Abstract
Background
Little is known about the disposition to autoimmune diseases (ADs) among children diagnosed with JIA. In this study, we provide a comprehensive overview of the prevalence of and factors associated with ADs in parents of children with juvenile idiopathic arthritis (JIA).
Methods
Prevalence rates of ADs and 95% Poisson confidence intervals were calculated for parents of JIA patients from the international Pharmachild registry and compared with general population prevalence rates as reported in the literature. Demographic, clinical and laboratory features were compared between JIA patients with and without a family history of AD using χ2 and Mann-Whitney U tests.
Results
Eight thousand six hundred seventy three patients were included and the most common familial ADs were psoriasis, autoimmune thyroid disease, rheumatoid arthritis and ankylosing spondylitis. The prevalence of several ADs was higher in parents of the included JIA patients than in the general population. Clinical Juvenile Arthritis Disease Activity Scores at study entry and last follow-up were not significantly different between patients with (n = 1231) and without a family history of AD (n = 7442). Factors associated with familial AD were older age at JIA onset (P < 0.01), Scandinavian residence (P < 0.01), enthesitis-related arthritis, psoriatic arthritis and undifferentiated arthritis (P < 0.01), ANA positivity (P = 0.03) and HLA-B27 positivity (P < 0.01).
Conclusions
Familial AD proves to be a risk factor for JIA development and certain diseases should therefore not be overlooked during family health history at the diagnosis stage. A family history of AD is associated with the JIA category but does not influence the severity or disease course.
Similar content being viewed by others
Background
Juvenile idiopathic arthritis (JIA) is an umbrella term that comprises seven subtypes of arthritis of unknown cause that begin before the age of 16 years and last for more than 6 weeks [1]. Six out of seven subtypes are considered an autoimmune disease (AD), except for systemic JIA, which resembles more an autoinflammatory disease [1]. ADs are known to cluster within families and share common pathogenic mechanisms and genetic factors [2, 3]. However, little is known about the relationship between JIA and familial ADs. A previous study reported that 32% of 4677 JIA patients had at least one first-degree relative with an AD [4]. Furthermore, JIA patients with a family history of AD were reported to have higher disease activity and more often enthesitis-related arthritis (ERA) and psoriatic arthritis than JIA patients without such family history [5, 6]. Frequently described ADs in relatives of JIA patients are insulin-dependent diabetes mellitus (IDDM), JIA, rheumatoid arthritis (RA), autoimmune thyroid disease (AITD), spondyloarthropathy and psoriasis [4,5,6,7,8,9,10,11]. Nonetheless, the few studies about familial autoimmunity in JIA are either based on a limited number of patients, do not report prevalence rates within families or only report pre-selected ADs.
The objective of this study is to provide a comprehensive overview of the occurrence of and factors associated with ADs in parents of children with JIA from a large international registry [12] and to compare prevalence rates with those reported in the general population.
Methods
Patients
Patients were included from the international observational Pharmachild registry. Pharmachild started in 2011 with the objective of studying safety and effectiveness of drug therapies in JIA. Patients are included from Paediatric Rheumatology International Trials Organisation (PRINTO) centers from 31 countries worldwide. The registry includes patients with a diagnosis of JIA as per International League of Associations for Rheumatology (ILAR) criteria that are being treated with nonsteroidal anti-inflammatory drugs (NSAIDs), intraarticular steroids, systemic steroids, and/or conventional synthetic (cs-) or biological (b-) disease-modifying antirheumatic drugs (DMARD) as decided by the treating physician. Additional information about the Pharmachild registry is previously reported [12]. The extracted Pharmachild data were locked on 12 November, 2020. Patients without available information for family history of AD were excluded from the current study.
