Abstract
Background
Systemic lupus erythematosus (SLE) is a life-threatening, chronic, autoimmune disease requiring long term subspecialty care due to its complex and chronic nature. Childhood-onset SLE (cSLE) is more severe than adult-onset, and the cSLE population in South Africa has been reported to have an even higher risk than patients elsewhere. Therefore, it is critical to promptly diagnose, treat, and manage cSLE. In this paper, we aim to describe and evaluate barriers and enablers of appropriate long-term care of cSLE South Africa from the perspective of caregivers (parents or family members).
Methods
Caregivers (n = 22) were recruited through pediatric and adult rheumatology clinics. Individuals were eligible if they cared for youth (≤ 19 years) who were diagnosed with cSLE and satisfied at least four of the eleven ACR SLE classification criteria. Individual in-depth, semi-structured interviews were conducted between January 2014 and December 2014, and explored barriers to and facilitators of ongoing chronic care for cSLE. Data were analyzed using applied thematic analysis.
Results
Four barriers to chronic care engagement and retention were identified: knowledge gap, financial burdens, social stigma of SLE, and complexity of the South African medical system. Additionally, we found three facilitators: patient and caregiver education, robust support system for the caregiver, and financial support for the caregiver and patient.
Conclusion
These findings highlight multiple, intersecting barriers to routine longitudinal care for cSLE in South Africa and suggest there might be a group of diagnosed children who don’t receive follow-up care and are subject to loss to follow-up. cSLE requires ongoing treatment and care; thus, the different barriers may interact and compound over time with each follow-up visit. South African cSLE patients are at high risk for poor outcomes. South African care teams should work to overcome these barriers and place attention on the facilitators to improve care retention for these patients and create a model for other less resourced settings.
Similar content being viewed by others
Background
Systemic lupus erythematosus (SLE) is a life-threatening, chronic, autoimmune disease that manifests through multisystem episodic inflammation and causes severe morbidity and early mortality. Accordingly, SLE requires long term subspecialty care due to its complex and chronic nature [1, 2]. Worldwide, rheumatic diseases like SLE are understudied despite being the second leading cause of disability adjusted life years, as measured by years lost to disability [3]. Genetic predisposition coupled with healthcare disparities in medically underserved areas may worsen SLE outcomes [4]. In high-income countries, individuals of African descent experience SLE at a higher rate and have more severe symptoms and worse outcomes [5]. Childhood-onset SLE (cSLE) is more severe than adult-onset SLE, as children have higher disease activity, require more medications, and accrue more damage than adult counterparts [6]. Therefore, it is critical to promptly diagnose, treat, and manage cSLE. cSLE is a chronic disease with no cure and requires routine follow-up visits for disease monitoring and management. Managing cSLE is optimized with a multidisciplinary team to oversee clinical management in order to educate families about prevention of disease flares which can lead to irreversible damage, address concerns about reproductive health, encourage medication adherence, acknowledge the mental health burden of chronic illness, and ease the transition to medical care upon adulthood [6]. Early recognition and ongoing access to care and care retention may impact outcomes, preventing progression and complications [6].
In a recent study with participation from 44 African countries, 12 countries have between one and ten rheumatologists while 17 have no rheumatologists; the majority of rheumatologists are in Northern Africa [7]. South Africa is a lower-middle income country that is a leader in health care for Africa, yet the health system still has significant challenges and disparities. Despite the increasing burden of chronic diseases in South Africa, little is known about the barriers to accessing and utilizing health care for pediatric chronic conditions. South Africa is burdened with poverty, communicable diseases such as tuberculosis and human immunodeficiency virus (HIV), malnutrition, racial tension and community violence [8]. South Africa is still dealing with repercussions of its apartheid history and subsequent entrenched far-reaching disparities [9]. Ongoing health care delivery to patients with chronic disease requires coordination of most aspects of the medical systems: health financing, governance, health workforce, health information, medical products and technologies, and health-service delivery [10].
In South Africa, cSLE is characterized by patients who have more active disease, serious organ system involvement, and worse outcomes than North American peers [11, 12]. Previously, our team demonstrated that there are many barriers to diagnosing cSLE in South Africa. Among patients currently receiving care for cSLE, they face challenges at the level of cSLE caregivers (lack of knowledge about SLE, financial difficulties, social stigma of SLE) and the health system (misdiagnosis, lack of trained staff, a complex medicine systems) [13]. Continued long term medical care is essential for cSLE maintenance, as lapses in care are often linked to disease flares [14]. The barriers to receiving sustained medical care in this population have not been explored, and it is not known how they differ from the barriers experienced in receiving an initial diagnosis. The purpose of this study is to describe caregivers’ experiences engaging in long term medical care for cSLE, and to identify barriers and facilitators to long term care continuity and retention among cSLE patients. This study utilizes a qualitative approach to understand the experience of managing cSLE in the context of the South African healthcare system.
