Abstract
Background
Early antenatal care visit is important for optimal care and health outcomes for women and children. In the study area, there is a lack of information about the time to initiation of antenatal care. So, this study aimed to determine the time to initiation of antenatal care visits and its predictors among pregnant women who delivered in Arba Minch town public health facilities.
Methods
An institution-based retrospective follow-up study was performed among 432 women. A systematic random sampling technique was employed to select the study participants. The Kaplan-Meier survival curve was used to estimate the survival time. A Multivariable Cox proportional hazard regression model was fitted to identify predictors of the time to initiation of antenatal care. An adjusted hazard ratio with a 95% confidence interval was used to assess statistical significance.
Results
The median survival time to antenatal care initiation was 18 weeks (95% CI = (17, 19)). Urban residence (AHR = 2.67; 95% CI = 1.52, 4.71), Tertiary and above level of education of the women (AHR = 1.90; 95% CI = 1.28, 2.81), having pregnancy-related complications in a previous pregnancy (AHR = 1.53; 95% CI = 1.08, 2.16), not having antenatal care for previous pregnancy (AHR = 0.39; 95% CI = 0.21, 0.71) and unplanned pregnancy (AHR = 0.66; 95% CI = 0.48, 0.91) were statistically significant predictors.
Conclusion
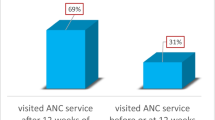
Half of the women initiate their antenatal care visit after 18 weeks of their pregnancy which is not in line with the recommendation of the World Health Organization. Urban residence, tertiary and above level of education of the women, having pregnancy-related complications in a previous pregnancy, not having previous antenatal care visits and unplanned pregnancy were predictors of the time to initiation of antenatal care. Therefore, targeted community outreach programs including educational campaigns regarding antenatal care for women who live in rural areas, who are less educated, and who have no previous antenatal care experience should be provided, and comprehensive family planning services to prevent unplanned pregnancy are needed.
Similar content being viewed by others
Background
Antenatal care (ANC) is the care provided by skilled health professionals to pregnant women to ensure the best health conditions for both the mother and the baby during and after pregnancy. Risk identification, prevention and management of pregnancy-related complications, health education and promotion are the major components of ANC [1]. ANC reduces maternal and newborn morbidity and mortality both directly, through the identification and treatment of pregnancy-related complications and indirectly, through the detection of women at high risk of developing complications during labour and delivery, thus enabling referral to an appropriate level of care. In 2016, the WHO recommended a minimum of eight ANC contacts, with the first contact to take place in the first trimester [2].
Every two minutes, somewhere on our planet especially in low-income countries, women of reproductive age die from problems linked to pregnancy and childbirth [3]. According to WHO, in 2020, there were 287,000 maternal deaths, 2.4 million neonatal deaths and an estimated 2 million stillbirths, almost all of which occurred in low and middle-income countries, especially in sub-Saharan Africa and South Asia [3,4,5,6]. By 2030, one of the targets of ending preventable maternal and neonatal mortality is to lower the global maternal mortality ratio (MMR) to less than 70 per 100,000 live births and to reduce neonatal mortality to at least as low as 12 per 1,000 live births [7]. Early ANC initiation plays an important role in achieving the above goals. It maximizes the probability of adherence to the clinically indicated check-up schedule while giving healthcare providers enough time to identify and successfully treat diseases like syphilis, anaemia, malaria, and hypertension and to alleviate and mitigate health conditions that may lead to complications for the mother and baby later on [8].
However globally, the prevalence of early ANC bookings was only 58.6%. In developing countries, only half of the women initiated ANC within the first trimester of pregnancy. ANC within the first trimester of pregnancy was 69.1% and 68.1%, in Asia, and Latin America respectively and 40.8% in Sub-Saharan Africa (SSA) [9]. Although there has been good progress in the coverage of early antenatal care visits; it is still low in developing countries, especially in SSA [10]. In Ethiopia, only 28% of the woman had their first ANC contact during the first trimester [11].
