Abstract
Background
Sexually transmitted infection is a common public health issue of youths and is characteristically transmitted through sexual intercourse. Even though early treatment for sexually transmitted infection is very important to reduce further complications and economic burden, studies to identify the proportion and the possible factor of early treatment seeking is rare in Ethiopia.
Objective
To assess the proportion of early treatment seeking for sexually transmitted infections and associated factors among patients attending youth friendly service in Bahir Dar city health centers, northwest, Ethiopia 2023.
Method
Institutional based Cross-sectional study was used among 407 participants from April 25 to May 24 /2023. A systematic random sampling technique was used to select the participants. An interview-administered questionnaire was used for data collection, whereas Epi-data version 4.6.0.2 and the statistical package for statistical science version 23 were used for data entry and analysis respectively. A frequency table and bar chart were used for descriptive analysis. Multiple binary logistic regression was employed to identify the factors at p-value of <0.05. The necessary assumption of the model was also checked by the Hosmer and Lemishow test.
Results
The response rate of this study was 391 (96.1%) and the proportion of early treatment for sexually transmitted infection was 108 (27.6%, 95%CI; 23-32). Good knowledge about sexually transmitted infection (AOR=1.98, 95CI%; 1.13-3.47) know about their HIV status (AOR=1.95, 95%CI; 1.13-3.36), perceive severity of sexually transmitted infection (AOR=11.23, 95%CI; 6.15-20.45), and not fear the stigma about being infected with sexually transmitted infection (AOR=2.29, 95%CI; 1.32-3.96) were the significantly associated factors for early treatment of sexually transmitted infection.
Conclusion and recommendation
The proportion of early treatment for sexually transmitted infection in Bahir Dar city was low. Knowledge about STIs, testing/ knowing HIV status, perception of the severity about sexually transmitted infection, and fear of stigma about sexually transmitted infection were the statistically significant factors for early treatment of sexually transmitted infection. So the government better give attention to health education and other health promotion activities to increase the knowledge of youths about sexually transmitted infection and to change their perception of sexually transmitted infection.
Similar content being viewed by others
Introduction
Sexually transmitted infection is a common public health issues of youths and is characteristically transmitted through sexual intercourse that can either end or advanced into sexually transmitted disease [1]. Bacteria, viruses and parasites are responsible for STIs such as for gonorrhea, chlamydial infection, syphilis, trichomoniasis, chancroid, genital herpes, human immunodeficiency virus infection and hepatitis B infection [2].
Especially, STI affects the young and adolescents groups [3, 4]. Unless STIs patients seek treatment early, it is endanger to transmit the infection and can be increase the risk of complications [5]. Thus the transmission rate of the human immunodeficiency virus can be increased by because of the treatment of STIs is not early [6]. Unmanaged STIs could be causes of obstetrics and gynecologic complication, severe psychological problems and cervical cancer [7]. Additionally, not early treatment of these infection could lead to health and economic burden. Particularly, in less developed countries the impact of untreated STI accounts about 17% of all economic losses [8]. The World Health Organization (WHO) report showed that, about 374 million new cases of curable STI (syphilis, gonorrhea and chlamydia) has occurred in 2021 [9]. From this figure, 40% of the global burden of STI is from sub-Saharan Africa [10]. As report in Benishangul Ethiopia revealed, the proportion of early treatment for STI is 40.1% [11]. As evidences showed, patients with one or more sign/symptom of STI usually visit health institutions too late. Because of some STI symptoms causes embracement and so patients are favor to be have self-medication and access the drugs from drugs stores with very minimum counseling that leads to drug resistance [12]. The other reason for not treating STIs early is because social stigma [13].
Studies showed that early treatment seeking behavior of the STI can be influenced by several factors such as educational status [14,15,16], knowledge about STIs [11, 15, 17, 18], perception about STIs [19, 20]., fear of stigma [11, 14, 20], numbers of sexual partners [11]. The WHO set a strategy on STIs in 2016 to end up the epidemic of STIs between 2016- 2021 [21]. But treatment seeking for STIs is still too low. Even though there are key strategic objectives about the quality services of adolescent health in Ethiopia [22], there is no adequate studies about early treatment seeking of STIs to design evidence based prevention mechanisms, strategies and policy to promote early treatment seeking behavior of STIs. Therefore this study was aimed to assess the prevalence of early treatment seeking and its associated factors among youths in Bahir Dar health centers.