Methods
Setting
Participants were recruited through pediatric and adult rheumatology clinics at two government-funded tertiary hospitals (Red Cross War Memorial Children’s Hospital and Groote Schuur Hospital) and a private practice clinic in Cape Town, South Africa.
Participant recruitment
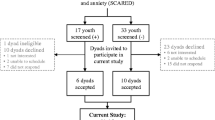
Family caregivers were considered eligible for recruitment if they cared for youth (< 19 years) who were diagnosed with cSLE and satisfied at least four of the eleven ACR SLE classification criteria. Out of the potential caregivers for the 72 patients identified across the three centers, we attempted to contact each family unit to identify a named contact for study participation. Thirty were contacted successfully in-person, by phone, or by email. Of the 30 contacted, 22 cSLE caregivers enrolled in the study and completed an interview.
Ethical review
The study was approved by the Duke Institutional Review Board (#Pro00045133) and University of Cape Town Human Research Ethics Committee (#424/2013). Participants completed written informed consent in their preferred language prior to the interview.
Procedures
Individual, in-depth, semi-structured interviews were conducted between January 2014 and December 2014. The interview guide was developed based on a literature review on specific hurdles embedded in the South African medical system and challenges in managing cSLE. The guide included open-ended questions and follow-up probes about the barriers to and facilitators of ongoing long–term care for cSLE ( Supplement 1). Participants were offered the flexibility of having the interview conducted at home (n = 3) or at the clinic attended (n = 19) to minimize the burden of travel. Interviews were conducted by author LBL and lasted 30 to 90 min. Interviews were conducted in the primary language of participants (English [n = 16]; Afrikaans [n = 3]; Xhosa [n = 3]). Non-English interviews required a linguistically and culturally competent translator who provided real-time, simultaneous translation.
Self-described participants were requested to report how they self-identify (racially/ethnically) with categories based on those in South African population surveys [15].
Analysis
The interviews were audio-recorded and transcribed verbatim. They were analyzed using applied thematic analysis to identify recurring themes related to barriers to and facilitators of chronic care management perceived by caregivers of cSLE patients [16]. Major themes were reviewed by two coders to reach consensus, and analytic memos were written to organize the content of the interviews and incorporate relevant quotes. The memos were manually coded for primary thematic categories related to chronic care retention barriers and facilitators at the levels of the patient and/or health system.
Results
There were 22 cSLE caregivers in the sample: 18 mothers, 2 fathers, 1 grandmother, and 1 foster mother. In all cases, the race/ethnicity of the caregiver was consistent with that of the child. Descriptive characteristics, such as age, household income, means of transportation, and education level, are described in Table 1. Although 36% of South Africans live below the poverty line (R620/$43 USD per month), none of the caregivers reported monthly household incomes below this threshold [17, 18]. The majority of caregivers (59%) received government social welfare grants (R450/$29 USD per month), and would likely live below the poverty line without the grants [19]. 18% of caregivers reported living without running water or electricity.
Barriers
Four barriers to engagement and retention in cSLE were identified (Table 2). Three barriers were at the level of the caregiver (knowledge gap, financial burdens, and social stigma of SLE) and one barrier was at the level of the health system (complexity of the South African medical system).
Caregiver knowledge gap
Most caregivers expressed little to no prior knowledge of SLE. Subsequently, caregivers were unable to distinguish SLE symptoms from other illnesses, and severe symptoms from typical ones. Upon receiving the diagnosis of cSLE, many caregivers still reported confusion over diagnosis and were unable to comprehend the disease itself, much less be able to define it for others. One caregiver conveyed that “[if someone asks what lupus is], I just only told them when she had the first bad problem, then I couldn’t explain it. I can’t really explain it.” In addition to the lack of understanding of cSLE at diagnosis, there was a knowledge gap in chronic care management of SLE. For example, many caregivers did not understand that the medications for SLE are not only to be used to improve symptoms during a flare, but also to maintain disease control and to prevent flare, and need to be taken even when the patient feels well. Additionally, many caregivers did not realize that severe damage that occurs prior to proper treatment cannot always be reversed, even with optimal therapeutics.
Furthermore, the caregivers did not always envision themselves as partners of the healthcare team in managing cSLE over time. Patient-centered care and shared decision making are increasingly recognized as pillars of quality healthcare. Shared decision making can empower patients and families to take an active role in their care [20]. There has been a slower adoption of these practices in low- and middle-income countries (LMIC) settings [21]. Yet, there is a hidden burden on caregivers to manage cSLE, transferring most of the effort from the health system and providers to caregivers who lack knowledge, experience, and resources.