According to previous studies, socio-demographic factors such as maternal age and wealth status, and obstetrics factors such as previous ANC use were found to be important determinant factors for the time of ANC visit initiation [8, 12,13,14,15]. In Ethiopia, particularly in the study area, studies targeted the time of antenatal care initiation (survival time) was scarce and they were limited to few variables. Therefore, this study aimed to assess the time to initiation of antenatal care visit and its predictors among pregnant women who delivered in Arba Minch town public health facilities and the finding will provide important evidence on time to initiation of antenatal care visit to concerned bodies to take evidence-based intervention according to the identified predictors. Thus, it will be useful in reducing maternal and neonatal morbidity and mortality by promoting early initiation of antenatal care visits.
Methods
Study setting, design and period
An institution-based retrospective follow-up study was carried out at public health facilities in Arba Minch town. Arba Minch is located in the Gamo Zone, southern Ethiopia approximately 500 km south of Addis Ababa and 275 km from Hawassa at an elevation of 1285 m above sea level. It has one general and one primary public hospital with two health centres:- Naming Arba Minch General and Dilfana primary hospitals, Secha and Woze health centers. There were a total of 953 healthcare providers in all health facilities. All facilities provide maternal health services like ANC, delivery and post-natal care, in addition to other routine health services. The ANC and delivery services were mainly given by midwives [16]. According to the “Population Projection of Towns as of July 2021” conducted by the CSA ( SCentral Statistical Agency), this town has a total population of 192,043 [17]. The study was conducted from June 01, 2023, to June 30, 2023.
Population
All pregnant women who delivered in Arba Minch town public health facilities were the source population whereas all selected pregnant women who delivered in Arba Minch town public health facilities during the study period who fulfilled the inclusion criteria were the study population. Women who were unable to respond due to severe illness or whose gestational age during antenatal care initiation was not registered in their ANC follow-up cards were excluded.
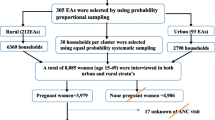
Sample size determination and sampling technique
The sample size was determined by using Stata17.0 by taking a confidence level of 95%, power of 80%, and a 10% withdrawal. Having a higher education level, being an urban resident, and being the richest were found to be major predictor variables from a previous study and the final sample size was 436 [12, 14]. The study was done in one month and the average number of deliveries per month in all health facilities was 1302. So, the systematic random sampling technique with a K value of 3 (1302/436) was used to get the respective respondents from each health facility. We collected our data during delivery so as to get those mothers who came for delivery without having ANC throughout pregnancy (censored mothers).
Variables
The time to initiation of antenatal care visit was the outcome variable whereas Socio-demographic and socio-economic factors like residence, age, marital status, educational status, occupation, religion, average monthly income, family size, partner education and occupation, obstetric factors like age at marriage, gravidity, parity, birth interval, age at first birth, place of delivery for previous pregnancy, mode of delivery for previous pregnancy, previous ANC use, previous pregnancy complication, pregnancy intention, means of pregnancy recognition, autonomy on a decision, and partner involvement during ANC were the independent variables.
Operational definitions
Time to initiation of ANC
The time was measured in weeks from the date of pregnancy to the time of ANC initiation [18].
Event
The event was considered to occur if the pregnant woman had at least one ANC visit throughout pregnancy.
Censored
The event was considered censored if a pregnant woman delivered without any ANC visit.
Pregnancy-related complications
Are defined as health problems that occur during Pregnancy and affect the mother’s health, baby’s health or both [19].
Data collection and management
A structured interviewer-administered questionnaire was prepared after reviewing different literature to collect relevant data [8, 12,13,14,15]. The data were collected by two health professionals with one supervisor. Data collectors obtained all relevant data related to socio-demographic, socio-economic, and obstetric-related factors by interviewing a woman and the outcome variable by reviewing ANC cards. The data collection tool was first prepared in English language and translated into Amharic language and then back to English. A 5% pretest was performed. Two days of training were provided to data collectors. The supervision was performed at each step of data collection and the collected data were checked for consistency and completeness before data analysis.
