \,1.49\), which showed that the variance is 49% larger than mean [20]. Using these estimated values, Eqs. (3) and (5) for our data, mean value (cut-off point) which made over-dispersion for Quasi-Poisson [17] and negative-binomial [24] equal to each other was μ = 10.5 cells/mm3 which is less than the mean of CD4 cell count change (15.9 cells/mm3) for our analysis. Therefore, based on the selection criterion, the Quasi-Poisson was selected to fit our data [20]. The two models were also compared using information criteria such as Akakai and Bayesian information criterion [30], and the result is given in Table 2.
From Table 2, we observed that deviance was less than Pearson Chi square for both models, but AIC and BIC were smaller for Quasi-Poisson which indicated that Quasi-Poisson was preferable. Hence parameter estimation and identification of predictors of initial CD4 cell count should be conducted using the selected model (Quasi-Poisson model).
From Table 3, considering adherence as a predictor variable, compared to good adherence, log of the expected CD4 cell count change difference between poor adherent patients and good adherent patients was about −0.68 cells/mm3, and the difference between fair adherent and good adherent patients was −0.525 cells/mm3 per month. In other words, the CD4 cell count change for poor adherents was 0.51 times that of good adherent patients (aRR = 0.51, P value = 2e−16). And the rate of change of CD4 cell count for fair adherent patients was 0.59 times (aRR = 0.59, P value = 0.0120) that of good adherent patients keeping the other variables constant. For one year increase of the age of a patient, the log of expected CD4 cell count change decreased by 0.012 cells/mm3 (aRR = 0.986, P value = 2.38e−12).
The other predictor variable with significant effect for the variable of interest was found to be initial CD4 cell count (refer to Table 3). For 1 cell/mm3 increase of initial CD4 cell count, the log of expected change of CD4 cell count was increased by 0.003 (aRR = 1.02, P value = 1.54e−15), keeping the other variables constant. A patient with low household income experienced lower CD4 cell count change as compared to the household with high income (aRR = 0.63, P value = 6.71e−14). However, a patient with middle household income, CD4 cell count change was lower than that with high household income. The variable ownership of cell phone had significantly affected CD4 cell count change for 1 month of therapy. Hence, the expected change of CD4 cell count for a patient without cell phone decreased by 43% (aRR = 0.67, P value = 0.0226) as compared to otherwise identical patients with a cell phone. With regard to WHO stages, stages 2 and stage 3 patients’ CD4 changes were lower than that of stage 1 patients. Table 3 also shows significant interaction effects with main effects and the following were significant interaction effects in Table 3.
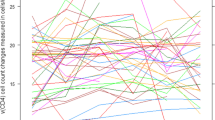
Interaction effects of owner of cell phone and age of patients
Naturally, as age of a patient increases, CD4 cell count decreases, but the decreasing rate of those patients with cell phone was less likely than that of patients without cell phone (aRR = 0.987, P value = 0.007) (refer to Table 3). Figure 3 indicates that the decreasing rate of patients with owner of cell phone is less likely as comapred to those patients without cell phone.
Interaction between adherence and marital status
The log of CD4 cell count change for patients with poor and fair adherence living without partners decreased by 2.316 and 2.415, respectively as compared to patients with good adherence living with their partners (aRR = 0.099, P value = 0.003 for poor adherence) and (aRR = 0.089, P value = 0.002 for fair adherent patients) (see Table 3). Figure 4 shows that the incident rate of CD4 cell count change for patients living with partners was by far better than those patients living without their partners.
Interaction effects of marital status and initial CD4 cell count
Another significant interaction effect on CD4 cell count change based on 1 month therapy was marital status with initial CD4 cell count. In this 1 month therapy, CD4 cell count change appreciated as initial CD4 count increased, but it was more accelerated for patients living with partners (refer to Fig. 5).
Discussions
In a month of therapy, CD4 cell count change was highly affected by age, weight, initial CD4 cell count, marital status, income, cell phone ownership, adherence, level of exposedness and WHO stages from the main effect and age with owner of cell phone, marital status with adherence and marital status with initial CD4 cell count from the interaction effect. In this study, as age of an individual increased, CD4 cell count decreased. This is also supported by previous joint longitudinal study [16]. In adherence category, poor adherent patients who did not properly take their medication on time, lose their CD4 cell count. On the other hand, patients with good adherent, who took pills on time regularly, increased their CD4 cell count. A patient living with his/her partner may be encouraged or reminded to take his/her medication on time and this contributes to increase CD4 cell count. A patient who does not expose the disease to family members may not have good adherence to HAART, since he/she takes pills only when nobody is around; and this leads to reduction of CD4 cell count. Naturally, aged people are less likely to have high CD4 cell count as compared to young people. But the decreasing rate of CD4 cell count as age increases was different for patients having cell phone and without having cell phone. Hence patients with cell phone had less decreasing rate as compared to those patients without cell phone.