Financial burden of care
The financial burden of cSLE longitudinal management was the most frequently cited issue. There is an economic burden associated with a chronic illness like SLE. The burden includes specific treatment costs, transportation, and caregiver loss of productivity/income [22]. Caregivers who were above the poverty line pay medical bills for hospitalization on an income-based level, and many were on a payment plan for bills from initial diagnosis. Accessing sick leave for chronic illness management for their child was identified as a barrier by many caregivers. Although missing work once for the initial illness was viewed by employers as justifiable, missed work accumulated with repeated follow-up visits, and there is less awareness of chronic illness in childhood. Most caregivers reported insufficient sick leave to cover appointments at 2-to-3-month intervals. Some caregivers reported disappointment that their supervisors did not understand that the caretaker’s child’s health issues required critical follow-up visits and thus did not understand why these visits took priority over work. Transportation costs were also a financial burden, as the majority of caregivers did not have access to private transportation and had to rely on public transportation. They had to pay to get to and from the medical facility, and the high transportation costs accumulated over time and were a burden on tenuous family finances. The time it took to commute to the clinic was great and costly. One caregiver stated that “we come to clinic every two weeks in a taxi…it takes 1 hour…last week [we didn’t have taxi fare], so we walked. [The walk] took three hours.” The ongoing new costs due to time away from work at any visit and the costs of transportation to clinic compound the already often lingering high costs of previous outpatient visits to these and other specialists and bills form the initial hospitalization.
Social stigma of cSLE
While caregivers themselves had limited knowledge of cSLE, the caregivers reported that the general public appears to hold negative misconceptions about SLE. Caregivers feel the effects of this stigma, reporting that people outside their family unit, such as neighbors and school community members, believe that cSLE is contagious, when in reality “it’s only in [one’s] joints…[and] not contagious for somebody else to get.” Many caregivers cited that they felt like they had to hide their child’s condition from the community out of fear of lasting social stigmatization. This stigma is a barrier to longitudinal care. Taking a child out of school for care may call attention to the cSLE diagnosis. If caregivers feel stigma about the illness, they are motivated to reduce actions which make the diagnosis more visible.
Complexity of medical system
Complexity of the medical system emerged as a barrier to continuing care. Sustained follow-up care is at the core of diagnosis and treatment of chronic disease without a cure like cSLE and requires multiple visits that are often difficult to navigate and access. cSLE patients may require multiple visits from other specialists, such as hematologists and nephrologists, which add to the care coordination obstacles. The time and transportation costs noted above were multiplied if the family has to make a visit to two different specialists on different days of the week. The medical team did not always fully communicate well the plan during disease maintenance and disease flares, which at times could lead to confusion and affect compliance.
Facilitators
While barriers to continuing to manage care for SLE were identified in this study, themes around factors which greatly facilitated chronic care emerged as well (Table 3). Three themes emerged for facilitators in chronic care of cSLE, all of which directly related to the caregiver level (patient and caregiver education, robust support system for the caregiver, and financial support for the caregiver and patient).
Patient and caregiver education
Good communication and continued education by the pediatric rheumatologist were noted as facilitators to receiving ongoing care for cSLE. This was accomplished if the doctor thoroughly answered any questions and equipped the caregiver with informational tools. One caregiver expressed that “Dr. – was excellent…he could tell us what was wrong with [our daughter] …He gave us brochures and stuff as well.” Another said, “I think I’ve been well informed, and I ask questions every time.” The lack of caregiver knowledge on cSLE and chronic care management that was described as a barrier above had been reduced in some families through consistent and targeted education of caregivers. This education enabled caregivers to understand the importance of ongoing visits for chronic disease and helped them provide optimal care between appointments for their child. Caregivers also reported that their children with SLE also benefited when they were aware of their own condition and had enough background knowledge to ask relevant questions.
Social support system for caregiver
When caregivers were surrounded with a robust social support system, the barriers to caring for a child with cSLE were lessened. The support tended to come mainly from the parents of the caregiver and fulfilled every aspect of a solid support system, as one caregiver said that without “[having] to ask, [my parents] are always there for me.” Another caregiver was grateful that “my mother [gives me support.] If I can’t get off work, she will look after [my daughter when she is sick.].” In some cases, the caregiver’s employer was part of the support system if they provided work flexibility; as one parent summarized, her employer was “very understanding and supportive.”
Financial support for caregiver and patient
The financial burden of missing work (therefore going without pay) as well as the expenses involved in hospital bills and transportation costs that accumulate with every follow-up visit are significant challenges. Support stems from “employers who have understood. So now when [my child] wasn’t feeling well I could stay at home and work from home. Also, when she was ill, I had a full-time job and they allowed me to stay out for the month she was ill.” Additional cited ways to lessen the financial burden on caregivers and patients extend beyond the workplace and into the realm of more convenient and less costly transportation to and from appointments. By providing financial support for the caregiver and the patient, this major barrier may be alleviated.
Discussion
Childhood-onset SLE is a chronic condition, and consistent longitudinal care is necessary to keep the disease in remission and prevent long term damage. cSLE patients in South Africa often have very active disease and poor long-term prognosis [11, 12]. The chronic nature of cSLE coupled with its multifaceted progression mandates that it is treated consistently and responsively, underlining the importance of the caregiver’s role in managing their child’s condition. It is therefore critical to retain diagnosed patients in care to keep disease in remission and prevent inflammation and subsequent organ damage.