Data processing and analysis
Data collection was performed using Kobo collect and Stata 17.0 was used for data cleaning and statistical analysis. Descriptive analysis, such as the mean with standard deviation, median with interquartile range, frequency and percentages were used to describe different variables. A Kaplan-Meier (KM) survival curve was used to estimate the median survival time and a Log-rank test was used to compare the survival probabilities. Cox proportional hazard regression analysis was used to identify predictor variables. Independent variables having a P-value ≤ 0.25 in the bivariable analysis were fitted into the final multivariable model for further analysis. Multi-collinearity between variables was checked using a variance inflation factor with a cut-off point with a median VIF < 5. The assumptions of the Cox proportional hazard regression model were checked based on the Schoenfeld residual global test and the goodness fit of the model was checked by using the Cox–Snell residual and Nelson Aalen cumulative hazard plot. Adjusted hazard ratios (AHRs) with 95% confidence intervals (CIs) and P-value ≤ 0.05 were used to assess the strength of association and statistical significance.
Results
Socio-demographic characteristics
Out of 436 women who were invited to participate, (99%) were interviewed and included in the analysis. The mean age of the women was 26.26 years, with a standard deviation of (± 4.78) years. The majority of the women (93.7%) were urban dwellers (Table 1).
Obstetrics and other related factors
Among the study participants, 93% of the women had a history of ANC visits for their previous pregnancy. The majority (83.1%) of the current pregnancies were planned and 16.4% of the women had a previous history of pregnancy-related complications (Table 2).
Time to initiation of the first ANC visit
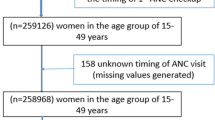
The survival function was computed using the Kaplan-Meier survival estimate. The overall median survival time to the first ANC initiation was 18 weeks (CI = 17, 19). The total follow-up time contributed by all study participants was 8332-person weeks. The cumulative probability of the first ANC initiation was 14.3% at 12 weeks, 52% at 18 weeks, 82.9% at 24 weeks, 94.7% at 30 weeks, and 97.9% at 40 weeks (Fig. 1).
Comparison of survival probabilities among categories of different independent variables
Kaplan-Meier survival curves together with the log-rank test were performed to compare the survival probabilities among categories of different predictor variables. Women who lived in urban areas had significantly lower survival probability than those who lived in rural areas (Pr > chi2 = 0.0000). Mothers with tertiary and above educational levels had statistically significantly lower survival probability compared to those with secondary and primary level education (Pr > chi2 = 0.0000) (Fig. 2).
Predictors of time to initiation of ANC visit
Bivariable and multivariable Cox regression analysis
In the Bivariable Cox proportional hazard regression analysis, statistical significance was observed among the variables place of residence, average monthly income, level of education of the women, level of education of the partner, birth interval, pregnancy-related complications, ANC follow-up for last pregnancy, and intention of pregnancy (Table 3).
Predictors that had an association at p-value ≤ 0.25 in bivariable Cox proportional hazard regression were included in multivariable regression to control the effect of confounders. Finally, place of residence, level of education of the women, pregnancy-related complications, ANC follow-up for the last pregnancy and intention of pregnancy were found to be predictors of the time to initiation of the first ANC visit.
The timing of ANC initiation was 2.67 times shorter among women who lived in urban areas than among those who lived in rural areas (AHR = 2.67; 95% CI = 1.52, 4.71; P < 0.001). The timing of ANC initiation was 1.9 times shorter for women who attained a tertiary and above level of education than for those who were in primary and under the primary level of education (AHR = 1.90; 95% CI = 1.28, 2.81; P < 0.001). The timing of ANC initiation was 1.53 times shorter for women who had pregnancy-related complications in their previous pregnancy than for those who had no history of pregnancy-related complications in their previous pregnancy (AHR = 1.53; 95% CI = 1.08, 2.16; P < 0.015). The timing of ANC initiation among mothers who had no ANC follow-up for their previous pregnancies was longer by 61% as compared to those who had ANC follow-up for their last pregnancy (AHR = 0.39; 95% CI = 0.21, 0.71; P < 0.002). The timing of ANC initiation among mothers who had unplanned pregnancies was longer by 34% as compared to those who had planned pregnancies (AHR = 0.66; 95% CI = 0.48, 0.91; P < 0.013) (Table 3).