Methods and materials
Study design, setting and study period
Institutional based cross-sectional study was employed from April 25/2023 to May 24/2023 in Bahir Dar city. Bahir Dar city is located about 565 km to the Addis Ababa, a capital city of Ethiopia. Bahir Dar city is located in the North Western part of Ethiopia. In the city, 15-24 age group accounts about 78,930 [23]. In Bahir Dar city administration, there are 10 health centers namely Shumabo, Shimbit, Bahir Dar, Meshentie, Abay, Dagmawi minilik, Zegie, Zenzelima, Tis Abay and Han. All these institutions provides the youth friendly service in a separate room.
Population
All patients with STI in youth friendly service of Bahir Dar city health centers were the source and study population. All patients of youth friendly service diagnosed with STI in Bahir Dar city health centers were included in the study.
Variables
Dependent variable
Early treatment seeking for STI (Yes, No)
Independent variables
Socio-demographic variables: age, sex, ethnicity, religion, residence, educational status and wealth index.
Knowledge and perception about STI: knowledge about STI, perception towards STI (severity, treatment), fear of stigma and believe about STI treatment.
Behavioral factors: numbers of sexual partner, age at the first sex, being tested for HIV, media exposure and distance from the health facility.
Operational definitions
Time of health care seeking for STIs: The extent of time of health care seeking is define to the patient “How long day did you wait or postpone before seeking treatment at the health facility after noticing the first symptoms of sexual transmitted infection?” It has two response categories: Early health care seeking refers to patients who seek care and/or advice within 7 days of the onset of the STI symptoms. And Delayed/not early health care seeking refers to patients who seek care and/or advice after 7 days of the onset of the STI symptoms [11].
Multiple sexual partners: are defined as the behavior of a person with two or more sexual partners [24].
Knowledge about STIs: A mean score was used to determine the knowledge status of respondents on STIs. Respondents who score above the mean were categorized as having good knowledge and those who score equal to or below mean were categorized as having poor knowledge [14].
Patients with STIs: in this study referred as patients who presented with one or more of STI symptoms like urethral discharges, vaginal discharges, lower abdominal pain, penile ulcers or ulcers of the vulva or vagina, perineal ulcers, genital or perineal warts or painful micturition and other STI symptoms [25].
Sample Size determination
The required sample size was determined by considering the single population proportion of early treatment seeking 40.1% which was conducted in Benishangul Gumuz Ethiopia [14] with the confidence level (CL) of 95% and a margin of error 5% . Based on these information, the sample size was calculated as follows.
Sampling procedure and sampling technique
First all health centers were identified namely Bahir Dar, Han, Shumabo, Meshentie, Tis Abay, Zenzelima, Dagmawi Minilik, Zegie, Shimbit and Abay and then all health centers were included in the study to be more representative and get adequate sample size. From each heath centers, numbers of participants was allocated proportionally to the size by using previous two consecutive months STI report of each health centers. Then to allocate the participants; “N” which was the number of patients treated in the previous two consecutive months and “n” was the number of samples allocated for a particular health centers then the interval (k) was determined by “N/n” and the random start was selected by lottery method (Fig. 1). Finally, a systematic random sampling method was used to select the eligible participants.