Our prior study highlighted missed opportunities for timely diagnosis of cSLE in South Africa, identifying the following barriers: (1) Knowledge gap regarding SLE; (2) Financial difficulties; (3) Social stigma of SLE; (4) Lack of trained staff; (5) Complex medical system; and (6) Misdiagnosis. In this study, similar themes related to barriers to care retention for South African cSLE patients were noted. These findings imply that just as there might be a population of children who never receive diagnosis for cSLE, there might be a subset of diagnosed children who don’t receive follow-up care and are subject to loss to follow-up [13].
In the US, Canada, and Europe, access to care for chronic conditions is relatively easier to attain [23,24,25]. In contrast, most low- and middle-income countries have historically prioritized infectious diseases and trauma, and have fewer medical professionals trained in managing pediatric rheumatic disease, as well as lack of access to proper testing and equipment for ongoing disease monitoring [26, 27]. Many infectious disease symptoms overlap with rheumatic disease such as inflammation and fever, making differentiation difficult. South Africa is unique because it has created infrastructure for the increasing number of chronic conditions, partly due to the gradual introduction of HIV/AIDS care over the past few decades and shift from episodic treatment to life-long care [28].
The two financial burdens of travel and caregiver-missed work was identified as the greatest barrier to ongoing cSLE care in this setting. Most of the patient caregivers were receiving social grants which supported inadequate household income, suggesting some degree of financial instability. Continued missed work or use of sick leave could threaten employment, and subsequently the financial situation of the entire family. Most cSLE patients will need to travel to clinic for SLE management every one to three months. If an employer is unfamiliar with SLE or chronic disease management, caregivers may be penalized or terminated for continuing to miss working days. In a study of adult patients in South Africa, unskilled workers and domestic employees faced the largest barriers to sick leave for chronic disease management [29].
Both hospital bills and the hidden costs of chronic care (taxi/transportation fare and missed work) compound at each follow-up visit, increasing the burden on the caregiver. Many caregivers reported they are without access to running water or electricity and this suggests that patients with lower socioeconomic status can be vulnerable to opting out of ongoing care due to high cost [9]. Structural racism contributes to adverse health outcomes through a variety of avenues, and racism is associated with poor physical health. The patients and caregivers in our cohort were primarily Black or of admixed ancestry, and therefore, likely affected by the impact of structural racism [30, 31]. The majority of caregivers didn’t have access to private transportation, and subsequently had to rely on minibus taxis, which are public and the least expensive yet most dangerous mode of transportation in Cape Town [32]. The financial barriers to cSLE care retention affect minority groups at a greater rate, partially explaining racial discrepancies in symptom severity and care received [5].
The complexity of the South African medical system was a barrier to timely SLE diagnosis and continues to impede ongoing care for SLE [10]. In this study, the complexity of care was more dependent on multiple subspecialists involved in the care of cSLE. For some patients, they may see multiple providers from different subspecialties, which often hold clinic on different days. Over time, providers can aim to decrease the burden of separate subspecialty visits by adding social workers or team members to appointments where the Rheumatology, although coordination of these teams in resource-limited settings remains a challenge.
The lack of caregiver knowledge about cSLE is another barrier to continuing cSLE care. This knowledge barrier is not unique to SLE but is characteristic of many chronic diseases like diabetes and HIV/AIDS, which are widespread in South Africa [33, 34]. In a study on diabetes in South Africa, the confusion over diabetes and its management is a reflection of poor access to healthcare, mistrust of that healthcare system, and/or little to no perceived social support [33]. There are few pediatric rheumatology providers in sub-Saharan Africa, limited to major urban centers. Lack of understanding about disease, mechanism and prognosis may lead to misperception about the importance of ongoing clinic visits for disease control, and subsequent disease activity and damage [35]. In other places in sub-Saharan Africa, there is varied understanding of the severity and subtypes of pediatric rheumatic disease leading to frustration among providers, patients, and their families [36]. The limited knowledge of the diagnoses and management of chronic rheumatic diseases in general practitioners led to addressing the more urgent challenge of managing pain control rather than conclusively working towards diagnosis and treatment, resulting in delays and lack of a definitive diagnosis.