Outcome and characteristics
Three researchers (JS, JvS and SdR) reviewed reported diseases in first degree relatives (i.e. mother and father) of the included JIA patients in order to ensure only definite diagnoses of ADs were included. Reported ADs were classified into the following categories: psoriasis, AITD, RA, ankylosing spondylitis, inflammatory bowel disease (IBD), JIA, asthma, IDDM, systemic lupus erythematosus, vitiligo, celiac disease, multiple sclerosis, uveitis, sarcoidosis, reactive arthritis, Sjögren’s syndrome, rheumatic fever, vasculitides, Still’s disease, familial Mediterranean fever, other autoimmune arthritis, other connective tissue disease and other AD. In addition, the following patient characteristics were collected: sex, geographic region, ethnicity, age at JIA onset, ILAR category of JIA, rheumatoid factor (RF) status, human leukocyte antigen (HLA) B27 status, antinuclear antibodies (ANA) status, number of active joints and clinical Juvenile Arthritis Disease Activity Score (cJADAS) at study entry and last visit and observation period (calculated from disease onset until last visit). Patients were grouped into the following geographic regions based on the country of the center in which they were treated: Western Europe, Central and Eastern Europe, Scandinavia, Northern Africa and the Middle East, Latin America and Southern Asia [13]. Ethnicity was reported at inclusion by the treating physician from a fixed set of categories. RF status was determined from two measurements at least 3 months apart according to ILAR criteria. Since not all patients had two available ANA tests, only the first test was used to determine ANA status. The cJADAS is a composite measure for disease activity that takes into account the number of active joints, physician global assessment of disease activity and parent/patient global assessment of well-being [14]. The latter two components of the cJADAS are measured on a 21-circle visual analogue scale ranging from 0 to 10 [15].
Statistical analysis
Characteristics of patients with a family history of AD and those without were compared using the χ2 test for categorical variables and Mann-Whitney U test for numerical variables. Pairwise comparisons of categories of geographic region, ethnicity and ILAR subtypes were performed with Bonferroni correction. For each AD category, prevalence rates among parents and corresponding 95% Poisson confidence intervals were calculated. Prevalence rates of ADs in the general population were collected from the literature. For this, we included data from worldwide literature reviews or surveillance studies. ILAR categories of patients with different familial ADs were compared using the Fisher’s exact test. All comparative analyses were performed on complete cases and a P-value of < 0.05 was considered statistically significant. All analyses were performed with R version 4.0.0.
Results
Patient characteristics
At the cut-off date, a total of 9111 JIA patients were enrolled in Pharmachild, of which 438 (4.8%) had no available information about parental ADs and were excluded from further analyses. For the remaining cohort of 8673 JIA patients, the total observation period was 43,800 years with a median duration of 4.0 years (IQR: 1.8–7.3). The median duration from disease onset until study entry was 139 days (IQR: 55–458). The majority of patients were treated in European centers (n = 7590; 87.5%) (Table 1). An overview of the classification of treatment center countries into geographic regions is provided in an additional table (see Additional file 1). Of all included patients, 1231 (14.2, 95% CI: 13.5–14.9%) had a family history of AD. Out of these, 1107 (89.9%) had a family history of one AD, 116 (9.4%) had a family history of two ADs and 8 (0.6%) had a family history of three or more ADs. Patients with a family history of AD more often had ERA, psoriatic arthritis and undifferentiated arthritis than patients without a family history of AD (P < 0.01), were more often ANA (P = 0.03) and HLA-B27 positive (P < 0.01) and had an older age at JIA onset (P < 0.01). Patients without a family history of JIA more often had systemic arthritis. Furthermore, the proportion of patients from Scandinavia and Southern Europe was higher in patients with a family history of AD than in patients without such family history (P < 0.01). The same effect was observed for patients of European Caucasian and Northern African or Middle Eastern ethnicity (P < 0.01). No significant differences in sex, RF status and disease activity were observed.
Prevalence rates of familial ADs
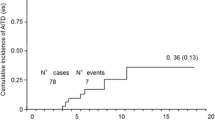
A total of 1366 ADs were reported in the parents (n = 17,346) of the included JIA patients. An overview of the classification of reported ADs is provided in an additional table (see Additional file 2). The most common diseases were psoriasis (n = 369; 2.1%), AITD (n = 275; 1.6%), RA (n = 141; 0.8%) and ankylosing spondylitis (n = 136; 0.8%). Prevalence rates of several ADs in parents of the included JIA patients were raised compared to reported prevalence rates in the general population, most notably ankylosing spondylitis, JIA and IDDM (Table 2). The observed prevalence of asthma and celiac disease was notably lower than the prevalence in the general population. The prevalence rates of separate diseases in the “other autoimmune disease” group are listed in an additional table (see Additional file 3). The distribution of ILAR categories amongst included JIA patients was significantly different for several familial ADs (Table 3). Of clinical relevance were the observations that patients with a family history of ankylosing spondylitis oftentimes had ERA or undifferentiated arthritis (P < 0.01), while patients with a family history of psoriasis oftentimes had psoriatic or undifferentiated arthritis (P < 0.01). For patients with different familial ADs, the absolute frequencies of ILAR categories are visualized in Fig. 1.