Discussion
The main goal of the study was to determine the time to initiation of ANC visit and its predictors among pregnant women who delivered in Arba Minch town public health facilities, Gamo zone, Southern Ethiopia, 2023. The overall median time to ANC initiation was 18 weeks. Being an urban resident, having a tertiary and above level of education, having pregnancy-related complications in a previous pregnancy, not having previous antenatal care visit and unplanned pregnancy were found to be the predictors for the time to initiation of antenatal care visit.
According to this study, the median time to ANC initiation was 18 weeks, meaning half of the pregnant women start their ANC visit after 18 weeks of their pregnancy, which is not in line with the 2016 WHO ANC recommendation which is before 12 weeks; this, in turn, implies that many women are at risk of several obstetric complications which may lead to maternal and neonatal morbidity and mortality. This finding is consistent with a study from low and middle-income countries (Malawi, Zambia, Uganda, Yemen, and Mali) [20] and Afghanistan [21] which is 4 months. However, the median time to ANC initiation was earlier as compared to the study performed in Nigeria [15, 22] which is 6 months, which may be due to differences in the study setting: the participants from this study were mainly from an urban area where women had access to education, media and health facilities whereas the study in Nigeria was from the Nigerian demographic and health survey where the majority of the women were from rural areas [15, 22]. The median time to ANC initiation was later than the findings from Paraguay, Indonesia and Cambodia [20]. This variation might be due to socio-demographic and, socio-economic differences.
In this study, place of residence was a significant predictor for time to initiation of ANC visit. Women who reside in urban areas initiate ANC visits earlier than those who live in rural areas. It is in line with a study conducted in Ethiopia [23, 24], Nepal [25], Nigeria [15, 22, 26], and Bangladesh [27]. Similarly, a study performed in low- and middle-income countries stated that women who initiated ANC early were mainly from urban areas [20]. Women from urban areas may be aware of the importance of early ANC initiation and its role in ensuring maternal and child health as they have better educational opportunities [28] and easy access to various media outlets [29]. Additionally, the geographical location of urban areas offers a distinct advantage in terms of healthcare accessibility. Urban regions are typically well-equipped with a variety of healthcare facilities, including hospitals, clinics, maternity centres, and specialized healthcare providers. The proximity of these facilities to residential areas may reduce travel time and logistical challenges, making it easier and more convenient for urban women to access ANC services timely [30, 31].
According to the findings of this study, the level of education of the women was found to be a significant predictor for the time to initiation of ANC visits. Women who have a tertiary and above level of education initiate their ANC visit earlier than those with secondary and primary levels, which is consistent with a study conducted in Ethiopia [8, 12, 14, 18], Nepal [25], Nigeria [15, 22, 26], and Bangladesh [27]. Education enhances women’s capabilities, particularly in understanding and accessing healthcare services [32]. Women with higher educational levels tend to initiate ANC earlier as they have easy access to health-related information and can easily comprehend information conveyed in various formats and methods [24]. Furthermore, educated women are empowered to make independent health decisions, allowing them to take charge of their own healthcare choices, including when and how to initiate ANC, based on their informed understanding and knowledge [32, 33].