Data collection procedures and data quality assurance
A structured interview administered questionnaire was used to assess the proportion of early treatment seeking for STI and associated factors. Based on the objective of the study, the questionnaire was adapted from different litratures [11, 17, 19, 26]. The total duration of data collection was one month (from April 25/2023 to May 24/2023). Data were collected at the health facilities when they were coming to get a service. The social desirability bias was reduced by informing the purpose of the study carefully, making the questionnaire anonymous and collect the data by the health care providors who diagnosed them (to get the valid response). The questionnaire was first prepared in English language and then translated to the Amharic language, which was the local language of the study subjects and back to English by language experts to check their consistency and conceptual equivalence. Amharic version of the questionnaire was used to obtain data from participants. Ten nurses were recrieted for data collectors and monitored by two senior nurse supervisors. Each completed questionnaire was cheeked for coherence, completeness, consistency at the same time. The daily evaluation was performed to correct the problem that was face during the course of data collection and the pretest was conducted at Hamusit health center among 21 (5%) participants. One day intensive training was also given for both data collectors and supervisors.
Data processing and analysis
After cleaning and checking, data were coded and entered into Epi-data version 4.6.0.2 statistical software and exported to SPSS Version 23 statistical software for analysis. Descriptive statistics was summarized by using frequency, table and bar graph. All variables with a p-value of < 0.25 in the simple binary logistic regression analysis was kept for multivariable binary logistic regression analysis. A variable with a p-values of < 0.05 was considered as a statistically significant. Adjusted odds ratios with 95% CL was used to report the association between dependent and independent variables. The model fitness of binary logistic regression was checked by using Hosmer–Lemishow goodness of fit test with a p-value of > 0.05.
Results
Socio demographic characteristics of the participants
The response rate of this study was 391 (96.1%). Out of these, 249 (63.7%) of the respondents were female. Two hundred forty-two (61.9%) of the respondents were from urban residence. Furthermore, more than half, 272 (69.6%) of the respondents were orthodox religious followers (Table 1).
Knowledge and perception about STI
One hundred eighty-six (47.6%) of the participants were perceived STIs as a curable disease and about 207 (52.9%) of the participants had good knowledge about STIs. Furthermore, 217 (55.5%) of the participants had ever heard about STIs (Table 2).
Sexual behavior and health service accessibility
About 209 (53.5%) of the participants were reported that distance as a big problem to access STI treatment. Two hundred (51.2%) of the participants were not used condom and 69 (34.5%) of them were because of the cost of condom. Furthermore, 251 (64.2%) of the respondents have had one sexual partner in the last 12 months (Table 3).
Proportion of early treatment for STI
In general, 27.6% (95%CI; 23-32) of the participants were found to be treated early for STI (Fig. 2).
Early treatment by sex
About 32% of the female participants were early treat STI (Fig. 3).
Reason for delayed treatment for STI
Among the participants who were not treated early for STI, about 145 of them were because they did not know where to go (Fig. 4).
Factors associated with early treatment for STI
Two subsequent analyses were conducted. The first analysis was a simple binary logistic regression analysis. Of the total variables, knowledge about STIs, educational status, perception of the severity of STIs, fear of stigma, knowing HIV status, perceiving the curability of STIs, attending STI-related messages and residence were the candidate variables for multivariable binary logistic regression at a p-value of < 0.25. In the multivariable binary logistic regression analysis, variables such as knowledge about STI, test/ knowing HIV status, perception of the severity of STI and fear of stigma were the statistically significant variables for early treatment of STI at a p-value of < 0.05 and 95% CL. The model was fitted with a Hosmer and Lemishow test with a p-value of 0.123.
Thus, the odds of early treatment for STI among participants who had good knowledge about STI was 1.98 (AOR=1.98, 95CI%; 1.13-3.47) times more likely than their counterparts. Participants who know about their HIV status were 1.95 (AOR=1.95, 95%CI; 1.13-3.36) times more likely to treat early for STI than they did not know their HIV status. The odds of early treatment for STI among participants who perceive STI as a very serious disease were 11.2 (AOR=11.2, 95%CI; 6.15-20.45) times more likely than those who perceive STI is not a serious disease. Furthermore, participants who did not fear the stigma of being exposed to STI was 2.3 (AOR=2.3, 95%CI; 1.32-3.96) times more likely to treat early for STI than their counterparts (Table 4).