cSLE is a relatively rare condition, and there is little public awareness which can lead to social stigmatization [37]. A disease typically becomes stigmatized if it is progressive and incurable, not well understood among the public, and presents symptoms that can’t be concealed [38]. Often, there is stigma associated with a sick child [26]. The stigma of a child with chronic disease may be more heightened than that of a chronically-ill adult, because the image disrupts expectations of a proper society with healthy children who are occasionally, if at all, susceptible to short-term illnesses and not ones conventionally viewed as byproducts of aging [39]. Some of the symptoms of cSLE, like alopecia and malar rash, can’t be easily masked, and may instill fear in uninformed individuals of contagion and easy transmission [40]. To protect their child from stigma, caregivers may isolate their family from a larger social network, which ultimately may result in lack of necessary support to continue to access care [41]. Caregivers may attempt to conceal the signs of illness, which may include frequent visits to clinic or hospital. Lapsed visits may contribute to inadequate treatment and less contact with the pediatric rheumatologist may further deepen the knowledge barrier. Strained relationships may emerge, and patients sometimes react by noncompliance to treatments and nonadherence to medications [40, 42]. The cumulative impact of social stigma is that cSLE patients with poor disease control are likely to have higher rates of depression, particularly those with lower education backgrounds [43]. The mental health comorbidities of cSLE further impedes patients from optimally managing cSLE [44].
We identified three primary facilitators for cSLE patient retention: education, financial support, and development of a robust social support system for patients and caregivers [13]. The possible solutions for each barrier are informed by other chronic disease models [33, 45,46,47]. Creating robust, local support systems through caregiver networks and support groups may improve chronic care return rates for cSLE patients in South Africa. To reduce the complexity of chronic care and the added burden of multi-specialty care, patient navigators have been used in other health systems to improve care retention in SLE [48]. Financial support in the form of transportation, flexible shifts, and monetary contributions, for example, are extensions of social support and filling in the present needs of a household managing cSLE. In addition to financial systems to ease the burden of transportation costs, innovative solutions to ongoing care could be considered in this setting. The use of health tools such as patient education texts could improve patient and caregiver health literacy. Alternating in-person visits with phone or telehealth visits could reduce the burden of missed days on the family and improve the patient and caregiver connection. The recent global COVID-19 pandemic has increased the infrastructure for telehealth in SLE clinics, and this may have long-term benefits to reduce time and travel costs for some cSLE caregivers [49,50,51,52]. Adaptations for the virtual format are underway, such as the virtual pediatric gait, arms, legs, spine screening examination is a component of a global telemedicine initiative [53]. Those families who lack access to internet services will continue to struggle with health care access.
Beyond direct financial support, support systems also include support groups, which have been proven to improve clinical as social outcomes, as peers are often perceived as more approachable and accessible that medical providers [47]. Online support groups, such as WhatsApp group chats, are very promising in the current technology-driven world and can reduce the gap between clinical and at-home care [54]. Similarly, other interventions that can be conducted by both medical and non-medical professionals, such as disease education and prevention programs, pain management strategies, school support, transition and career planning, family counseling, and psychotherapy, can be broadly designed so that they are personalized for the patient for maximal benefit [43]. The cumulative impact of support groups is the reduction of the knowledge gap in cSLE among caregivers, patients, and hopefully even extending to the public. Improving family education at diagnosis and follow-up visits may increase patient-physician trust, empower patients and caregivers, and motivate them to return for care.
This study has several limitations. Although the data utilized in this study is from 2014, nearly a decade prior, there have not been any interim studies regarding this subject matter. Further, the situation for such patients in South Africa has been worsened by the COVID-19 pandemic, which has exacerbated the existent barriers to assessing and maintaining healthcare care for people with disabilities including chronic health conditions [55]. More recent studies have demonstrated the economic and social repercussions of COVID-19 on healthcare retention among HIV patients [56]. Another limitation was posed by selection bias influencing the sample of caregivers, as those interviewed had been able to overcome barriers to attending follow-up visits. We were not able to capture the insights of caregivers for patients that had been diagnosed but lost to follow-up or those that were not diagnosed at all—these two subsets might have experienced different barriers which prevented them from coming back. Therefore, the barriers and facilitators described in this paper stem from a group of caregivers who have demonstrated resilience and had access to resources that enabled their children to receive long-term subspecialized cSLE care with optimal continuity of care. While some of the caregivers were below the poverty line, they received support via government social grants, which likely contributed to their successful retention. Additionally, the interviews were conducted in an urban setting at two government centers and one private practice, possibly creating selection bias. However, the likelihood of representative sampling was increased: 80% of South Africans use public health care [57], and the only cSLE providers in the region were located at these institutions.