JIA categories of patients with and without familial autoimmune diseases. A: absolute frequencies of JIA categories for patients without familial autoimmune diseases. B-D: absolute frequencies of JIA categories for patients with different familial autoimmune diseases, each panel is displayed on a different scale. AITD: autoimmune thyroid disease, ERA: enthesitis-related arthritis, IBD: inflammatory bowel disease, IDDM: insulin-dependent diabetes mellitus, JIA: juvenile idiopathic arthritis, RA: rheumatoid arthritis, RF: rheumatoid factor
Discussion
The objective of this study was to present prevalence rates of ADs in parents of JIA patients and identify factors associated with such family history. According to our study, the prevalence rates of several ADs in parents of JIA patients are higher than those in the general population, with the most frequent familial ADs in JIA being psoriasis, AITD, RA and ankylosing spondylitis. Factors associated with a family history of AD in JIA are the geographic region, ethnicity, age at JIA onset, ILAR category, ANA status and HLA-B27 status.
In this study, the observed proportion of JIA patients with a family history of AD in first-degree relatives (14.2, 95% CI: 13.5–14.9%) was lower than in previous studies (21.4–31.8%) [4, 11]. This is possibly explained by the method of reporting familial autoimmunity in Pharmachild, differences in the target population and/or the definition of first-degree relatives. In Pharmachild, familial ADs are registered using self-reporting by the patient or parent, which might have led to an underestimation of the absolute prevalence of familial AD in JIA. Pharmachild furthermore defines a first-degree relative as the mother or father of a patient, whereas other definitions also include siblings. In addition, Pharmachild captures whether or not first degree relatives of JIA patients have a history of AD but does not distinguish between mother and father. Because of this, we could not report an overall prevalence of AD in parents since one parent can have a history of multiple ADs. Based on the number of JIA patients with a family history of AD (n = 1231) in parents (n = 17,346) and the total number of reported ADs (n = 1366), the overall prevalence of AD in parents would have to be little over 7.1% for the current study. This number is still higher than the reported prevalence of AD in the general population of nearly 5% [2, 3, 32], which is in accordance with previous studies [7, 11, 33, 34]. To our knowledge, no overall prevalence rate for AD has yet been reported for parents of JIA patients.
We observed several differences in characteristics of JIA patients with and without a family history of AD. A small study by Tronconi et al [8] did not find an association between a family history of AD and the subtype and age at onset of JIA. On the contrary, the current study observed that patients with psoriatic arthritis, undifferentiated arthritis and ERA reported relatively often a family history of AD as opposed to patients with systemic arthritis and oligoarthritis, which is also in line with two previous studies [4, 6]. The association between HLA-B27 and a family history of AD corresponds with the observed effect for JIA category, given that, 73.7% of ERA patients and 38.3% of undifferentiated arthritis patients in our study were HLA-B27 positive. The association of familial AD with psoriatic arthritis and ERA can be explained by the ILAR criteria of these categories, which includes a family history of psoriasis for psoriatic arthritis, and a family history of ankylosing spondylitis, ERA, sacroiliitis with IBD, Reiter’s syndrome or acute anterior uveitis for ERA [35]. Also, the high frequency of familial AD in the undifferentiated arthritis group is likely due to the fact that many JIA patients are assigned to this group because of a family history of psoriasis, which serves as an exclusion criterion for all other JIA categories except psoriatic arthritis. It has previously been discussed whether or not this exclusion criterion should be revised [36]. Indeed, we observed that a family history of psoriasis was relatively common for patients with psoriatic and undifferentiated JIA and a family history of ankylosing spondylitis and uveitis for ERA. It was furthermore interesting to see that a family history of AITD was relatively common in JIA patients with oligoarthritis, given that several studies have reported a link between oligoarthritis and AITD in JIA [33, 34, 37, 38]. On the other hand, a family history of AD was negatively associated with systemic arthritis in the current study. This can be explained by the autoinflammatory instead of autoimmune nature of this JIA category [1]. Previous studies have reported contradictory relationships between the age at JIA onset and a family history of AD [5, 6, 8, 39,40,41]. In this study, familial AD was associated with older age at JIA onset. It is unclear what causes this effect, but it