Discussion
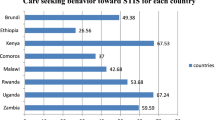
In the current study, an attempt has been made to assess the proportion and its associated factors of early treatment seeking for STI among youths in Bahir Dar city. Thus, the proportion of early treatment seeking for STIs among youths who attend treatment in Bahir Dar city was 27.6% (95% CI; 23-32). Factors like perception towards STIs, knowledge about STIs, knowing their HIV status and fear of stigma were statistically significant factors for early treatment of STIs. The proportion of early treatment seeking for STI in this study was lower than a study conducted in Benishangul 40.1% [14], in South Africa 76.9% [27], in Gahanna 36% [20], in Luwero of Uganda 42% [28], another study conducted in the same country Gahanna 75.4% [15], in United States of America (70%) (41), in Asian country of Laos 58% [29], in Kerala of India 41.9% [30] and in Vietnam 20% [16]. As compared to other parts of Ethiopia, the possible reason for the discrepancy might be because of cultural and health seeking behavior difference across the region of Ethiopia. As compared to other Asian and African countries, the difference might be associated with the variation in socioeconomic, cultural, and health utilization behavior across the countries. Again the war /social unrest in Ethiopia may be also make a difference in the proportion of early treatment for STIs as compared to other countries.
Regarding the factors of early treatment seeking for STI, participants who had good knowledge about STIs were more likely to treat STIs as compared to those who had poor knowledge about STIs. This was supported by a study conducted in South Africa, Ghana, southwest Ethiopia, Benishangul Ethiopia, and Addis Ababa Ethiopia [11, 15, 17, 18]. This can be justified by knowledge is a power for wise decisions and having good knowledge about STIs complications, signs/symptoms, transmission, prevention and the advantage of early treatment enables and motivates the youth to seek the treatment earlier.
The findings of the current study also revealed that the early treatment seeking for STIs was affected by the perceived severity of STIs. That means participants who perceive STIs as a serious diseases had the higher odds of early treatment for STIs than those who perceive STIs as not a serious diseases. This was supported by a study conducted in Ghana, southwest Ethiopia [19, 20]. This might be associated with perceiving the severity of the disease or fear about the complications of STI can positively affect health-seeking behavior, as compared to those who consider STIs is not a serious disease or who perceive SIT as a self-limited disease [11, 31].
Additionally, participants who did not fear about the stigma of being exposed to STIs were more likely to treat early than their counterparts. This was supported by studies conducted in Pakistan, Nkomazi East, and rural Ethiopia [18, 26, 32]. This is because people who are not fearful of being infected with STIs are not socially embarrassed and inform their health problems early to health care providers without embarrassments [33].
Furthermore, testing/knowing the status of HIV was also affects the early treatment of STIs. This means participants who test/know their HIV status had higher odds of early treatment for STI than did not test/know their HIV status. This was supported by studies conducted in India, an African cohort study, Ethiopia and Gambela [11, 34,35,36]. This might be because people who know their HIV status or test for HIV have an opportunity to learn or inform about STIs from their healthcare provider. The limitation of this study was since it was a Crossectional data it shares the limitations of a cross-sessional study design. This study also not assess any difference in treatment seeking behavior of STIs between government and private health institutions. We recommended to conduct a further research on a comparative study of treatment seeking behavior of STIs in government and private health institutions.
Conclusion
The proportion of early treatment for STI in Bahir Dar city was low. Knowledge about STIs, testing/ knowing HIV status, perception of the severity about sexually transmitted infection, and fear of stigma about STI were the statistically significant factors for early treatment of STI. So the government better give attention to health education and other health promotion activities to increase the knowledge of youths about STI and to change their perception of STI.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- CI:
-
Confidence Interval
- CL:
-
Confidence Level
- COVID-19:
-
Corona Virus Disease
- HIV:
-
Human Immune Virus
- OR:
-
Odds Ratio
- STI:
-
Sexually Transmitted Infections
- SPSS:
-
Statistical Package for Statistical Science
- WHO:
-
World Health Organization
References
Shim BS. Current concepts in bacterial sexually transmitted diseases. Korean J Urol. 2011;52(9):589.