The significant result of initial CD4 cell count on current CD4 cell count obtained under this study is consistent with a previous study [27]. Hence, a patient who started HAART with high initial CD4 cell count had high CD4 cell count change. On the other hand, an insignificant result of gender on CD4 cell count change in this study contradicted with previous research [27] and is supported by another research [14]. A significant result for marital status obtained in this study is supported by another previous study [11]. The significant result of WHO stages on CD4 cell count in this study is also supported by previous longitudinal study [11].
Limitations
One limitation of this study was that the interactions between variables were identified in model fit techniques which were not pre-specified or expected during data collection. Therefore, detail information on why these interactions affect on first month CD4 cell count change was not collected and therefore, the reason for some of these findings cannot be explained. Furthermore, this study focused on first month CD4 cell count change. There was no evidence whether or not the factors that affected the CD4 cell count change in first month therapy can also affect the change of CD4 cell count of longitudinal data for the same cohort. The study also tried to identify special characteristics of HIV positive adults and we should not generalize the result to the whole HIV positive people, since the investigation did not include HIV positive patients whose age were less than 15 years. Hence, the result may not be the same on this issue if we incorporate all HIV positive people whose ages are less than 15 years; and this needs further investigation. Therefore, for researchers who want to study this gap it can be considered as potential for further study.
Conclusions
Quasi-Poisson regression model was a better fit for the given data, and variables that significantly predict the response variable were identified using this model. The result under this investigation indicated that CD4 cell count change of HIV positive people had been affected by several factors. There should be a special attention and intervention for HIV positive adults, especially for those who had low CD4 cell count change, for pre-treatment counseling and awareness creation. The study also tried to identify a certain group of patients who were with maximum risk of CD4 cell count change and need high intervention for counseling and awareness creation. Hence, we recommend that the Ministry of Health (MOH) give due attention for awareness creation so that patients should expose the disease to family members and adhere to HAART directed by health care service providers on time using the alarm of their cell phone as remembrance.
Abbreviations
- AIC:
-
Akaike information criteria
- aRR:
-
adjusted rate ratio
- BIC:
-
Bayesian information criteria
- CI:
-
confidence interval
- CD4:
-
classification determinant four
- HAART:
-
highly active anti-retroviral therapy
- HIV:
-
human immune deficiency virus
- SPSS:
-
Statistical Package for Social Science
- WHO:
-
World Health Organization
- MLE:
-
maximum likelihood estimator
References
World Health Organization. Global update on HIV treatment 2013: results, impact and opportunities; 2013.
World Health Organization. Global health risks-mortality and burden of disease attributable to selected major risks. The Lancet. 2015.
Montaner JS, et al. Expansion of HAART coverage is associated with sustained decreases in HIV/AIDS morbidity, mortality and HIV transmission: the “HIV treatment as prevention” experience in a Canadian setting. Plos ONE. 2014;9(2):e87872.
Berhan Z, et al. Risk of HIV and associated factors among infants born to HIV positive women in Amhara region, Ethiopia: a facility based retrospective study. BMC Res Notes. 2014;7(1):1.
Feeley R, et al. The impact of HIV/AIDS on productivity and labor costs in two Ugandan corporations. Boston: Center for International Health and Development, Boston University; 2004.
Fortson JG. Mortality risk and human capital investment: the impact of HIV/AIDS in Sub-Saharan Africa. Rev Econ Stat. 2011;93(1):1–15.
Hladik W, et al. HIV/AIDS in Ethiopia: where is the epidemic heading? Sex Transm Infect. 2006;82(suppl 1):32–5.
Clark S, Bruce J, Dude A. Protecting young women from HIV/AIDS: the case against child and adolescent marriage. Int Fam Plan Perspect. 2006;32:79–88.
Erulkar A, Ferede A. Social exclusion and early or unwanted sexual initiation among poor urban females in Ethiopia. Int Perspect Sex Reprod Health. 2009;35:186–93.
Berhan Z, et al. Prevalence of HIV and associated factors among infants born to HIV positive women in Amhara Region, Ethiopia. Int J Clin Med. 2014;5(8):464.
Adams M, Luguterah A. Longitudinal analysis of change in CD4+ cell counts of HIV-1 patients on antiretroviral therapy (ART) in the Builsa district hospital. Eur Sci J. 2013;9(33):1.