Solutions to implement in the future should be grounded in the themes identified in the caregiver interviews (Tables 2 and 3). Since financial barriers were the most cited, transportation or transport subsidies arranged by employers would reduce the hassle of attending appointments, decreasing travel time, and thus reducing the amount of time away from work. A standardized letter written by the SLE care team to caregiver employers could be given to new patients and caregivers. The letter would explain that the caregiver has a child/dependent with cSLE and the crucial importance of the child and caregiver attending rheumatology clinic every 1–2 months. Such communication could minimize the unknown and confusing aspects of this disease and hopefully allow caregivers to better attend routine care at cSLE clinic appointments. SLE support groups would additionally improve caregiver and patient knowledge so they are empowered to return for care, and individuals that are part of their extended social network could be invited to attend, reducing social stigma and misconceptions surrounding cSLE. Clinic-based education sessions could complement caregiver or patient-led support groups to improve knowledge about SLE diagnosis and chronic management. Online support groups and educational materials are another format to be considered, although these may not be accessible for low-income families. Cohort monitoring could identify patients who have not returned to clinic, and patient- and family-centered interventions could be designed to optimize continued contact with the patient while minimizing the burden of travel and missed work on caregivers. Patient navigators are trained to help patients overcome modifiable barriers to health care and can improve care of chronic conditions. Navigators may be nurses, social workers, or lay health workers, including peers. Navigators trained in SLE may be a cost-effective way to retain families in care and reduce significant morbidity and mortality of cSLE.
Conclusion
The management of a chronic yet life-threatening pediatric disease such as cSLE is a worldwide challenge. South African cSLE patients are at high risk for poor outcomes; therefore, identifying barriers and facilitators to ongoing care is important. This work highlights challenges to patients and caregivers for cSLE patients to continued care in clinic. South African care teams can work to implement changes, such as consolidating multidisciplinary care, creating virtual/WhatsApp patient support groups, and connecting families to social services to improve care retention for these patients and create a model for other less resourced chronic disease care settings.
Data availability
The datasets generated during and analyzed during the current study are not publicly available, as the primary data consists of semi-structured interviews and contains information that could compromise the privacy of study participants. This data can be made available in part or full from the corresponding author (LBL) on reasonable request with proper privacy protection.
Abbreviations
- SLE:
-
Systemic lupus erythematosus
- cSLE:
-
Childhood-onset SLE
References
Livingston B, Bonner A, Pope J. Differences in clinical manifestations between childhood-onset lupus and adult-onset lupus: a meta-analysis. Lupus. 2011;20(13):1345–55.
Bilsborrow JB, Peláez-Ballestas I, Pons-Estel B, Scott C, Tian X, Alarcon GS, et al. Global Rheumatology Research: Frontiers, challenges, and opportunities. Hoboken, NJ: Arthritis & rheumatology; 2021.
Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the global burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):968–74.
Fernández M, Alarcón GS, Calvo-alén J, Andrade R, McGwin G Jr., Vilá LM, et al. A multiethnic, multicenter cohort of patients with systemic lupus erythematosus (SLE) as a model for the study of ethnic disparities in SLE. Arthritis Care Res. 2007;57(4):576–84.
Uribe AG, Alarcón GS. Ethnic disparities in patients with systemic lupus erythematosus. Curr Rheumatol Rep. 2003;5(5):364–9.
Ardoin SP, Schanberg LE. The management of pediatric systemic lupus erythematosus. Nat Clin Pract Rheumatol. 2005;1(2):82–92.
Dey D, Paruk F, Mody GM, Kalla AA, Adebajo A, Akpabio A, et al. Women in rheumatology in Africa. Lancet Rheumatol. 2022;4(10):e657–60.
Mayosi BM, Benatar SR. Health and Health Care in South Africa — 20 years after Mandela. N Engl J Med. 2014;371(14):1344–53.
Lewandowski LB, Scott C. Apartheid and healthcare access for paediatric systemic lupus erythematosus patients in South Africa. South Afr J Child Health. 2015;9:36–7.
Samb B, Desai N, Nishtar S, Mendis S, Bekedam H, Wright A, et al. Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. Lancet. 2010;376(9754):1785–97.
Lewandowski LB, Schanberg LE, Thielman N, Phuti A, Kalla AA, Okpechi I, et al. Severe disease presentation and poor outcomes among pediatric systemic lupus erythematosus patients in South Africa. Lupus. 2016;26(2):186–94.
Harrison MJ, Zühlke LJ, Lewandowski LB, Scott C. Pediatric systemic lupus erythematosus patients in South Africa have high prevalence and severity of cardiac and vascular manifestations. Pediatr Rheumatol Online J. 2019;17(1):76.
Lewandowski LB, Watt MH, Schanberg LE, Thielman NM, Scott C. Missed opportunities for timely diagnosis of pediatric lupus in South Africa: a qualitative study. Pediatr Rheumatol. 2017;15(1):14.
Brunner HI, Huggins J, Klein-Gitelman MS. Pediatric SLE—towards a comprehensive management plan. Nat Rev Rheumatol. 2011;7(4):225.
Stats S. Statistics South Africa. Formal census. 2011.
Guest G, MacQueen KM, Namey EE. Validity and reliability (credibility and dependability) in qualitative research and data analysis. Applied thematic analysis London: Sage; 2012. pp. 79–106.
Africa SS. Poverty trends in South Africa: an examination of absolute poverty between 2006 and 2011. Statistics South Africa Pretoria; 2014.
Lehohla P. Use of health facilities and levels of selected health conditions in South Africa: findings from the General Household Survey, 2011. Statistics South Africa Pretoria; 2013.