Otu A, Danhoundo G, Toskin I, Govender V, Yaya S. Refocusing on sexually transmitted infections (STIs) to improve reproductive health: a call to further action. Reprod Health. 2021;18:1–4.
Workowski KA. Sexually transmitted infections treatment guidelines, 2021. MMWR. Recommendations and Reports. 2021;70.
Kassie BA, Yenus H, Berhe R, Kassahun EA. Prevalence of sexually transmitted infections and associated factors among the University of Gondar students, Northwest Ethiopia: a cross-sectional study. Reprod Health. 2019;16:1–8.
Nasirian M, Karamouzian M, Kamali K, Nabipour AR, Maghsoodi A, Nikaeen R, et al. Care seeking patterns of STIs-associated symptoms in Iran: findings of a population-based survey. Int J Health Policy Manag. 2016;5(1):5.
Shewarega ES, Fentie EA, Asmamaw DB, Negash WD, Fetene SM, Teklu RE, et al. Sexually transmitted infections related care-seeking behavior and associated factors among reproductive age women in East Africa: a multilevel analysis of demographic and health surveys. BMC Public Health. 2022;22(1):1714.
Francis SC, Mthiyane TN, Baisley K, Mchunu SL, Ferguson JB, Smit T, et al. Prevalence of sexually transmitted infections among young people in South Africa: A nested survey in a health and demographic surveillance site. PLoS Med. 2018;15(2):e1002512.
Amin A. Addressing gender inequalities to improve the sexual and reproductive health and wellbeing of women living with HIV. J Int AIDS Soc. 2015;18:20302.
World Health Organization. Report on global sexually transmitted infection surveillance, 2018. 2018. Geneva: World Health Organization; 2022.
World Health Organization. Global health sector strategy on sexually transmitted infections 2016-2021: toward ending STIs. InGlobal health sector strategy on sexually transmitted infections 2016-2021: toward ending STIs 2016.
Tsadik M, Lam L, Hadush Z. Delayed health care seeking is high among patients presenting with sexually transmitted infections in HIV hotspot areas, Gambella town. Ethiopia HIV/AIDS-Research and Palliative Care. 2019;30:201–9.
Togoobaatar G, Ikeda N, Ali M, Sonomjamts M, Dashdemberel S, Mori R, et al. Survey of non-prescribed use of antibiotics for children in an urban community in Mongolia. Bulletin of the World Health Organization. 2010;88:930–6.
Balfe M, Brugha R, O'Donovan D, O'Connell E, Vaughan D. Triggers of self-conscious emotions in the sexually transmitted infection testing process. BMC Res Notes. 2010;3:1–4.
Misganaw D, Wodajo S, Minayehu A. Early Health Care Seeking and Associated Factors Among Patients with Sexually Transmitted Infections in Public Health Facilities of Assosa Zone, Benishangul Gumuz, Western Ethiopia, 2022; Cross sectional study. Insights Herbal Med. 2022;1(1):58–68.
Sawyerr R. Health seeking behaviour among persons with STIs in Ghana. University of Ghana; 2019.
Thu HT, Ziersch A, Hart G. Healthcare-seeking behaviours for sexually transmitted infections among women attending the National Institute of Dermatology and Venereology in Vietnam. Sex Transm Infect. 2007;83(5):406–10.
Nyalela M. Health seeking behaviour in men presenting with sexually transmitted infections at Prince Mshiyeni Gateway Clinic and KwaMashu Community Health Centre in 2015 (Doctoral dissertation).
Amsale C, Yemane B. Knowledge of sexually transmitted infections and barriers to seeking health services among high school adolescents in Addis Ababa, Ethiopia. J AIDS Clin Res. 2012;3(5):2–7.
Begashaw B, Tessema F, Gesesew HA. Health care seeking behavior in Southwest Ethiopia. PloS one. 2016;11(9):e0161014.
Agambire R, Clerk C. Healthcare seeking and sexual behaviour of clients attending the suntreso STI clinic. J Biol Agric Healthc. 2013;3(10):92–100.
Organization WH. 69th World Health Assembly closes. News release (28 May 2016). Geneva: World Health Organization; 2019.