Similarly, pregnancy-related complications were found to be another predictor for the time to initiation of ANC visits. Women who faced pregnancy-related complications in their previous pregnancy were more likely to initiate their ANC visit earlier than their counterparts, which is in line with the findings from Ethiopia [23, 34], Rwanda [35] and Tanzania [36]. Women who have previously experienced pregnancy complications or adverse outcomes are more proactive in seeking early ANC services for subsequent pregnancies [37]. Their past experiences may alert them to prioritize comprehensive ANC to prevent similar complications from recurring and to ensure better pregnancy outcomes. Having encountered challenges during a previous pregnancy, these women are often more informed and aware of the potential risks and complications associated with pregnancy. This heightened awareness can motivate them to be more diligent and attentive towards their antenatal health, prompting them to seek timely medical advice and interventions through ANC services [38]. ANC visits in previous pregnancies were found to be another predictor for the time to initiation of ANC visits. Women who had not had ANC service in their previous pregnancy initiated their ANC visit later than those who had. This is in line with the studies from Ethiopia [39, 40], and Afghanistan [21]. Health facilities often serve as crucial platforms for health education and promotion. Women attending ANC previously could receive information, guidance, and counselling on various aspects of pregnancy, ANC, and childbirth. These educational sessions empower them with knowledge related to maternal and child health thus enabling the timely initiation of ANC visits [41]. Women who have no previous ANC experience may not know the services given during ANC, so, they may fear and feel unfamiliar with getting ANC service in health facilities timely [39].
Furthermore, the intention of pregnancy is found to be a predictor for the time to initiation of ANC visits. Women who had unplanned pregnancies were found to initiate ANC visits later than those who had planned pregnancies, which is in line with the studies performed in Nepal [25], Afghanistan [21], Gambia [42], South Africa [43] and south and southwest Ethiopia [13, 44]. Women who find themselves with unplanned pregnancy may experience a range of emotions, including anxiety, sadness or regret. This emotional turmoil can affect their acceptance and attitude towards the pregnancy and can result in late ANC initiation [45]. Additionally, the unexpected nature of unplanned pregnancies can result in delayed recognition and awareness of their pregnancy status and can lead to late ANC initiation [46]. Furthermore, If the partner is not in favour of the pregnancy, he may exert control or dominance over the woman’s healthcare decisions, refusing to grant permission or accompany her to ANC appointments, further restricting her access to essential ANC services [47].
Limitations of the study
Knowledge and attitude about ANC were not measured due to the retrospective nature of the study. The outcome variable for different women was measured differently as there are different methods for gestational age measurement like; ultrasound measurement, and gestational age based on the last normal menstrual period.
Conclusion
The median time to ANC initiation was 18 weeks. Half of the pregnant women start their ANC visit after 4.2 months, which is not in line with the 2016 WHO recommendation as it schedules the first contact to take place before three months of pregnancy. Being an urban resident, having a tertiary and above level of education of the women, and having pregnancy-related complications in a previous pregnancy were found to be a positive predictor for antenatal care initiation whereas not having a previous antenatal care visit and having unplanned pregnancy were negative predictors for the time to initiation of antenatal care. Therefore, targeted community outreach programs including educational campaigns regarding ANC for women who live in rural areas, who are less educated, and who have no previous antenatal care experience should be provided, and comprehensive family planning services to prevent unplanned pregnancy are needed.
Availability of data and materials
The datasets used during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ANC:
-
Antenatal care
- AHR:
-
Adjusted hazard ratio
- CHR:
-
Crude hazard ratio
- CI:
-
Confidence interval
- EDHS:
-
Ethiopian demographic and health survey
- KM:
-
Kaplan-meier
- NGO:
-
Non-governmental organization
- SSA:
-
Sub saharan africa
- WHO:
-
World health organization
References
Debelo BT, Danusa KT. Level of late initiation of Antenatal Care visit and Associated factors amongst Antenatal Care Attendant mothers in Gedo General Hospital, West Shoa Zone, Oromia Region, Ethiopia. Front Public Heal. 2022;10(June):1–8.
Tesfaye G, Loxton D, Chojenta C, Semahegn A, Smith R. Delayed initiation of antenatal care and associated factors in Ethiopia: A systematic review and meta-analysis. Reprod Health. 2017;14(1):1–17.
Abrams J. New Jersey medicine: the journal of the Medical Society of New Jersey. Matern Mortal. 1990;87:975–6 [cited 2023 Mar 15]. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality .
Estimates by WHO U, UNFPA WBG and, Division the UNP. Vol. 390, The Lancet. 2017 p. S29 Trends in Maternal Mortality 2000 to 2017. [cited 2023 Mar 11] https://www.unfpa.org/featured-publication/trends-maternal-mortality-2000-2017.
Liu L, Hug L, Yeung D, You D, Oxford Research Encyclopedia of Global Public Health. 2023 Newborn Mortality. [cited 2023 Mar 15]. https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-child-mortality-report-2021.
The Lancet. Ending preventable stillbirths: an Executive Summary for The Lancet’s Series. Lancet. 2016;1–8.
Healthwell-being G. A legal guide.
Kitaw TA, Haile RN. Time to first antenatal care booking and its determinants among pregnant women in Ethiopia: survival analysis of recent evidence from EDHS 2019. BMC Pregnancy Childbirth [Internet]. 2022;22(1):1–11. https://doi.org/10.1186/s12884-022-05270-1.
Moller AB, Petzold M, Chou D, Say L. Early antenatal care visit: a systematic analysis of regional and global levels and trends of coverage from 1990 to 2013. Lancet Glob Heal [Internet]. 2017;5(10):e977-83. https://doi.org/10.1016/S2214-109X(17)30325-X.
United Nations International Children’s Emergency Fund. 2019. 2019 pp. 1–7 Antenatal Care - UNICEF data. [cited 2023 Mar 13] https://data.unicef.org/topic/maternal-health/antenatal-care/.
Ethiopian Public Health Institute (EPHI), ICF. Ethiopia Mini Demographic and Health Survey 2019: Final Report [Internet]. 2021. 1–207 p. https://dhsprogram.com/pubs/pdf/FR363/FR363.pdf.
Seid A, Ahmed M. Survival time to first antenatal care visit and its predictors among women in Ethiopia. PLoS One [Internet]. 2021;16:1–11. https://doi.org/10.1371/journal.pone.0251322.
Gebremeskel F, Dibaba Y, Admassu B. Timing of First Antenatal Care Attendance and Associated Factors among Pregnant Women in Arba Minch Town and Arba Minch District, Gamo Gofa Zone. South Ethiopia J Environ Public Health. 2015;2015:1–8.
Dewau R, Muche A, Fentaw Z, Yalew M, Bitew G, Amsalu ET, et al. Time to initiation of antenatal care and its predictors among pregnant women in Ethiopia: Cox-gamma shared frailty model. PLoS One [Internet]. 2021;16:1–18. https://doi.org/10.1371/journal.pone.0246349. (2 February).
Fagbamigbe AF, Abel C, Mashabe B, Adebowale AS. Survival analysis and prognostic factors of the timing of first antenatal care visit in Nigeria. Adv Integr Med [Internet]. 2019;6(3):110–9. https://doi.org/10.1016/j.aimed.2018.12.002.
Mersha A, Shibiru S, Girma M, Ayele G, Bante A, Kassa M, et al. Health professionals practice and associated factors towards precautionary measures for COVID-19 pandemic in public health facilities of Gamo zone, southern Ethiopia: A crosssectional study. PLoS One [Internet]. 2021;16:1–17. https://doi.org/10.1371/journal.pone.0248272. (3 March).
Adiyabo-wereda T, Hageray-town A. Daero-town A. Population Size of Towns by Sex. Region, Zone and Weredas as of July; 2021.
Fentaw KD, Fenta SM, Biresaw HB, Mulugeta SS. Time to first antenatal care visit among pregnant women in Ethiopia: secondary analysis of EDHS 2016; application of AFT shared frailty models. Arch Public Heal. 2021;79(1):1–14.
Tamale BN, Bulafu D, Isunju JB, Jamu AV, Baguma N, Tigaiza A et al. 1,5,3,. 2022.
Jiwani SS, Amouzou A, Carvajal-Aguirre L, Chou D, Keita Y, Moran AC, et al. Timing and number of antenatal care contacts in low-and middle-income countries: Analysis in the Countdown to 2030 priority countries. J Glob Health. 2020;10(1):1–12.