South Africa: South African Government. 2014 [ https://www.gov.za/services/child-care-social-benefits/child-support-grant.
Qu H, Shewchuk RM, Alarcón G, Fraenkel L, Leong A, Dall’Era M, et al. Mapping perceptions of Lupus Medication decision-making facilitators: the importance of patient context. Arthritis Care Res. 2016;68(12):1787–94.
De Man J, Mayega RW, Sarkar N, Waweru E, Leys M, Van Olmen J et al. Patient-centered care and people-centered health systems in sub-Saharan Africa: Why so little of something so badly needed? 2016.
Zhu TY, Tam LS, Li EK. Cost-of-illness studies in systemic lupus erythematosus: a systematic review. Arthritis Care Res. 2011;63(5):751–60.
Stellefson M, Dipnarine K, Stopka C. Peer reviewed: the chronic care model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis. 2013;10.
Ronksley PE, Sanmartin C, Campbell DJT, Weaver RG, Allan GM, McBrien KA, et al. Perceived barriers to primary care among western canadians with chronic conditions. Health Rep. 2014;25:3.
Busse R, Organization WH, Blümel M. Systems EOoH, policies. Tackling Chronic Disease in Europe: strategies. Interventions and Challenges: World Health Organization; 2010.
de-Graft Aikins A, Unwin N, Agyemang C, Allotey P, Campbell C, Arhinful D. Tackling Africa’s chronic disease burden: from the local to the global. Global Health. 2010;6:5.
Lewandowski LB. Tackling global challenges in pediatric rheumatology. Curr Opin Rheumatol. 2020;32(5):414–20.
Bisson GP, Stringer JSA. Lost but not forgotten—the Economics of improving patient Retention in AIDS Treatment Programs. PLoS Med. 2009;6(10):e1000174.
Magadzire BP, Mathole T, Ward K. Reasons for missed appointments linked to a public-sector intervention targeting patients with stable chronic conditions in South Africa: results from in-depth interviews and a retrospective review of medical records. BMC Fam Pract. 2017;18(1):1–10.
Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–63.
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS ONE. 2015;10(9):e0138511.
Norman R, Matzopoulos R, Groenewald P, Bradshaw D. The high burden of injuries in South Africa/Forte charge de morbidite due aux traumatismes en Afrique Du Sud/La Gran carga de lesiones en Sudafrica. Bull World Health Organ. 2007 2007/09//:695+.
Mendenhall E, Norris SA. Diabetes care among urban women in Soweto, South Africa: a qualitative study. BMC Public Health. 2015;15(1):1300.
Peltzer K, Matseke G, Mzolo T, Majaja M. Determinants of knowledge of HIV status in South Africa: results from a population-based HIV survey. BMC Public Health. 2009;9(1):174.
Tsang-A-Sjoe MW, Bultink IE, Heslinga M, Voskuyl AE. Both prolonged remission and Lupus Low Disease Activity State are associated with reduced damage accrual in systemic lupus erythematosus. Rheumatology. 2016:kew377.
Migowa A, Bernatsky S, Ngugi AK, Foster HE, Muriuki P, Riang’a RM, et al. Bridging gaps: a qualitative inquiry on improving paediatric rheumatology care among healthcare workers in Kenya. Pediatr Rheumatol. 2023;21(1):144.
Smith EM, Ainsworth S, Beresford MW, Buys V, Costello W, Egert Y, et al. Establishing an international awareness day for paediatric rheumatic diseases: reflections from the inaugural World Young Rheumatic diseases (WORD) day 2019. Pediatr Rheumatol. 2020;18(1):1–6.
Gilbert L, Walker L. ‘My biggest fear was that people would reject me once they knew my status… stigma as experienced by patients in an HIV/AIDS clinic in Johannesburg, South Africa. Health & Social Care in the Community. 2010;18(2):139 – 46.
Campbell C, Foulis CA, Maimane S, Sibiya Z. I have an evil child at my House: Stigma and HIV/AIDS management in a South African Community. Am J Public Health. 2005;95(5):808–15.
Aggarwal A, Srivastava P. Childhood onset systemic lupus erythematosus: how is it different from adult SLE? Int J Rheum Dis. 2015;18(2):182–91.
Brennan KA, Creaven A-M. Living with invisible illness: social support experiences of individuals with systemic lupus erythematosus. Qual Life Res. 2016;25(5):1227–35.
McGrady ME, Hommel KA. Medication Adherence and Health Care Utilization in Pediatric Chronic illness: a systematic review. Pediatrics. 2013;132(4):730.
Knight A, Weiss P, Morales K, Gerdes M, Rearson M, Vickery M, et al. Identifying differences in risk factors for depression and anxiety in Pediatric Chronic Disease: a matched cross-sectional study of youth with Lupus/Mixed connective tissue Disease and their peers with diabetes. J Pediatr. 2015;167(6):1397–e4031.