FMoH, Ethiopia. Health sector transformation plan. Addis Ababa, Ethiopia. 2015. vol. 184.
Bureau BDCAE. 2012 Annual Report (Unpublished). [Citation Time(s):1]. 2012.
Yosef T, Daniel A, Nigussie T, Girma Y. Sexual behaviour among technical vocational and educational training (TVET) college students at Mizan-Aman Town, South West Ethiopia, 2018. J AIDS Clin Res. 2019;10(10):803.
Phrasisombath K, Thomsen S, Sychareun V, Faxelid E. Care seeking behaviour and barriers to accessing services for sexually transmitted infections among female sex workers in Laos: a cross-sectional study. BMC Health Serv Res. 2012;12(1):1–9.
Govender I, Eche M. Health-seeking behaviour of people with sexually transmitted infections in the community of Nkomazi East, Mpumalanga. Southern African J Epidemiol Infect. 2012;27(4):195–8.
Nyalela M, Dlungwane T, Taylor M, Nkwanyana N. Health seeking and sexual behaviour of men presenting with sexually transmitted infections in two primary health care clinics in Durban. Southern African J Infect Dis. 2018;33(5):1–6.
Lubega GN, Musinguzi B, Omiel P, Tumuhe JL. Determinants of health seeking behaviour among men in Luwero District. J Educ Res Behav Sci. 2015;4(2):037–54.
Armstrong G, Medhi GK, Kermode M, Mahanta J, Goswami P, Paranjape R. Exposure to HIV prevention programmes associated with improved condom use and uptake of HIV testing by female sex workers in Nagaland. Northeast India BMC public health. 2013;13(1):1–12.
Jayapalan S. Determinants of delay in the health care seeking behaviour of STD patients. Clinical Epidemiology and Global Health. 2015;3:S69–74.
Voeten HA, O’hara HB, Kusimba J, Otido JM, Bwayo JJ, et al. Gender differences in health care-seeking behavior for sexually transmitted diseases: a population-based study in Nairobi, Kenya. Sex Transm Dis. 2004;31:265–72.
Molla M, Emmelin M, Berhane Y, Lindtjørn B. Readiness of youth in rural Ethiopia to seek health services for sexually transmitted infections. African Journal of AIDS Research. 2009;8(2):135–46.
Csa IJCSA. Central Statistical Agency (CSA)[Ethiopia] and ICF. Addis Ababa: Ethiopia Demographic and Health Survey; 2016.
Puthuchira Ravi R, Athimulam Kulasekaran R. Care seeking behaviour and barriers to accessing services for sexual health problems among women in rural areas of Tamilnadu state in India. J Sex Trans Dis. 2014 2(3):4.18.
Semwogerere M, Dear N, Tunnage J, Reed D, Kibuuka H, Kiweewa F, et al. Factors associated with sexually transmitted infections among care-seeking adults in the African Cohort Study. BMC public health. 2021;21(1):1–11.
Handebo S. Sexually transmitted infections related care-seeking behavior and associated factors among reproductive age women in Ethiopia: further analysis of the 2016 demographic and health survey. BMC Women’s Health. 2020;20:1–7.
Acknowledgments
No.
Funding
No funding source.
Author information
Authors and Affiliations
Contributions
Conceptualization: MCA, GZ and AM. Data curation: GZ and AM. Formal analysis: MCA and GZ. Investigation: TA, GZ and AM. Methodology: MCA, TA and GZ. Software: MCA, GZ and AM. Supervision: MCA, GZ. Visualization: TA, AM, GZ. Writing – original draft: Tigist Abuhay and Getachew Zeleke.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the institutional ethical review board of GAMBY medical and Business College.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zeleke, G., Mekonnen, A., Abuhay, T. et al. Proportion of early treatment seeking for sexually transmitted infections and associated factors among patients attending youth friendly service in Bahir Dar City health centers, Northwest, Ethiopia. Reprod Health 21, 85 (2024). https://doi.org/10.1186/s12978-024-01794-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-024-01794-1