Samiah S, Stanikzai MH, Wasiq AW, Sayam H. Factors associated with late antenatal care initiation among pregnant women attending a comprehensive healthcare facility in Kandahar Province, Afghanistan. Indian J Public Health. 2021;65(3):298–301.
Fagbamigbe AF, Mashabe B, Lepetu L, Abel C. Are the timings and risk factors changing? Survival analysis of timing of first antenatal care visit among pregnant women in Nigeria (2003–2013). Int J Womens Health. 2017;9:807–19.
Adulo LA, Hassen SS. Magnitude and Factors Associated with late initiation of Antenatal Care Booking on First visit among women in rural parts of Ethiopia. J Racial Ethn Heal Disparities. 2023;10(4):1693–702.
Ambaye E, Regasa ZW, Hailiye G. Early initiation of antenatal care and its associated factors among pregnant women attending antenatal care at public health centres in Bahir Dar Zuria Zone, Northwest Ethiopia, 2021: a cross-sectional study. BMJ Open. 2023;13(1):e065169.
Paudel YR, Jha T, Mehata S. Timing of First Antenatal Care (ANC) and inequalities in early initiation of ANC in Nepal. Front Public Heal. 2017;5(September):1–6.
Fagbamigbe AF, Olaseinde O, Fagbamigbe OS. Timing of first antenatal care contact, its associated factors and state-level analysis in Nigeria: a cross-sectional assessment of compliance with the WHO guidelines. BMJ Open. 2021;11(9):e047835.
Sarker BK, Rahman T, Rahman T, Rahman M. Factors associated with the timely initiation of antenatal care: findings from a cross-sectional study in Northern Bangladesh. BMJ Open. 2021;11(12):1–10.
Sisaye S. Education and Rural Development in Ethiopia. Agric Admin. 1985;20(4):237–55. https://doi.org/10.1016/0309-586X(85)90015-9.
Gilano G, Hailegebreal S, Sako S, Seboka BT. Understanding the association of mass media with the timing of antenatal care in Ethiopia: an impression from the 2016 Ethiopia demographic and health survey. J Matern Neonatal Med. 2023;36(1). https://doi.org/10.1080/14767058.2023.2183760.
Demsash AW, Walle AD. Women’s health service access and associated factors in Ethiopia: application of geographical information system and multilevel analysis. BMJ Heal Care Inf. 2023;30(1):1–9.
Spasojevic N, Vasilj I, Hrabac B, Celik D. Rural - Urban Differences in Health Care Quality Assessment. Mater Socio Med. 2015;27(6):409.
Raghupathi V, Raghupathi W. The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015. Arch Public Heal. 2020;78(1):1–18.
Raru TB, Ayana GM, Zakaria HF, Merga BT. Association of higher Educational Attainment on Antenatal Care utilization among pregnant women in East Africa Using Demographic and Health Surveys (DHS) from 2010 to 2018: a Multilevel Analysis. Int J Womens Health. 2022;14(February):67–77.
Ewunetie AA, Munea AM, Meselu BT, Simeneh MM, Meteku BT. DELAY on first antenatal care visit and its associated factors among pregnant women in public health facilities of Debre Markos town, North West Ethiopia. BMC Pregnancy Childbirth. 2018;18(1):1–8.
Schmidt CN, Butrick E, Musange S, Mulindahabi N, Walker D. Towards stronger antenatal care: understanding predictors of late presentation to antenatal services and implications for obstetric risk management in Rwanda. PLoS ONE. 2021;16(8 August):1–4.
Gross K, Alba S, Glass TR, Schellenberg JA, Obrist B. Timing of Antenatal Care for Adolescent and Adult Pregnant Women in South-Eastern Tanzania. BMC Pregnancy and ChildB. 2012;12(1):1–12. https://doi.org/10.1186/1471-2393-12-16.