Chang JC, Davis AM, Klein-Gitelman MS, Cidav Z, Mandell DS, Knight AM. Impact of Psychiatric diagnosis and treatment on Medication Adherence in Youth with systemic Lupus Erythematosus. Arthritis Care Res. 2021;73(1):30–8.
Ku GMV, Kegels G. Adapting chronic care models for diabetes care delivery in low-and-middle-income countries: a review. World J Diabetes. 2015;6(4):566–75.
Coleman K, Mattke S, Perrault PJ, Wagner EH. Untangling practice redesign from Disease Management: how do we best care for the chronically ill? Annu Rev Public Health. 2009;30(1):385–408.
Rachlis B, Naanyu V, Wachira J, Genberg B, Koech B, Kamene R, et al. Identifying common barriers and facilitators to linkage and retention in chronic disease care in western Kenya. BMC Public Health. 2016;16(1):741.
Feldman CH, Bermas BL, Zibit M, Fraser P, Todd DJ, Fortin PR, et al. Designing an intervention for women with systemic lupus erythematosus from medically underserved areas to improve care: a qualitative study. Lupus. 2013;22(1):52–62.
Migowa A, Bernatsky S, Ngugi A, Foster HE, Muriuki P, Lusambili A, et al. An iceberg I can’t handle: a qualitative inquiry on perceptions towards paediatric rheumatology among healthcare workers in Kenya. Pediatr Rheumatol. 2023;21(1):6.
Makhlouf Y, Nessib DB, Ferjani H, Triki W, Maatallah K, Dhia K. The concept of telemedicine in pediatric rheumatology in Tunisia: parents’ perceptions. J Pediatr Nurs. 2023;69:6–9.
Migowa AN, Hadef D, Hamdi W, Mwizerwa O, Ngandeu M, Taha Y, et al. Pediatric rheumatology in Africa: thriving amidst challenges. Pediatr Rheumatol. 2021;19(1):69.
Lewandowski LB, Hsieh E. Global rheumatology in the time of COVID-19. Lancet Rheumatol. 2020;2(5):e254–5.
Shenoi S, Hayward K, Curran ML, Kessler E, Mehta JJ, Riebschleger MP, et al. Telemedicine in pediatric rheumatology: this is the time for the community to embrace a new way of clinical practice. Pediatr Rheumatol. 2020;18(1):1–4.
Barak A, Boniel-Nissim M, Suler J. Fostering empowerment in online support groups. Comput Hum Behav. 2008;24(5):1867–83.
McKinney EL, McKinney V, Swartz L. Access to healthcare for people with disabilities in South Africa: bad at any time, worse during COVID-19? South Afr Family Pract. 2021;63(3).
Jardim CGR, Zamani R, Akrami M. Evaluating the impact of the COVID-19 pandemic on accessing HIV services in South Africa: a systematic review. Int J Environ Res Public Health. 2022;19(19):11899.
Al-Mutairi KD, Al-Zahrani MS, Bahlas SM, Kayal RA, Zawawi KH. Periodontal findings in systemic lupus erythematosus patients and healthy controls. Saudi Med J. 2015;36(4):463.
Acknowledgements
We would like to thank all the lupus patients and their caregivers and families for their contributions to this study. We would like to acknowledge the research team at Red Cross War Memorial Children’s Hospital, including Dr. Kate Webb, Dr. Lawrence Okongo’o, Dr. Nicola Brice, Sr. Angel Phuti, Sr. Dorothy Brown, Sr. Caroline, and Zodwa Sam.
Funding
LBL was funded by the Intramural Research Program at NIAMS, the Lupus Foundation of America Early Career Award, a training grant at Duke University (T32 AI0007217), a Duke Global Health Institute Fieldwork grant, and the Fogarty International Center (NIH R25TW009337).
Open access funding provided by the National Institutes of Health
Author information
Authors and Affiliations
Contributions
LBL collected, analyzed, and interpreted the data. MHW supported the analysis and interpretation of the data. NI interpreted themes and codes. All authors were involved in study concept and design, drafting the article, or revising it critically for important intellectual content. All authors read and approved the final version to be submitted for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Duke Institutional Review Board (#Pro00045133) and University of Cape Town Human Research Ethics Committee (#424/2013).
Consent for publication
Written informed consent was obtained in the participant’s preferred language prior to the interview.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
*The racial groups on the South African census are Black African, White, Admixed, Indian/Asian, or Other. (S.S. Africa Census 2011: Community Profile Databases Statistics South Africa, Pretoria (2012))
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ikram, N., Lewandowski, L.B., Watt, M.H. et al. Barriers and facilitators to medical care retention for pediatric systemic lupus erythematosus in South Africa: a qualitative study. Pediatr Rheumatol 22, 59 (2024). https://doi.org/10.1186/s12969-024-00994-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12969-024-00994-0