might be confounded by the category of JIA since oligoarthritis commonly presents at a young age and ERA during late childhood [42]. We furthermore found that familial AD was associated with ANA positivity in the included JIA patients while previous studies report opposing results [5, 39, 40]. These differences might be due to the number and type of familial ADs investigated in each study. ANA are a marker of several ADs including AITD [43], which was a frequently reported AD in the parents of the included JIA patients. We also observed a statistically significant difference in the distribution of geographic regions. Patients from Scandinavia, Southern Europe, Western Europe, Northern Africa and the Middle East had relatively more often a family history of AD compared to patients from Central and Eastern Europe, Latin America and Southern Asia. The same effect was observed for patients of European Caucasian and Northern African or Middle Eastern ethnicity compared to patients of other ethnicities. These findings largely support existing epidemiological data on the worldwide distribution of AD, with higher relative frequencies in industrialized countries compared to developing countries [44]. Therefore, at the diagnosis stage of possible JIA, physicians might want to ask about a family history of AD especially in children of the before mentioned ethnicities with relatively increased prevalence. In the current study, we found no effect of familial autoimmunity on (the course of) disease activity in the included JIA patients. Previously, two studies reported that JIA patients with a family history of AD had higher disease activity and longer active disease duration than JIA patients without such family history [5, 6]. This contradiction might be a result of differences in the target population and study design, given that one of the mentioned studies included a highly consanguineous JIA population from Saudi Arabia and the other study only included JIA patients from Iran in a case-control design. Nevertheless, other studies indicate a more severe disease course and unfavorable outcome for psoriatic arthritis patients compared to other JIA categories [45, 46]. Also, it has been reported that a family history of AD is associated with the development of comorbidities in JIA [47, 48], which was beyond the scope of the current study.
Amongst others, psoriasis, RA, ankylosing spondylitis, JIA, IDDM and Still’s disease were more prevalent in parents of the included JIA patients than in the general population based on the available literature. Familial AD therefore proves to be a risk factor for JIA development. In a study of Finnish JIA patients, Pohjankoski et al. also observed higher prevalence rates of RA, spondyloarthropathy, psoriatic arthritis, JIA and IDDM in parents and full siblings of JIA patients compared to the general population [11]. The population prevalence rates for AITD reported in the literature varied to a large extent, most definitely due to differences in diagnostic criteria. Therefore, in the present study we could not conclude with certainty if AITD is more common in parents of JIA patients than in the general population. Nevertheless, a previous study reported that the prevalence of Hashimoto’s thyroiditis in first and second-degree relatives was significantly higher for JIA patients compared to age-matched healthy controls [7]. All these findings are consistent with the hypothesis that clinically distinct ADs share common genetic susceptibility factors [4]. On the other hand, the prevalence of asthma and celiac disease in our data was decreased compared to the reported general population prevalence rates, perhaps due to the self-reporting mechanism of capturing familial autoimmunity data in Pharmachild. As an example, many children outgrow asthma [49] and might therefore not report this disease in adulthood. Pohjankoski et al. also reported no increased frequency of celiac disease in families of JIA patients compared to the general population [11].
Our study has a few limitations. First, it is likely that the absolute prevalence of familial autoimmunity in JIA is underestimated by our data since these were gathered using self-reporting by the patients and their parents, as described previously. In order to minimize the probability of recall bias, we focused only on parents and did not include ADs in second and third-degree relatives. Secondly, the majority of included patients were treated in European centers, which might also have influenced prevalence rates of familial ADs. Lastly, since it was not possible to distinguish between male or female parents in our data, we could not study a possible parent-of-origin effect. A previous study has reported that the prevalence of ADs among mothers of JIA patients was significantly higher than that of fathers, suggesting a maternal parent-of-origin effect wherein the sex of the parent with an AD influences the expression of JIA in offspring [50].