Pennap G, Chaanda M, Ezirike L. A review of the impact of HIV/AIDS on education, the workforce and workplace: the African experience. Soc Sci. 2011;6(2):164–8.
Cameron AC, Trivedi PK. Regression analysis of count data. 3rd ed. Cambridge: Cambridge University Press; 2013.
Smith CJ, et al. Factors influencing increases in CD4 cell counts of HIV-positive persons receiving long-term highly active antiretroviral therapy. J Infect Dis. 2004;190(10):1860–8.
Rodriguez S, et al. Effective management of high-risk medicare populations; 2015.
Seid A, et al. Joint modeling of longitudinal CD4 cell counts and time-to-default from HAART treatment: a comparison of separate and joint models. Electron J Appl Stat Anal. 2014;7(2):292–314.
Lambert D. Zero-inflated Poisson regression, with an application to defects in manufacturing. Technometrics. 1992;34(1):1–14.
Ismail N, Jemain AA. Handling overdispersion with negative binomial and generalized Poisson regression models. In: Casualty Actuarial Society Forum; 2007. Citeseer.
McCullagh P, Nelder JA. Generalized linear models. 7th ed. Boca Raton: CRC Press; 1989.
Ver Hoef JM, Boveng PL. Quasi-Poisson vs. negative binomial regression: how should we model over dispersed count data? Ecology. 2007;88(11):2766–72.
Feria-Domínguez JM, Jiménez-Rodríguez E, Sholarin O. Tackling the over-dispersion of operational risk: implications on capital adequacy requirements. North Am J Econ Finance. 2015;31:206–21.
Cameron AC, Johansson P. Count data regression using series expansions: with applications. J Appl Econometr. 1997;12(3):203–23.
Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: poisson, over dispersed Poisson, and negative binomial models. Psychol Bull. 1995;118(3):392.
Lindén A, Mäntyniemi S. Using the negative binomial distribution to model overdispersion in ecological count data. Ecology. 2011;92(7):1414–21.
Power JH, Moser EB. Linear model analysis of net catch data using the negative binomial distribution. Can J Fish Aquat Sci. 1999;56(2):191–200.
Potts JM, Elith J. Comparing species abundance models. Ecol Model. 2006;199(2):153–63.
Asfaw A, et al. cd4 cell count trends after commencement of antiretroviral therapy among HIV-infected patients in Tigray, Northern Ethiopia: a retrospective cross-sectional study. Plos ONE. 2015;10(3):e0122583.
Hosmer DW, Lemeshow S. Applied logistic regression. Hoboken: Wiley; 1989. p. 8–20.
Collett D. Modelling binary data. Boca Raton: CRC Press; 2002.
Pongsapukdee V, Sukgumphaphan S. Goodness of fit of cumulative logit models for ordinal response categories and nominal explanatory variables with two-factor interaction. Silpakorn U Sci Tech J. 2007;1(2):29–38.
Authors’ contributions
The principal author wrote the proposal, developed data collection format, supervised the data collection process and analysed the data in consultation with the second and the third authors. The second and the third authors edited the document, gave critical comments for the betterment of the manuscript applying their rich experiences. All authors read and approved the final manuscript.
Acknowledgements
Amhara Region Health Research & Laboratory Center at Felege-Hiwot Referral Hospital, Ethiopia, is gratefully acknowledged for the data supplied for our health research.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
We confirm that the research is based on secondary data obtained at Felegehiwot-Hiwot Referal Hospital. We can avail the data up on request.
Consent for publication
This manuscript has not been published elsewhere and is not under consideration by another journal. All authors have approved the final manuscript and agreed with its submission to AIDS Research and Therapy. We also agreed the authorship and order of authors for this manuscript.
Ethical consideration
Ethical clearance certificate had been obtained from two universities namely Bahir Dar University, Ethiopia with Ref ≠ RCS/1412/2006 and University of South Africa (UNISA), South Africa, Ref ≠ :2015 – SSR – ERC_006. We can attach the ethical clearances certificate up on request. Hence all of the authors have appropriate permission for the data we used.
Funding
There is no agent that funds the manuscript to be published or “not applicable”.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Seyoum, A., Ndlovu, P. & Zewotir, T. Quasi-Poisson versus negative binomial regression models in identifying factors affecting initial CD4 cell count change due to antiretroviral therapy administered to HIV-positive adults in North–West Ethiopia (Amhara region). AIDS Res Ther 13, 36 (2016). https://doi.org/10.1186/s12981-016-0119-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-016-0119-6