Gelassa FR, Tafasa SM, Kumera D. Determinants of early antenatal care booking among pregnant mothers attending antenatal care at public health facilities in the Nole Kaba district, western Ethiopia: unmatched case-control study. BMJ Open. 2023;13(10):1–9.
Cǒté-Arsenault D, Mahlangu N. Impact of Perinatal Loss on the Subsequent Pregnancy and Self: Women’s Experiences. J Obstet Gynecol Neonatal Nurs [Internet]. 1999;28(3):274–82. https://doi.org/10.1111/j.1552-6909.1999.tb01992.x.
Girma N, Abdo M, Kalu S, Alemayehu A, Mulatu T, Hassen TA, et al. Late initiation of antenatal care among pregnant women in Addis Ababa city, Ethiopia: a facility based cross-sectional study. BMC Womens Health [Internet]. 2023;23(1):1–8. https://doi.org/10.1186/s12905-022-02148-4.
Grum T, Brhane E. Magnitude and factors associated with late antenatal care booking on first visit among pregnant women in public health centers in central zone of Tigray Region, Ethiopia: a cross sectional study. PLoS ONE. 2018;13(12):1–9.
by Dove Press published. IJWH-75164-review- - - -. 2015;239–42.
Nigatu SG, Birhan TY. The magnitude and determinants of delayed initiation of antenatal care among pregnant women in Gambia; evidence from Gambia demographic and health survey data. BMC Public Health. 2023;23(1):1–10.
Ebonwu J, Mumbauer A, Uys M, Wainberg ML, Medina-Marino A. Determinants of late antenatal care presentation in rural and peri-urban communities in South Africa: a cross-sectional study. PLoS ONE. 2018;13(3):1–16.
Tadele F, Getachew N, Fentie K, Amdisa D. Late initiation of antenatal care and associated factors among pregnant women in Jimma Zone Public Hospitals, Southwest Ethiopia, 2020. BMC Health Serv Res. 2022;22(1):1–8. https://doi.org/10.1186/s12913-022-08055-6.
Tolossa T, Turi E, Fetensa G, Fekadu G, Kebede F. Association between pregnancy intention and late initiation of antenatal care among pregnant women in Ethiopia: a systematic review and meta-analysis. Syst Rev. 2020;9(1):1–10.
Watson K, Angelotta C. The frequency of pregnancy recognition across the gestational spectrum and its consequences in the United States. Perspect Sex Reprod Health. 2022;54(2):32–7.
Kazemi A, Ghaedrahmati M, Kheirabadi G. Partner’s emotional reaction to pregnancy mediates the relationship between pregnancy planning and prenatal mental health. BMC Pregnancy Childbirth. 2021;21(1):1–8.
Acknowledgements
We would like to thank Arba Minch University, Gamo Zone health department, Arba Minch Town health office, managers of health facilities staff at Arba Minch Town public health facilities who work in maternal and child health units and the study participants for their great cooperation in this research.
Funding
There is no funding obtained for this study.
Author information
Authors and Affiliations
Contributions
AGB: Developed the proposal, did analysis and interpretation of the result, and prepared the manuscript. MKD, MKG, NBS, MSS and MYT: assisted in the design and the proposal development, assisted during analysis, and revised subsequent drafts of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Before the study was conducted, an ethical clearance letter was obtained from the institutional review board (IRB) of Arba Minch University with reference number IRB/1447/2023. Then, an official support letter was obtained from the School of Public Health, Arba Minch University and permission was obtained from the Gamo Zone Health Bureau, Arba Minch City Health Office and managers of health facilities. Informed consent was obtained from each respondent. The purpose, potential risks and benefits of participating, and the right to withdraw from the study at any time were explained to the study participants. The information collected for this research was kept confidential and stored in files.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Belete, A.G., Debere, M.K., Gurara, M.K. et al. Time to initiation of antenatal care and its predictors among pregnant women who delivered in Arba Minch town public health facilities, Gamo Zone, southern Ethiopia, 2023: a retrospective follow-up study. Reprod Health 21, 73 (2024). https://doi.org/10.1186/s12978-024-01818-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-024-01818-w