Nevertheless, we present the largest study on familial AD in JIA so far. We included patients from multiple countries around the world, making it possible to study geographical differences in prevalence rates. We furthermore present information for all reported familial ADs in parents of JIA patients from the Pharmachild registry, and did not focus on a pre-selected set of diseases. This study confirms previously reported associations with familial AD in JIA and demonstrates that a family history of AD is not related to the disease course. These study results might provide useful information for pediatric rheumatologists at the diagnosis stage of a child with (possible) JIA.
Conclusions
In conclusion, we provide for the first time a comprehensive overview of the frequency of different ADs in parents of JIA patients. Several of these diseases have an increased prevalence compared to the general population. Psoriasis, AITD, RA and ankylosing spondylitis were most often reported and should therefore not be overlooked during family health history at the diagnosis stage of a child with possible JIA. A family history of AD is particularly associated with psoriatic arthritis, undifferentiated arthritis and ERA but does not influence the severity or course of JIA.
Availability of data and materials
All relevant data are reported in the article. Additional details can be provided by the corresponding author upon reasonable request. The Pharmachild registry is registered at Clinicaltrials.gov (NCT01399281) and at the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP; http://www.encepp.eu/encepp/viewResource.htm?id=19362).
Abbreviations
- AD:
-
Autoimmune disease
- ANA:
-
Antinuclear antibodies
- CD:
-
Crohn’s disease
- CI:
-
Confidence interval
- cJADAS:
-
Clinical JADAS
- ERA:
-
Enthesitis-related arthritis
- GD:
-
Graves’ disease
- HLA:
-
Human leukocyte antigen
- HT:
-
Hashimoto’s thyroiditis
- IQR:
-
Interquartile range
- IBD:
-
Inflammatory bowel disease
- IDDM:
-
Insulin-dependent diabetes mellitus
- ILAR:
-
International League of Associations for Rheumatology
- JIA:
-
Juvenile idiopathic arthritis
- oJIA:
-
Oligoarthritis
- pJIA:
-
Polyarthritis
- psJIA:
-
Psoriatic arthritis
- RA:
-
Rheumatoid arthritis
- RF:
-
Rheumatoid factor
- sJIA:
-
Systemic arthritis
- SLE:
-
Systemic lupus erythematosus
- UC:
-
Ulcerative colitis
- uJIA:
-
Undifferentiated arthritis
References
Martini A, Lovell DJ, Albani S, et al. Juvenile idiopathic arthritis. Nat Rev Dis Primers. 2022;8(1):5. Published 2022 Jan 27. https://doi.org/10.1038/s41572-021-00332-8.
Cárdenas-Roldán J, Rojas-Villarraga A, Anaya J-M. How do autoimmune diseases cluster in families? A systematic review and meta-analysis. BMC Med BioMed Central. 2013;11:1–22.
Anaya JM. Common mechanisms of autoimmune diseases (the autoimmune tautology). Autoimmun Rev Elsevier. 2012;11:781–4.
Prahalad S, McCracken CE, Ponder LA, Angeles-Han ST, Rouster Stevens KA, Vogler LB, et al. Familial autoimmunity in the childhood arthritis and rheumatology research alliance registry. Pediatr Rheumatol. 2016;14:1–7 2016 141. BioMed Central.
Khani M, Ziaee V, Moradinejad M-H, Parvaneh N. The effect of positive family history of autoimmunity in juvenile idiopathic arthritis characteristics; a case control study. Iran J Pediatr. 2013;23:569 Kowsar Medical Institute.
Al-Mayouf SM, Alrasheedi A, Almsellati I, Hashad S, Khawaja K, Abdwani R, et al. Familial aggregation of juvenile idiopathic arthritis with other autoimmune diseases: impact on clinical characteristics, disease activity status and disease damage. Int J Rheum Dis. John Wiley & Sons, Ltd. 2021;24:1080–5.
Prahalad S, Shear E, Thompson S, Giannini E, Glass D. Increased prevalence of familial autoimmunity in simplex and multiplex families with juvenile rheumatoid arthritis. Arthritis Rheum. 2002;46:1851–6.
Tronconi E, Miniaci A, Pession A. The autoimmune burden in juvenile idiopathic arthritis. Ital J Pediatr. 2017;43:1–6.
Huang C, Yang Y, Chiang B. Different familial association patterns of autoimmune diseases between juvenile-onset systemic lupus erythematosus and juvenile rheumatoid arthritis. J Microbiol Immunol Infect. 2004;37:88–94.
Pachman LM, Hayford JR, Hochberg MC, Pallansch MA, Chung A, Daugherty CD, et al. New-onset juvenile dermatomyositis. Comparisons with a healthy cohort and children with juvenile rheumatoid arthritis. Arthritis Rheum. 1997;40:1526–33 John Wiley & Sons, Ltd.
Pohjankoski H, Kautiainen H, Kotaniemi K, Korppi M, Savolainen A. Diabetes, coeliac disease, multiple sclerosis and chronic arthritis in first-degree relatives of patients with juvenile idiopathic arthritis, vol. 101: Acta Paediatr; 2012. p. 767–71. John Wiley & Sons, Ltd
Swart J, Giancane G, Horneff G, Magnusson B, Hofer M, Alexeeva Е, et al. Pharmacovigilance in juvenile idiopathic arthritis patients treated with biologic or synthetic drugs: combined data of more than 15,000 patients from Pharmachild and national registries. Arthritis Res Ther. 2018;20:285.
Consolaro A, Giancane G, Alongi A, van Dijkhuizen EHP, Aggarwal A, Al-Mayouf SM, et al. Phenotypic variability and disparities in treatment and outcomes of childhood arthritis throughout the world: an observational cohort study. Lancet Child Adolesc Heal. 2019;3:255–63.
Swart JF, EHP VD, Wulffraat NM, De Roock S. Clinical Juvenile Arthritis Disease Activity Score proves to be a useful tool in treat-to-target therapy in juvenile idiopathic arthritis. Ann Rheum Dis. 2018;77:336–42
Filocamo G, Davì S, Pistorio A, Bertamino M, Ruperto N, Lattanzi B, et al. Evaluation of 21-numbered circle and 10-centimeter horizontal line visual analog scales for physician and parent subjective ratings in juvenile idiopathic arthritis. J Rheumatol. 2010;37:1534–41.
Parisi R, Iskandar IYK, Kontopantelis E, et al. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;369:m1590. Published 2020 May 28. https://doi.org/10.1136/bmj.m1590.
Vanderpump MPJ. The epidemiology of thyroid disease. Br Med Bull. 2011;99:39–51.
Almutairi K, Nossent J, Preen D, Keen H, Inderjeeth C. The global prevalence of rheumatoid arthritis: a meta-analysis based on a systematic review. Rheumatol Int. 2020;41:863–77 2020 415 Springer.
Stolwijk C, Onna M v, Boonen A, Tubergen A v. Global prevalence of Spondyloarthritis: a systematic review and Meta-regression analysis. Arthritis Care Res (Hoboken). 2016;68:1320–31 John Wiley & Sons, Ltd.
Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390:2769–78.
Thierry S, Fautrel B, Lemelle I, Guillemin F. Prevalence and incidence of juvenile idiopathic arthritis: a systematic review. Joint Bone Spine. 2014;81(2):112-7. https://doi.org/10.1016/j.jbspin.2013.09.003.
To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12:204.
Mobasseri M, Shirmohammadi M, Amiri T, Vahed N, Fard HH, Ghojazadeh M. Prevalence and incidence of type 1 diabetes in the world: a systematic review and meta-analysis. Heal Promot Perspect. 2020;10:98 Tabriz University of Medical Sciences.
Rees F, Doherty M, Grainge MJ, Lanyon P, Zhang W. The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology Oxford. 2017;56:1945–61.
Zhang Y, Cai Y, Shi M, Jiang S, Cui S, Wu Y, et al. The prevalence of Vitiligo: a Meta-analysis. PLoS One. Public Library of Science. 2016;11:163806.
Singh P, Arora A, Strand TA, Leffler DA, Catassi C, Green PH, et al. Global prevalence of celiac disease: systematic review and Meta-analysis. Clin Gastroenterol Hepatol. 2018;16:823–836.e2 WB Saunders.
García-Aparicio Á, García de Yébenes MJ, Otón T, Muñoz-Fernández S. Prevalence and Incidence of Uveitis: A Systematic Review and Meta-analysis. Ophthalmic Epidemiol. 2021;28(6):461-8. https://doi.org/10.1080/09286586.2021.1882506.
Wallin MT, Culpepper WJ, Nichols E, Bhutta ZA, Gebrehiwot TT, Hay SI, et al. Global, regional, and national burden of multiple sclerosis 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019;18:269–85.
Arkema EV, Cozier YC. Sarcoidosis epidemiology: recent estimates of incidence, prevalence and risk factors. Curr Opin Pulm Med. 2020;26(5):527-34. https://doi.org/10.1097/MCP.0000000000000715.
Qin B, Wang J, Yang Z, Yang M, Ma N, Huang F, et al. Epidemiology of primary Sjögren’s syndrome: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74:1983–9 BMJ Publishing Group Ltd.
Efthimiou P, Kontzias A, Hur P, Rodha K, Ramakrishna GS, Nakasato P. Adult-onset Still’s disease in focus: clinical manifestations, diagnosis, treatment, and unmet needs in the era of targeted therapies. Semin Arthritis Rheum. 2021;51:858–74 WB Saunders.
Wang L, Wang F-S, Gershwin ME. Human autoimmune diseases: a comprehensive update. J Intern Med. 2015;278:369–95 John Wiley & Sons, Ltd.
Stagi S, Giani T, Simonini G, Falcini F. Thyroid function, autoimmune thyroiditis and coeliac disease in juvenile idiopathic arthritis. Rheumatology. 2005;44:517–20 Oxford Academic.
Robazzi TC, Adan LF, Pimentel K, Guimarães I, Magalhães Filho J, Toralles MB, et al. Autoimmune endocrine disorders and coeliac disease in children and adolescents with juvenile idiopathic arthritis and rheumatic fever. Clin Exp Rheumatol. 2013;31:0310–7.
Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, et al. International league of associations for rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31:390–2.
Chan MO, Petty RE, Guzman J. A family history of psoriasis in a first-degree relative in children with JIA: to include or exclude? J Rheumatol. 2016;43:944–7.
Harel L, Prais D, Uziel Y, et al. Increased prevalence of antithyroid antibodies and subclinical hypothyroidism in children with juvenile idiopathic arthritis. J Rheumatol. 2006;33(1):164-6.
Alpigiani M, Cerboni M, Bertini I, D’Annunzio G, Haupt R, Iester A, et al. Endocrine autoimmunity in young patients with juvenile chronic arthritis. Clin Exp Rheumatol. 2002;20:565–8.
Moroldo MB, Chaudhari M, Shear E, Thompson SD, Glass DN, Giannini EH. Juvenile rheumatoid arthritis affected sibpairs: Extent of clinical phenotype concordance. Arthritis Rheum. 2004;50:1928–34 John Wiley & Sons, Ltd.
Säilä HM, Savolainen HA, Kotaniemi KM, Kaipiainen-Seppänen OA, Leirisalo-Repo MT, Aho KV. Juvenile idiopathic arthritis in multicase families. Clin Exp Rheumatol. 2001;19:218–20.
Al-Mayouf SM, Madi SM, AlMane K, Al Jummah S. Comparison of clinical and laboratory variables in familial versus sporadic systemic onset juvenile idiopathic arthritis. J Rheumatol. 2006;33(3):597-600.
Ravelli A, Martini A. Juvenile idiopathic arthritis. Lancet. 2007;369:767–78.
Segni M, Pucarelli I, Truglia S, Turriziani I, Serafinelli C, Conti F. High prevalence of antinuclear antibodies in children with thyroid autoimmunity. J Immunol Res. 2014;2014:150239. https://doi.org/10.1155/2014/150239.
Bach JF. The hygiene hypothesis in autoimmunity: the role of pathogens and commensals. Nat Rev Immunol. 2017;18:105–20 Nature Publishing Group.
Flatø B, Lien G, Smerdel-Ramoya A, Vinje O. Juvenile psoriatic arthritis: Longterm outcome and differentiation from other subtypes of juvenile idiopathic arthritis. J Rheumatol. 2009;36:642–50.
Ekelund M, Aalto K, Fasth A, et al. Psoriasis and associated variables in classification and outcome of juvenile idiopathic arthritis - an eight-year follow-up study. Pediatr Rheumatol Online J. 2017;15(1):13. Published 2017 Feb 22. https://doi.org/10.1186/s12969-017-0145-5.
Ünsal E, Ören O, Salar K, Makay B, Abacı A, Özhan B, et al. The frequency of autoimmune thyroid disorders in juvenile idiopathic arthritis. Turk J Pediatr. 2008;50:462–5.
van Straalen JW, Krol RM, Giancane G, et al. Increased incidence of inflammatory bowel disease on etanercept in juvenile idiopathic arthritis regardless of concomitant methotrexate use. Rheumatology (Oxford). 2022;61(5):2104-12. https://doi.org/10.1093/rheumatology/keab678.
Trivedi M, Denton E. Asthma in children and adults—what are the differences and what can they tell us about asthma? Front Pediatr. 2019;7:256 Frontiers Media SA.
Zeft A, Shear ES, Thompson SD, Glass DN, Prahalad S. Familial autoimmunity: maternal parent-of-origin effect in juvenile idiopathic arthritis. Clin Rheumatol. 2008;27:241–4.
Acknowledgements
The authors would like to thank all PRINTO centers for their contribution to the data collection and PRINTO personnel for data quality control. The authors furthermore express their acknowledgements to the European Reference Network for Immunodeficiency, Autoinflammatory, Autoimmune and Paediatric Rheumatic diseases (ERN-RITA). We also thank all patients and their parents or guardians for participating in Pharmachild.
Funding
This work was supported by a research grant from FOREUM Foundation for Research in Rheumatology. Pharmachild has been supported by funding from the Italian public hospital IRCCS Istituto Giannina Gaslini and a grant from the European Union (grant 260353).
Author information
Authors and Affiliations
Consortia
Contributions
JvS performed the data-analysis and drafted the final manuscript. JS and SdR conceptualized and designed the study and critically reviewed and revised the manuscript. GG, EA, EK, PMC, FZ, AC, DM, NW and NR collected data and critically reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Pharmachild and all participating centers obtained approval from their respective ethics committees and were conducted in accordance with the Declaration of Helsinki. All patients provided written informed consent/assent based on existing national regulations.
Consent for publication
Not applicable.
Competing interests
NR has received honoraria for consultancies or speaker bureaus from the following pharmaceutical companies in the past 3 years: 2 Bridge, Amgen, AstraZeneca, Aurinia, Bayer, Brystol Myers and Squibb, Celgene, inMed, Cambridge Healthcare Research, Domain Therapeutic, EMD Serono, Glaxo Smith Kline, Idorsia, Janssen, Eli Lilly, Novartis, Pfizer, Sobi, UCB.
The IRCCS Istituto Giannina Gaslini (IGG), where NR works as full-time public employee has received contributions from the following industries in the last 3 years: Bristol Myers and Squibb, Eli-Lilly, F Hoffmann-La Roche, Novartis, Pfizer, Sobi. This funding has been reinvested for the research activities of the hospital in a fully independent manner, without any commitment with third parties.
All other authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Classification of treatment center countries of JIA patients into geographic regions.
Additional file 2.
Classification of reported autoimmune diseases in parents of included JIA patients.
Additional file 3.
Prevalence rates of diseases from the “other autoimmune disease” category in parents of included JIA patients (n = 17,346).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
van Straalen, J.W., de Roock, S., Giancane, G. et al. Prevalence of familial autoimmune diseases in juvenile idiopathic arthritis: results from the international Pharmachild registry. Pediatr Rheumatol 20, 103 (2022). https://doi.org/10.1186/s12969-022-00762-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12969-022-00762-y